Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The glymphatic system is a network of perivascular pathways that supports the exchange of subarachnoid CSF and brain interstitial fluid. Cisternal CSF is carried in the perivascular arterial spaces into the brain and then into the extracellular space. The fluid in the extracellular space distributes molecules from the CSF to brain tissue and takes up waste from cell metabolism. Extracellular solutes exchange into the CSF via perivascular pathways, from which they are cleared to the systemic circulation and along the cervical lymphatic drainage.
This system controls the delivery of nutrients to the brain via the CSF and the removal of interstitial waste products from the brain. Abnormalities in the system are found in many important neurologic conditions including head trauma, subarachnoid hemorrhage (SAH), stroke, and neurodegenerative diseases that are associated with protein accumulation and slowed flow.
The astroglial water channel aquaporin 4 supports the movement of fluid and solutes along these perivascular spaces. Pathologic conditions that alter the perivascular localization of aquaporin 4 also impair glymphatic exchange.
Changes in the size of the extracellular spaces are seen in normal sleep and in many pathologic states including hydrocephalus, brain tumors, SAH, and cerebral trauma.
The distribution of solutes in the CSF and the brain interstitial fluid is governed both by diffusion (fluid flow down a concentration gradient) and convection (fluid flow propelled by a hydrostatic or osmotic pressure gradient). The relative contribution of these processes to the distribution and clearance of different solutes depends on solute size, chemistry, anatomic location, and the physiologic and pathophysiologic state of the brain tissue.
The brain and spinal cord are composed of distinct fluid compartments, including the blood, cerebrospinal fluid (CSF), extracellular fluid, and intracellular compartments (see Chapter 42, Chapter 69 ). To support the demanding function of neural cells, the movement of fluid among these compartments is tightly controlled by the blood-brain barrier (BBB) (see Chapter 68 ). Neurosurgical conditions such as hydrocephalus (see Chapter 41, Chapter 42, Chapter 43, Chapter 44, Chapter 45 and 223–230) and vasogenic cerebral edema (see Chapter 70 ) are clearly related to abnormalities in fluid movement among these compartments, and their treatment generally centers on restoration of physiologic fluid dynamics, either by correcting pathologic causes of altered fluid movement, reducing fluid production, creating alternative fluid pathways, or using pharmacologic agents to promote osmotic fluid reabsorption. Recent research suggests that the CSF and the extracellular fluid of the brain exchange contents more extensively than previously appreciated and that this process is a critical element of normal brain function. In this chapter, the anatomic and functional communication between CSF and extracellular fluid will be presented along with the implications that this emerging research has for understanding a diverse group of neurologic conditions. Finally, a section will be presented outlining the implications of these insights on the delivery of medicines into the CSF or the brain parenchyma.
Peripherally, interstitial fluid (ISF) is formed as an ultrafiltrate from vascular capillaries and serves as a sink for cellular metabolic waste products. ISF and waste are cleared by reabsorption into the venous circulation and drainage along lymphatic vessels. Because the brain and spinal cord lack lymphatic vessels while the BBB restricts the free movement of solutes to the blood, , the clearance of ISF and waste products from the brain must be accomplished by an alternative mechanism.
In contrast with the brain parenchyma, the meninges have lymphatic channels, some of which drain into the cervical lymph nodes. These pathways are one of several routes of CSF efflux from the subarachnoid space, others being arachnoid granulations and the sleeves of exiting cranial and spinal nerve roots. In rodents, lymphatic vessels are observed both over the dorsal surface of the brain associated with the superior sagittal and transverse sinuses as well as within the skull base. These populations of lymphatic vessels are anatomically distinct, with dorsal sinus-associated lymphatics contributing to immune cell exit from the brain and CSF and with lymphatic vessels in the skull base supporting the majority of CSF solute efflux. The function of meningeal lymphatic vessels is inferred from studies in which they are blocked or ablated, after which meningeal T-cell numbers increase and amyloid plaque deposition increases. , Although meningeal lymphatic vessels have been observed both histopathologically and radiographically in human subjects, , their contributions to CSF and interstitial solute efflux and CNS immune surveillance in the human brain remain largely undefined.
