Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]()
Orthophoria: Exact ocular balance. In this state, perfect equilibrium occurs in the oculomotor apparatus, and the visual axes of each eye intersect at the object of regard.
Phoria (Heterophoria): A latent (hidden/controlled) tendency of visual axis deviation manifesting only when the fusion is disrupted.
Tropia (Heterotropia): A manifest (obvious/seen all the time) visual axis deviation (also known as strabismus or squint ). This condition can be unilateral or alternating, depending on the vision.
Intermittent tropia: An intermittently manifesting visual axis deviation that may exist only in certain gaze positions, at certain target distances, or when the fusion is altered (when person is ill, tired, etc.).
Ductions: Monocular movements into various gaze positions; each eye views in the same direction.
Versions: Synchronous simultaneous movements of the two eyes in the same direction.
Vergences: Binocular eye movements in opposite gaze directions.
Primary Position: Position of the eyes when one is looking straight ahead, with the body and head also straight and erect.
Alignment of the visual axes can be evaluated by objective and subjective clinical methods.
Evaluation of eye movements can be accomplished by objective and subjective techniques.
Patients who have mechanical limitations of eye movements, if cooperative, can be evaluated in an outpatient setting using forced-duction testing and active-force-generation testing.
The clinician evaluating ocular alignment must first decide which information is required—the eye alignment during everyday binocular viewing, the maximal deviation of the visual axes under conditions of disrupted binocular vision, or both of these. Subjective methods are useful for cooperative, communicative older patients, but objective methods must be used in younger patients or those less cooperative. Finally, some testing methods are useful only under research laboratory conditions.
Most laboratory tests are objective. The absolute position of the eye in space may be determined by measurement of the quantity of light reflected by the sclera from a deviated eye. The electro-oculogram (EOG) is generated by alterations in direct current between the front and back of the eye as the eye rotates; this voltage change is detected by suitably placed electrodes. Finally, insulated wire placed in a silicone rubber limbal annulus (eye coil) generates a current in response to a magnetic field; this very precise technique is limited by irritation from the device but may be used to detect horizontal, vertical, and torsional changes in eye position.
The examination of the patient starts as soon as the patient enters the clinic. The way the patient moves, interacts, and navigates around the room and the presence or absence of anomalous head positioning should be evaluated, especially when the patient is comfortable in their own setting. In the examination room, the patient may be stressed enough to hide problems such as intermittent strabismus and phorias. Ideally the clinician should accompany the patient from the waiting room to the examination chair and carefully note the position of the patient’s head when it is mobilized in free space. The clinician should continue to observe the eyes, head positioning, and visual behaviors while the simple pleasantries and conversations take place and also during the history taking. While the patient relaxes, the natural state of the ocular and musculoskeletal system can be seen. Anomalous head positions may indicate restrictive or paralytic strabismus, the presence of a null point in a patient who has nystagmus, or alphabet-pattern strabismus. But it also can be present for other conditions, such as refractive errors, amblyopia, neck musculoskeletal system anomalies, and so forth. Usually, a patient places the head in a position that provides comfortable single binocular vision for the straightened view, but occasionally the head is placed to separate diplopic images maximally or to suppress the less desired second image. The examiner must differentiate between head turns, tilts, and vertical head positions and attempt to quantitate these. The persistency and consistency of these findings are more predictive of true anomalies. Although the amount of turn, tilt, and vertical head positions can be estimated, objective measurements will help to determine if the condition is progressing, regressing, or unchanged over time. Objective measurements using protractors or smartphone applications (i.e., eyeTilt app) can help calculate the exact amount of treatment needed for a given anomalous head positioning resulting from the underlying eye muscle condition.
Once the patient is seated in the examination chair, the patient’s lid position is noted; lid asymmetry is usually present in patients who have vertical strabismus. In cases of hypotropia, pseudoptosis of the eyelid often is associated because of the downward rotation of the eye. Once the eye is straightened, the lid is no longer ptotic. Other soft tissue and bone structures that surround the eye may give false impressions about the ocular alignment to the family and the examiner. Epicanthal skin folds that extend over the nasal sclera in a small child may simulate esotropia; this is noted by parents particularly in pictures and/or when patients are looking at their parents with a head turn and/or with a side gaze. Unilateral or asymmetrical lower-lid retraction may give an impression that the eye on the same side is higher than the fellow eye. Vertical displacement of an orbit may simulate vertical strabismus, and hypertelorism may simulate exotropia. The examiner can declare a patient to be strabismic only after the appropriate alignment testing has been performed.
