Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Follicular unit hair transplantation (FUHT) is a method of hair restoration surgery that relocates permanent donor hair to balding areas in naturally occurring follicular unit hair groupings. The small size of the units allows for tremendous versatility in their placement, the creation of hair patterns that closely mimic nature, and the transplantation of a large enough number of grafts so that a full restoration can often be achieved in just one or two sessions.
In follicular unit transplantation (FUT), the donor hair is harvested from the back and sides of the scalp via a long, thin strip and then dissected into individual follicular units using stereo-microscopes. In follicular unit extraction (FUE), individual follicular units are removed directly from the donor area through tiny round incisions. Follicular unit hair transplantation requires large numbers of grafts, so it is important to accurately assess patients' donor reserves in the initial planning. Densitometry enables the physician to estimate the total amount of movable hair, the size of the individual follicular units, and the degree of miniaturization in both the donor and recipient areas; scalp laxity assessment is also crucial to the surgical planning.
Great care should be taken to screen for patients who are too young for hair restoration surgery or whose hair loss may be diffuse, making the donor supply inadequate for a hair transplant.
Identifying androgenetic alopecia often proves difficult in women as other medical conditions can have a similar presentation. Options for medical treatment are more limited in women and many experience diffuse hair loss, a relative contraindication to surgery.
Determining the right size and location of the donor area maximizes the yield and prevents problems such as widened and/or visible scars.
The follicular units obtained from the donor area are delicate structures. Careful dissection, gentle handling, and adequate hydration are essential to their survival. In order to dissect and place the thousands of grafts often required in follicular unit transplantation, the surgical team must be proficient in stereomicroscopic dissection and insertion techniques – skills that can take a year or more to develop. Follicular unit extraction requires its own sets of skills, some of them now being performed robotically.
Follicular unit hair transplantation requires an astute aesthetic sense for optimal hairline design, correct angling and distribution of grafts, and the establishment of a master plan that anticipates further hair loss and is consistent with the long-term goals of the patient.
Within the past two decades, follicular unit hair transplantation has transformed hair restoration surgery from a cosmetically unpredictable procedure to one that can produce consistently natural results. The key to its effectiveness lies in the fact that scalp hair tends to grow in tiny bundles, called “follicular units,” rather than individually. By working with these naturally occurring units, instead of larger or smaller grafts, one can create as natural a look as possible, while minimizing the transplant wound size and accelerating postoperative healing.
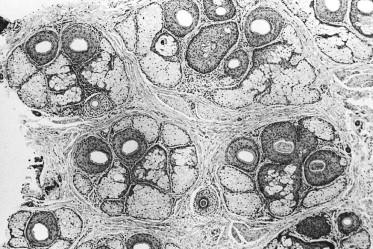
Follicular units are made up of 1–4 terminal hairs, 1–2 vellus hairs, their associated sebaceous glands, neurovascular plexus, an erector pilorum muscle, and a circumferential band of adventitial collagen, the perifolliculum. The tendency of scalp hair to grow in this way, rather than as single hairs, can be most easily demonstrated by clipping the hair to approximately 1 mm in length and then viewing it with a densitometer ( Fig. 30.1 ) at ×30 magnification in a 10 mm field. What this also reveals is that these compact units are surrounded by significant amounts of non-hair-bearing scalp ( Fig. 30.2 ). Including this extra skin in the dissection – as do transplants with larger grafts, such as plugs and mini-grafts – requires a larger recipient wound, as well as risking visible scarring in the skin around the grafts and distortions of the growing hair.


Follicular unit hair transplantation takes advantage of the anatomic proximity of the hairs within each unit to:
Keep the recipient site wound size to a minimum
Prevent skin surface change in the recipient area
Facilitate postoperative healing
Enable grafts to be placed very close together
Permit large numbers of grafts to be safely transplanted in a single session (because of the small recipient wound size).
The ability to insert up to four hairs in a tiny recipient site is especially valuable cosmetically and has been instrumental in eliminating the see-through quality of older micrografting techniques where follicular units were not kept whole. When using follicular units, the transplanted hair will look natural – given that the transplant surgeon makes the right aesthetic decisions about graft placement, angling, and distribution.
Follicular unit hair transplantation (FUHT) is the general term used for hair restoration surgery using individual follicular units. In follicular unit transplantation (FUT), the donor hair is harvested from the back and sides of the scalp via a long, thin strip and then dissected into individual follicular units using stereomicroscopes. In follicular unit extraction (FUE), individual follicular units are removed directly from the donor area through tiny round incisions.
The purpose of this chapter is to describe the basic technical skills and aesthetic judgments involved in FUHT. It should be taken as a framework for physicians interested in learning the procedure, not an exhaustive review of the various surgical techniques used in FUHT or of other hair restoration methods. The chapter will not cover mini-micrografting; the combining of large and small grafts; laser hair transplantation; scalp reductions; scalp lifts; or flaps. These procedures are infrequently used today and have been detailed in many excellent publications, as well as in two comprehensive textbooks.
When learning FUHT, the importance of hands-on experience and beginning with small sessions until skills develop cannot be overemphasized. Having a well-trained team of assistants is also important to a successful outcome, particularly for those procedures involving a large number of grafts.
Although simple in concept, FUHT has many nuances and complexities. Those wishing to perform FUT in their clinical practice are encouraged to join the International Society of Hair Restoration Surgery (ISHRS) and attend its annual meeting, to subscribe to Hair Transplant Forum International (the trade publication for hair restoration surgeons), and to follow relevant medical literature. Although it is an independent board, certification by the American Board of Hair Restoration Surgery (ABHRS) indicates a basic competency in the field. Certification requires several years of clinical experience and passing both oral and written examinations. The process of preparing for ABHRS certification is a worthwhile endeavor and recommended for those serious about surgical hair restoration.
Reports of successful hair transplants appeared as early as 1930 in the Japanese literature, beginning with Sasagawa's hair-shaft insertion procedure and then Okuda's technique of using 2–4 mm punches for the treatment of various alopecias of the scalp, eyebrows, and moustache. Okuda made the important observation that using smaller punches in the recipient area improved cosmetic results.
By 1943, Tamura had treated 137 cases of non-androgenetic alopecia of various etiologies using techniques very similar to modern day hair transplantation. For instance, he harvested donor grafts by making an elliptical incision that was sutured closed, prepared recipient sites with a thick needle, stored grafts in physiologic saline, and observed postoperative telogen effluvium (shedding). Most significantly, Tamura demonstrated that single-hair grafting resulted in growth practically indistinguishable from naturally grown hair – and much more natural looking than transplants using larger grafts. Unfortunately, it took several decades before Western surgeons would apply Tamura's insights to their hair restoration procedures.
The first hair transplant in the USA was performed by Dr Norman Orentreich in 1952, with grafts measuring 6–8 mm in diameter, significantly larger than those of either Tamura or Okuda. At first, incredulous editors rejected Orentreich's work, not believing that hair transplantation was even possible. In 1959, the Annals of the New York Academy of Science finally agreed to publish his work. The paper laid out the concept of “donor dominance” – the idea that grafts continue to show the characteristics of the donor site after they have been transplanted to a new location. This remains the basic tenet of all hair transplantation surgery. Yet, while donor dominance insured that transplanted hair could grow, it did not guarantee that the results would look natural.
Not until 40 years later would hair transplants in the USA start to produce consistently natural-looking results and promise predictable cosmetic improvements in most patients. It was a slow evolution, but the large grafts used throughout the 1960s and 1970s eventually gave way to mini-grafts in the 1980s and mini-micrografting in the early 1990s. The stage was then set for follicular unit transplantation. First appearing in the medical literature in 1995, it quickly emerged as the gold standard – supplanting mini-micrografting in the treatment of androgenetic alopecia and rendering other well-established procedures such as scalp reductions, scalp lifts, and flaps virtually obsolete.
