Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Pediatric electrophysiology has evolved into a fully recognized subspecialty within the field of pediatric cardiology, and recent growth has led to the continued expansion of this subsection. The aging adult population with congenital cardiac disease, growing in size and in complexity, is increasingly burdened with arrhythmias. Arrhythmic sudden death conditions and the evaluation of victims and families at risk for sudden death have pointed to the need for the electrophysiologist to have an understanding of clinical and molecular genetics and to have advanced the path toward personalized medicine and multidisciplinary care. Advanced mapping techniques allow catheter ablation procedures and arrhythmia cures with little or no fluoroscopic exposure. Pacemakers to improve ventricular function, entirely subcutaneous implantable cardioverter defibrillators (ICDs), devices compatible with magnetic resonance imaging (MRI), and even leadless pacemakers are expanding the ways in which we can approach our unique population more safely and effectively. Finally, registries are in place that will allow us to examine successes and avoid failures, assess risk, and plan for the future; these may help to fill the gap in our lack of large evidence-based studies. We have had a unique overlap with adult electrophysiology, with overlapping disease substrates and physiology allowing us to gain from their larger patient numbers and multicenter trials. However, we have embraced and fostered some of the diseases and technology before or at least simultaneously with our colleagues who deal with adults. We deal with a unique population, patients who are smaller; their complex and diverse anatomy requires unique approaches, hardware, and thinking outside of the box. This chapter provides an overview of the field that is applicable to general cardiologists, trainees, and advanced practitioners.
Bradycardia is defined as a heart rate below the normal range for age that may result from intrinsic injury to the sinus node, atrioventricular (AV) node, or His-Purkinje conduction system or secondary to extrinsic factors acting on native conduction. The decision to intervene for bradycardia often relates to its impact on systemic perfusion, exacerbation of heart failure, or the possibility of pause-dependent tachyarrhythmias. Symptoms of bradycardia—such as syncope, dizziness, chest pain, shortness of breath, and fatigue—especially in younger children, are not always readily apparent. The differential diagnosis of symptomatic bradycardia is broad ( Box 22.1 ), and aside from structural congenital heart defects and cardiomyopathies, consideration should be given to endocrinopathies, infections, drug ingestion, breath-holding spells, apnea, anorexia, and central nervous system disorders. In addition, various genetic abnormalities (i.e., NKX2.5, SCN5A, SCN1B and TRPM4 ) have been implicated in the pathogenesis of sinus node dysfunction or progressive cardiac conduction defects. A simplistic yet clinically relevant approach to the patient with bradycardia from a conduction vantage point begins with abnormalities in the sinus node and progresses through block within the AV node/His-Purkinje system.
Congenital heart disease
Heart block
Endocarditis
Cardiomyopathy
Channelopathies
Heart transplant
Hypoxia
Hypothermia
Trauma (increased intracranial pressure)
Increased vagal tone
Myotonic muscular dystrophy
Autonomic dysfunction
Immature breathing (premature infant)
Gastroesophageal reflux (infant)
Acidosis
Hyperkalemia
Hypokalemia
Malnutrition
Anorexia
Hypoglycemia
Systemic lupus erythematosus
Rheumatoid arthritis
Digoxin
β-blockers
Calcium-channel blockers
Clonidine
Lithium
Lyme disease
Chagas disease
Acute rheumatic fever
The sinus node is located at the cavoatrial junction between the crista terminalis and the sulcus terminalis on the epicardial surface. The sinus node comprises a complex and heterogeneous arrangement of ion channels including the I f (“funny hyperpolarization-activated inward current” and the L- and T-type calcium currents) responsible for a self-propagating action potential ( ). Sinus node abnormalities may be secondary to a slower than normal sinus rate (sinus bradycardia), sinus arrest, sinus pause, sinuatrial block, loss of a normal P-wave axis with default to an ectopic atrial rhythm (most often low right atrial), or complete loss of atrial activity and default to a junctional rhythm (typically narrow QRS complex). Sinus pauses or sinus arrest are almost always related to previous surgeries in the region of the sinus node or its blood supply, drugs, enhanced vagatonia, metabolic derangements, or hypoxemia.
Sinus node dysfunction is increasingly recognized as a late complication following congenital heart surgery either from scarring of the sinus node or injury to the sinus nodal artery or its autonomic inputs. In addition, certain anatomic substrates, such as left atrial isomerism (heterotaxy), may have an absent sinus node as part of their anatomic constellations.
Patients with sinus node dysfunction are frequently asymptomatic; however, that does not reliably translate into the fact that those individuals would not benefit from atrial pacing. Patients with sinus node dysfunction may exhibit chronotropic incompetence and have symptoms of exertional fatigue. Each of these bradycardias may also occur as part of the bradycardia-tachycardia syndrome with concomitant atrial reentrant arrhythmias.
The primary criterion for antibradycardia pacing is the presence of symptoms at rest or with exercise. The relative heart rate labeling someone as bradycardic is age dependent. For example, a resting heart rate of 45 beats/min may be a normal heart rate in a fit adolescent, but in a neonate would invoke significant concerns. Symptomatic bradycardia is defined as a documented bradyarrhythmia that is directly responsible for the clinical manifestations of syncope or near syncope, transient dizziness, light-headedness, or periods of confusion resulting from cerebral hypoperfusion. Fatigue, exercise intolerance, and heart failure may also result from bradycardia.
Although a resting electrocardiogram (ECG) will give a snapshot assessment of the sinus node, 24-hour ambulatory monitors are better measures of the sinus node and provide low, average, and high heart rates. Guidelines for the Holter diagnosis of sinus bradycardia have been proposed; for neonates and infants, they are less than 60 beats/min sleeping and less than 80 beats/min while awake. However, there is little distinction between the low heart rate at rest and the low heart rate while awake. The relevant rate for children aged 1 to 6 years is less than 60 beats/min; for those aged 7 to 11 years, less than 45 beats/min; for adolescents and young adults, less than 40 beats/min; and in highly trained athletes, less than 30 beats/min. None of these numbers are based on children and adolescents with congenital heart disease. Correlation of symptoms with periods of bradycardia should be sought before a patient receives a permanent pacemaker. Likewise, elite athletes may have low resting heart rates, and this level of physiologic sinus bradycardia should not be confused with a pathologic mechanism.
Certain channelopathies (i.e., long-QT syndrome [LQTS] may manifest as bradycardia; see later). Patients with congenital heart disease may have significant hemodynamic perturbations due to the loss of AV synchrony even with acceptable normal junctional rates and may benefit from atrial pacing. This has been well demonstrated in single-ventricle patients after the Fontan procedure and in adults who underwent an atrial baffle procedure for transposition of the great arteries. Rychik showed that in patients with a univentricular circulation following a superior cavopulmonary connection, junctional rhythm results in early systolic flow reversal in the pulmonary veins and reduces effective single-ventricular cardiac output.
In the healthy newborn the heart rate ranges from 120 to 160 beats/min, but the range exists from 90 to 230 beats/min. Transient bradycardia is relatively common in newborns in the form of sinus bradycardia, sinus arrest, and junctional escape rhythm; it may relate to stressful labor or delivery and typically resolves within 48 to 72 hours. Potential causes of transient bradycardia in the neonate relate to sedation given to the mother that crosses the placenta to the baby as well as jaundice, hypothyroidism, increased intracranial pressure, apnea, and increased vagal tone. Pauses of greater than 1 second are not infrequently observed in neonates and generally do not require anything beyond observation. Pauses greater than 2 seconds are less common and should be considered abnormal.
Bradycardia in the preterm and term neonate can also be a result of blocked premature atrial contractions (PACs). PACs are relatively common (0.7% to 14%) in healthy newborns. As in older children, PACs may be conducted, blocked, or conducted with aberrancy. In an otherwise well-appearing acyanotic neonate with PACs, there is near-zero morbidity, and they will persist in fewer than 5% of those beyond 12 weeks of age. Premature atrial beats may appear in patterns of bigeminy, trigeminy, or quadrigeminy but still have a relatively benign prognosis. It is important that nonconducted PACs are not confused with complete AV block. Careful observation of P-wave morphology and the P-wave axis may be helpful in confirming atrial and AV nodal escape beats in neonates.
Episodes of apnea in term and preterm infants may precede transient bradycardia. Longitudinal polysomnographic studies have reported these transient episodes of bradycardia to be a normal neonatal reflex. Premature ventricular beats have been reported in 0.2% of healthy newborns; however, an echocardiogram should likely be performed to rule out structural heart defects or an associated cardiomyopathy. Rare, isolated premature ventricular contractions in an otherwise healthy newborn with a structurally normal heart are generally considered to have a similarly benign natural history to their premature atrial counterparts. Increasing the sinus rate typically abolishes both the atrial and ventricular ectopy.
First-degree AV block is PR prolongation beyond the upper limit of normal for age. Normative pediatric ECG data have been published. First-degree AV block may be observed in patients with dilated atria, where the impulse takes longer to propagate through the atrial tissue. This is frequently seen in patients with a functionally univentricular heart following an atriopulmonary Fontan procedure. First-degree AV block is one of the minor criteria used in the affirmation of rheumatic heart disease. Second-degree AV block can be subdivided into Mobitz type I (Wenckebach) and Mobitz II second-degree block. Mobitz I AV block is typically associated with a narrow QRS complex and is typically considered benign. In contradistinction, Mobitz II AV block is a rare pattern with less reliable escape rhythms and is always infranodal.