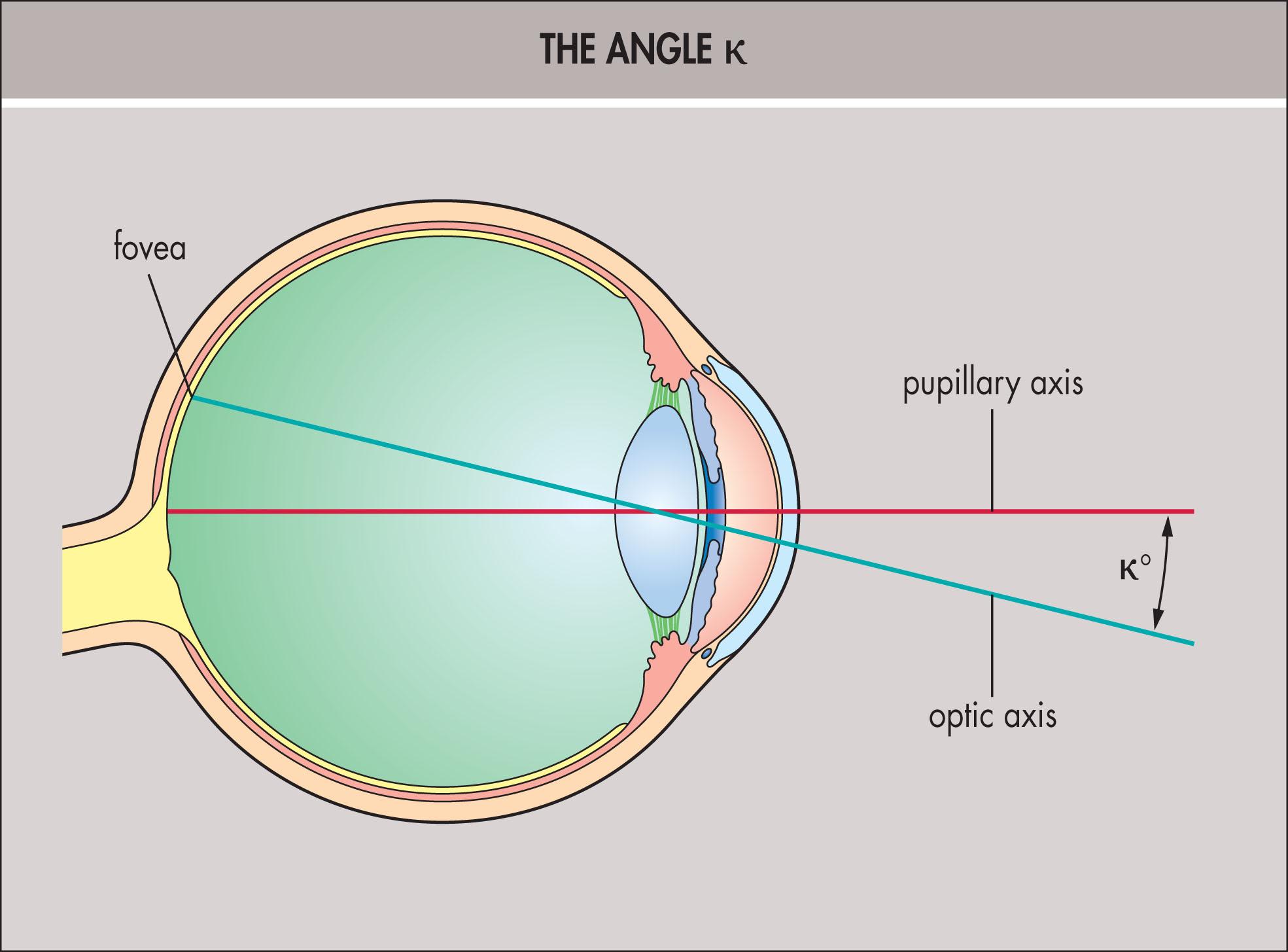
The optic axis can be determined accurately only by alignment of the Purkinje images with a coaxial light through a telescope; this light intersects the retina between the disc and fovea. For clinical purposes, the optical axis may be assumed to strike the fovea. An observer considers the eye to view along its pupillary axis, a line through the pupillary center perpendicular to the cornea. The visual axis outside the eye is usually nasal to the pupillary axis (“positive angle kappa [κ]”) at an average angle of 5° in emmetropic eyes, 7.5° in hyperopic eyes, and 2° in myopic eyes ( Fig. 11.3.1 ). In some myopic eyes, the visual axis is temporal to the pupillary axis, which gives a “negative angle κ.” In some children who have cicatricial retinopathy of prematurity, the fovea is dragged temporally, which results in a large positive angle κ and pseudoexotropia.
Objective clinical methods to determine and measure deviations of the visual axes include corneal light reflex tests, cover tests, and haploscopic tests (i.e., synoptophore/amblyoscope, etc.). These tests do not require any response by the patient and thus are independent of the patient’s ability to interpret the testing environment.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here