So swift was the ascent of FUT that the two standard textbooks on surgical hair restoration, published in 1995 and 1996, as well as the most comprehensive text on trichology, published in 1997, make not one mention of the terms “follicular unit” or “follicular unit transplantation.” At the 1996 meeting of the ISHRS, three 7-min presentations on the procedure were given; but at the 2002 meeting, FUT was the subject of entire seminars and workshops and suffused every aspect of the week-long gathering.
The follicular unit was first defined by Headington in his landmark 1984 paper entitled “Transverse microscopic anatomy of the human scalp.” Follicular unit transplantation had its origins in the microscopic dissection techniques of Dr Limmer in 1988 that was described in his paper, “Elliptical donor stereoscopically assisted micrografting as an approach to further refinement in hair transplantation” in 1994. The term “follicular unit” was introduced into the hair transplant literature by Bernstein and colleagues in 1995. The conceptual framework for FUT was mapped out by these authors in their 1995 publication “Follicular transplantation” and in the paired articles “Follicular transplantation: patient evaluation and surgical planning” and “The aesthetics of follicular transplantation” in 1997.
The name “follicular unit transplantation” was formalized by a group of hair restoration surgeons in 1998. In this paper, the procedure was precisely defined and included the two basic techniques: single-strip harvesting and stereomicroscopic dissection, as integral parts of the procedure. However, because follicular units can now be harvested directly from the donor area without the necessity of a strip incision (using follicular unit extraction ), the original definition has become too restrictive.
The term follicular unit hair transplantation (FUHT) should now be used to encompass all hair restoration procedures that utilize naturally occurring individual follicular units exclusively in the surgery, regardless of how these units are harvested. Follicular unit transplantation (FUT) refers to the technique of obtaining follicular units through the microscopic dissection of a donor strip and follicular unit extraction (FUE) refers to harvesting individual units directly from the scalp. In 2011, the first follicular unit extraction procedure was performed using a video-guided robotic device and a new acronym was introduced into the field of hair transplant surgery, R-FUE.
The diagnosis of androgenetic alopecia in men is usually straightforward. It is made by observing a “patterned” distribution of hair loss. It is confirmed by the presence of miniaturized hairs in the areas of thinning. The diagnosis is supported by a history of baldness in the family. In women, the diagnosis is more complex since the most common presentation, a diffuse pattern, can be mimicked by a host of non-androgenetic etiologies.
Miniaturization – the progressive diminution of the hair shaft's diameter and length in response to androgens – can be most readily observed with a densitometer, a hand-held instrument that magnifies a small area of the scalp where the hair has been clipped to about 1 mm. One type, the Rassman densitometer, magnifies by ×30 in a visual field of 10 mm 2 , making it easy to identify miniaturization and calculate hair density ( Figs 30.1–30.3 ). With video-densitometry ( Fig. 30.1B ), the doctor can project the image onto a computer screen so that it is immediately visible to the patient. It can also provide a permanent digital record of the person's density and miniaturization status.
When describing hair loss, particularly in the early phases, it is preferable to think in terms of changes in volume rather than density. Density is simply the number of hairs per unit area, whereas volume reflects both hair shaft diameter as well as the absolute numbers of hairs.
A new device, called the Cross Section Trichometer, takes both of these factors into account by measuring the cross-sectional area of a demarcated bundle of hair. This instrument measures hair mass – the cross-sectional area of a bundle of hair present in a premeasured area of scalp. It detects small changes in both hair density and diameter. Since the earliest sign of hair loss results in volume changes caused by individual hairs decreasing in size (miniaturization) without a decrease in number, devices that can assess hair shaft diameter are useful for identifying early hair loss. Only in more advanced balding will the actual number of hairs start to decrease.
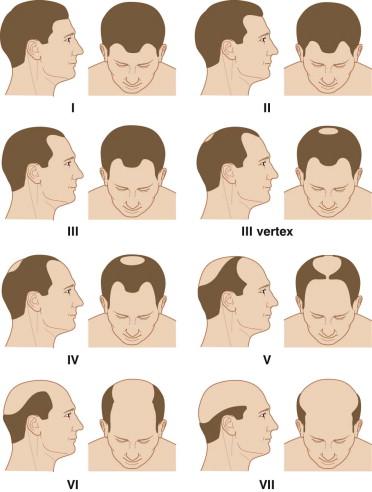
The Norwood classification of male pattern hair loss, published in 1975, remains the most widely used. It defines two major patterns and several less common types ( Fig. 30.4 ). In the regular Norwood pattern, two areas of hair loss – a bitemporal recession and thinning crown – gradually enlarge and coalesce until the entire front, top, and crown (vertex) of the scalp are bald. A less common Norwood variety, Norwood class A, is characterized by a distinctly anterior-to-posterior progression, usually resulting in baldness on the front and top of the scalp, but more limited loss in the crown. In both patterns, the sides and back tend to resist androgenetic changes, though the sides may exhibit significant thinning in senile alopecia.
Two other types of genetic hair loss not emphasized in the literature – diffuse patterned alopecia (DPA) and diffuse unpatterned alopecia (DUPA) – pose the greatest challenge both for diagnosis and patient management. A thorough familiarity with all of these patterns is essential for diagnosing androgenetic alopecia and planning FUHT ( Table 30.1 ).
| Norwood classes | Regular classes I –VII |
| Type A variant (IIA–VA) | |
| Variations: persistent frontal forelock; persistent frontal hairline | |
| Diffuse androgenic alopecias | Diffuse patterned alopecia (DPA) |
| Diffuse unpatterned alopecia (DUPA) | |
| Senile alopecia | |
| Female pattern alopecia | Ludwig classes I–III |
DPA is an androgenetic alopecia that manifests as diffuse thinning in the front, top, and vertex, with a stable permanent zone. In DPA, the entire top of the scalp gradually miniaturizes without passing through the typical Norwood stages. DUPA is also androgenetic but lacks a stable permanent zone. It affects men much less often than DPA. DUPA tends to progress more rapidly than DPA and eventuates in a horseshoe pattern resembling the Norwood class VII. However, unlike the Norwood class VII, the DUPA horseshoe can look almost transparent due to the low density of the back and sides. Differentiating between DPA and DUPA is very important because DPA patients often make good transplant candidates, whereas DUPA patients almost never do, as they inevitably have extensive hair loss without a stable zone for harvesting.
The early warning signs of DUPA include:
A rapid decrease in hair volume and a change in hair texture at an early age, often in the teens
The maintenance of an adolescent hair pattern and persistent frontal hairline in spite of dramatic volume change
A see-through donor area (most easily visualized when the hair is wet or lifted up)
Significant miniaturization of the donor area (>35%)
A donor density of <1.5 hairs per mm 2 .
The sensitivity of densitometry in detecting early DUPA justifies its routine use in the evaluation of hair loss. Once a diagnosis of DUPA is considered, any decisions regarding surgical hair restoration should be postponed. The possibility of missing a DUPA diagnosis is one of the most powerful arguments against performing hair transplantation at an early age.
Both DPA and DUPA occur in women but, in contrast to men, DUPA is far more common. As with men, women with DUPA do not make good transplant candidates (except possibly when donor hair is used solely to soften the frontal edge of a wig). Indeed, the higher DUPA incidence in women explains why a smaller proportion of women than men qualify as transplant candidates. Interestingly, the most common classification used for women, the Ludwig classification, does not differentiate between DPA and DUPA.
There is a home test that screens for variations in the androgen receptor gene on the X chromosome, a gene associated with male pattern hair loss. Its purpose is to identify persons at increased risk of developing hair loss before it is clinically apparent so that medical intervention can be started early, when it is most effective. The presence of one of the variants indicates a moderately increased risk for the development of androgenetic alopecia and the other indicates a substantially decreased risk of becoming bald. A similar screening test is also available for the detection of hair loss in women.