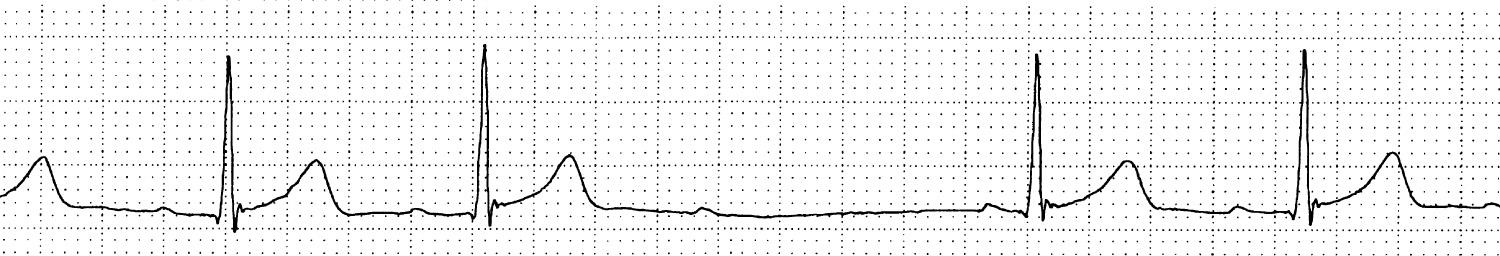
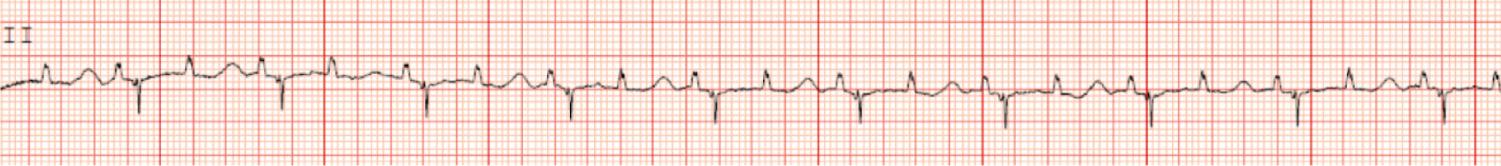
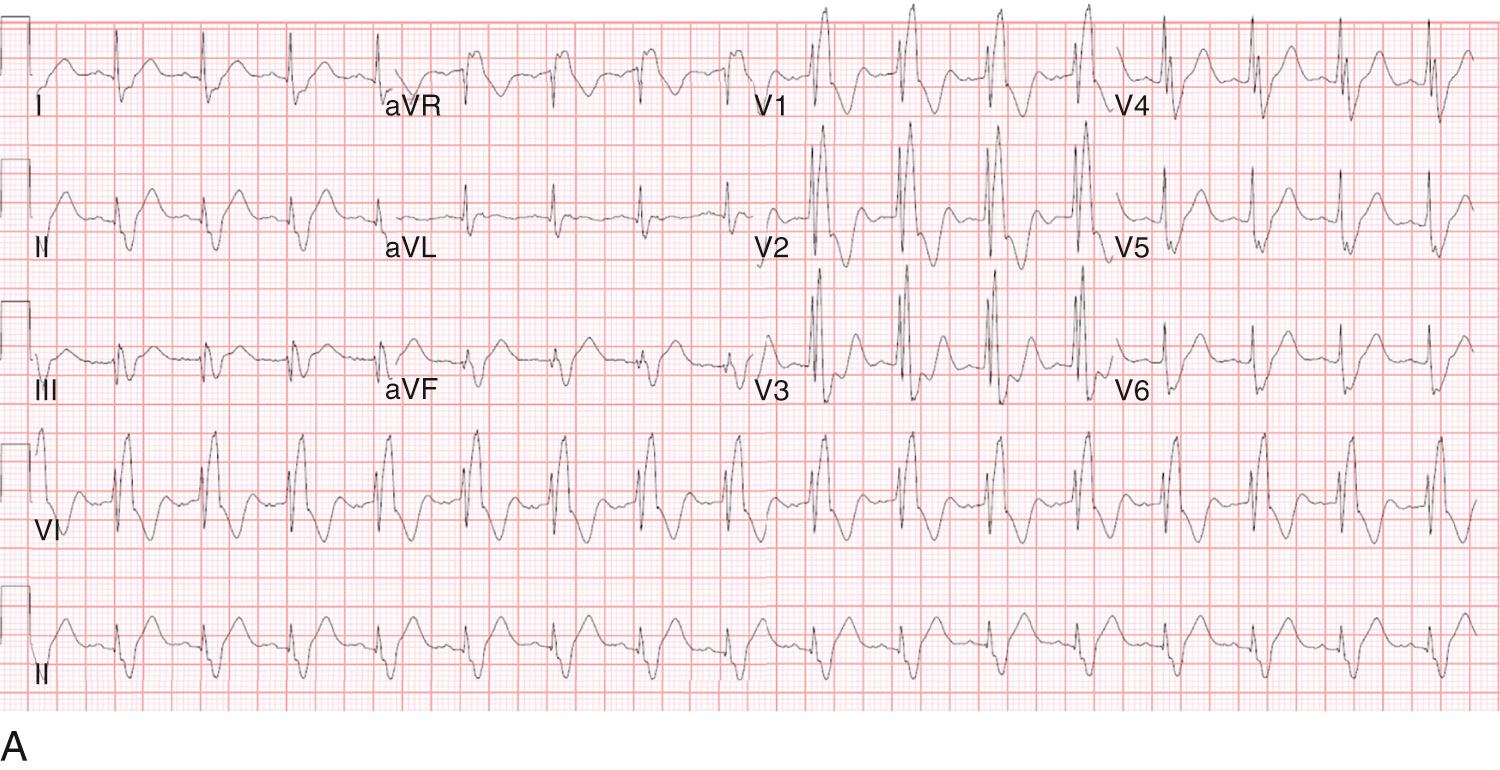
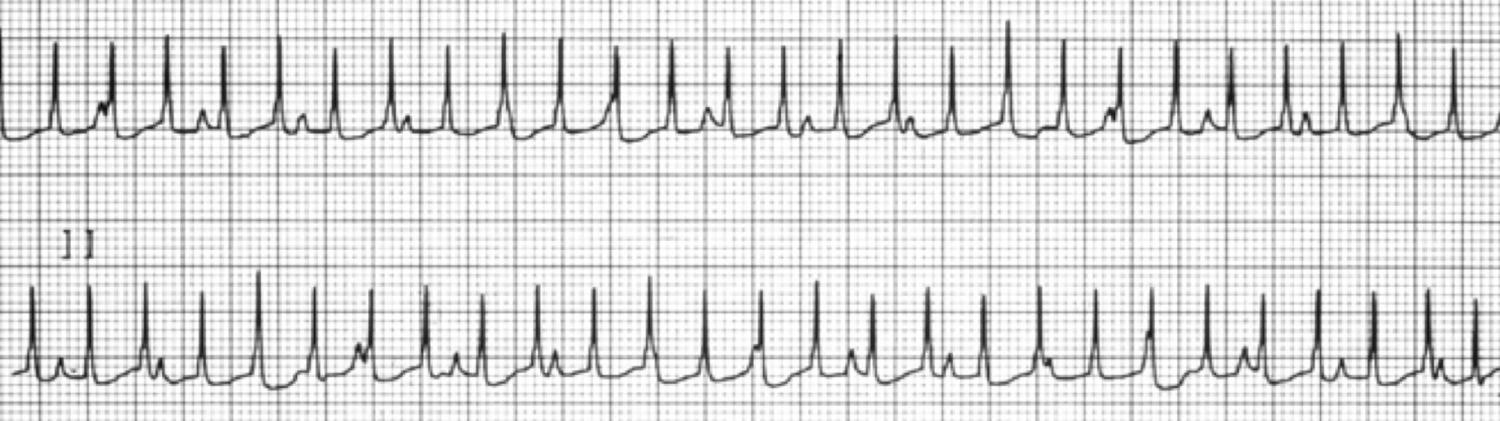
Mobitz type I AV block ( Fig. 22.1 ) is characterized by progressive PR prolongation before a single nonconducted P wave and is typically associated with a narrow QRS complex unless the patient has an underlying bundle-branch block. Clues to the diagnosis include the observation that the postblock PR interval is shorter than the preblock PR interval as well as the recognition of what has been described as grouped beating. Mobitz I AV block is frequently observed in very healthy adolescents with high vagal tone in the early morning hours of sleep. In contrast, type II second-degree AV block is characterized by fixed PR intervals before and after blocked beats and is usually associated with a wide QRS. Caution should be exercised before labeling someone as having type II second-degree AV ( Fig. 22.2 ) block, as the natural history and management of Mobitz type I ( Fig. 22.3 ) and Mobitz type II AV block are different. It is often helpful to obtain a long rhythm strip to accurately measure the PR intervals over a period of time. Generally it would be uncommon to see both Mobitz I and Mobitz II in the same patient, as one relates to block above the node and one below the node. It is important to pay close attention to a 2 : 1 pattern of AV block whereby neither Mobitz I nor Mobitz II may be affirmed, although a wide QRS in the setting of 2 : 1 AV block suggests Mobitz II AV block.
