Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The esophagus, stomach, and duodenum are studied. The radiologist evaluates the morphology and motility of these organs.
The radiologist evaluates the motility of the oral cavity, pharynx, and esophagus, and the morphology of the pharynx, esophagus, and gastric cardia. The radiologist records the fluoroscopic images of oral, pharyngeal, and esophageal motility directly into the picture archiving and communication system (PACS), into a proprietary computer system, onto a videocassette recorder (VCR), via a digital video disc (DVD) recorder, or on film (“cine”). Film has been almost completely replaced as the recording medium for motility because of increased radiation exposure, cost, and difficulty of film processing. The term “cine-esophagram” is outdated.
Figure 24-1 shows a normal lower thoracic esophagus. The esophagus is a muscular tube within the mediastinum. The esophagus is usually collapsed unless distended by liquid or solid food; swallowed air; or, in this image, swallowed air and barium. In this patient, swallowed high-density barium coats the mucosa. The swallowed carbon dioxide (effervescent agent) and swallowed air distend the lumen of the esophagus. The mucosa of the esophageal tube seen in profile appears as a white line (arrows). The mucosal surface of the normal esophagus seen en face is smooth and varies from white to gray (representative mucosa identified by S ). Normal structures in the mediastinum push on the distended esophagus, manifested as alterations of the normal straight tubular contour of the esophagus. These indentations are identified as the bottom of the aortic arch ( a ), the left mainstem bronchus ( b ), and the left atrium ( l ).

For the answer, see the figure legend.
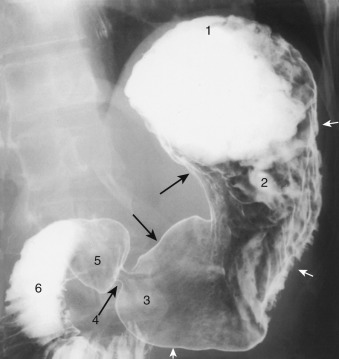
Barium sulfate absorbs and scatters x-rays, but air does not. X-rays passing through barium are blocked and do not reach the x-ray detector. X-rays easily pass through gastrointestinal (GI) structures filled with air and reach the x-ray detector. The relatively exposed areas of the x-ray detector appear as shades of black; the relatively unexposed areas of the x-ray detector appear as shades of white. The heavy barium falls to the lowest or most “dependent” portion of the stomach. This image was obtained with the patient recumbent, with the back against the fluoroscopic tabletop (i.e., a supine radiograph). The gastric fundus is posterior to the gastric antrum; barium falls into the gastric fundus when the patient lies in a supine position. Because barium absorbs more x-rays than air, the gastric fundus appears “white.” In this radiograph, the anteriorly located gastric antrum is filled with air and is also “etched in white” by a thin layer of barium. Most of the x-rays, but not all, pass through the antrum, partially exposing the x-ray detector. The gastric antrum appears gray, not black as a purely air-filled structure would appear.
Today, most radiographs are not obtained using real film as the recording medium but instead use some type of image capture device. The relative exposures on the image capture device are digitized and are assigned gray-scale values, from white to black. The images are displayed on a monitor or flat panel. Depending on the radiologist, large exposures are assigned either “white” or “black” values. In the United States, barium is usually assigned a “white” value, air a “black value”; in Japan, barium often is assigned a “black” value and air a “white” value.
This is a semiannular carcinoma of the esophagus. The tumor originated on the side of contour irregularity and has begun to spread circumferentially. The wall opposite the tumor is smooth and uninvolved by the tumor but has been pulled inward by the desmoplastic tumor. The barium pool in Figure 24-3, A , shows the contour of a luminal organ but obscures mucosal detail. The air contrast image in Figure 24-3, B , reveals the luminal contour in profile, as does the barium pool. The air contrast image also reveals the mucosal surface en face. In this case, the air contrast image shows the surface and the edge of the semiannular cancer.