It is important to realize that these markers reveal an association with hair loss and that a cause and effect relationship has not been proven. A danger is that patients may overreact to this relatively incomplete information. It is best to have the tests performed under a doctor's supervision so that the results can be put in the context of other information that the physician gleans through a careful history and physical and so that the patient may be properly counselled.
It is important to emphasize that a non-androgenetic differential must be considered in all cases of unpatterned alopecia because a wide variety of medical conditions can produce diffuse hair loss. This is particularly relevant in evaluating women since unpatterned hair loss is the rule rather than the exception ( Box 30.1 ). The following laboratory tests are often useful when a non-androgenetic cause for diffuse hair loss is suspected: chemistry screen, complete blood count, serum iron, total iron-binding capacity, tri-iodothyronine, thyroxine, thyroid-stimulating hormone, antinuclear antibody, and serologic test for syphilis.
Anemia.
Endocrine diseases (especially thyroid)
Connective tissue disease
Obstetric/gynecologic conditions (e.g., postpartum, polycystic ovarian disease)
Weight loss (especially crash diets)
Emotional and physical stress (e.g., surgery, anesthesia)
Medications: oral contraceptives, thyroid drugs, anti-hypertensives (especially β-blockers), psychotropics, anticoagulants, antilipemics, gout therapy, prednisone, excessive vitamin A or tryptophan use
In women, diffuse or patterned hair loss may be a sign of excessive androgen production. A further medical evaluation is indicated when the hair loss is associated with any of the following: cystic acne, irregular menses, hirsutism, virilization, infertility, or galactorrhea. Serum levels of dehydroepiandrosterone (DHEA) sulfate, androstenedione, total and free testosterone, and prolactin can serve as a useful screen.
When the diagnosis of androgenetic alopecia is uncertain, further diagnostic information can be gleaned from a hair-pull test for telogen effluvium, a potassium hydroxide mount and culture for fungus, a microscopic examination of the hair bulb and shaft, and a scalp biopsy (sectioned horizontally). A dermatologic consultation is warranted whenever the diagnosis of hair loss is unclear.
In all cosmetic procedures, a successful outcome depends on proper patient selection ( Box 30.2 ). In surgical hair restoration, proper timing is also crucial. There are no medical or surgical advantages to transplanting at an early age. The popular rationale that transplants should be performed at a young age so that “no one will notice” does not make sense: if there is nothing to notice from the transplant, why perform it in the first place? FUHT heals so quickly and the hair growth is so gradual that, once the short postoperative period ends, the process is almost always undetectable. When hair loss is early, medical therapy is the treatment of choice.
Age 25 years or older
Inadequate response to medication after 1 year
Significant hair loss: Norwood class III or greater
Diffuse unpatterned alopecia (DUPA) has been ruled out
Non-androgenetic causes of hair loss have been ruled out a
a Many non-androgenetic causes of hair loss can be treated with hair transplantation.
No medical contraindications to surgery (drug sensitivities, keloids, connective tissue disease) b
b Some are relative contraindications.
Reasonable patient expectations
Patients seeking hair transplantation while still in their early 20s invariably wish to have their adolescent hairline and original density restored. Since neither of these goals can be achieved surgically without compromising the patient's future appearance, the procedure should not be performed at this age. It should be explained that hair transplantation moves, rather than creates, hair. It does not increase overall hair volume. In fact, the challenge is to have the pattern of the transplanted hair take into account the person's ever-decreasing total hair mass. In other words, patients who will have significant balding need to have built-in temporal recession, and possibly a crown that is significantly thinner than the surrounding hair, for the transplant to look natural over time. Unfortunately, neither of these is generally acceptable to a young man in his early 20s.
Another reason to postpone transplants for those under 25 years, or with only limited hair loss, is to give medications – minoxidil and finasteride – adequate time to work. As patients may continue to show regrowth for 1–2 years after treatment is initiated, they should in general use medical therapy at least this long before surgery is considered. It is inappropriate, therefore, to start younger patients on minoxidil and finasteride and schedule surgery at the same time. Fortunately, minoxidil and finasteride work best in younger patients, and especially those with large areas of miniaturized hair, rather than areas that are totally bald. On the other hand, for older patients who would be taking medication to maintain rather than regrow hair, and for those whose advanced state of hair loss makes results from minoxidil and finasteride unlikely, the medications may be prescribed concomitantly with surgery.
With the availability of finasteride, medication plays an increasingly important role in the management of androgenetic hair loss. Although the incidence is small (2–4%), the fear of possible sexual side-effects has turned many against this drug. Some also consider surgery a more conservative form of treatment than the potential lifetime use of medication. Because of these concerns and the pressure from patients for surgery's apparent “quick fix,” the physician should take time to thoroughly discuss the pros and cons of medical therapy.
In the Norwood classification, class I represents a normal adolescent pattern and class II a normal non-balding adult. Therefore, as a minimum, patients should qualify as class III before transplants are contemplated. Early class III patients will often benefit from medication alone, so this should be considered first.
Although the opportunities for a complete restoration in a person who is extensively bald (i.e., a Norwood class VII) is limited, extensive balding is not necessarily a contraindication to surgery. If the person's donor zone is stable (miniaturization of <20%) and the patient's expectations are commensurate with his or her limited available donor supply, a hair transplant may be considered. As long as the patient is in good health, there is no upper age limit for surgery. In fact, older patients tend to have the most reasonable expectations and are often the most satisfied. Even a small amount of hair can make a dramatic improvement in the appearance of a person who has been bald for many years.
There are few absolute medical contraindications to surgical hair restoration, particularly because it is an outpatient procedure not requiring general anesthesia. Relative contraindications include: bleeding disorders, drugs that increase bleeding such as clopidogrel (Plavix), immunodeficiency, unstable arrhythmias, chronic obstructive pulmonary disease, sensitivity to local anesthetics or epinephrine, a history of keloid formation or connective tissue disease, and major psychiatric disorders. When in doubt about the patient's medical condition, it is always best to get medical clearance from their primary physician.
Patients should be able to tolerate being in the surgical chair for a good part of the day; consequently, back and neck problems as well as claustrophobia can sometimes make the procedure problematic. Special care should be taken when evaluating patients with significant psychiatric issues, particularly depression, trichotillomania, body dysmorphic disorder, or severe obsessive compulsive disorder. In such cases, a psychiatrist or psychologist should participate in the decision-making process.
Possibly the most difficult aspect of the consultation is managing patients' expectations. It is almost a cliché to say that they must have “reasonable expectations,” but ensuring this is the essence of the evaluation. The surgeon cannot stress strongly enough that because hair restoration procedures move rather than create hair, the resulting transplanted density will be significantly less than the person's non-balding density. It is also important to emphasize that it is the patient's own hair from the sides and back of the head that will be transplanted. Therefore, the final result can be best described with reference to the texture, color, curl, and other qualities of the person's existing hair. It is also helpful to provide prospective patients with printed material and photos, and to make past patients available for them to speak with or meet.
The main factors in determining total donor reserves are donor density, scalp laxity, and the physical size of the donor area.
The number of follicular units in the mid-portion of the donor area of a normal non-Hispanic white man who has not had surgery is approximately 70–95 follicular units per cm 2 . In the first procedure, therefore, the donor area should yield approximately 70–95 follicular grafts per cm 2 of scalp, provided there is no significant wastage during surgery. The average yield declines when longer strips are taken because density decreases towards the sides. In some people, density varies dramatically throughout the donor area and this must be accounted for in the surgical planning. Follicular unit density also varies according to race; therefore the number of grafts obtained per unit area of donor tissue will exhibit racial variability and must be accounted for in the surgical planning.
In general, as hair density increases (hairs/cm 2 ) the number of hairs per follicular unit (hairs/FU) increases rather than follicular units being spaced closer together (FU/cm 2 ). If the scalp has been stretched from previous transplants, scalp reductions, or scalp lifts, the follicular units will be spaced further apart.