In principal, ISF and solutes move through the brain through two different processes: diffusion and bulk flow (convection) ( Fig. 71.1A–B ). Diffusion is movement of particles down a concentration gradient that occurs because of random thermal motion and is influenced by the size of the molecule, the geometry of the extracellular space, and the chemical interactions among the particles and their surroundings (see Fig. 71.1C–D ). Bulk flow is the movement of fluid under the influence of hydrostatic or osmotic pressure. Associated solutes are carried along largely at the rate of the fluid and independent of molecular size, like boats of different sizes drifting together in the current of a river. This principle is limited, naturally, in the case of molecules and particles whose size approaches the dimensions of the extracellular space itself.
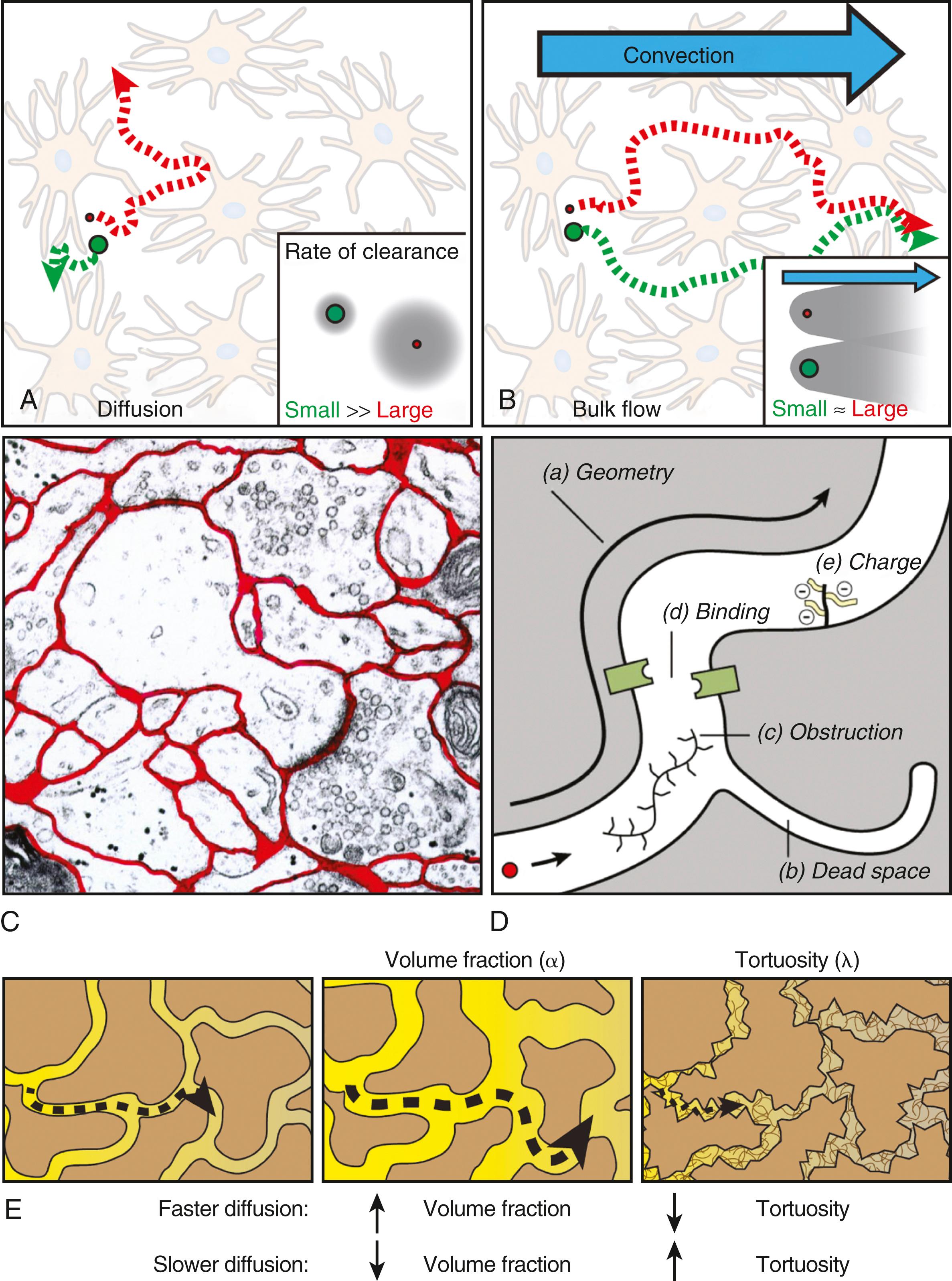
Solutes are cleared from the brain interstitium by three principle routes. Nonpolar solvents are cleared to the blood by diffusing directly across the BBB, whereas for many polar molecules, specific BBB transporters facilitate clearance across the BBB. Because diffusion is highly efficient within cellular dimensions (the tens of microns that separate neurons and astrocytes from the nearest BBB surface), the efflux of such solutes across the BBB is dependent primarily on diffusion and is constrained by the factors that influence diffusion. Solutes that do not cross the BBB are cleared from the brain interstitium to the CSF of the ventricular, subarachnoid, and cisternal spaces. , However, within the anatomic dimensions of the wider brain (the millimeters and centimeters that