Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Forearm instability is a complex and debilitating condition. The term Essex-Lopresti injury refers to injuries consisting of fracture of the radial head with longitudinal disruption of the interosseous membrane (IOM) and distal radioulnar joint (DRUJ). This instability has been termed longitudinal radioulnar dissociation (LRUD), and DRUJ disruption also may involve injury to the triangular fibrocartilage complex (TFCC). These injuries were first described in 1946 by Curr and Coe and coined Essex-Lopresti injuries after two cases were reported in 1951. The IOM, also frequently referred to as the interosseous ligament (IOL) due to its biomechanical properties, is an important structure in forearm and wrist stability. It plays an important role in axial load transmission through the forearm and is an anchor for several forearm muscle attachments.
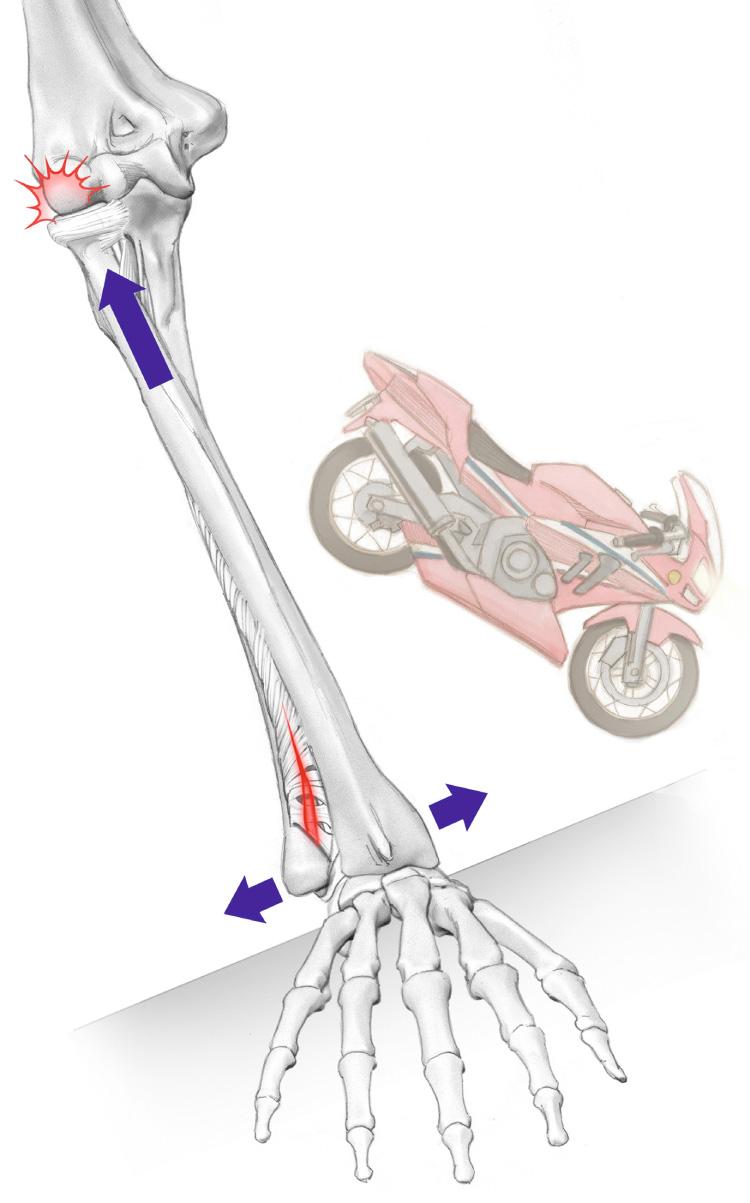
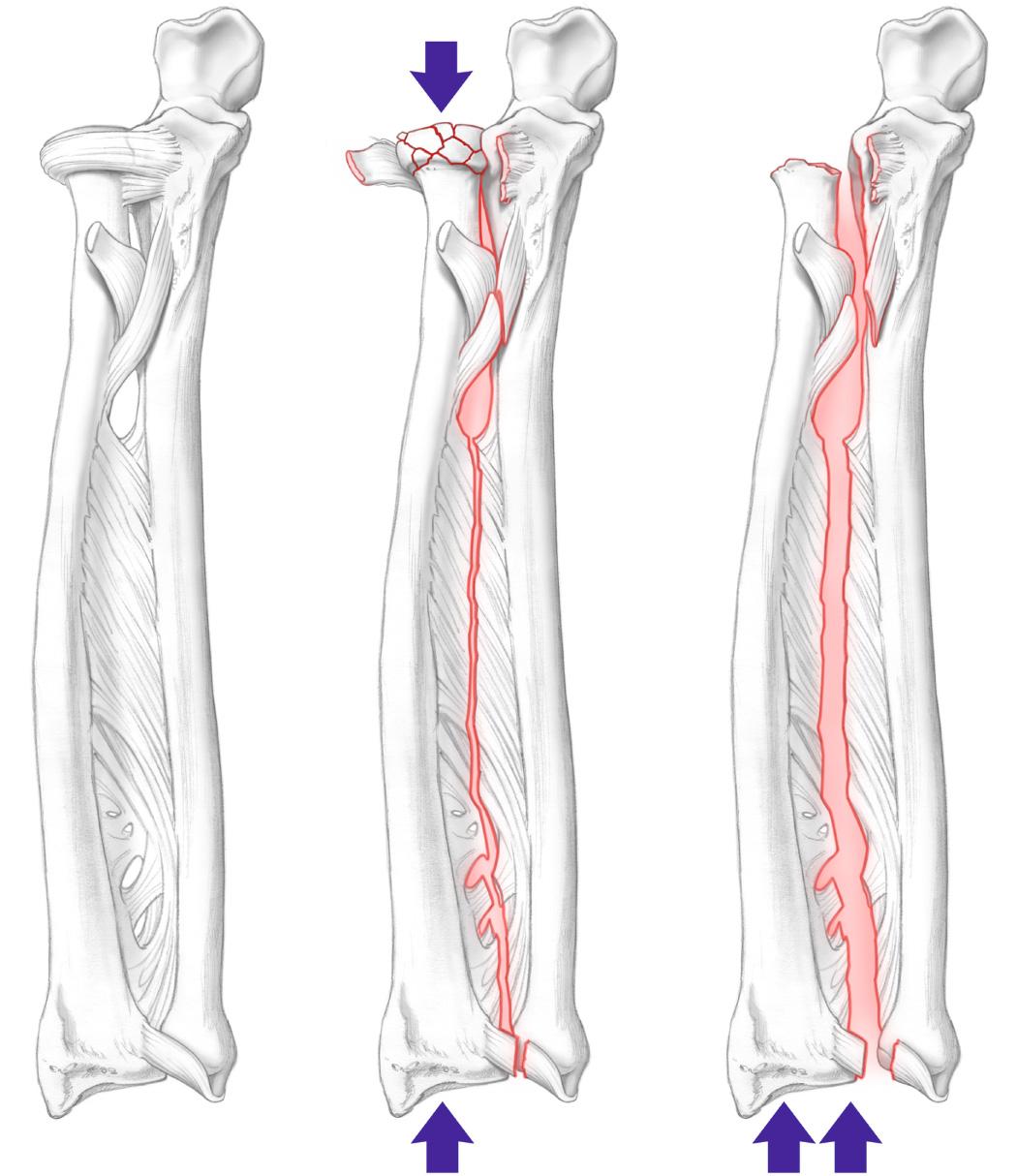
The injury occurs when a longitudinal force is transmitted through the forearm, resulting in fracture of the radial head possibly with dislocation and disruption of the IOM and DRUJ ( Fig. 41.1 ). The loss of forearm stability causes functional limitations, pain, and motion. These injuries are frequently missed, acutely leading to late complications of forearm instability and proximal radius migration and ulnocarpal impingement. The Edwards and Jupiter classification of radial head fracture is shown in Table 41.1 . Many cases were observed as a late complication after excision of comminuted fractures of the radial head. The injury has even been associated with presumed simple stable fractures of the radial head.
| Description | Treatment | |
|---|---|---|
| Type I | Large displaced fragment + no/minimal comminution | Open reduction internal fixation |
| Type II | Comminuted fracture not amenable to fixation | Radial head excision or arthroplasty |
| Type III | Chronic with irreducible proximal migration | Ulnar shortening |
Essex-Lopresti injuries and LRUD are uncommon. The incidence of forearm instability occurs in 0.3% to 5% of all radial head fractures. Incidence and symptoms can be commonly unrecognized, with possible adverse late consequence.