Donor scarring from previous surgeries will also significantly diminish the donor yield. All donor harvests, no matter how perfectly executed, entail some loss of hair. In addition, the angle of the hair surrounding the scar will be altered slightly, creating more transection in any subsequent harvest.
A person can lose a substantial amount of hair volume – either due to actual loss of hair or to miniaturization – before it becomes noticeable. When hair is blond or white, it takes longer for thinning to show. Thinning is most evident in persons with black hair and white skin. For those with average density and average hair attributes, approximately half of the hair in the donor area may be moved without a significant change in appearance.
Scalp laxity (looseness) is an important factor in determining a person's total available donor hair. There appears to be two main factors that contribute to laxity: redundancy and distensibility. Redundancy is simply extra scalp skin. Distensibility is the ability of the scalp to stretch. In those with lax scalps due to redundancy, harvesting the donor strip merely removes some of the extra scalp tissue while only slightly affecting density (hairs/mm 2 ); therefore, the yield will be high, as the density will not decrease significantly over subsequent procedures. With little redundancy, however, each procedure stretches the skin, measurably decreasing density. The limitations of a tight scalp are usually not apparent in the initial surgery, but in subsequent procedures, it can become much harder to perform a non-tension closure or, in the face of decreased density, to harvest a significant amount of hair. Therefore, the long-term goals of those with tight scalps must reflect a more limited donor supply.
Patients with very loose scalps, due to increased distensibility, tend to heal with widened scars and so often make poor candidates for procedures using a linear incision. Some, in fact, may have undiagnosed connective tissue disease. Follicular unit extraction should be considered in cases of both very loose and very tight scalps; however, it is important to keep in mind that although FUE is often easy in patients with average to tight scalps, it is sometimes very difficult in patients with loose scalps, as the skin is difficult to stabilize and the follicular units may shred during the extraction process.
The mid-portion of the harvestable donor zone generally lies over the occipital protuberance and extends laterally to within 3 cm of the temple hairline on either side. This distance is approximately 32–35 cm. Besides limiting the length of the incision, temple recession can signal extensive balding and portends a diminished donor supply. The height of the permanent zone can vary markedly from person to person and should be carefully measured. Hair should be harvested only where it is stable, i.e., where it lacks significant miniaturization. An often overlooked sign is the “ascending” hairline, characterized by miniaturization in the lower margin of the permanent zone at the back of the scalp. Both receding temples and an ascending posterior hairline indicate a shrinking donor zone and mandate conservative surgical planning.
Ideally, the main goals of the first transplant session should be:
To establish the frontal hairline and frame the face
To provide coverage to all bald areas of the scalp, from the frontal hairline to the vertex transition point
To create sufficient density so that the results will look natural after one session, though additional sessions may be desired.
These goals should be the ultimate aim of those performing hair restoration surgery, but may not be achievable with a small or inexperienced surgical team. In this author's opinion, there is little medical or aesthetic justification for performing the surgery in arbitrarily small sessions. It is preferable that each procedure cover the entire area of hair loss intended to be treated and be designed to “stand-alone.”
In an alternate approach to surgical planning, the objective is to achieve final density in a one-pass procedure by creating high density in a more limited area and then transplanting another area in a subsequent session. This is accomplished in part by using very small recipient sites, limiting graft size to three hairs and using the stick-and-place method, in which grafts are inserted as soon as the recipient sites are made.
As the number of grafts placed per unit area (density) rises, so too does the risk of vascular compromise that may result in suboptimal graft growth. Technical problems of popping that may cause the grafts to become desiccated or that expose the grafts to mechanical injury on reinsertion also become more likely. Proper patient selection and technical expertise help avoid such problems, but the risks are increased nevertheless. It certainly behoves those with more limited experience to be conservative when determining the number of grafts to be transplanted.
Because the blood supply to the scalp is extensively collateralized, the risk of vascular compromise is related more to the density of grafts in a specific area and the size of the recipient wounds, than the absolute number of grafts placed. For this reason, the transplantation of a large number of grafts over a broad area does not seem to pose the same problems as producing very high densities in specific areas. In addition, popping becomes less of a technical issue when the same numbers of grafts are placed over a larger area. However, transplanting a large number of grafts (in “mega-sessions”) poses its own challenges, such as increasing the time the grafts remain outside the body, requiring more staff, contributing to patient and staff fatigue, and creating organizational issues. As with dense packing, the use of very large sessions should be reserved for only the most experienced surgical teams.
Though the amount of hair needed to cover the front and top of the patient's scalp will vary, an attempt should be made to achieve this coverage, if only lightly, in the first session. Crown coverage should not be a goal of the first session unless the patient has an above-average donor supply; if it is attempted in the first session, the patient's options will be more limited and the chances for an aesthetically balanced transplant may be permanently compromised.
Table 30.2 offers general guidelines as to the number of follicular units recommended for the first hair transplant procedure.
| Norwood class | Follicular units | Total units with crown |
|---|---|---|
| IIA | 800–1400 | – |
| III | 1000–1600 | – |
| III Vertex | 1200–1600 | 1600–2200 |
| IIIA | 1400–1800 | – |
| IV | 1600–2200 | 2200–2600 |
| IVA | 1800–2400 | – |
| V | 2000–2500 | 2500–2800 |
| VA | 2200–2800 | – |
| VI | 2400–3000 | 2800–3400 |
| VII | 2500–3200 | 3000–3600 |
Transplanted hair sheds around 2–6 weeks after the procedure and the first signs of new growth occur on average in approximately 10 weeks, though the onset can vary considerably, taking as long as 4–6 months or more. Hair gradually increases in both thickness and in length, so that the initial growth is often not indicative of the final result. In less than 5% of patients, hair growth proceeds unabated after surgery, without shedding.
One should generally wait 10–12 months to best appreciate the cosmetic impact of the procedure. During this time, the continued increase in the diameter and length of the newly growing hair strikingly alters the appearance of the restoration. Once hair reaches styling length, both the patient and physician can make aesthetic judgments about the desirability of an additional treatment session.
It will also be advantageous to delay the second procedure to maximize the donor harvest. Although each procedure results in a potentially tighter scalp, some of the preoperative donor laxity returns in the months following the surgery. Although, the major change will occur during the first month as the edema and inflammation subside, further loosening occurs as the scalp stretches over the next 12 months.
In the uncommon event of telogen effluvium occurring in the donor area, the telogen follicles may not be easily identifiable in the dissection. Since recovery in the donor area may take up to a year, it is essential that patients wait until complete regrowth has taken place before a second session is performed. In rare cases, if the closure is too tight, the effluvium may eventuate in permanent hair loss.
The main goals of the second session are:
To add density to areas transplanted in the first session
To refine the hairline
To follow the progression of the hair loss (if necessary)
To extend the transplant into the crown (when appropriate)
To complement a specific grooming pattern
At 1-year follow up, approximately 50% of patients are satisfied with the density achieved in the first session. However, if the first session is planned properly (as a stand-alone procedure) it should always look natural, regardless of the desire for more fullness. This gives the person who may want further density to perform the next procedure at his or her leisure, or not at all.
The hairline can sometimes benefit from a little fine-tuning to make the leading edge softer and more irregular. Placing the hairline too low is a common mistake, but so is placing it too high, where it fails to frame the face. One should avoid transplanting a hairline with the intention of bringing it down on the second session, once the patient can see how it looks. It is better to try to get the hairline position right in the first session; lowering it later often leaves the leading edge too thin and may necessitate an additional, otherwise unnecessary procedure.
The decision regarding crown coverage is important because it is the least visible of the balding regions, but can potentially occupy a very large surface area, producing an almost inexhaustible demand upon the donor supply.