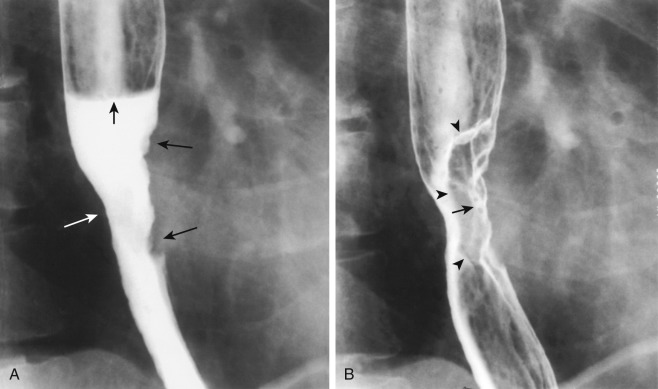
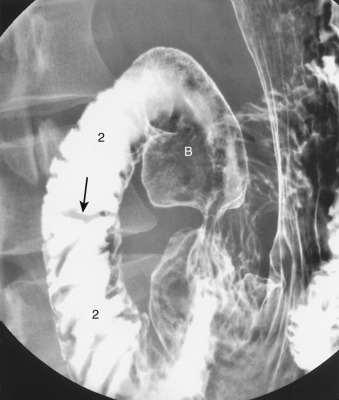
A single-contrast study of a GI structure means that one contrast agent is used, such as a suspension of barium sulfate, an ionic water-soluble contrast agent such as diatrizoate meglumine (Gastroview/Gastrografin), or a nonionic water-soluble contrast agent such as iohexol (Omnipaque). Figure 24-4 is an example of a single-contrast image obtained with the patient swallowing barium while lying in a prone position. A column of “thin” barium fills the distal esophageal lumen. The radiologist examines the luminal contour in profile for abnormalities that either protrude into the lumen or protrude outside of the expected luminal contour of the organ. The radiologist also looks for abnormalities en face. Large protrusions into the lumen displace the barium column, allow x-rays to pass through the esophagus, and appear as radiolucent “filling defects” in the barium column. Large protrusions outside the luminal contour fill with barium and, when seen en face, appear as a “double density” of barium.

In this patient, there is a small hiatal hernia ( h ). At the esophagogastric junction, a thin, smooth, symmetric ringlike narrowing, 3 mm in height, is seen in profile as a shelflike indentation of the luminal contour ( white arrows ). En face, the ring is manifested as a thin radiolucent filling defect in the barium column ( black arrow ). This is a Schatzki ring, a narrowing that commonly causes dysphagia with solids.
In a double-contrast study, the radiologist uses two contrast agents to examine the organs in question. A double-contrast upper GI series uses an effervescent agent that creates carbon dioxide to distend the luminal organs and high-density barium to “scrub and paint” the mucosa. This study is also known as an air contrast upper GI series or a biphasic upper GI series . Figure 24-5 is a double-contrast image of the distal stomach. Rugal folds are seen as radiolucent filling defects in the barium pool (white arrow) and as parallel barium etched lines ( black arrows ). Rugal folds are composed of mucosa and submucosa and are most prominent along the greater curvature of the stomach. The normal gastric antrum ( A ) has few, if any, rugal folds in most patients.

Clinical indications for performing an upper GI study include heartburn, dysphagia, or odynophagia referred to a substernal location; upper abdominal pain or discomfort; upper GI bleeding; and vomiting.
Clinical indications for performing a video/DVD pharyngoesophagogram include dysphagia or odynophagia referred to the head, neck, and suprasternal regions; history of globus sensation; chronic cough; aspiration pneumonia or cerebrovascular accident; dribbling from the mouth; abnormal tongue motions; and history of surgery or radiation of the tongue, palate, pharynx, or larynx.
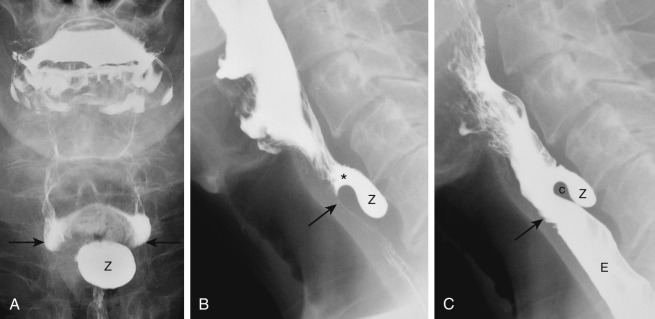
Figure 24-6 shows incomplete opening of the cricopharyngeal muscle, depicted as a smooth, hemispheric radiolucent extrinsic impression on the posterior wall of the pharyngoesophageal segment.