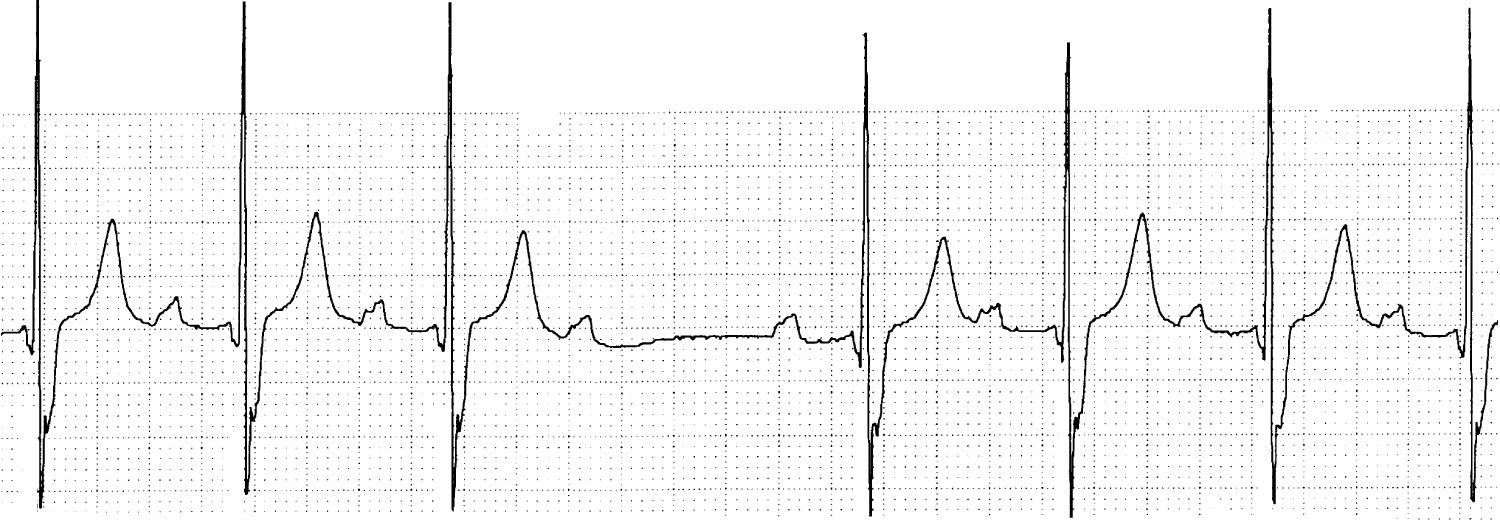
Advanced second-degree AV block refers to lack of conduction of two or more consecutive P waves but with some conducted beats indicating some preservation of AV conduction. Third-degree AV block (complete heart block) refers to complete dissociation of the atrial and ventricular conduction ( Fig. 22.4 ). Although patients with congenital complete AV block typically have a regular slow escape rhythm, the same may not hold true for third-degree AV block following cardiac surgery, where the escape rhythm may not be as reliable. In patients with AV dissociation secondary to third-degree block the atrial rate (PP) tends to be faster than the junctional rate (RR) (PP > RR). This is generally in contradistinction to junctional ectopic tachycardia (JET), where AV dissociation exists but the ventricular rate is faster than the atrial rate (RR > PP). In patients with AV dissociation suspected to be secondary to JET, atrial pacing (AAI) faster than the junctional rate reestablishes AV synchrony, whereas the same would not hold true for complete AV block.
The occurrence of 2 : 1 AV block is a form of second-degree AV nodal block whereby every other P wave is not conducted through the AV node and into the ventricles. Thus a QRS complex does not follow every other P wave. This type of AV block can result from either second-degree type I or type II AV block. As a general rule, if the PR interval of the conducted beat is prolonged and the QRS complex is narrow, then it is most likely second-degree Mobitz type I block. Alternatively, if the PR interval is normal and the QRS duration is prolonged, then it is most likely second-degree AV block type II.
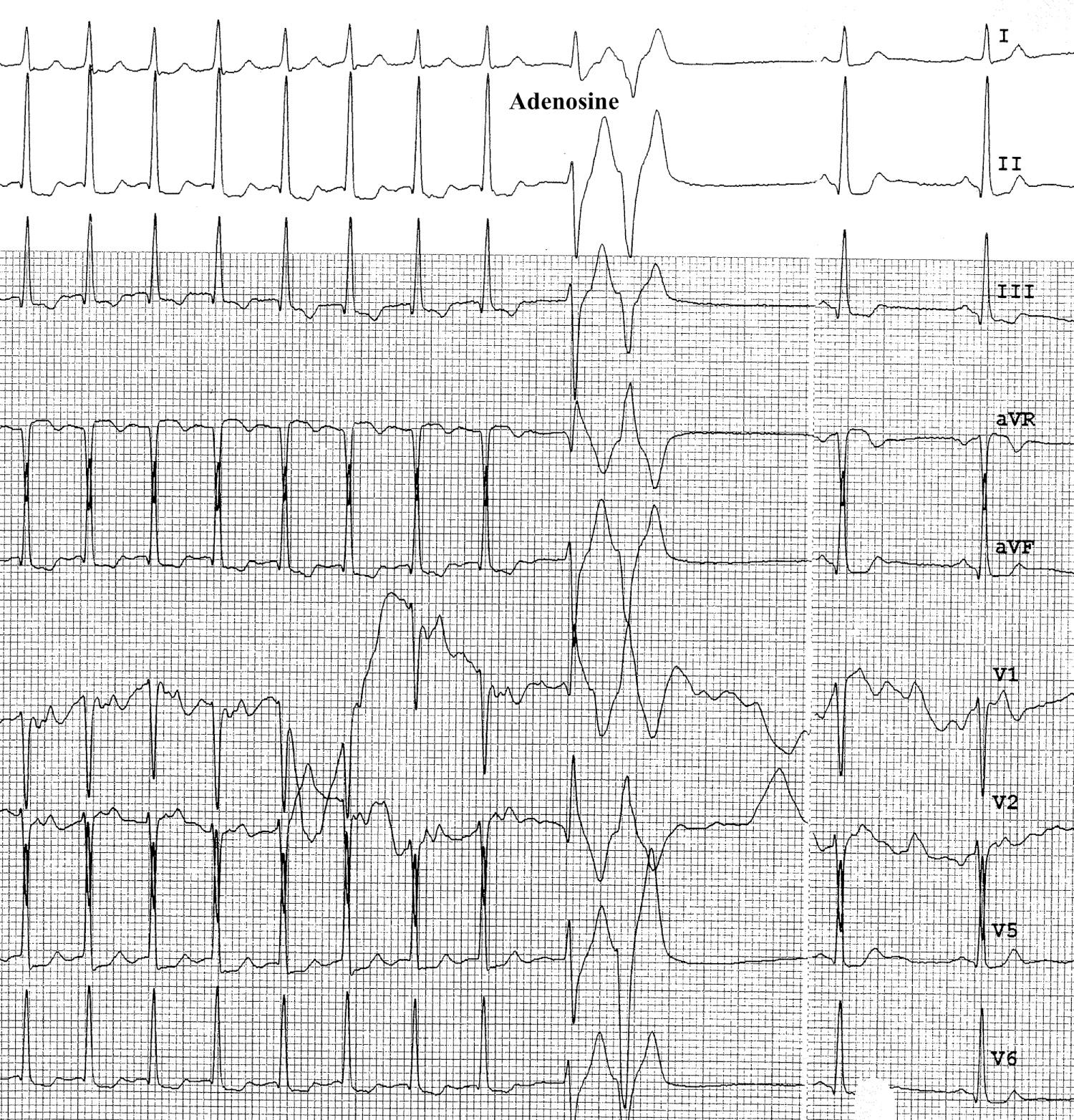
This distinction is critical, as the former tends to have a very benign course and the latter requires ongoing follow-up, as AV block may progress and the nature and rate of the escape rhythm are unpredictable. The pathophysiology of the two variants of AV block is quite disparate, with Mobitz type I block being a disease of the AV node and subject to sympathetic and parasympathetic inputs. Type II second-degree AV block is infranodal and relates to perturbations in the His-Purkinje conduction axis; it is not subject to the same level of parasympathetic and sympathetic inputs. Various maneuvers (atropine, adenosine, exercise) can distinguish between the two forms of 2 : 1 AV block based on these principles.
In 1982, Michaëlsson and Engle published the well-known natural history study of congenital complete AV block, with a reported incidence between 1 in 15,000 and 1 in 23,000 and a familial incidence of 2.3%. However, more recent evidence out of Finland, likely a result of improved perinatal monitoring and increased successful deliveries of mothers with connective tissues disorders, revealed an incidence closer to 1 in 11,000. Of the patients diagnosed with congenital complete AV block, approximately 25% to 35% have associated structural heart defects. The pathophysiology of congenital complete AV block in structural heart disease may relate to a lack of communication between the AV node and the penetrating bundle. There may also be a lack of communication between the atria and AV node such that the AV node may be totally absent, or there may be an aberrant conduction system such that the AV node and distal conduction tissue may be formed from anterior endocardial tissue. In the original natural history study of congenital complete AV block, mortality was 15% in infants without congenital heart disease compared with 43% if congenital heart disease was present. This early observation partly explains the difference in antibradycardia pacing recommendations between the two cohorts.
1718 Gerbezius, first to report a slow pulse in an infant.
1827 William Stokes (Irish physician), described syncope associated with bradycardia.
1846 Robert Adams (Irish physician), described syncope with bradycardia (Stokes-Adams attacks).
1901 Morquio reported a familial condition describing five siblings with a permanently slow pulse and syncope, all of whom died suddenly.
1908 Van Heusel first described the electrocardiographic findings of complete atrioventricular block.
1913 Anatomist Mockenberg described the anteriorly positioned atrioventricular node in atrioventricular discordant hearts.
1929 Yater presumptively diagnosed complete atrioventricular block in utero.
1966 Hull presented the first report of maternal congenital atrioventricular block in association with maternal connective tissue disease.
1977 McCue was the first to demonstrate the association of systemic lupus erythematosus and congenital complete atrioventricular block.
1977 Chameides supported the association between maternal systemic lupus erythematosus and congenital heart block in six infants.
The pathogenesis of congenital complete AV block related to maternal autoimmune conditions is incompletely understood but is believed to be a result of SSA (Ro) and SSB (La) immunoglobulins crossing the placenta between 12 and 23 weeks of gestation and interacting with antigens on AV node, fibrous body, and annulus. Despite what seems to be a simple pathophysiologic explanation, only 5% of fetuses exposed to maternal immunoglobulins develop congenital complete AV block. Part of this observation may relate to varying amounts of anti-Ro and anti-La that cross the placenta as well as potential differences related to ethnicity. Significant predictors of death appear to be low ventricular rate (<55 beats/min), hydrops, endocardial fibroelastosis, and right ventricular (RV) endocardial wall thickness. The most sensitive predictors of increased risk of congenital complete AV block are having a child with previous AV block, high anti-Ro/La titer, or the presence of HLA-DR3 titers. The indications for pacemaker implantation are discussed further on.