If extensive balding appears likely and the patient has a modest donor supply, the crown should be treated only by extending the transplant of the top of the scalp posteriorly, rather than by transplanting the crown as an isolated region. This will help to ensure that the patient will not be short of hair if the intervening bridge between the front and crown were to require additional grafts. Unless the patient's history, age, and physical examination indicate limited balding, it is particularly important to avoid creating significant density in the crown, as subsequent balding could leave an isolated island of hair.
A useful alternative to covering the crown with transplanted hair is to end the transplant at the vertex transition point (the curved line that delineates the area where hair changes from a predominantly forward direction into a swirl). The patient can then groom the forward-pointing hair back to conceal the non-transplanted area. This is recommended when direct crown coverage is not realistic, or it is too early in the balding process to determine whether significant crown coverage will be possible in the future. Another advantage of sparing, or lightly covering, the crown is that donor reserves may be saved to address possible further diminution of the lateral donor fringe, which would separate the transplanted hair on the top of the scalp from the sides. Connecting these two areas is generally more important cosmetically than covering the crown.
Particularly when a person has been bald for many years, it is not known how the person will want to style his or her hair after the restoration. Once the first procedure has grown in, many people will feel comfortable committing to a specific grooming pattern. If this is the case, then the second procedure may be used to complement a specific way of styling the hair. For example, if a man is relatively certain that he will continue to comb his hair from left to right, then the transplant can be left-weighted to enhance the appearance of density when the hair is groomed in this manner. If, however, the person prefers to comb his hair straight back, or wants to vary his look, then the second transplant should be symmetrical, mimicking the distribution of the first.
The surgeon should make every attempt to accomplish the restoration in as few sessions as possible, rather than putting patients through an unnecessarily protracted course of multiple surgeries that can adversely affect their donor area and their lifestyle. The number of grafts required to achieve patient satisfaction varies widely due to the great variability in hair characteristics and patient tastes. Moreover, because hair loss patterns form a continuum, the number of grafts necessary for each discrete Norwood class can vary significantly. Table 30.3 shows the approximate number of follicular unit grafts necessary for a complete restoration, with and without crown coverage.
| Norwood class | Follicular units | Total units with crown |
|---|---|---|
| IIA | 1400–2200 | |
| III | 1600–2400 | – |
| III Vertex | 1800–2600 | 2600–3200 |
| IIIA | 2000–3000 | – |
| IV | 2200–3400 | 3400–3800 |
| IVA | 2400–3600 | – |
| V | 2600–3800 | 3800–4500 |
| VA | 2800–4200 | – |
| VI | 3000–4600 | 4600–5600 |
| VII | 3200–5000 | 5000–6400 |
It is common practice for doctors to place patients on finasteride before surgery to minimize the chance of post-surgical effluvium (shedding). Although there are no scientific studies confirming that it is effective for this purpose, it would seem that if the goal is to prevent post-surgical shedding, the medication should be prescribed at least a month before the procedure. If, however, the intent is to postpone or obviate the need for surgery, then it should be taken for a minimum of 1 year to allow sufficient time for the patient's hair to regrow.
Patients using topical minoxidil are advised to discontinue its use several days before surgery (because of its vasodilator properties) and wait until a week after the procedure before resuming it (to avoid the irritating effects of the alcohol in the 2% solution or the propylene glycol in the 5% solution). Although we suggest minoxidil in combination with finasteride for patients with early hair loss, we generally do not recommend the use of minoxidil after a hair transplant, unless it is being used in an area other than that which was transplanted (such as the crown). We feel that minoxidil has little added value for the average post-transplant patient. We do, however, encourage the continued use of finasteride to help retard further balding. Those who do not plan to use minoxidil after surgery should discontinue it immediately, so that any of its beneficial effects may be reversed by the time of surgery and the true extent of a person's hair loss be more easily appreciated.
Patients are advised to avoid products that are used to thicken the hair or that stain the scalp for 3 days before the procedure, as these often take several days to completely wash out of the scalp. Their presence during surgery can decrease visibility and make placing more difficult. Hair systems should be removed before surgery and be replaced with, or converted to, a clip-on system. The front edge of the piece can be kept in place with a stiffening rod, obviating the need for tape or glue. However, any form of attachment at or near the frontal hairline risks dislodging grafts. Patients are encouraged to permanently discontinue the system after the procedure, but those who feel the need to use them until their hair grows in should wait at least 10 days postoperatively when the grafts are secure.
Systemic antibiotics are not indicated for clean surgical wounds in healthy patients, so their routine use in hair transplantation is not necessary; however, many doctors routinely use them. Because there are no specific guidelines for antibiotic prophylaxis in hair transplantation for patients with a history of endocarditis or mitral valve prolapse, the decision to use them must be based on the individual patient's risk factors.
Other preoperative instructions are relatively straightforward and will depend to some degree on the preferences of the operating surgeon. Patients should be notified well in advance of the procedure date regarding the need to discontinue certain medications, to stop smoking, and abstain from alcohol. Box 30.3 is a summary of the main preoperative instructions.
Continue medications currently prescribed by the physician, particularly those for high blood pressure. Those taking broad β-blockers (such as propranolol) should switch to selective β-blockers, as the former may interact with epinephrine. This should be done under a doctor's supervision.
Discontinue topical minoxidil and avoid products used to thicken the hair or stain the scalp 3 days before the procedure.
In order to minimize bleeding, avoid the following before surgery: aspirin or other anti-inflammatory medications (1–2 weeks), vitamin B or vitamin E (1 week), and alcoholic beverages (3 days). Do not drink coffee or any other caffeinated beverages on the day of the procedure as these substances will increase sensitivity to medications such as epinephrine.
Do not smoke tobacco products for at least 24 h before the procedure and at least 10 days after. Smoking will slow down healing and heighten the chances of wound infection and scarring.
On the morning of the procedure, take a bath or shower and wash the hair thoroughly using a surgical scrub (containing 3% chloroxylenol).
In the weeks prior to surgery, if possible, leave the hair long in the back and on the sides to cover the sutures (FUT only).
Wear clothes that do not need to be pulled on over the head; this will help keep bandages in place and avoid any damage to the grafts immediately after surgery.
Eat breakfast in the morning if the surgery is scheduled in the afternoon, have a light lunch before arrival.
Because medications given during the procedure can make you drowsy, do not drive home following the surgery. If necessary, plan to have a driver or take public transportation. Please let the doctor know ahead of time.
All patients undergoing hair transplantation should be treated with universal precautions. Although there is no consensus on the need to perform routine blood tests before the procedure, the following tests provide an additional level of safety:
Complete blood count
Metabolic panel
Hepatitis B surface antigen and antibody
Hepatitis C antibody
HIV screen.
One should obtain medical clearance for HIV-positive patients to make sure that they are immunocompetent enough to withstand a potential series of procedures. With hepatitis antigen positivity, one should inform the patient's primary physician to rule out active disease. Other tests, such as a platelet count and prothrombin and thromboplastin times, are performed only if warranted by the history and physical exam.
The surgical consent form should be given to patients to read at their leisure well in advance of the procedure and should be signed by the patient before taking any medications that can cause drowsiness or impair judgment. The exact time of signing should be indicated. The major elements of the consent form are listed in Box 30.4 .
Nature of the hair transplant procedure, with specific reference to its cosmetic aspects
Indications for surgery
Discuss the pros and cons of FUT vs FUE
Risks: reactions to anesthetics; allergic reactions; sterile folliculitis, infection; cyst formation at graft site; scarring in donor area; hair loss related to the procedure; hair texture changes; failure of transplanted hair to grow; numbness; paresthesia; temporary swelling or bruising
Benefits
Alternatives: doing nothing, change hair styles (e.g., lightening or keeping hair very short); medical therapy; another form of hair restoration surgery (e.g., mini-micrografting); wearing a hairpiece
Results are not guaranteed
Consent for photograph as part of the medical record
Caution about driving under the influence of medication
Statement that the above are understood and all questions have been answered
Signature of the patient with date and time (before the administration of drugs), countersigned by the operating physician and witnessed by a staff member
Although not universally recommended, some doctors have the patient shower the morning of surgery using a chlorhexidine surgical scrub as shampoo. Though it does not sterilize the scalp, the chlorhexidine binds to the stratum corneum, decreasing transient and pathogenic microorganisms and resident skin flora. Caution is advised as it can be toxic to the middle ear and irritating to the eyes. In our practice, we advise patients to use a simple baby shampoo. After showering, the patient should dress in comfortable clothes and wear a button-down shirt.
