Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Since the first report of ERCP and endoscopic biliary sphincterotomy in 1974, there have been numerous advances in ERCP techniques. Less invasive diagnostic modalities including EUS, CT, and MRCP have replaced diagnostic ERCP. However, therapeutic ERCP remains useful for the treatment of pancreatic diseases, and continually evolves. This chapter reviews the endoscopic treatment of acute pancreatitis and its complications, as well as the endoscopic treatment of recurrent acute pancreatitis, chronic pancreatitis, pancreatic cancer, and pancreatic cysts.
When a patient presents with acute pancreatitis, the role of endoscopy is limited to 2 situations: first, those patients with gallstone-induced pancreatitis (see Chapters 58 and Chapter 66 ) and, second, to provide nutritional support via enteric feeding (see Chapter 6 ). Gallstone pancreatitis is caused by transient or sustained impaction of sludge or a stone within the common channel of the ampulla of Vater. ERCP and biliary sphincterotomy are used to improve the outcome of gallstone pancreatitis by removal of an impacted stone and subsequent relief of pancreatic ductal obstruction. Early studies of patients with acute gallstone pancreatitis suggested that ERCP and sphincterotomy within 72 hours of admission improved outcomes in patients with clinically severe acute pancreatitis. Meta-analyses have not, however, demonstrated that early routine ERCP significantly affects mortality and local or systemic complications of pancreatitis, regardless of predicted severity. However, there is support for current recommendations that early ERCP should be considered in patients with coexisting cholangitis or biliary obstruction. Thus ERCP is best reserved for patients with suspected biliary obstruction, based on hyperbilirubinemia and evidence of clinical cholangitis, because it is unlikely that the ampulla is obstructed in the presence of a normal serum bilirubin. Less invasive imaging modalities that can evaluate bile duct stones in patients with severe biliary pancreatitis include CT, MRCP, and EUS. These tests can help select patients for ERCP if bile duct stones are identified, and prevent unnecessary ERCP and the risk of potential adverse events. , If bile duct stones are not identified during ERCP performed for acute gallstone pancreatitis, there are no data to guide whether an empiric biliary sphincterotomy should be performed. Sphincterotomy can reduce the risk of recurrent acute pancreatitis and cholangitis prior to cholecystectomy. However, early