The primary goal of antibradycardia pacing for congenital complete AV block is to prevent syncope, Stokes-Adams attacks, and sudden cardiac death. Patients with symptoms of heart failure have a class I indication for pacemaker implantation. However, not all children display classic heart failure symptoms, and the clinician caring for the younger child should be aware of atypical symptoms such as long naps and nightmares as well as exertional fatigue compared with siblings around the same age. Predictors of symptoms include atrial enlargement, QT prolongation, and cardiomegaly. Additional class I indications include a wide QRS escape rhythm, complex ventricular ectopy, or ventricular dysfunction. Congenital third-degree AV block in an infant with a ventricular rate less than 50 to 55 beats/min or in association with congenital heart disease and a ventricular rate less than 70 beats/min is considered a class I recommendation for permanent pacing. If such rate criteria are met, it is standard practice to place a pacing system using epicardial leads (preferably bipolar) along with an abdominally placed generator. Newborns can be paced VVI at rates generally between 70 and 90 beats/min; however, if easily achievable, an atrial and ventricular lead dual-chamber system should be placed to maintain AV synchrony. Whereas pacemaker syndrome is unusual in small children, it remains preferable to have an atrial and ventricular lead unless technical challenges limit such an application. A recent study by Janousek and colleagues has shown that left ventricular (LV) pacing in patients with AV block and a structurally normal heart has had a major impact on LV mechanical synchrony and efficiency; it has the potential to reduce pacing-induced ventricular dysfunction. A novel fetal micropacemaker has recently been invented by Vest and colleagues and is in early clinical trials for fetuses with serologically positive congenital complete heart block and associated hydrops. It is unclear whether early pacing can alter the natural history in this exceedingly high-risk cohort.
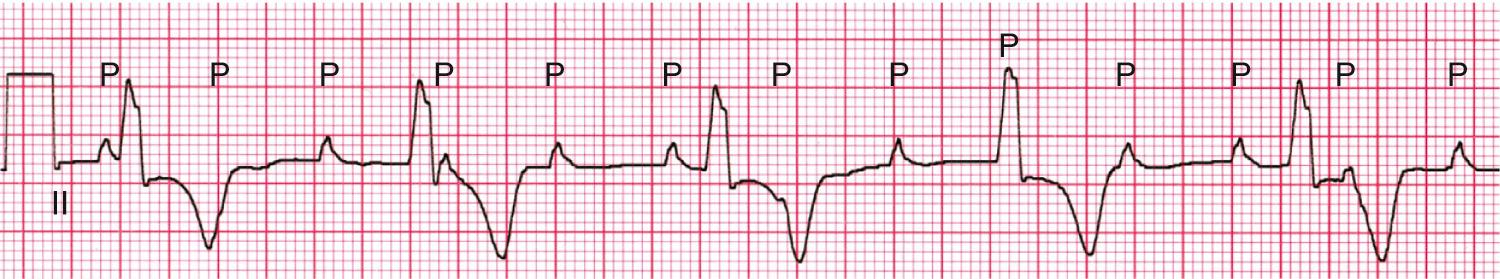
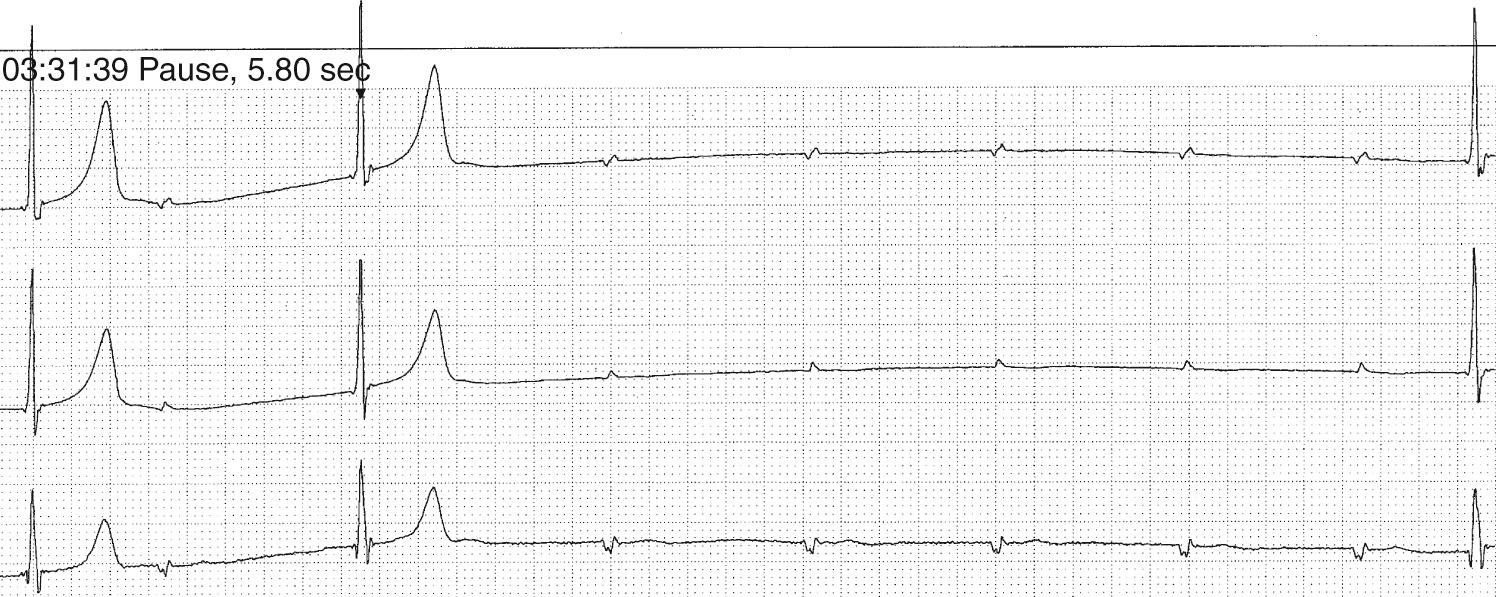
Pacing recommendations for those with congenital complete AV block beyond the first year of life are a mean heart rate below 50 beats/min (class IIA) or pauses of at least 3 seconds while awake or 5 seconds while asleep ( Fig. 22.5 ). One concern for children with isolated congenital complete AV block is the development of a dilated cardiomyopathy. This is reported in 6% to 11% of patients, even when pacing suggestive of a pacing-induced ventricular dyssynchrony is a contributor to the development of ventricular dysfunction. Unfortunately, pacing-induced dyssynchrony cannot explain all causes of a dilated cardiomyopathy, as reports of a myopathic process occurred in relation to some children who were not paced. There are early data that pacing the left ventricle (apical) at a young age may prevent the development of pacing-induced dyssynchrony and dilated cardiomyopathy. Longer-term follow-up of such patients will be required to see whether, in this rare condition of congenital complete heart block, LV pacing will abolish the even rarer development of a dilated cardiomyopathy. However, such a simplistic explanation cannot address the presence of a dilated cardiomyopathy in all such patients.