Follicular unit hair transplantation is typically performed in an outpatient office setting. The guidelines of care for office surgical facilities delineated by the American Academy of Dermatology should be reviewed before setting up facilities. Though major complications occur only rarely, protocols should be in place to handle emergencies such as hypersensitivity reactions or anaphylaxis, stroke, seizures, arrhythmias, acute myocardial infarction, and hypertensive crisis. Specific arrangements should be made with a local Emergency Medical Services (EMS) facility to take care of distressed patients.
The medical staff should be comfortable dealing with problems such as bleeding, syncope, petit mal episodes, and anxiety reactions. The medical staff should be certified in cardiopulmonary resuscitation (CPR), and at least some clinical staff in advanced cardiac life support (ACLS). The amount of in-office emergency equipment will depend on staff capability and training, and proximity to an EMS unit. Basic equipment includes portable oxygen, an automated defibrillator, intravenous set-up, and an oral and nasopharyngeal airway.
Because of the scalp's abundant vascular supply and relative resistance to infection, it is common practice for doctors' technique to be aseptic, rather than sterile. And because the scalp is not usually shaved and prepped, strict sterile technique is not practical. However, at least until the donor area is sutured closed, a sterile environment should be maintained. This issue is discussed in greater detail by Sebben.
The single most important instrument for FUT is the dissecting stereomicroscope, which is available with either a binocular view or an LCD screen. There should be one microscope for each member of the surgical team performing dissection. Experienced teams generally require one staff member per 500–750 grafts (for graft dissection and placing), so that a typical 2000-graft procedure would necessitate three or four staff members in addition to the physician, though this will vary considerably among practices. Less experienced teams may require more people. The staff's other office responsibilities, as well as possible absenteeism, must also be taken into account in calculating the number needed. The staffing requirements for FUE are somewhat smaller.
Regular operating room tables are generally inadequate. Rather, the tables must be contoured and provide some lumbar support when patients are sitting. They also need to be low to the ground, with the seat not more than 56 cm from the floor, so the staff can work comfortably around the head, while the patient is seated.
Equally important are comfortable working areas for the staff. Dissecting tables with a bull nose, rather than squared edge, are easier on their arms, and adjustable seating saves them from bending over to look into the microscopes ( Fig. 30.5 ). The long duration of the surgery makes meticulous attention to ergonomic issues all the more crucial. Bright fluorescent ceiling lighting is preferable to surgical operating room lights because it generates less heat. We use high-intensity surgical lights only for working on the patient's donor area, as they can be angled to illuminate the posterior scalp of the seated patient.

Petri dishes containing grafts pending placement should be kept on a stable, wall-mounted surface to keep them from being inadvertently knocked over ( Fig. 30.6 ). The typical operating room Mayo stand is not sufficiently stable. Normal saline is the most frequently used holding solution for grafts. Limmer has shown a high survival rate for grafts kept in chilled saline for up to eight hours. More exotic solutions with potential graft-sustaining properties, such as platelet-rich plasma or those containing ATP, have been developed, but they are not yet widely used.

Although it is standard practice to chill grafts in order to slow down cellular metabolism and increase their survival outside the body, there is concern that isotonic holding solutions (such as normal saline and lactated ringers) may not be ideal for this cooled environment. At temperatures used for hypothermic storage (2–8°C) the ATP-driven ion pumps that maintain osmotic balance are inactivated, allowing salt and then water influx. This can result in intracellular edema and cell death.
New holding solutions, that contain impermeant macro-molecules which mimic the intracellular environment of grafts, can prevent fluid influx at cooler temperatures. Antioxidants that decrease free radical formation and buffers that keep the pH in an optimal range can also be added to the mix in order to increase the survival of transplanted grafts.
It is preferable to have all the dissection performed in the operating room. A small cooling station for grafts should be located between every two dissectors. Performing all the dissection and storing the grafts in the same room eliminates the risk of inadvertently placing grafts in the wrong patient. This is particularly important in a busy practice where more than one person is being operated on per day. The minimum room size for a physician and five staff members to work comfortably is approximately 15.5 square meters.
In advance of the procedure, it is helpful to set up complete surgical trays, including the local anesthetic mixtures pre-drawn into syringes. This serves a number of purposes: it makes it easier to keep track of how much anesthetic is used in each part of the procedure, it helps to ensure that safe dose limits are not exceeded, and it minimizes the risk of needle-stick injury, because the preparation takes place before the operating room begins to bustle.
Local anesthesia is administered with a ring block consisting of lidocaine, bupivacaine, and epinephrine buffered with sodium bicarbonate. Lidocaine, the major component, is used for its safety and quick onset. Bupivacaine is added to increase the duration of anesthesia, but in smaller quantities to limit its potential cardiac toxicity. Epinephrine increases the anesthetic duration while decreasing its toxicity and providing some hemostasis – although its vasoconstrictive action is relatively short lived.
Sodium bicarbonate can be added to bring the acidic pH of the epinephrine-containing solution closer to 7.4, lessening its sting. This is particularly useful for injections at the hairline, where the scalp tends to be most sensitive. It is important to stress that the combined use of epinephrine and broad β-blockers (e.g., propranolol) can result in potentially life-threatening reactions.
The anesthetic solution used for a typical 2000-graft session is listed in Table 30.4 . The anesthetic is drawn into 13 5-mL syringes then fitted with 27-gauge needles. The tumescent mixture consists of three 10-mL syringes with 25-gauge needles. These quantities are pre-printed on the operative report and circled as each syringe is used. If the patient requires additional anesthesia, the medication is drawn up and the additional doses are recorded.
| Ring block | ||
| Component | Concentration | Amount in mixture |
| Lidocaine | 0.50% | ≈60% |
| Bupivacaine | 0.25% | ≈40% |
| Sodium bicarbonate a | 8.40% | 1 : 10 |
| Epinephrine | – | 1 : 200 000 |
| Volume b | Initial quantity | Boost |
| Donor area | 20 cc | 10 mL |
| Recipient area | 25 cc | 10 mL |
| Tumescent mixture for donor harvest | ||
| Component | Concentration | Amount in mixture |
| Lidocaine | 0.17% | ≈100% |
| Epinephrine | – | 1 : 600 000 |
| Volume b | Quantity | |
| Donor area | 30 cc | |
On arriving at the office, patients sign the consent form which was given to them well in advance. The surgical plan is reviewed and any last-minute questions are answered. Next, density is checked to confirm the measurement taken at the initial consultation. If the number differs or it appears that density varies in the donor area, multiple measurements are taken. Scalp laxity is also reassessed and recorded on the operative report.
Patients are given cotton surgical gowns to wear and their pictures are taken with a digital camera against a light-blue background. Next, the hairline and other important landmarks, such as the vertex transition point and crown swirl, are marked in gentian violet and shown to the patient using two mirrors. If the patient approves of the hairline design, additional pictures are taken, this time of the marked scalp, usually from the front, top and posterior views. Three-quarter and close-up photographs are taken to illustrate particular cosmetic issues. Occasionally, pictures are taken during the operation for teaching purposes. At least one photograph is taken at the end of the procedure. All photographs are kept as part of patients' permanent medical records.
