Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Endovenous thermal ablation (ETA) procedures are advantageous for the treatment of primary varicose veins over both stripping surgery and foam sclerotherapy.
Most evidence exists for endovenous laser ablation (EVLA) and radiofrequency segmental ablation (RFSA).
ETA procedures can prevent the complications of varicose vein disease.
Preoperative duplex ultrasound (US) investigation of the complete superficial and deep venous system and in particular of the veins to be treated, is obligatory.
Appropriate phlebological training and skills in the different ETA methods are mandatory.
Untreated primary chronic venous disease (CVD) can lead to symptoms such as edema, stasis dermatitis, hypodermitis, skin hyperpigmentation, dermatoliposclerosis, skin atrophy, and, in 1–2% of the population, venous ulceration. Early treatment of varicose veins reduces the incidence of these complications. For many decades, stripping and ligation of the saphenous veins has been the standard treatment for this condition. Surgery, usually performed in general or spinal anesthesia, was associated with postoperative hematoma and pain, with scars and a high recurrence rate. An alternative treatment to traditional stripping and ligation is the endovenous thermal ablation (ETA) of the saphenous varicose veins with radiofrequency, laser or steam. Radiofrequency, laser or steam energy thermally denatures vein wall collagen, leading to vein wall inflammation, fibrosis, and finally to the occlusion of the treated vein.
Different devices are available for the treatment of varicose veins with endovenous thermal ablation (ETA). Best evidence exists today for radiofrequency segmental ablation and for endovenous laser ablation (EVLA). The evidence for bipolar radiofrequency ablation or for the ablation with steam is still poor.
The indications for treatment are: insufficient great (GSV) and small (SSV) saphenous veins, intrafascial parts of accessory saphenous veins (ASV), Giacomini vein and cranial extension of the SSV, insufficient perforating veins, and venous malformations.
The absolute contraindications are: acute deep venous thrombosis, acute infections at puncture sites, and deep venous obstruction if the vein to be treated is a functional collateral.
Relative contraindications are: immobile or hardly ambulating patients, severe peripheral arterial occlusive disease, patients who are unable to undergo local or general anesthesia, high thromboembolic risk, pregnancy, and uncontrolled severe diseases (e.g., active cancer) ( Table 37.1 ).
| Inclusion criteria: |
| Insufficient intrafascial superficial vein (GSV, SSV, accessory saphenous veins, Giacomini vein, cranial extension of the SSV) |
| Exclusion criteria: |
| Tortuous vein difficult to catheterize |
| Completely or partly occluded vein (thrombosed, hypoplastic, intraluminal webs) |
| Vein segment to be treated shorter than required for the safe insertion of the catheter (depending on the type of the catheter; commonly >5 cm) |
| Patients with acute deep venous thrombosis |
| Patients with significant leg edema who cannot be adequately monitored by ultrasound |
| Immobile or hardly ambulating patients a |
| Concomitant significant peripheral arterial disease (ankle : brachial pressure index <0.8), which prevents post-procedural compression b |
| Patients unable to undergo anesthesia |
a A relative contraindication;
b A study showed that the lowest value of the ABI may be even 0.6 (eccentric compression allows sufficient vein compression without a further compromise of the arterial circulation).
Apart from the general equipment and materials required for a free-standing phlebologic surgery office, those more or less specific for the procedure of RFSA and EVLA are listed in Box 37.1 .
Sterile (disposable) drapes for protection of the operative field
Sterile 10 × 10 cm 2 gauze pads
Infiltration pump with accompanying sterile tubing
20G or 22G needles for tumescent anesthesia infiltration
Sterile adhesive tape or surgical clamps for fixation of tubing and ultrasound probe cable
19G or 21G ultra thin-walled Seldinger needle
Scalpel blade No.11
A sterile 0.025 inch guide-wire
A sterile 7F (2.33 mm), 11 cm-long introducer sheath (for RFSA) or introducer sheath for EVLA depending on the fiber used
Sterile ultrasound gel
Sterile ultrasound transducer cover
Sterile physiologic saline
Sterile plastic 10 mL syringes
VNUS RFG Plus RF generator
ClosureFast™ catheter, 60 cm or 100 cm length (with a 7 cm or 3 cm-long heating element)
Laser device (810 nm, 940 nm, 980 nm, 1064 nm, 1320 nm, or 1470 nm)
Laser fiber (bare or radial fiber)
Adhesive sterile tape (Steri-Strip)
Tilt operating table
Mayo stand
Duplex ultrasound scanner with peripheral vascular probe (7.5–10 MHz)
Cardiac/blood pressure/pO 2 monitor
Skin disinfectant
Compression stockings (class 2: 30–40 mmHg graduated support stockings)
Protective skin underwrap
Absorbent pads
As with any procedure, informed patient consent is mandatory prior to the operation. After a detailed explanation of the treatment procedure (including consequences of the “non-treatment” option), we give patients written explanatory material about the procedure and post-procedural care. When the patient has made the final decision, the date of surgery is fixed.