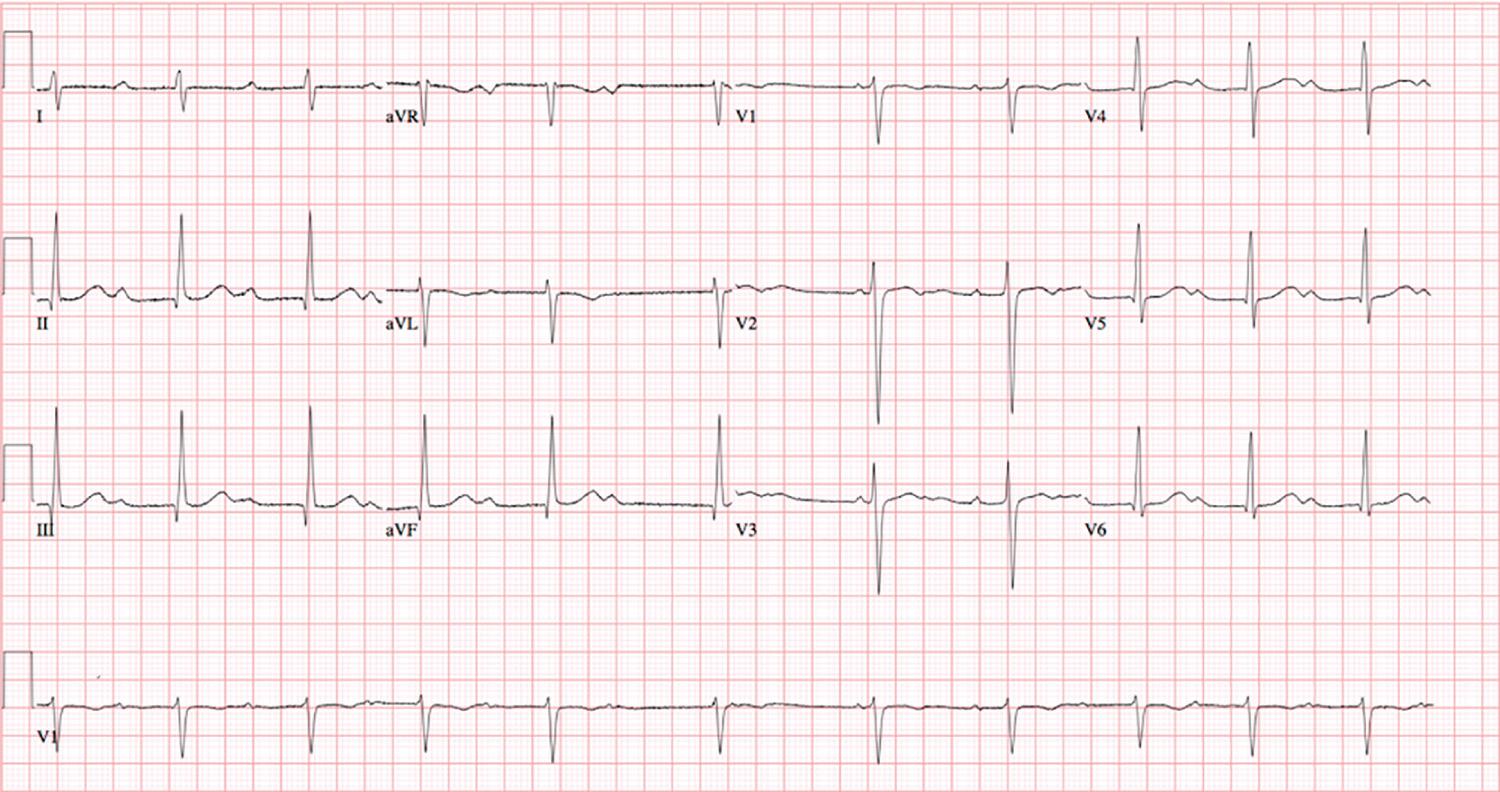
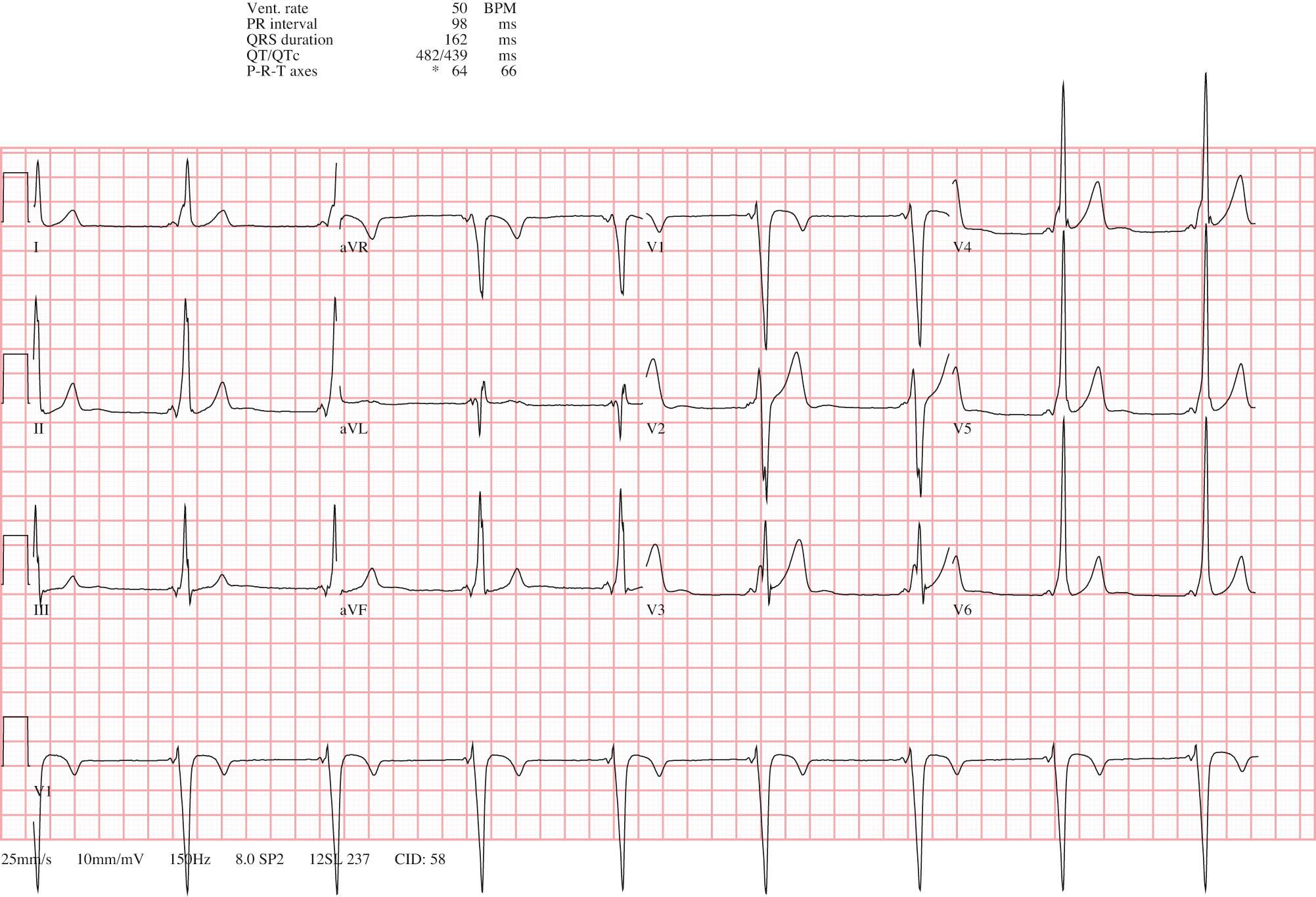
High-grade functional AV block (≥2 : 1 AV block) with concomitant QT prolongation ( Fig. 22.6 ) is a class IIA indication for a permanent pacemaker and relates to extreme prolongation of ventricular refractoriness. Whereas prolonged QT intervals can be seen with AV block, concomitant torsades de pointes (TdP) is rare. However, the presence of TdP in the setting of AV block may be a marker of underlying repolarization reserve, and genetic variants of LQTS have been identified in 36% of this high-risk cohort. Michaëlsson has recommended that all patients with congenital complete AV block be paced by the time they reach adolescence because of a significant risk of syncope or sudden death at any time thereafter, even in the absence of poor prognostic signs. Although this recommendation is class IIB, it is increasingly accepted.
Patients with significant and persistent bradycardia and sinus node or AV block who do not undergo antibradycardia pacing require ongoing follow-up with serial ECGs, Holter monitors, and echocardiograms. The frequency of such testing should be based on the clinical status of the patient after discussions with the medical team caring for him or her. There are few data on the use of serial echocardiograms in establishing definitive recommendations for a pacemaker, but it is generally helpful to assess ventricular size and function, the degree of AV valve regurgitation, and atrial size.
Postoperative AV block occurs in 1% to 3% of cardiac operations, with the greatest risk occurring following repair of AV canal defects, tetralogy of Fallot, and ventricular septal defects as well as in hearts with AV discordance (L-looped) and heterotaxy syndrome. Although transient AV block has been reported in nearly 7% of surgical cases, resolution may occur; if so, it will do so in 97% by 10 days following surgery. As such, the risk of sudden cardiac death following surgical advanced second- or third-degree AV block that is not expected to resolve or persists for at least 7 days after cardiac surgery is a class I indication for pacemaker implantation. In addition, junctional JET may be a concomitant observation in patients with complete AV block. Patients in whom postoperative advanced second- or third-degree AV block has resolved and in whom conduction returns to normal have a good prognosis, and pacing is not indicated. If there is incomplete recovery with new residual bifascicular block (complete right-bundle-branch block [RBBB] and left axis deviation), uncertainty remains (class IIB in the American College of Cardiology/American Heart Association recommendations and class IIa in the European Society of Cardiology). Postoperative AV interval determination may help to assess the risk of late-onset AV block in patients with residual conduction disorders (bifascicular block and PR prolongation); however, this is not always practical. If epicardial wires are available and there is concern about the stability of the residual conduction abnormality, it may be worth evaluating the AV node's Wenkebach cycle length. Discussions with the cardiac intensive care unit and surgical teams regarding leaving epicardial wires in place to assess AV nodal conduction should occur. Long-term instability of the conduction system has been postulated in patients with transient postoperative heart block and is thought to contribute to late sudden death in some patients. Thus patients should be monitored for any recurrence of heart block or evidence of arrhythmia with regular ambulatory monitors.
Syncope (transient loss of consciousness) is a result of cerebral hypoperfusion and is most commonly a result of autonomic nervous system dysfunction. Neurally mediated (or vasovagal) syncope results in loss of consciousness typically after being in an upright posture (for more than 30 seconds) or with emotional stress or pain, often with associated symptoms of vision changes, warmth, diaphoresis, and nausea. Hypotension and bradycardia may exist and patients are often profoundly fatigued following the event. The frequency of syncope peaks at 11 years of age, with a lesser peak between 6 and 18 months of age in the form of pallid breath-holding events. Guidelines for the evaluation and treatment for vasovagal syncope and postural orthostatic hypotension syndrome were recently published by the American Heart Association, American College of Cardiology, and Heart Rhythm Society.
Cardiologists are frequently asked to evaluate a child with syncope in both the acute and outpatient settings. Each evaluation should begin with a detailed personal history surrounding the event from the individual as well as from any witnesses, a thorough physical examination, and a carefully constructed family history concerning unexplained syncope, seizures, or sudden cardiac death in the young. Although current guidelines support an initial routine ECG examination in patients presenting with syncope, the yield in those with clinically suspected vasovagal syncope is low, and efforts should be made to reduce false positives. It is of utmost importance to be aware of any potential red flags that warrant additional testing ( Table 22.1 ). In a retrospective study of 60 patients with exertional syncope, 53% were identified as having a cardiac etiology. Syncope that occurs during exertion should be differentiated from postexertional syncope, which tends to be more aligned with neutrally mediated syncope. A pediatric cardiologist or adult congenital heart disease specialist should urgently evaluate patients with syncope in the setting of repaired or palliated congenital heart disease. Detailed evaluation for the possibility of bradyarrhythmias or tachyarrhythmias should be sought in this high-risk cohort. The Heart Rhythm Society along with pediatric and adult specialists from North America and Europe recently published guidelines on the evaluation and management of the adult patient with congenital heart disease and syncope.
| History and Physical Findings | Differential Diagnosis |
|---|---|
| Midexertional syncope | Cardiomyopathy, WPW, LQTS, CPVT |
| Syncope with loud noise/startle | LQTS |
| Syncope with chest pain | Hypertrophic cardiomyopathy, anomalous coronary |
| Syncope with palpitations | SVT, WPW, CPVT, LQTS |
| Family history sudden cardiac death | Any channelopathy or cardiomyopathy |
| Syncope with fever | Brugada syndrome |
| Syncope while swimming | LQTS, CPVT |
| Abnormal cardiac examination | Cardiomyopathy, congenital heart disease |
| Abnormal electrocardiogram | |
| Absence of a prodrome | |
| Sternotomy or thoracotomy |
A number of tools are available for further evaluating unexplained syncope including 24-hour ambulatory monitors, 30-day event recorders or implantable loop recorders. Implantable loop recorders may be of particular benefit in guiding the management of patients with suspected or confirmed inherited arrhythmia syndromes. Implantable loop recorders can be placed subcutaneously in most adolescents with local anesthesia in approximately 10 minutes. Patients with exertional syncope should be considered for an exercise stress test to potentially recapitulate the clinical history. In patients too young to exercise, a running 12-lead ECG during an isoproterenol infusion in a controlled environment may be a reasonable test to consider. The treatment of the patient with syncope should be individualized and tailored to the condition identified.