Typically, for a procedure of 1500 grafts or more, patients are pre-medicated with oral diazepam 5–15 mg and intramuscular midazolam 2–4 mg about 15 min prior to surgery. Dosing will depend upon the patient's body weight, age, sex, and past sedative/analgesic use. Sedatives are not given to patients who will be driving themselves home from the procedure. Intramuscular methylprednisolone 80 mg is given to reduce postoperative swelling. Oral antibiotics are not routinely given, but are considered in patients with implanted prosthetic devices, valvular heart disease, and other medical conditions requiring prophylaxis.
In preparation for the donor harvest, patients are seated upright on the operating table. The hair in the donor area (hair in the proposed donor strip plus 0.5 cm above and below the strip to facilitate suturing or stapling) is then cut to a length of 2 mm using electric clippers. The trimmings are thoroughly vacuumed away and the hair above the strip is held back with paper tape, fully exposing the donor area. A gauze headband is placed around the patient's head just below the clipped area and sterile drapes are taped to the headband.
In the first session of FUT, in a patient with average scalp laxity, we generally harvest a donor strip that is 1.2–1.4 cm wide. In calculating the length, we use the general rule of 70–95 follicular units/cm 2 . For example, if a 2000-follicular unit graft hair transplant is planned for a non-Hispanic white male with an average density of 85 FU/cm 2 , a 1.2 cm-wide strip would need to be about 20 cm in length (plus tapered corners to allow a flat closure). People of African and Asian descent characteristically have a lower follicular unit density and a strip of this dimension will yield a lower number of follicular unit grafts.
When performing follicular unit extraction, one can generally extract about 18 FU/cm 2 , so the surgeon would need about five times the area of an FUT strip to get the equivalent number of grafts. Thus, to extract the 2000 grafts in the above example, one would need an area measuring 1.2 × 20 × 5 cm or 120 cm 2 . In FUE, the hair should be clipped to a length of 1 mm (half the length of the 2 mm needed for FUT).
A ring block is established using an anesthetic mixture of lidocaine, bupivacaine, and epinephrine (see Table 30.4 ). The anesthetic solution is injected into the subcutaneous fat layer approximately 1 cm below the lower portion of the clipped area and extending several centimeters past it on either side. In addition to buffering the anesthetic, already discussed, discomfort from the injections can be reduced by pressing a vibrating hand massager to the skin below the area of insertion of the needle. The sting of the injection can also be reduced by a device that controls the flow of the anesthetic solution.
Approximately 0.75 mL of anesthesia is used per centimeter of donor area, so that a 25 cm-long incision would require slightly less than 20 mL of anesthetic solution. It is important to avoid injecting into the muscle, as epinephrine will cause vasodilatation, due to the action on β 2 -receptors, quickly dissipating the local effects of the anesthetic and increasing its toxicity.
The ring block takes approximately 15 min to induce anesthesia. As soon as the donor-area skin becomes numb, tumescent anesthesia is administered by injecting larger quantities of a more dilute lidocaine–epinephrine solution into the mid-fat to make the area firm. The tumescence serves six purposes: (1) to widen the distance from the follicles residing in the upper fat to the nerves and larger blood vessels lying just above the fascia; (2) to increase the rigidity of the donor area; (3) to decrease follicular transection; (4) to decrease bleeding; (5) to produce more uniform anesthesia; and (6) to reduce the amount of anesthetic required.
Tumescence can be achieved using a dilute solution of epinephrine and lidocaine (see Table 30.4 ). This will provide additional anesthesia that is particularly important in repeat procedures, or for patients with significant donor scarring. In situations where there is prior surgery, direct cutaneous innervation to the donor area from the occipital branches can be blocked by scar tissue, so that innervation to the donor area arrives in a rostral–caudal direction, rendering inferiorly placed ring block anesthesia alone ineffective. At times, when there is an excessive amount of donor scarring, the anesthetic mixture must be injected above or directly into the scarred area to make it numb.
The ideal position for the donor incision is in the mid-portion of the permanent zone. This generally lies at the level of the external occipital protuberance (at the midline). The donor strip can be excised using two parallel blades set 1.0–1.5 cm apart or the strip can be harvested using a single blade. When using the parallel blade technique, a convenient harvesting device is the Rassman handle that is loaded with two no.10 blades. The handle holds the blades at an angle of 30°, making them parallel to the emergent hair. The handle should hold the blades in a pre-angled position to allow both blades to lie flush with the skin surface when aligned with the hair follicles; otherwise, the surgeon may cut too superficially with the upper blade and too deep into the scalp with the lower ( Fig. 30.7 ). Once the main parallel portion of the incision is complete, a single scalpel blade is used to taper the ends into an ellipse and to dissect the base of the strip in mid-fat, just below the level of the follicles. In general, the length of each tapered end should measure at least 1.5 times the width of the strip, so that the ends lie flat ( Fig. 30.8 ).


Alternatively, the skin can be marked and the entire excision can be made with a long free-hand ellipse. This has the advantage of allowing the angle of the blade to be adjusted to the angle of the follicles as each edge is cut. However, this technique makes it harder to keep the width uniform, which is necessary for predictable graft yields. In addition, the first incision causes the strip to lose its rigidity, making the cutting the second edge more difficult
Regardless of the harvesting method, once the strip is removed it is immediately placed into a holding solution.
The most common types of closures include metal staples, a running non-absorbable suture, or a running absorbable suture. If staples are used to close the wound edges, it is important to be certain that the wound edges are flush before the staples are applied. The edges can be approximated by grasping the lower edge with a skin hook and using rat-toothed forceps to hold and slightly evert the upper edge (this requires the help of an assistant) ( Fig. 30.9 ). The staples should then be placed approximately 0.6 cm apart. Staples have very little tissue reactivity, but they make flush apposition of wound edges a little more difficult and can be uncomfortable in the postoperative period. In the author's practice, we routinely remove alternating staples at 10 days and the remainder at 18–25 days postoperatively, depending on the degree of tension, the patient's age and the amount of anticipated activity. We feel that leaving in staples for this longer period of time leads to a finer donor scar, particularly in younger or active patients and in those with tighter than average closures.

Non-absorbable sutures, of either nylon or polypropylene, are usually placed using a single running stitch and are removed in 10–14 days. A problem is that if they are placed too far from the wound edge, they entrap hair follicles and this may result in the destruction of donor hair if there is significant postoperative edema. If placed too close to the wound edge, they can become buried and difficult to remove. These two problems are avoided with the use of staples and probably speak to why staples are used by so many hair transplant surgeons in spite of the preference that patients have for the more comfortable sutured closure.
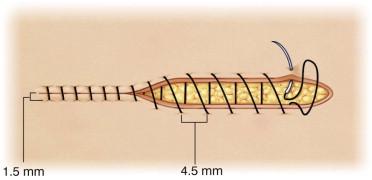
Absorbable sutures should be placed close to the wound edge ( Fig. 30.10 ). This will tend to minimize the amount of suture material used, decrease the entrapment of follicles and avoid strangulation if there is significant postoperative edema. To further limit damage to follicles, the sutures should be placed approximately 4.5 mm apart and the suture should be advanced on the surface, rather than under the skin, as this will minimize the amount of suture in contact with the follicles ( Fig. 30.11 ). With this technique, the needle should be passed through the full thickness of the dermis and exit the wound edge, just below the level of the bulbs, without incorporating any significant amount of subcutaneous tissue. The needle track must be kept parallel to, and within, 1.5 mm of the wound edge. Particular attention should be paid to placing the needle parallel to the upper wound edge where the angle is very acute. Although hypoallergenic, in our experience, poliglecaprone can cause allergic reactions in some patients. Basic guidelines for using poliglecaprone 25 sutures can be found in Box 30.5 .

Plan width of donor strip so that there is little or no tension on closure.
Use tumescent anesthesia to harvest donor strip in mid-fat.
Use sutures no heavier than 5–0.
Use a simple running stitch, advance each loop on the skin surface.
Keep needle parallel to and within 1.5 mm of wound edge.