On the day of surgery, the pertinent health-related data are again reviewed with the nurse, through a short structured form. Any further questions regarding the procedure are answered. The patient is then taken into the changing room, undresses and puts on a light operation gown and special disposable underpants.
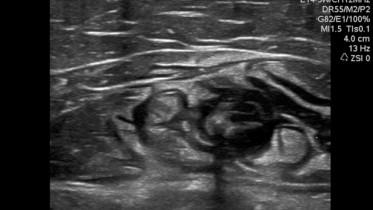
In the operating room, we first perform preoperative marking of the veins to be treated. Marking is performed with the patient standing. If only ETA is planned, then marking may be limited to this particular vein. However, most of the time, other varicose veins are treated simultaneously with sclerotherapy and/or phlebectomy, and marking must include all of these veins. The veins are visualized by observation, palpation, and duplex ultrasound scanning. If the patient has worn compression bandages or stockings, they are removed, and if additional treatment of varicose veins by phlebectomy or sclerotherapy is planned, the patient is left standing or sitting for 15–20 min prior to marking, in order to allow varicosities to refill. The veins are marked with an indelible surgical pen. First, the visible varicose veins are marked. At this stage, we improve vein tracing with palpation and percussion. Then, insufficient veins are identified by duplex scanning ( Fig. 37.1 ) with the high frequency transducer (>7.5 MHz) and also marked. In the case of ETA, it is mandatory to examine the vein to be treated in its whole length. The access point into the vessel is marked on the skin (usually the most distal point of the refluxing vein – the distal point of insufficiency). For GSV, it is marked along its whole direction with special attention paid to great saccular dilatations (may require more thermal cycles or higher energy density than usual); tortuosity (may require special attention and manual assistance during catheter advancement); intraluminal webs (may make catheter advancement difficult or impossible); position with respect to the saphenous intrafascial compartment and distance from the skin surface (if a vein segment is outside the compartment and/or close to the skin surface, it is necessary to infiltrate more tumescent solution in order to protect the skin from burns); and relative position of the GSV to the deeper structures, especially the femoral artery. The latter is very important in very thin individuals in whom the two vessels may be separated by a narrow space of a few millimeters – the space should be carefully filled with a large volume of tumescent solution in order to prevent thermal damage of the artery. If the GSV is doubled or even tripled, the refluxing vessel(s) should be precisely marked. The position of the saphenofemoral junction (SFJ) is also marked, which facilitates proper infiltration of tumescent solution in the uppermost portion of the GSV. A similar approach is followed for SSV. The popliteal fossa may be rather demanding for examination but it is crucial to precisely map the SSV and saphenopopliteal junction (SPJ) or, if it is not present, to determine the upper point of ablation. Duplex is very helpful in distinguishing an incompetent popliteal fossa perforator from the SPJ. In addition, the position of the sciatic nerve and its major branches (tibial and common fibular nerves), and the sural nerve in relation to the SSV may be analyzed and hence, appropriate infiltration of tumescent solution may help prevent nerve damage during the procedure. In cases of accessory saphenous veins, the intrafascial part of the vein may be treated by ETA if feasible in length for the catheter used. This part is also marked on the skin. The remaining, usually varicose subcutaneous, segments are best removed with stab phlebectomy or sclerosed with foam. In a very obese patient, marking of the GSV is best performed in the sitting position, as the vein will move in the recumbent position away from its skin marking if it was made while the patient was standing.

Radiowaves generated with a frequency of 200–3000 kHz (alternating current) raise tissue temperature by so-called “resistive heating” – the electric current passing through the tissue is slowed down by resistance of the latter (impedance), and the net result is the generation of heat. Usually, the heat generated in this way affects a narrow rim of tissue (<1 mm) around the source of the radiowaves (electrode) and slowly dissipates into deeper planes, with a gradual drop in the temperature. The highest temperature of 120°C around the electrode leads to coagulative necrosis of endothelium and shrinkage of collagen in the vein wall. The damaged tissue is replaced by fibrosis and scarring, leading, after many months, to the ablation of the vein.