may separate a volume of brain interstitium from the nearest CSF space), the efficiency of diffusion drops off precipitously, particularly for macromolecules such as peptides and proteins, and cannot account for the rapid clearance from the brain interstitium. Rather, these interstitial solutes are proposed to be cleared from the brain by the bulk flow of interstitial fluid to the CSF compartments.
The extracellular space makes up 15% to 20% of the total brain volume. It is a tortuous space filled with the complex gel of the extracellular matrix and composed of dead ends and branching connections (see Fig. 71.1C ). Thus diffusion in the brain extracellular space is an order of magnitude slower than in free solution. The characteristics of the extracellular space that influence diffusion can be quantified experimentally, resulting in two commonly used parameters: the extracellular volume fraction (volume of extracellular space divided by total tissue volume) and the extracellular tortuosity (a composite parameter that encompasses the shape of the space, the presence of cul-de-sacs, and the characteristics of the matrix itself). Reductions in extracellular volume fraction and increases in tortuosity both decrease the rate of diffusion, whereas changes in the opposite direction increase the rate of diffusion (see Fig. 71.1E ).
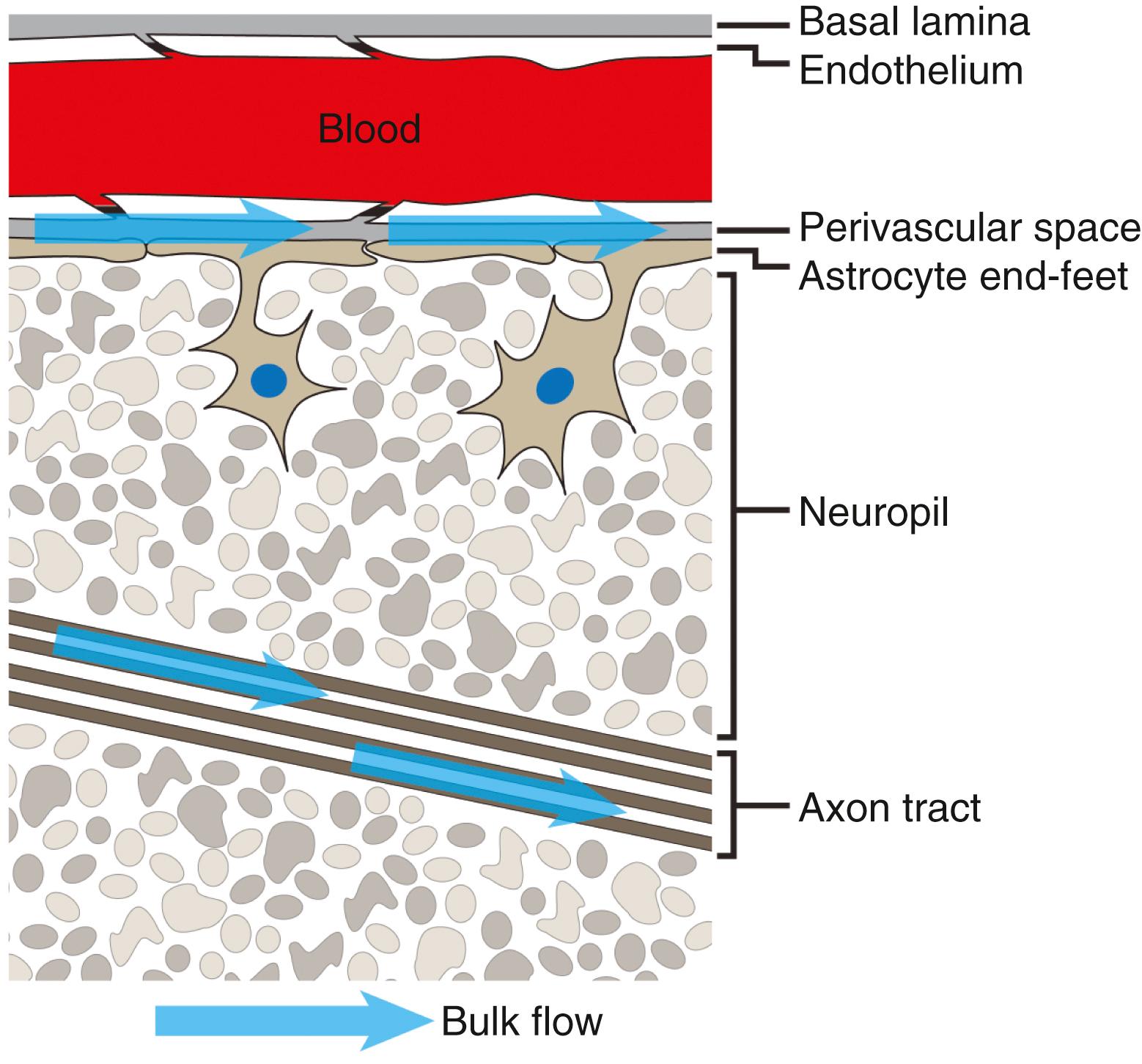
These parameters represent global measurements of the brain extracellular space and their influence on diffusion. However, the local architecture of brain tissue can have profound effects on both diffusion and bulk flow. Two clear examples of this are white matter tracts and perivascular spaces