laparoscopic cholecystectomy (within 3 days) in mild biliary pancreatitis, without waiting for normalization of liver enzymes, can improve outcomes and decrease the need for subsequent ERCP. Indeed early cholecystectomy is considered the standard of care. In those patients who do not undergo cholecystectomy, ERCP with biliary sphincterotomy reduces the risk of recurrent gallstone pancreatitis.
Evidence supports early enteral feeding for patients with severe acute pancreatitis, based on randomized prospective studies. Lower-cost and fewer infectious complications are seen with enteral feeding as compared to parenteral nutrition (see Chapter 6 ). NG feeding appears to be as effective as tubes placed beyond the ligament of Treitz, although the latter are preferred in patients who do not tolerate NG feeding owing to gastric retention from severe duodenal edema. There are a variety of endoscopic techniques for placing nasojejunal feeding tubes in the setting of acute pancreatitis, including transnasal endoscopy.
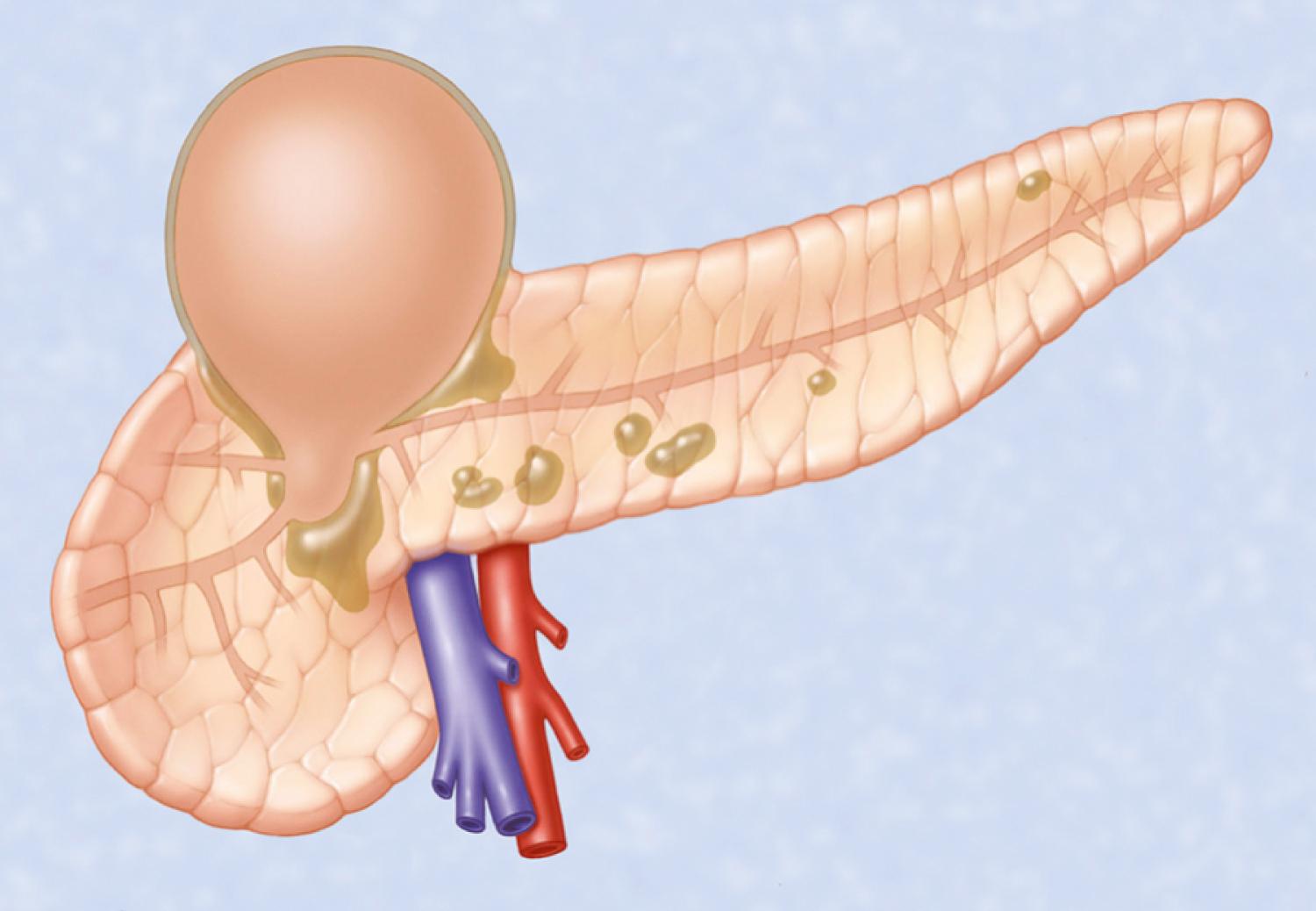
There are a variety of local complications that can arise as a complication of acute pancreatitis with defined nomenclature. These include peri-pancreatic fluid collections, pancreatic and peripancreatic necrosis (sterile or infected), and pseudocyst and walled-off necrosis (WON; sterile or infected). Patients with well-demarcated symptomatic and/or infected collections that are in close proximity (apposition) to the gastric or duodenal wall can be treated with endoscopic drainage. Acute peripancreatic fluid collections form early in the course of acute pancreatitis and usually resolve without therapy. Acute pseudocysts arise as a sequela of acute pancreatitis, require at least 4 weeks to encapsulate, and are devoid of significant solid debris. Acute pancreatic pseudocysts usually form as a result of a pancreatic ductal leak ( Fig. 61.1 ). Alternatively, areas of pancreatic and peripancreatic fat necrosis may liquefy over time and become a pseudocyst. Despite the requirement of at least 4 weeks for a pseudocyst to encapsulate, it is important to realize that in some patients with significant early acute pancreatic necrosis (>30% necrosis), the pancreatic and peripancreatic necrosis may evolve into a collection that radiographically resembles a pseudocyst. These collections contain significant solid debris, and endoscopic treatment of them using typical pseudocyst drainage methods often results in infectious complications because of contamination and inadequate removal of solid debris.