The second-generation radiofrequency (RF) catheter (ClosureFast™, Covidien, Mansfield, MA), introduced in 2007, has a 7-cm or 3-cm long monopolar electrode (fixed diameter 7F) at its distal end, which produces radiofrequency current ( Fig. 37.2 ). The heating element is designed in such a way as to prevent the build-up of coagulum, and the catheter itself is covered with a lubricious material to avoid sticking after every heating cycle. A thermocouple device integrated within the electrode and connected to the microprocessor in the radiofrequency generator monitors tissue temperature and automatically adjusts delivered energy. It ensures that the tissue around the electrode is exposed to the desired temperature, i.e., 120°C. A series of animal experiments were used to select the best parameters: temperature of 120°C and 20 s heating cycle duration. In order to achieve optimal tissue effects, the heating element must be in a close apposition with the vein wall. Three maneuvers assure that the vein wall is in close contact with the electrode, the first being the most important: tumescent anesthesia infiltrated around the vein completely compresses the vessel, the leg is in the Trendelenburg position, and additional external manual compression is exerted by the ultrasound probe or a fabric roll. The catheter shaft is marked at every 6.5 (or 2.5) cm, so that considering the 7 (or 3) cm length of the heating element, following the marks ensures a 0.5 cm overlapping zone, and guards against skipping up vein segments. As the heating cycle takes 20 s for every segment, the treatment of a 35 cm-long GSV takes roughly 2 min.

The first generation of VNUS ® catheters for radiofrequency ablation (ClosurePlus™) required a continuous pull-back similar to endovenous lasers and the target temperature was only 85°C. Even with these technical characteristics it proved to be superior to standard surgical procedures (high ligation and stripping of the GSV). In the prospective randomized comparative study published in 2003 (EVOLVeS), patients returned to normal activities after the mean 1.15 days vs 3.89 days for classic surgery, and the percentage of patients returning to routine activities within 1 day was 80.5% vs 46.9% for the RFA and GSV stripping groups, respectively. At the 2-year follow-up, patients treated with RFA experienced a superior quality of life compared with those treated with vein stripping surgery. Outcomes of RFSA in the treatment of GSV insufficiency in terms of venous closure and clinical improvement after up to 3 years have been published. Rates of complete vein closure as a measure of technical success after 1, 2, or 3 years have been reported to be 97%, 94%, and 93%, respectively. The proportion of treated GSV without reflux was even higher: 96.5% and 95.7% after 2 and 3 years. In particular, the newer version of the catheter (ClosureFast™) seems to be more effective in comparison to the original catheter used until 2007; the latter resulted in 88% GSV without reflux after 3 years. The average time from ClosureFast™ catheter insertion to its removal, including the time required for the administration of tumescent anesthesia, was a remarkable 16.4 min. It was well tolerated and patient recovery after the intervention was minimal. In these studies, no patient developed skin burns, DVT, extension of thrombus into the common femoral vein, or other serious adverse events. The most common side-effects were bruising, paresthesia, and hyperpigmentation, reported in 6.4%, 3.2%, and 2% of patients, respectively. The average VCSS score improved from 3.9 ± 2.1 at screening, to 0.7 ± 1.2 at 24 months follow-up ( p < 0.0001). While only 41.1% of patients were free of pain before treatment, at 24 months 99.3% reported no pain and 96.4% did not experience pain during the 12 months before. These studies confirmed the efficacy of RFSA when using ClosureFast™ with few side-effects and almost no post-procedural pain. A recent similarly designed single-center, randomized UK study also compared EVLA (980 nm) and RFSA (ClosureFast™) in the treatment of GSV reflux in 131 patients. RFSA with ClosureFast™ was associated with less post-procedural pain than EVLA using a bare fiber, whereas clinical and quality-of-life improvements were similar after 6 weeks for the two treatments. In addition, patients who underwent RFSA returned to work quicker than those treated with EVLA (median 5 vs 9 days). However, new generation EVLA using high wavelength laser systems and radial fibers produces significantly less pain and bruising. Personal experience of the authors, who have performed RFSA with the ClosureFast™ catheter on more than 400 patients, confirms high patient satisfaction and occlusion rates at 2 and 3 years after the procedure (97%). RFSA is perfectly suited for an office-based intervention, which can be performed solely in the tumescent anesthesia. The majority of patients after ClosureFast™ ablation return to work 1–3 days after surgery. Contrary to the classical surgical approach, RF ablation has not been shown to cause neovascularization at the groin. Overall, the data support efficacy and safety of the RFSA procedure in the treatment of insufficient GSV. Small saphenous vein (SSV) can also be effectively treated with RFA in the same way as in the case of GSV paying greater attention to the catheter tip position and the amount of tumescent anesthesia infiltrated in order to protect adjacent nerves. The efficacy is even more clinically important in light of higher recurrence rates after saphenopopliteal surgery.