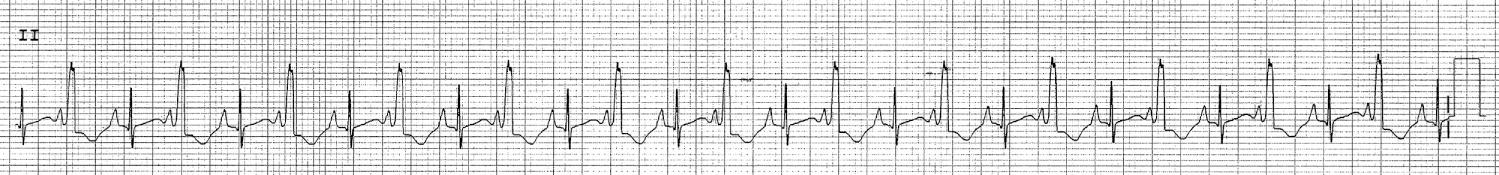
Supraventricular tachycardia (SVT) represents one of the most commonly encountered significant cardiac conditions in childhood, occurring in 1 in 250 to 1 in 1000 children, and is the most common sustained arrhythmia from intrauterine life onward ( Fig. 22.7 ). The mechanism of SVT is age related, with atrioventricular reentry tachycardia (AVRT) representing the most common tachycardia substrate in the fetus, infants, and in young children, with atrioventricular node reentry tachycardia (AVNRT) becoming more common in older children and young adults.
The presentation and symptoms of tachycardia are age-dependent. Fetal tachycardia can be noted incidentally during routine obstetric evaluation or can be associated with hydrops fetalis, the fetal manifestation of heart failure. Newborn infants can present with tachycardia that is noted incidentally; however, it is more often present with unexplained tachypnea, poor feeding, and other manifestations of heart failure in the newborn. Older children usually complain of palpitations and thus are usually seen before heart failure ensues.
Clinically important clues that suggest SVT include the abrupt onset of palpitations and tachycardia with or after exercise. Parents often report noting pounding in the child's neck and chest as well as pallor; in infants they note poor feeding and irritability. Termination of tachycardia with vagal maneuvers is a clue to diagnosis, indicating a tachycardia that uses the AV node or specific types of ventricular tachycardia (VT) described later in this chapter. Incessant arrhythmias may go unrecognized for months or even years until heart failure symptoms ensue. This arrhythmia-induced cardiomyopathy represents a reversible cause of heart failure in children and adolescents and should be a consideration at the evaluation of every patient with new-onset cardiomyopathy. Some arrhythmias present with hemodynamic collapse and should raise concern for complex or polymorphic ventricular arrhythmias, arrhythmias in the setting of channelopathic conditions, heart disease, or Wolff-Parkinson-White syndrome.
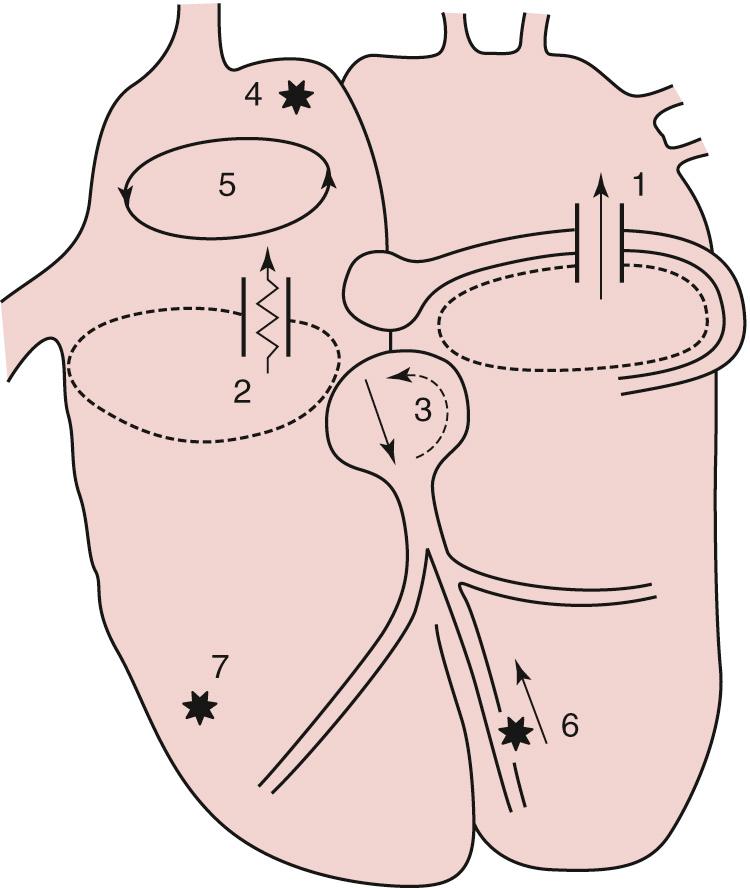
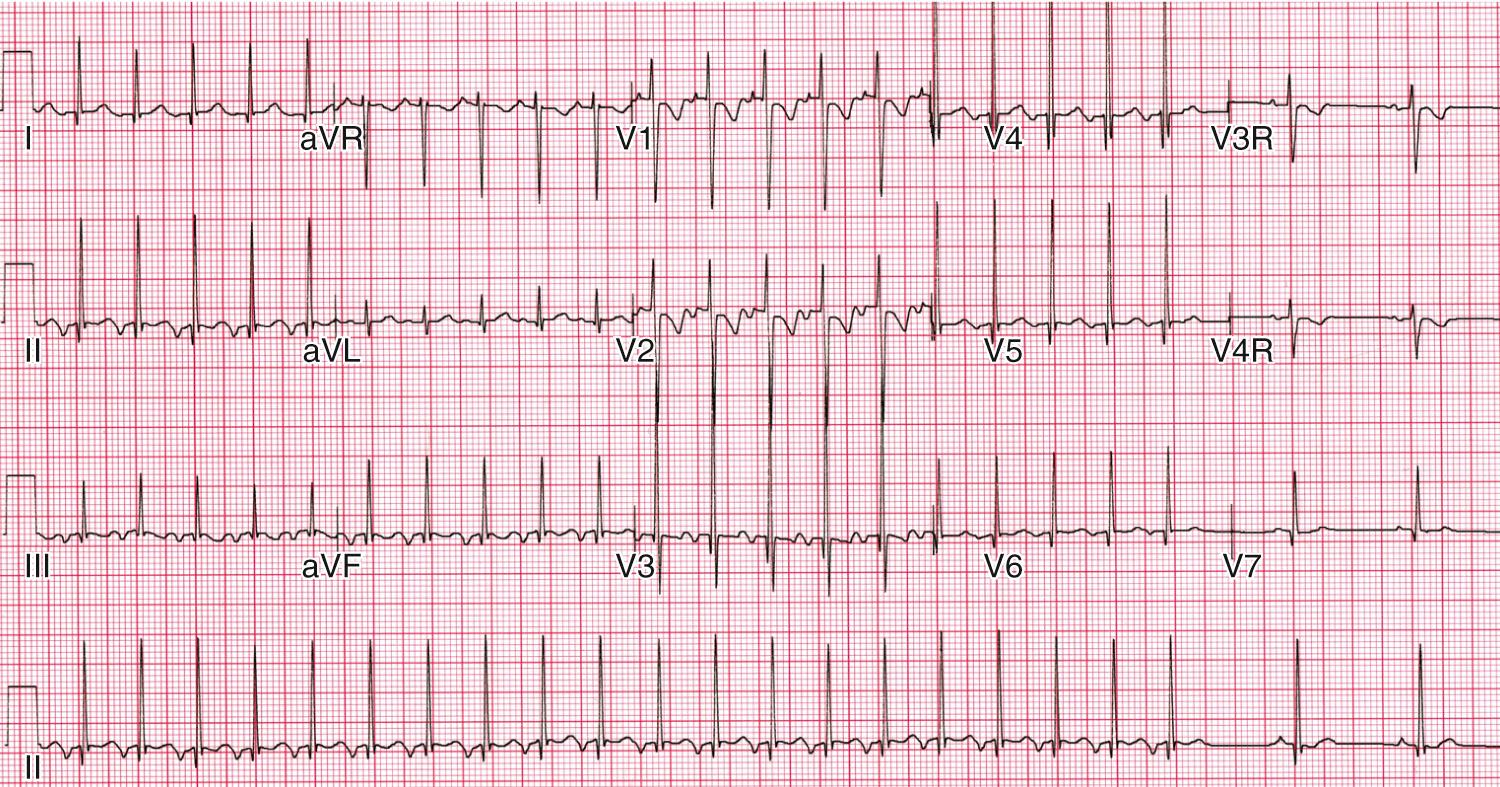
Reentry SVT ( Fig. 22.8 ) requires an anatomic substrate for abnormal conduction and the appropriate electrophysiologic environment. Reentrant tachycardias, such as AVRT and AVNRT, require a difference in the electrophysiologic properties of two AV pathways to initiate tachycardia; this allows the occurrence of unidirectional block in one pathway while maintaining conduction in the other. Patients presenting with a reentrant arrhythmia often report symptoms consistent with an abrupt onset and termination. They may go so far as to recognize that coughing or holding their breath (vagal maneuvers) will terminate the tachycardia. Both AVRT and AVNRT are typically narrow QRS tachycardias with a 1 : 1 relationship between the atrium and ventricles. One exception to this rule is patients who have an underlying bundle-branch block (i.e., tetralogy of Fallot), as the tachycardia will have the same underlying wide QRS morphology as seen in sinus rhythm. In this regard it is always helpful to review old ECGs, if available, in patients presenting with palpitations ( Figs. 22.9A and B ). Both tachycardias use the AV node as the anterograde limb of the tachycardia circuit and thus will terminate with vagal maneuvers and AV nodal blocking agents such as adenosine.