Drainage of an acute pseudocyst is indicated for treatment of symptomatic pseudocysts that may or may not be infected and for progressive enlargement on imaging studies. Symptoms and signs from an acute pseudocyst include abdominal pain (often exacerbated by eating), weight loss, gastric outlet obstruction, obstructive jaundice, and pancreatic duct leakage, which may result in pancreatic ascites or pancreatic fistulae. Pseudocysts may be drained through the papilla (transpapillary), through the gastric or duodenal wall (transmurally), or by using a combination of these modalities. ,
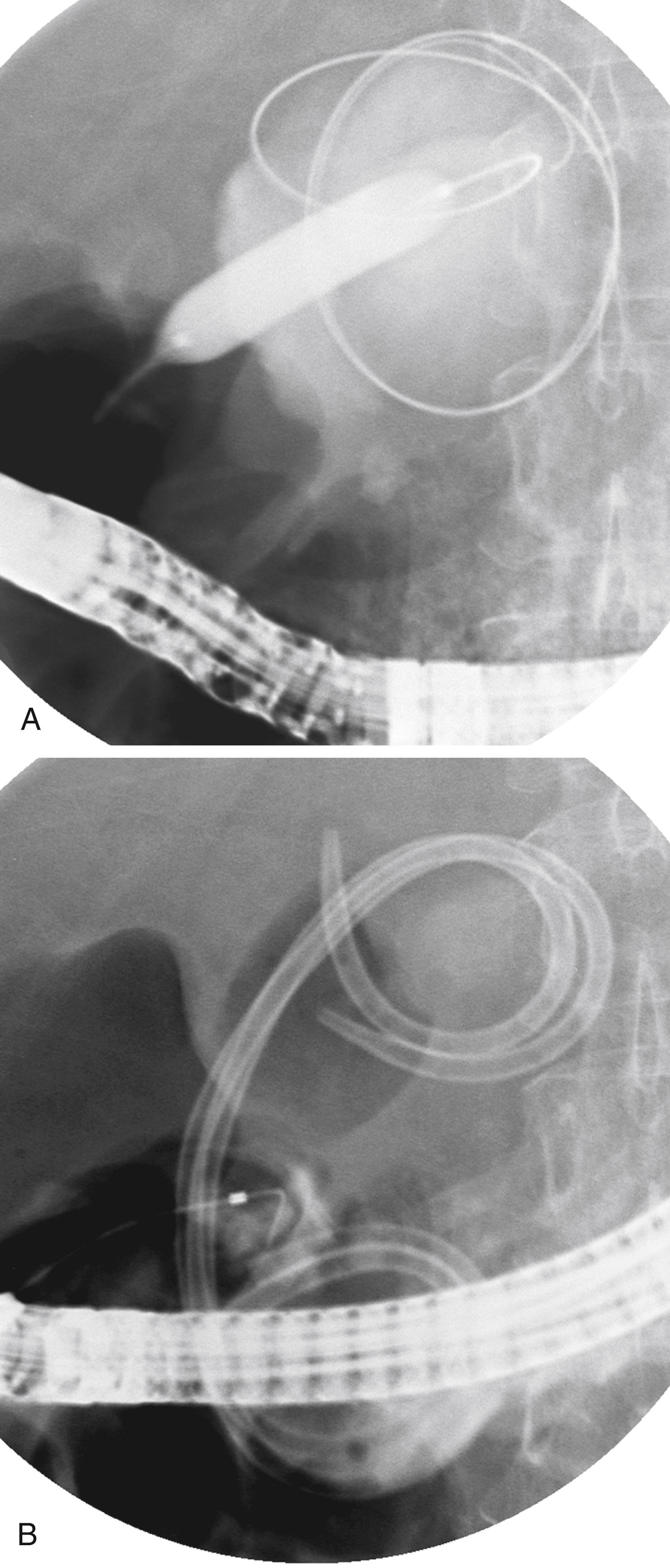
If the pseudocyst communicates with the main pancreatic duct, placement of a pancreatic duct stent with or without pancreatic sphincterotomy is effective, especially for smaller pseudocysts (<5 to 6 cm) that are not otherwise approachable transmurally. , The proximal end of the stent (toward the pancreatic tail) may directly enter the pseudocyst, bridge the area of leak into the pancreatic duct upstream from the leak, or lie completely downstream to the leak. Bridging the leak is the preferred approach because it restores ductal continuity and appears to be more effective ( Fig. 61.2 ). , Transpapillary drainage avoids bleeding or perforation that may occur with transmural drainage. However, pancreatic stents may induce scarring of the main pancreatic duct in patients with a normal duct.