The RFSA procedure can be comfortably performed by an operator and two assistants. One of the assistants works in non-sterile conditions and is available to use the duplex ultrasound machine and RF generator when necessary.
An assistant hands the ultrasound transducer to the operator who takes it into the sterile cover previously filled with the non-sterile ultrasound gel. The cover is then fixed around the transducer with a sterile elastic rubber ring. The site where the vein will be accessed is infiltrated with a small amount of 1% lidocaine. Sterile ultrasound gel is spread over the site. Under ultrasound guidance, the operator cannulates the vein with the 19G needle using the Seldinger technique ( Fig. 37.3 ). When venous return is noted, a gauze pad is placed below the needle to absorb the blood, and the guide-wire is gently inserted through the needle into the vein. The needle is withdrawn. The patient is then placed in the Trendelenburg position.

The insertion site is then widened with a scalpel blade, which cuts the skin at an acute angle to make an incision some 2 mm long. Introducer sheath and dilator are separately flushed with sterile saline through the Luer port with cap and lumen, and then reassembled. The introducer sheath is passed over the guide-wire into the vein lumen (assure that the end of the guide-wire is protruding at the back end of the introducer sheath). Stop advancement if there is resistance. The introducer sheath may be placed into the vein at its whole length or only a part of its length may be introduced (preferably at least a half). The guide-wire is then withdrawn. A ClosureFast™ catheter is removed from the pouch and cable connector passed out of the sterile field to the assistant who connects it to the RF generator. The catheter lumen is flushed with sterile normal saline through the Luer port at the handle. The port is then capped. Under ultrasound guidance, the catheter is then advanced through the introducer sheath. The catheter tip should be placed just below the ostium of the superficial epigastric vein or approximately 2–2.5 cm below the SFJ ( Fig. 37.4 ). The catheter is adjusted so that the closest shaft mark is aligned with the hub of the sheath. Check the catheter tip position by ultrasound again.
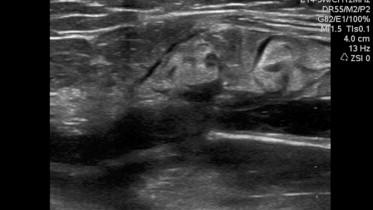
At this point, the operator proceeds with the infiltration of tumescent anesthesia. Solution made for the RFSA is the same as prepared for EVLA or stab phlebectomies ( Table 37.2 ). The final lidocaine concentration is 0.1% or 0.05%. Usually, roughly 500–700 mL of the solution is infiltrated per GSV, and the volume rarely exceeds 1 L. It is well below the safety margin for lidocaine toxicity for an average person weighing 70 kg; some 3.5 bags (1000 mL bag) of 0.1% lidocaine (total dose <55 mg/kg). For infiltration of the anesthesia we use the infiltration pump on a low setting. Infiltration starts at the distal end, close to the puncture site. Ultrasound is crucial for proper placement of tumescent solution within the saphenous fascial compartment ( Fig. 37.5 ). In general, the amount of solution infiltrated per 1 cm of the vein's length should be roughly 10 mL. In practice, the space should be filled enough so that the vein collapses around the catheter, and the distance from the skin surface should be at least 1 cm. When the needle is within the saphenous compartment, the solution relatively easily flows proximally, and as few as 4–5 punctures along the vein's length are enough to infiltrate the whole space. The needle punctures should be painless as the needle is inserted through the most proximal part of already infiltrated portion. Special attention is paid to the area of the SFJ/SPJ. After the infiltration of the area, some 5 cm distal to the junction, the catheter tip position is again visualized and checked for the proper placement, and the last portion is infiltrated (over and beyond the junction). It is of paramount importance not to allow the catheter tip to slide down the deep vein (femoral or popliteal) and cause thermal damage. Within the popliteal fossa, the proper amount of tumescent solution around SSV reduces the possibility of thermal damage to the sciatic nerve and its major branches (tibial and sural nerves).
| Component | Solution with 0.05% (500 mg/L) lidocaine | Solution with 0.1% (1000 mg/L) lidocaine |
|---|---|---|
| Physiologic solution | 960 mL | 940 mL |
| Lidocaine (2%) | 25 mL | 50 mL |
| Adrenaline (1 mg/mL) | 1 mL | 1 mL |
| Sodium bicarbonate (8.4%) | 10 mL | 12.5 mL |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here