Incorporate epidermis and dermis only.
Use 4.5 mm spacing between loops.
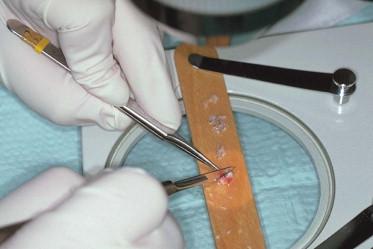
Once the donor strip is removed, it is immediately placed into the holding solution and passed to the surgical team leader stationed at a stereomicroscope ( Fig. 30.12 ). The strip dimensions are measured and recorded. The next step is performed under strict stereomicroscopic control in a process called “slivering.”

In one method of slivering, the donor strip is placed on its side, on a wooden tongue-depressor blade, soaked in Ringer's, with the hair pointing away from the dissector and the convex surface of the strip facing upward. For a right-handed person performing dissection, the left end of the strip is held with rat-toothed forceps in the dissector's left hand. An assistant applies tension to the strip, holding it a few centimeters away from the area being cut with rat-toothed forceps held in the right hand. Using a Persona no.10 blade on a no.3 blade handle held in the right hand, the dissector begins to cut the strip into 2–2.5 mm-wide sections, by guiding the blade between follicular units using a one-directional fillet-like movement from the epidermal side to the subcutaneous surface. A back-and-forth sawing motion should be avoided, as it will increase the risk of transection ( Figs 30.13 , 30.14 ). The pieces generated are then distributed to the other members of the surgical team who complete the dissection. In the last step, the individual pieces are placed on their sides, stabilized with straight jeweler's forceps, and then dissected under the stereomicroscope with a scalpel into individual follicular units of one to four hairs each ( Figs 30.15 , 30.16 ).



Next, the units are sorted according to the number of hairs they contain and placed into Petri dishes with 4-quadrant dividers to hold separate the different size follicular units. The Petri dishes containing holding solution are placed on a cooling unit to keep the solution at a specified temperature ( Fig. 30.17 ). The temperature is monitored with a digital sensing device.

An alternate slivering method involves dissecting the donor strip into slivers as wide as one follicular unit, approximately 1 mm. The units are then isolated from the very thin strip. The key to either method is that every step is performed under stereomicroscopic control, which keeps the units intact and avoids follicular transection. It is also vital that all the pieces of the strip remain in chilled Ringer's lactate, except when they are being cut. While under the microscope they should be kept well hydrated using 10-mL syringes containing Ringer's lactate that is kept at each cutting station.
Follicular unit extraction (FUE) is a conceptually simple procedure, where individual follicular units are harvested through small circular incisions created by a trephine or similar round instrument. In FUE, the punch cuts down through the reticular dermis and the follicular unit is pulled (extracted) from the scalp. The advantage of this procedure is that it obviates the need for a linear incision. Difficulties lie in the increased risk of follicular transection compared to strip harvesting, the inability to harvest all the hair from the mid-portion of the donor area, and the intrinsic variability of each patient with respect to the ease of extraction. There are also the organizational challenges of not being able to have multiple persons working in parallel (as can be done with the microscopic dissection of a harvested strip) and the inability to easily harvest and place grafts at the same time. Both of these constraints serve to increase the length of the FUE procedure.
The main indication for FUE is for patients who want to wear their hair so short that the linear donor scar of FUT may become visible. FUE is also useful in patients who are at risk of having a widened donor scar. This includes very athletic patients, particularly those engaged in contact sports, bodybuilders, and younger patients in general. Other indications include patients with very tight scalps (in whom a strip excision is not practical) and those with a history of healing poorly, i.e., those that heal with stretched or hypertrophic scars, or with keloids. Some patients simply prefer not to have a linear donor scar.
An important application of FUE is to camouflage a widened linear donor scar from prior hair transplant procedures. As stated earlier in this chapter, it is unfortunate that patients with very loose scalps are at risk of healing with widened scars but may also be poor candidates for FUE due to a difficulty in adequately stabilizing the scalp.
FUE's main limitation is that it is less efficient in harvesting hair than FUT performed with strip harvesting. In FUT, all the hair from the optimal (central) part of the donor region can be removed and transplanted, and the resulting defect is sewn closed. In contrast, the FUE defects remain open to heal by second intention with significant amounts of intervening hair left behind and, therefore, a much larger region of the scalp must be accessed to harvest the necessary amount of donor hair. In a single procedure, to obtain the equivalent number of grafts, FUE requires approximately five times the area needed when using a strip. In FUE, the greater area required significantly increases the risk of harvesting hair from non-permanent areas of the scalp or from areas where the hair is of poorer quality. Figure 30.18 shows the donor area immediately after the extraction of 1891 follicular unit grafts and the same area 1 and 2 weeks postoperatively.

As mentioned, transection during the harvest is greater in FUE than with stereomicroscopically controlled FUT. This is due to the inability of the instruments used in FUE to fully account for the variable angles and curved path of the individual follicles that comprise each follicular unit as they pass deeper in the skin. With FUE, the second intention healing causes microscopic fibrotic changes in the donor area, distorting adjacent follicular units and making subsequent sessions more difficult. Taken together, these factors limit the total number of intact follicles that can be harvested through FUE, rendering it a less robust procedure than FUT. In a procedure where a finite donor supply is the main constraint, the inefficient use of donor tissue poses a significant problem. Table 30.5 summarizes the pros and cons of FUE.
| Pros | Cons |
|---|---|
|
|
The ability to perform FUE with minimal transection varies significantly among patients and in different regions of the scalp. Because of this, a test measuring the ease of extraction (the FOX Test) should be performed prior to recommending the procedure in patients where extraction is likely to be difficult. Patients undergoing FUT can easily be tested for FUE at the time of surgery in case the latter procedure is considered at a future date.
A significant advance in the technique of FUE is to first score the top of the follicular unit with a sharp punch and then use a blunt instrument to separate the follicular unit from the surrounding tissue, thereby minimizing follicular transection. The main limitations of this technique are the increased incidence of buried grafts and increased surgical time in an already very laborious process. Robotic FUE, based on this two-step concept, addresses the limitations of conventional techniques.
Follicular unit extraction consists of two main steps: (1) separation of the follicular units from the surrounding skin, and (2) extraction (removal) of the follicular units from the scalp. Step one is a highly repetitive and labor-intensive process that requires great precision. This step requires the centering of the punch over a follicular unit and the alignment of the dissecting instrument parallel to the follicles. Since this process must be repeated hundreds to thousands of times in a typical FUE hair transplant, it is subject to significant human variability and error.
A major advance in follicular unit extraction is the use of a robotically controlled extraction device that automates this crucial first step of FUE. The robotic system increases the accuracy of graft harvesting, which in turn minimizes damage to hair follicles, potentially increasing graft survival.
The current robotic technology is based on the two-step method of extraction, namely, it uses a sharp punch to penetrate the skin and a dull rotating punch to separate the deeper part of the follicular unit from the surrounding tissue. The main improvement is a very precise, image-guided robotic arm that operates a dual-needle punch mechanism in order to increase the accuracy of extraction ( Fig. 30.19 ).

Compared with manual systems, the robot is more versatile in its ability to harvest grafts from patients with different hair characteristics, patients from various ethnic backgrounds, and hair from different parts of the scalp. It is particularly useful in extracting grafts from the sides of the scalp, where the hair lies flatter on the skin.
Introduction of the robotic system into a physician's practice can present a formidable challenge. Besides the expense of the technology, the robot requires an operating room larger than those that exist in many doctors' offices and requires that the room be dedicated to this purpose. In addition to special training required to operate the system, the FUE procedure itself should be modified, so that grafts are kept out of the body for as short a time as possible and kept in an environment that will ensure maximum growth. This can be accomplished by making recipient sites prior to the robotic harvesting and by using special biologic solutions to hold the grafts.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here