within the brain parenchyma ( Fig. 71.2 ). Because axon bundles within a white matter tract tend to orient along a single axis, diffusion within the white matter extracellular spaces exhibits anisotropy, the tendency to move more freely along one axis than along orthogonal axes. Similar effects on bulk flow are observed: bulk flow along white matter tracts is more rapid than through gray matter. Bulk flow through the extracellular spaces surrounding large intraparenchymal blood vessels (perivascular spaces) is also more rapid than through the bulk extracellular space. , These local architectural features exert important influences on the movement of ISF and solutes through different brain regions and the brain as a whole by providing an interconnected low-resistance pathway for the distribution of solutes through and efflux of solutes from the wider brain interstitium.
While tracer efflux studies in rodents demonstrate that the clearance of interstitial macromolecules is dependent on bulk flow, it is unclear whether bulk flow is present throughout the brain interstitium or it is restricted to permissive pathways such as perivascular spaces or white matter tracks. Recent modeling studies suggest that the hydraulic resistance of the extracellular space and capillary basal lamina may be too high to support rapid distributed bulk flow. , However, for large molecules such as peptides and proteins, even very slow rates of bulk flow would play an important role in clearance from the extracellular space. Thus the relative contributions of diffusion and bulk flow along permissive anatomic routes versus the wider interstitium remain to be conclusively defined.