AVRT is usually due to a reentrant circuit that involves anterograde conduction over the AV node and retrograde conduction over an accessory AV pathway (orthodromic reentrant SVT). The accessory pathway or bypass tract is a microscopic muscular connection that traverses the mitral or tricuspid annulus, allowing electrical continuity between the atrium and the ventricles. Some accessory pathways allow conduction from the atrium to the ventricle anterograde; thus there is a pattern of manifest preexcitation, a delta wave, on the surface ECG. Some pathways can conduct only in the retrograde (ventricle-to-atrium) direction and are thus concealed, without evidence of a delta wave on the surface ECG. Finally, some pathways can conduct in both directions. There is an association between AVRT and structural heart disease, especially the Ebstein malformation of the tricuspid valve and congenitally corrected transposition of the great arteries (AV and ventriculoatrial [VA] discordance), cardiac tumors, tuberous sclerosis, and hypertrophic cardiomyopathy. These conditions may have concealed or manifest accessory pathways; if surgery is being contemplated, a discussion with the medical team regarding a presurgical assessment and catheter ablation is often warranted.
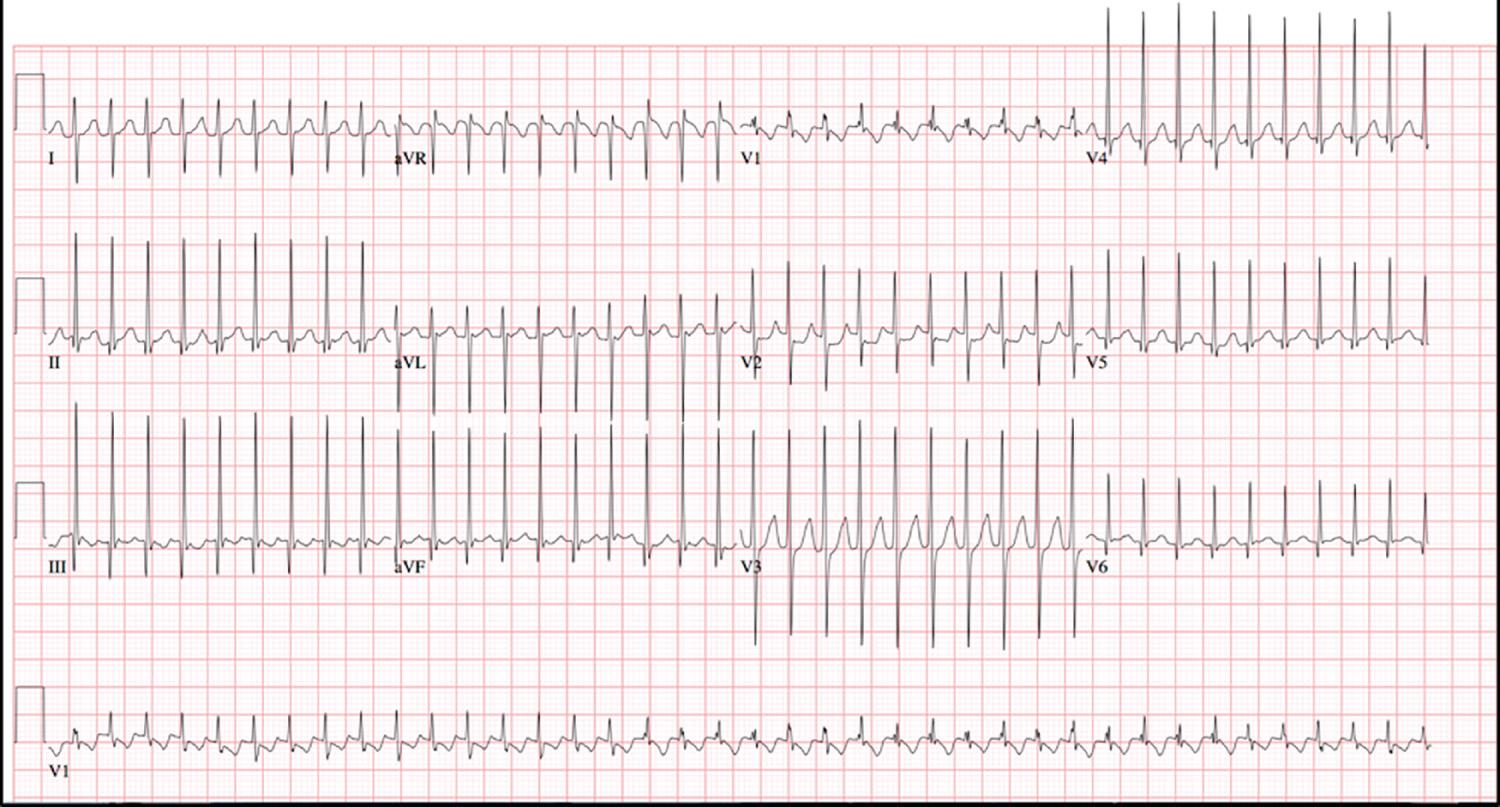
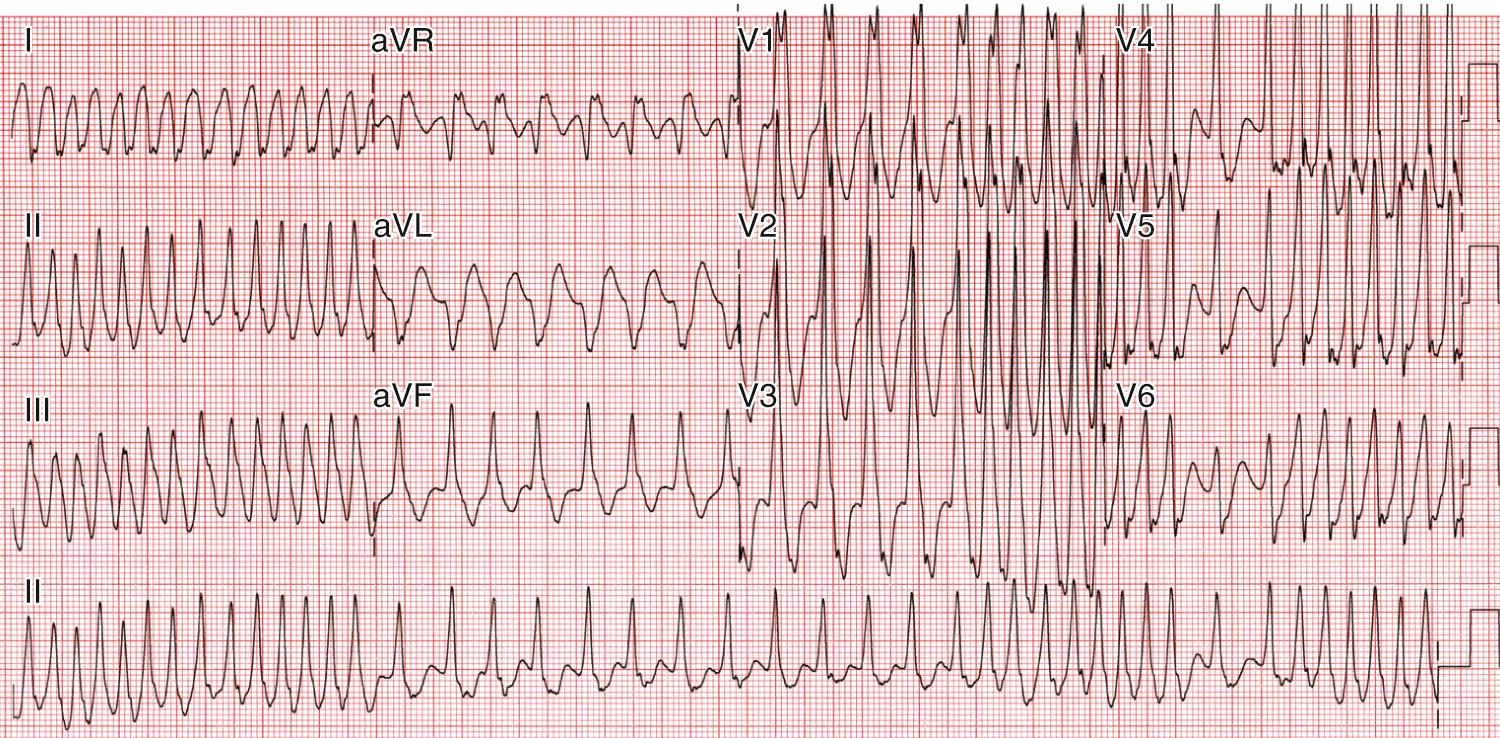
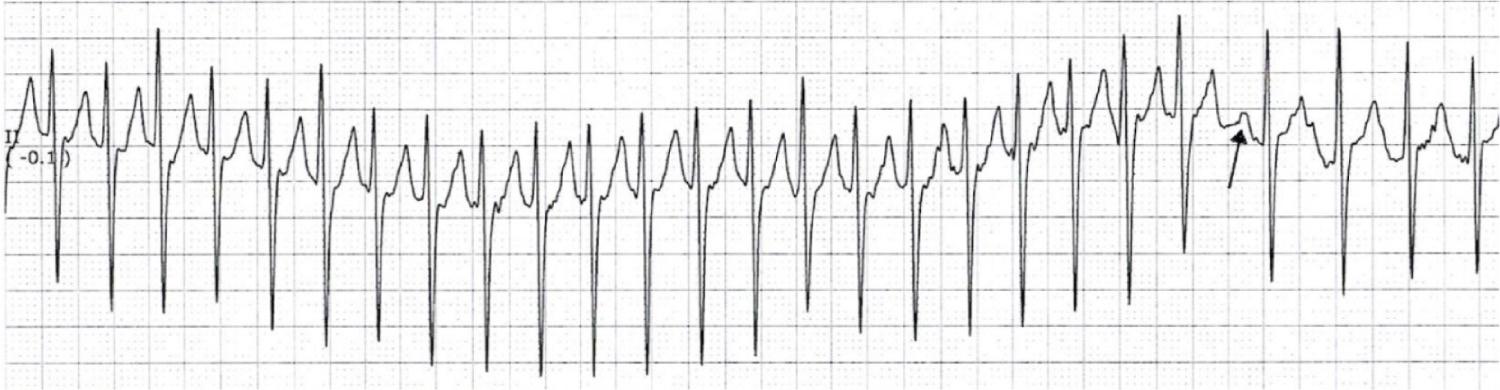
Wolff-Parkinson-White Syndrome (WPW) syndrome is a condition in which anterograde conduction occurs over the accessory pathway during sinus rhythm and results in a manifest change on the surface ECG ( Fig. 22.10 ). Because accessory pathways may be capable of a more rapid rate of conduction from the atria to the ventricles than the normal AV node, ventricular depolarization occurs before activation from the AV node and bundle of His (preexcitation), causing a short PR interval and wide QRS complex with a “slurred” upstroke or a delta wave. Patients with WPW syndrome may have no symptoms (asymptomatic WPW syndrome), reentrant SVT (typical WPW SVT), or rarely but incredibly concerning degeneration of SVT into atrial fibrillation (AF) over the accessory pathway followed by ventricular fibrillation (VF) and potentially sudden cardiac death. Although AF occurs more commonly in children with WPW syndrome than in those without, AVRT is the most common arrhythmia seen in WPW syndrome. Antidromic reciprocating tachycardia is far less common and is a tachycardia circuit that uses the accessory pathway in the anterograde direction and the AV node retrograde. This is a maximally preexcited tachycardia and therefore is a wide QRS tachycardia that can be mistaken for VT.