A globus sensation is usually related to delayed opening, incomplete opening, or early closure of the cricopharyngeal muscle. Abnormal cricopharyngeal opening is usually a vagal-mediated reflex response to gastroesophageal reflux. When a patient refluxes, the normally tonically contracted upper esophageal sphincter (comprised mainly of the cricopharyngeal muscle) remains tight to prevent reflux of esophageal contents into the pharynx and hence to prevent aspiration.
This is an example of the interrelationship of esophageal and pharyngeal function. Abnormalities in the esophagus often result in symptoms in the neck. For example, when food is stuck in the distal esophagus, the patient often complains of food being stuck in the throat. This is also an example of why a pharyngoesophagram on an outpatient should include images of the oral, pharyngeal, and esophageal phases of swallowing. This is also an example of why, if an upper GI series is ordered for gastroesophageal reflux rather than a pharyngoesophagram, the radiologist should look for complications of gastroesophageal reflux in the pharynx, especially abnormal epiglottic tilt with resulting laryngeal penetration and abnormal cricopharyngeal opening.
Figure 24-7 shows a Zenker's diverticulum. Zenker's diverticulum is an acquired herniation of mucosa and tunica propria through Killian's dehiscence, an area of congenital weakness between the thyropharyngeal muscles and the cricopharyngeal muscle on the posterior wall of the pharyngoesophageal segment. Although the pathogenesis is uncertain, there is a strong association between the development of a Zenker's diverticulum and the presence of a hiatal hernia and gastroesophageal reflux disease. It is postulated that the presence of gastroesophageal reflux leads to incomplete opening of the cricopharyngeal muscle, such that a pulsion-type diverticulum (the Zenker's diverticulum) forms in the area of muscle weakness above the cricopharyngeal muscle. Zenker's diverticulum is another example of the interrelationship between the esophagus and the pharynx and the reason that the radiologist should evaluate both regions given the appropriate clinical history and fluoroscopic findings.
Each hospital or outpatient facility has its own preparation routines for these studies. These preparations should be available from the radiologists in hard copy form or in an institutional document online. At our institution, a handout describing the examination and explaining the preparation (see the following) is available to all referring physicians:
Patients should have nothing by mouth after 9 PM.
Insulin-dependent diabetics should eliminate or decrease the dose of insulin the morning of the examination.
Patients should not take antacids or bismuth subsalicylate (Pepto-Bismol) on the morning of the examination.
Patients should wear dentures or other swallowing appliances.
If patients have solid food dysphagia, they should bring a type of food that causes dysphagia.
After the examination, patients are encouraged to drink liquids and may take a laxative if additional radiologic tests are scheduled or if there is a history of colonic hypomotility.
Contraindications include:
Known or suspected gastrointestinal tract perforation.
Inability to swallow.
In the case of inability to swallow, an examination of the stomach and small bowel may be performed by sending the patient to fluoroscopy with a nasogastric tube placed in the stomach.
In patients with known or suspected perforations of the pharynx, esophagus, or duodenum, an ionic water-soluble contrast agent such as diatrizoate meglumine (Gastroview or Gastrografin) should be used initially. This type of agent is readily absorbed from the soft tissues of the neck, mediastinum, and peritoneal cavity. This type of agent, if aspirated, has the theoretical potential to cause pulmonary edema because it is hyperosmolar and draws fluid into the lungs. If aspiration is a likely possibility, the radiologist may start with a nonionic water-soluble contrast agent that is either only mildly hyperosmolar (iohexol [Omnipaque for Oral Use]) or iso-osmolar. Other radiologists start with barium if a perforation of the pharynx or esophagus is suspected, and there is a high risk of aspiration because barium in the soft tissues of the neck or mediastinum is relatively harmless. Barium entering the peritoneal cavity from a gastric or duodenal perforation can potentially cause mild barium peritonitis. This situation is not as serious, however, as barium entering the peritoneal space from a colonic perforation. The combination of barium and feces entering the peritoneal space during a barium enema has a much greater likelihood of causing peritonitis and has a high mortality rate.
Double-contrast examinations focus on showing mucosal detail. Single-contrast examinations focus only on the big picture to detect obstruction, perforation, abnormal motility, or fistulas. A single-contrast examination is performed to detect a complication along a staple/suture line, at an anastomosis, or near a wound; to evaluate an organ as it passes through a surgically created tunnel; or to identify a rent in a mesentery. A single-contrast examination may also be performed to evaluate emptying of surgically created pouches after surgery for morbid obesity and in conjunction with a small bowel follow-through examination.
For the answer, see the figure legend.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here