Bulk flow differs from diffusion in that it requires a hydrostatic or osmotic force to drive the movement of extracellular fluid and associated solutes down the respective pressure gradients. In the periphery, extremely small hydrostatic pressure gradients between the interstitial space and the primary lymphatics are sufficient to maintain bulk flow of interstitial fluid and solute clearance. Within the brain, the sources of hydrostatic or osmotic forces that drive interstitial bulk flow are unclear. A small amount of water is produced by cellular metabolism in the brain, whereas water filtration across the relatively impermeable but vast capillary surface area may account for a substantial fraction of brain ISF production and may provide one of the driving forces for interstitial bulk flow. ,
With each cardiac cycle, pressure waves propagate along the cerebrovascular tree and drive bulk flow along perivascular spaces surrounding large intraparenchymal vessels within the brain. , , This may be a result of the action of the cerebral arterial wall on the surrounding fluid as the pulse wave passes. The movement of the systolic and diastolic elements of the pulse waves through the complex cerebral vasculature and system of sinuses may generate hydrostatic pressure gradients between the different CSF compartments that could drive interstitial bulk flow. Phase-contrast MRI shows that with each cardiac cycle, a prominent pressure gradient originates within the cisterna magna and then propagates to the prepontine, interpeduncular, and suprasellar cisterns. Propagation diminishes within the sylvian cistern and along the cerebral convexity but is maintained along the middle cerebral artery. In contrast with pressure gradients associated with each cardiac cycle, standing posterior CSF flows were observed in the ambient and quadrigeminal cisterns as well as crural cisterns, whereas standing superior-posterior CSF flow was observed in the pericallosal cistern. In principle, the interactions between transient and standing hydrostatic pressures within these CSF compartments may determine the magnitude and direction of interstitial bulk flow throughout the brain. However, the important subject of the interrelationship between pressure dynamics and fluid flow in different brain regions remains to be explored.