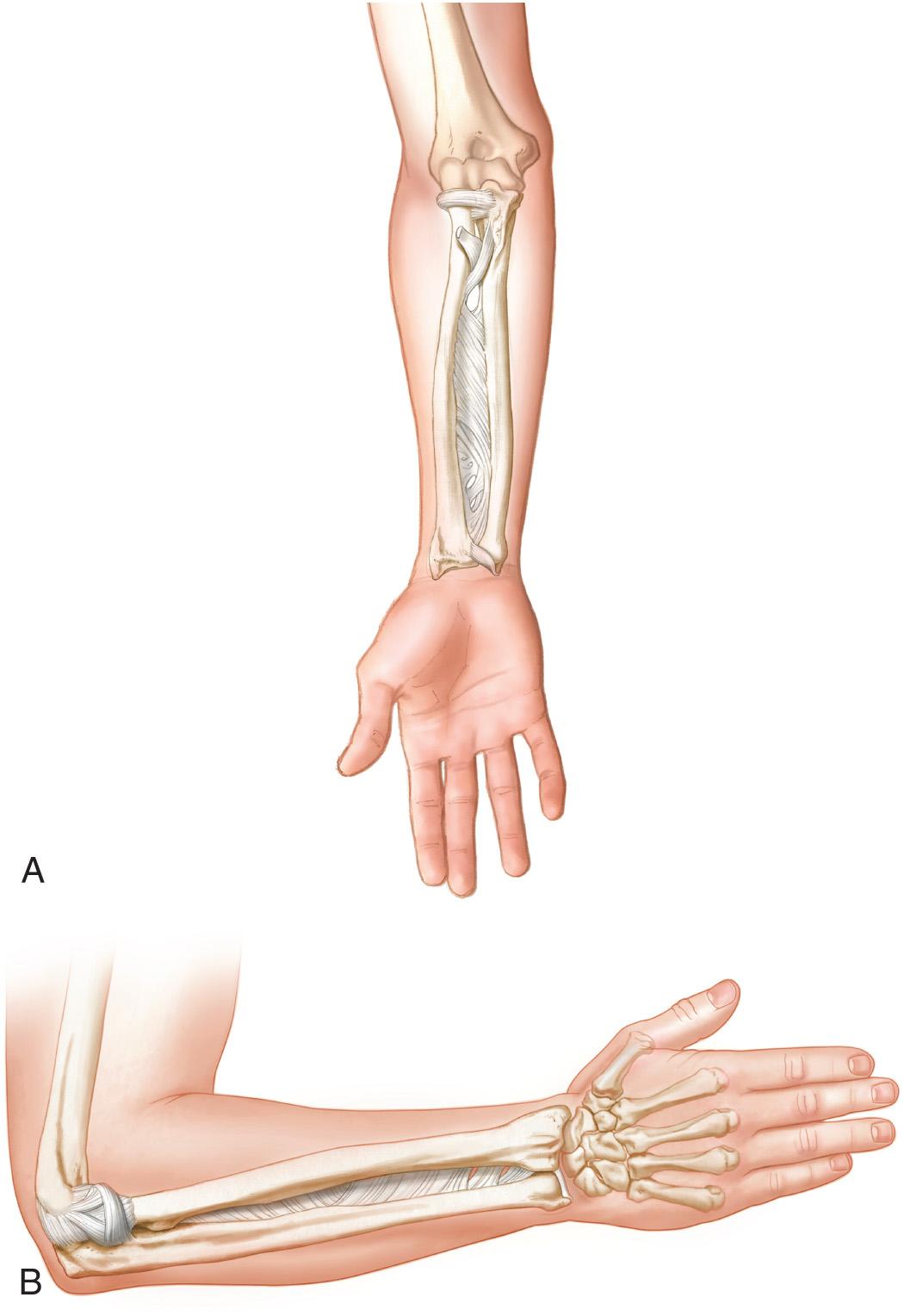
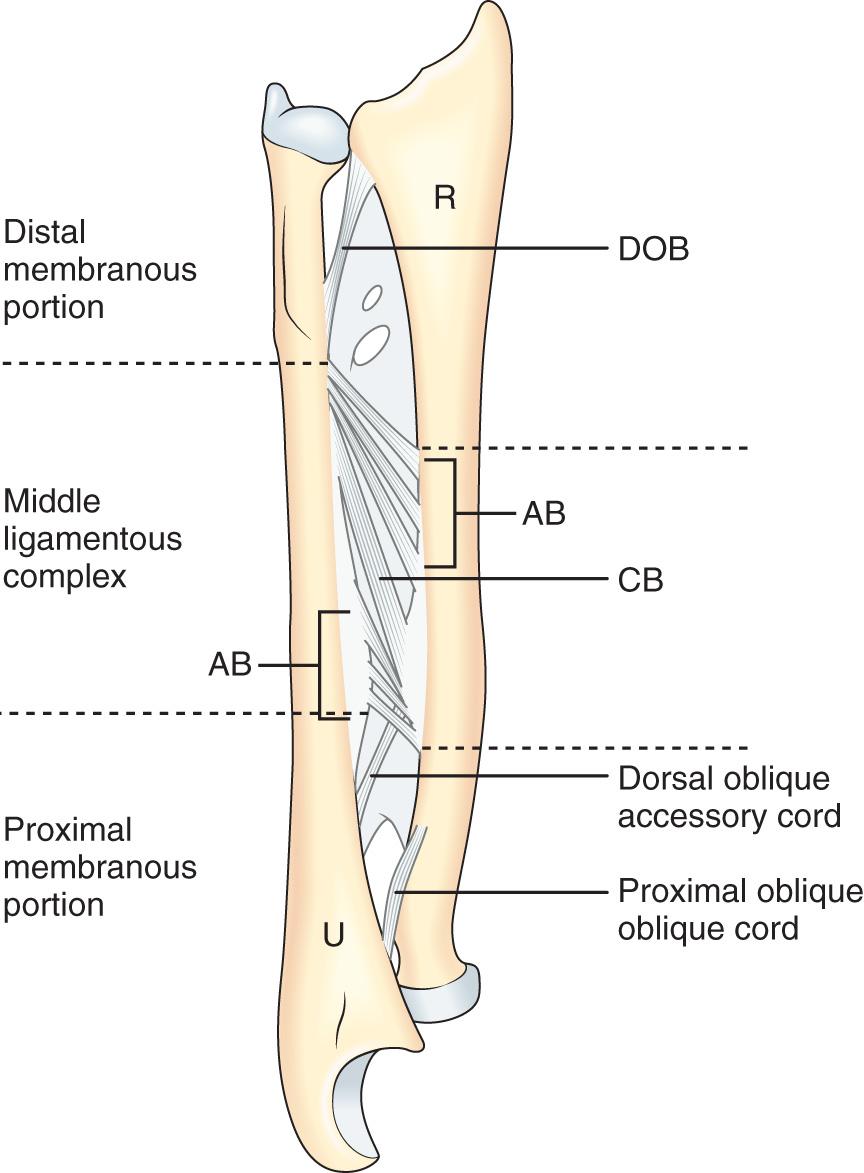
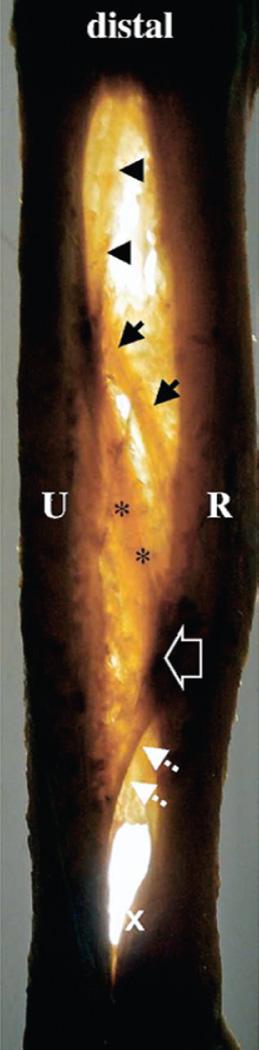
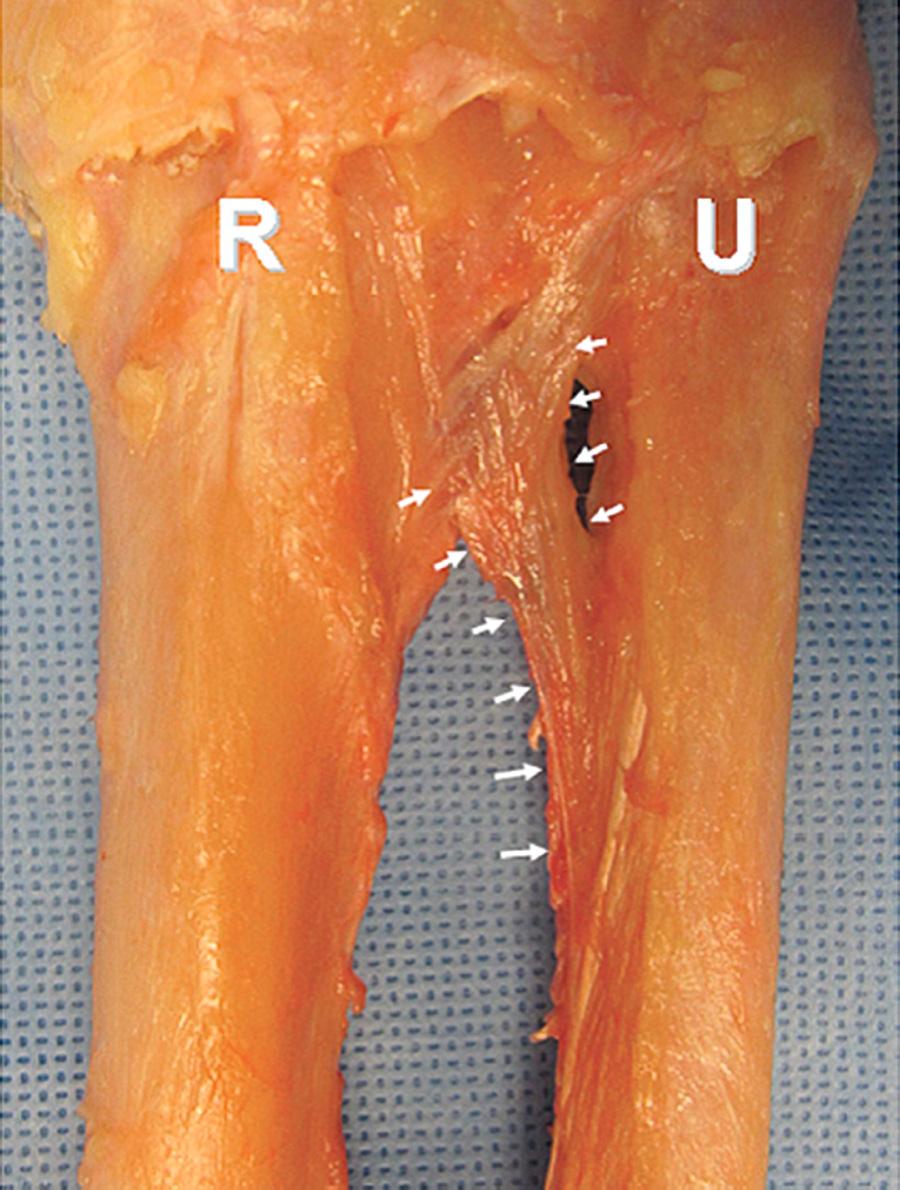
The forearm requires stability in order to maintain its function as a lever arm while allowing for motion at the wrist, elbow, and forearm. An illustration of relevant forearm anatomy is provided in Fig. 41.2A and B . The primary stabilizer of the forearm is the radial head, with the IOM and TFCC playing secondary roles. The IOM is a stout ligamentous complex made up of five kinds of ligaments: a large central band, a proximal interosseous band (proximal oblique cord), a distal oblique bundle, a dorsal oblique accessory cord, and occasionally other accessory bands ( Figs. 41.3 and 41.4 ). The central portion of the IOM is thickened and thought to be a major portion of