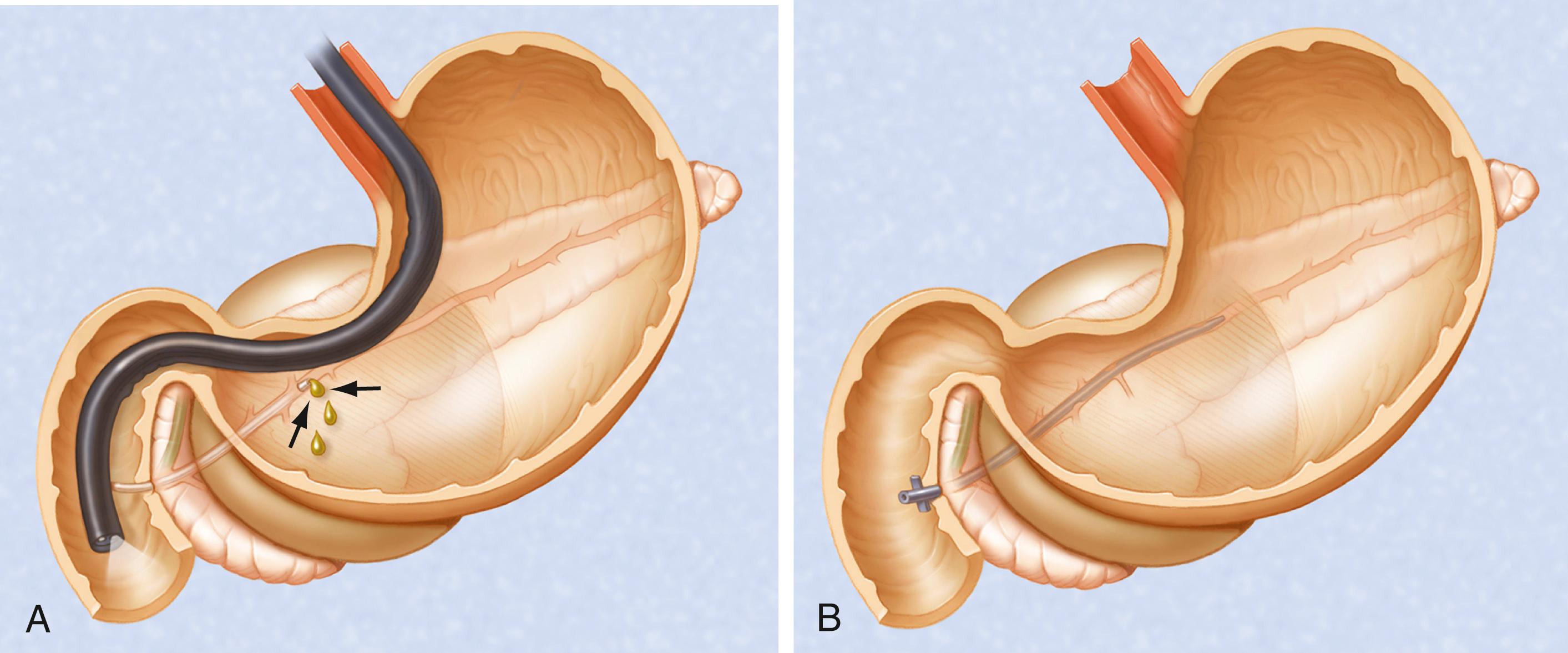
There is no standardized approach to transmural pseudocyst drainage. Transmural drainage is performed by entering the collection using a needle without electrocautery or using an electrocautery device (e.g., needle knife, cystotome, cautery-enhanced lumen-apposing metal stent [LAMS]) EUS-guided drainage is preferred over non-EUS-guided drainage to prevent adverse events such as bleeding and perforation. Although the superiority of EUS-guided versus non–EUS-guided drainage has not been clearly demonstrated, data support its routine use during transmural drainage, especially when non–EUS-guided drainage fails. EUS-guided entry is successful in more than 95% of patients and has low adverse event rates. Traditionally, once the pseudocyst cavity is successfully entered, the transmural tract is balloon dilated to 8 to 10 mm in diameter to allow placement of 1 or 2 double pigtail 10-French stents ( Fig. 61.3 ). Covered self-expandable stents have been used instead of, and in addition to, plastic stents. A novel LAMS has been recently developed to mitigate many of the limitations of traditional drainage techniques. Two FDA-approved LAMS stent delivery systems are available for the management of pancreatic fluid collections, one which requires placement via traditional drainage techniques (i.e., step 1-puncture, step 2-guidewire placement, step 3-tract dilation, step 4-stent deployment) and the other which is fitted with an electrocautery tip allowing simultaneous puncture and tract dilation, followed by stent deployment, without the need of guidewire placement in select circumstances.
Following uncomplicated attempted endoscopic drainage, a follow-up CT is obtained 4 to 6 weeks after the procedure. All internal stents are endoscopically removed after documented radiographic pseudocyst resolution. Success rates, recurrence rates, and adverse event rates of endoscopic drainage of pancreatic pseudocysts are variable, likely because many published reports are heterogeneous, including patients with both acute and chronic pseudocysts, as well as “pancreatic abscesses.” In addition, some patients underwent transpapillary drainage, others underwent transmural drainage, and some underwent both interventions. Nonetheless, cumulatively, successful drainage is achieved in approximately 75% to 90%, with adverse event rates of about 5% to 10% and pseudocyst recurrence rates of 5% to 20%. ,
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here