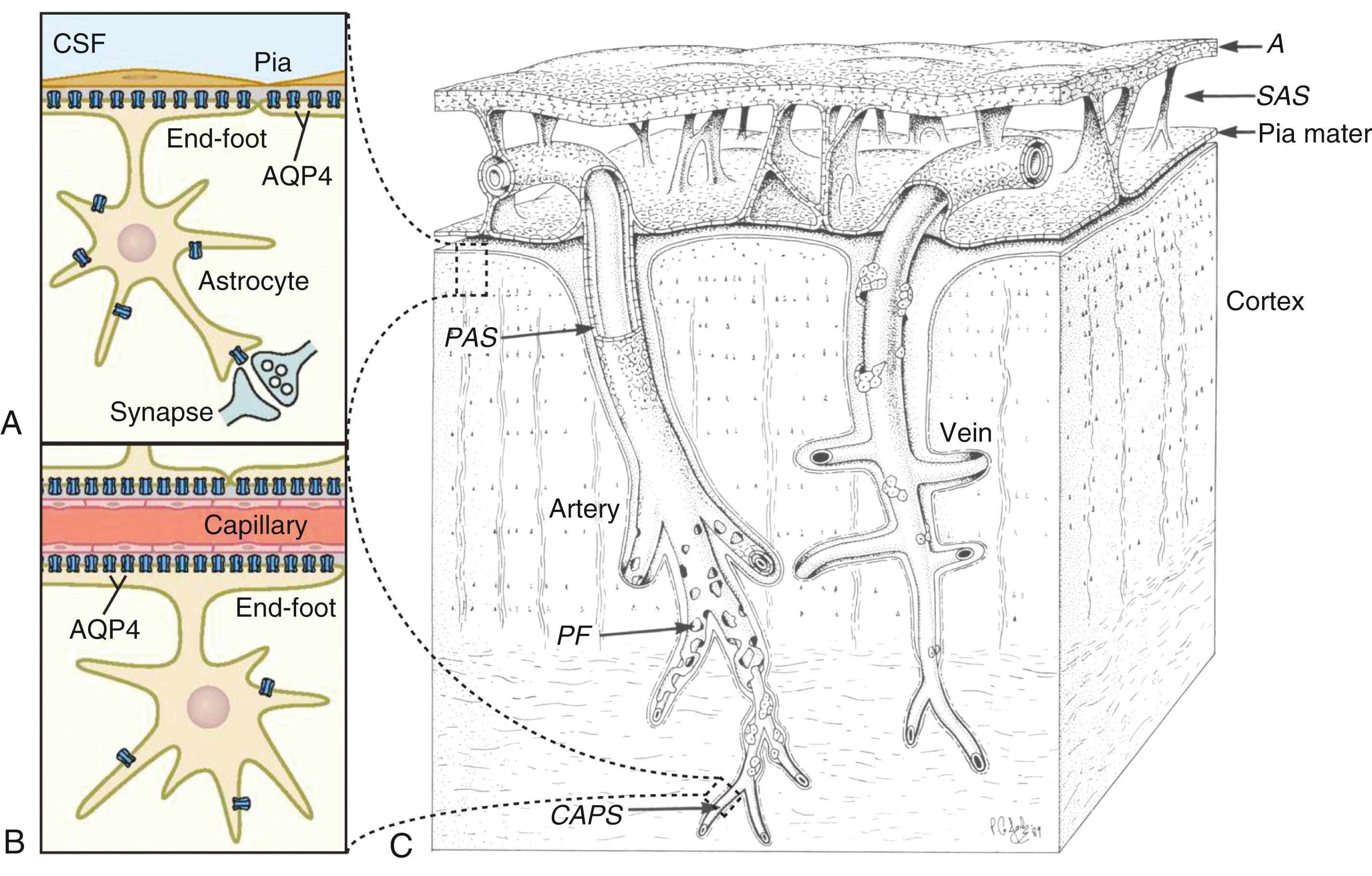
In addition to the dimensions and characteristics of the extracellular space, the presence of intracellular and intercellular pathways for fluid and solute movement are important determinants of fluid movement through the brain. Astrocytes extend processes that surround millions of synapses within a 100- to 200-μm span and are coupled by gap junctions, potentially permitting the free movement of water and solutes throughout the entire network. Astrocytes surround the entire cerebral microcirculation with perivascular end-foot processes and form the glia limitans that bounds the subpial space and the Virchow-Robin spaces associated with penetrating cerebral blood vessels ( Fig. 71.3 ). Thus astrocytes form the interface between the subarachnoid CSF compartments, perivascular spaces, blood vessels, and the wider brain interstitium. At end-feet that surround cerebral blood vessels and at the glia limitans, astrocytes express massive amounts of the water channel aquaporin 4 (AQP4) (see Fig. 71.3A–B ). AQP4 is also expressed by ependymyal cells lining the cerebral ventricles. The presence of this water channel at the BBB and the brain-CSF barrier provides a low-resistance pathway to facilitate fluid movement between the CSF, perivascular spaces, and the wider brain interstitium.
Although this chapter will briefly discuss aspects of CSF physiology relevant to ISF flow and solute clearance, the physiologic basis for CSF secretion is presented in detail in Chapter 62 . In the classical model, CSF secreted at the choroid plexus moves by bulk flow through the ventricular system, eventually spilling into the cisternal compartments and subarachnoid space through the foramina of Magendie and Luschka. From the subarachnoid space, CSF is believed to be reabsorbed into the blood through arachnoid granulations that protrude into the dural sinuses by traveling along cranial nerve sheaths or through the dural lymphatics. The bulk reabsorption of CSF along these pathways is the reason that CSF can function as a sink for interstitial solutes as they are cleared from the brain interstitium to the periphery.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here