restraint to proximal radial migration. This central portion is referred to as the central band (CB) and is generally used indistinguishably from the IOM and IOL as it exerts the greatest biomechanical component to forearm stability of the complex. The CB has tensile strength comparable to the patellar tendon. The CB attaches primarily on the volar aspect of the apex of the radius and on the dorsal aspect of the ulna and maintains a 22- to 24-degree angle between the radius and ulna. The width of the CB has been reported from 1.1 cm to 2.6 cm. The CB is found along the radius and ulna between 53% and 64% (midpoint 49%) from the distal radius and 29% to 44% (midpoint 42%) from the distal ulna. IOM variations with thickened fibers at the distal IOM termed the distal oblique bundle have been described, and some reconstruction techniques have focused on this segment. The distal oblique bundle runs from the distal one-sixth of the ulnar shaft to insert on the inferior rim of the radius sigmoid notch ( Fig. 41.5 ). It was noted to be present as an obvious distinct structure in 12 of 30 cadaver specimens, originating from the distal one-sixth of the ulnar shaft and inserting into the inferior rim of the sigmoid notch. The dorsal oblique accessory cord has been shown to be present in just over half of cadaver specimens, originating from the distal two-thirds of the ulnar shaft and inserting onto the interosseous crest of the radius. The proximal oblique cord is universally present, originating from the anterolateral coronoid process of the ulna and inserting just distal to the radial tuberosity. A description of ligamentous attachments is shown in Table 41.2 .
| Ligament | Origin | Insertion | Width | Thickness | Notes |
|---|---|---|---|---|---|
| Central band | Interosseous crest of radius | Interosseous border of ulna | 9.7 ± 3 mm (range, 4–16 mm) | 1.3 ± 0.2 mm (range, 1–1.6 mm) | Universally present |
| Distal oblique bundle | Distal one-sixth of ulnar shaft | Inferior rim of sigmoid notch of radius | 4.4 ± 1.1 mm (range, 2–6 mm) | 1.5 ± 0.5 mm (range, 0.4–2 mm) | Seen in 12 of 30 cadavers. Runs along proximal border of pronator quadratus and distal fibers blend with capsular tissue of distal radioulnar joint. |
| Dorsal oblique accessory cord | Distal two-thirds of ulnar shaft | Interosseous crest of radius | 3.2 ± 1 mm (range, 1.9–5 mm) | 0.9 ± 0.2 mm (range, 0.5–1 mm) | Seen in 16 of 30 cadaver specimens. Runs along posterior aspect of forearm |
| Proximal oblique cord | Anterolateral aspect of coronoid process of the ulna | Distal to radial tuberosity | 3.7 ± 1.6 mm (range, 1.5–8 mm) | 1.1 ± 0.5 mm (range, 0.4–2 mm) | Universally present. Also known as the ligament of Weitbrecht . |
The IOM fibers align from the proximal radius to insertion on the ulna distally and are loaded when the radius is displaced proximally. With an axial load applied to the forearm, the IOM stabilizes bending forces to prevent bowing or splaying of the radius and ulna. The forearm IOM provides both longitudinal and transverse stability to the forearm. The IOM acts as a secondary stabilizer of the DRUJ with the TFCC as primary stabilizer. The distal IOM stabilizes in the dorsal-volar plane as well as in the longitudinal (proximal-distal) plane, constraining dorsal dislocation of the radius at the DRUJ. The IOM functions in transverse stability by maintaining the radio-ulnar relationship and keeping them from splaying apart with loading and to counteract bending and twisting forces applied between them. The pathologic condition in longitudinal dissociation associated with Essex-Lopresti injuries is proximal migration of the radius, which causes the ulna to become more prominent, leading to increased forces on the ulna at the wrist and ulnocarpal impaction ( Fig. 41.6 ). Ulnocarpal impaction can lead to ulnar-sided wrist pain and degenerative changes in the wrist.
The IOM plays an important role in load transmission. Two-thirds of the mean axial load was transmitted through the radius and one-third through the ulna normally. A biomechanical study by Palmer and Werner found that the ulna transmits 20% of load at the wrist. In other studies, this number ranged from 9% to 40%. A more positive ulnar variance will increase force transmission through the ulna. The total axial load at the elbow is nearly equalized due to the load transfer. The IOM only becomes the primary load-bearing structure when there is an initial gap between the radial head and capitellum. After radial head excision, the TFCC accounts for 8% of the total forearm stiffness, and the IOM accounts for 71%. For significant proximal migration to occur, some have proposed that both the IOM and TFCC must be affected. Sectioning of the proximal and distal thirds of the IOM had no effect on force. However, total sectioning of IOM causes significantly increased force in all wrist positions. With IOM compromised, the loads at the wrist also become equal, and no load transfer is performed. In pronation, stresses at the DRUJ are lower and more uniform throughout. Proximal fibers are more stressed in neutral rotation, whereas distal fibers are more stressed in supination.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here