Sudden death occurs in WPW syndrome as consequence of rapid anterograde conduction of AF over the accessory pathway resulting in VF ( Fig. 22.11 ). The incidence of sudden death in WPW syndrome is low (estimated at 1 in 1000 patients per year); but without a premortem ECG or comprehensive autopsy evaluation of the conduction system and AV junction, it is impossible to be certain. It is disconcerting that studies have identified previously asymptomatic children with ventricular preexcitation whose only symptom was VF. Although it would seem reasonable that symptomatic patients would constitute a higher-risk cohort than asymptomatic patients, the risk profiles may be relatively similar. Catheter ablation seems to be effective at eliminating the WPW substrate and the risk of sudden cardiac death; however, ablation itself carries a risk of adverse events, including AV block, coronary artery injury, and vascular injury. As an initial starting point, the Pediatric and Congenital Electrophysiology Society in conjunction with the Heart Rhythm Society published recommendations regarding the management of the asymptomatic child/adolescent with ventricular preexcitation and a structurally normal heart. The recommendations centered on understanding the refractoriness of the accessory pathway. Clear and abrupt loss of the delta wave on the exercise test has been shown to correlate with a low-risk accessory pathway, with confirmatory invasive testing showing accessory pathway block at a heart rate below 222 beats/min (100% sensitivity and positive predictive value). Unfortunately, less than 20% of children demonstrate this finding. Therefore invasive electrophysiology testing has been recommended with the goal of assessing the shortest RR interval during inducible AF or rapid atrial pacing. This test has had relatively good sensitivity in identifying a low-risk accessory pathway in asymptomatic children (sensitivity 88% to 100%), and the use of isoproterenol may increase the sensitivity to counter the effects of general anesthesia. However, no noninvasive or invasive electrophysiologic testing is 100% predictive of a completely benign accessory pathway. In fact, reports of patients with intermittent ventricular preexcitation, previously thought to be completely benign, may warrant additional testing ( Fig. 22.12 ). Identification of a low-risk accessory pathway by electrophysiologic testing (an accessory pathway that cannot conduct 250 beats/min or more at baseline or on isoproterenol) may point to a low-risk accessory pathway but does not confer zero risk of a life-threatening event. In a recent multicenter study of children with WPW syndrome, patients with a life-threatening event were compared with those without. In this study, there were 96 children who had experienced a life-threatening event: rapidly conducted preexcited AF (49%), aborted sudden death (45%), and sudden death (6%); there were 816 controls without an event. In the cohort with a life-threatening event, this was the sentinel symptom in 65%. Risk factors for a life-threatening event included male sex, the Ebstein malformation, rapid pathway conduction, and multiple pathways. Among the cohort who had experienced a life-threatening event, 60 had had an electrophysiologic study (EPS) that was of adequate detail to characterize risk; of these, 37% had no data to suggest a high-risk accessory pathway, and 25% had neither concerning pathway characteristics nor inducible SVT. Thus, even data obtained at the time of an EPS may not allow complete identification of children with WPW syndrome who are at risk for sudden death. Careful and thoughtful discussions must take place with the patient and family regarding the short-term potential complications associated with catheter ablation versus the rare but lifetime risk of a life-threatening arrhythmia. Patients and families who choose not to proceed with invasive electrophysiologic testing and catheter ablation must be seen for follow-up and report any symptoms such as syncope or palpitations. One must balance the risks of the procedure—which should take into account the age and size of the patient and the location of the accessory pathway—with the long-term risk of developing SVT or AF.
The ability to generate AVNRT implies dual AV node physiology, likely a consequence of two or more distinct AV nodal pathways with distinct electrophysiologic properties. Anterograde conduction occurs over one AV nodal pathway; usually the slower and retrograde conduction occurs over the other in typical AVNRT, and the converse is atypical AVNRT. Atypical AVNRT is very uncommon in children. AVNRT is less common than AVRT in the neonate and infant, occurring in 10% to 15% of patients under age 1; it increases in frequency with age. The development of AVNRT in children as they age may be due to maturational changes in the electrophysiologic properties of the AV node. In an attempt to assess this, AV node function was evaluated by electrophysiologic testing in two different pediatric age groups (approximately 4 months to 13 years and from 13 to 20 years). The AV node in the younger patients was able to tolerate much faster pacing rates before developing anterograde AV block. In contrast, retrograde VA conduction was not age dependent and was common, with no differences related to age. Dual AV node pathways occurred significantly more often in the older children. These observations indicate that the substrate for AVNRT (dual AV node pathways, with inducible anterograde block in one limb at moderately rapid rates) is more likely to be present in adolescents and is rare in children and infants. AVNRT is also seen in simple as well as complex congenital heart disease either before or after surgical or interventional cardiac catheterization procedures. AVNRT appears to be more common in substrates that have either a pressure- or volume-loaded RV. An unsuccessful AVNRT ablation was more common in those with complex congenital heart disease, likely related to the malposition of the AV node.
Acute events of tachycardia can terminate with vagal maneuvers, adenosine, and overdrive pacing ( Figs. 22.13 and 22.14 ). Cardioversion is usually restricted to hemodynamically unstable patients or those where other termination methods have been unsuccessful. Decisions concerning chronic medical therapy or a cure by catheter ablation must take into account the natural history, SVT burden and symptoms, patient age and size, structural and functional heart disease, and whether the patient has WPW syndrome.
Although episodes of SVT are common during infancy, most patients are free of tachycardia during early childhood, although some infants do not have a recurrence of SVT after the initial presentation. Natural history studies have suggested that approximately 30% of infants lose SVT inducibility by 1 year of age. Factors at presentation, characteristics of the tachycardia, or data from an initial esophageal EPS failed to predict which infants would have continued SVT recurrences and thus require antiarrhythmic medication and which infants would not need medication. However, all infants with the diagnosis of AVNRT continued to have inducible SVT at 1 year of age. Most infants are free of medications at 1 year of age.
The use of chronic antiarrhythmic medications in the infant may prevent recurrent SVT events and allow the time needed for SVT resolution. There have been few clinical trials to direct chronic SVT management in children, and the choice of antiarrhythmic medications is often based on personal preference and institutional practice as opposed to data from controlled clinical trials. In the first randomized controlled trial of medical prophylaxis for SVT in a pediatric population, the researchers detected no differences in SVT recurrence between digoxin and propranolol, the two most common clinical choices for SVT prophylaxis in infants. A low SVT recurrence rate was seen in both groups. In this study, all recurrences were seen in the first few weeks of life, and the majority of patients were arrhythmia free at 4 months of age. Currently it is standard practice to use prophylactic medication for 6 to 12 months, but this duration of therapy may not be necessary. Both digoxin and propranolol represent a reasonable first-line choice for the neonate with SVT. However, if WPW syndrome is present, digoxin is not recommended owing to reports that this can shorten the effective refractory period of the accessory connection. In an older child a β-blocker with twice daily dosing may be preferable and atenolol is a reasonable first-line agent.
Decisions concerning the need for other antiarrhythmic agents depend on the tachycardia burden and symptoms, coexisting structural and functional heart disease, personal experience, and institutional practice. Numerous agents exist, although few have had rigorous testing in a pediatric population.
Decisions are often based on input from the patient and family. Pediatric catheter ablation indications were assessed in two large pediatric studies, and the most common indication for catheter ablation was patient and parent wishes.
Children with WPW syndrome are different. Because this condition is associated with a small risk of sudden death, there should be a low threshold for ablation in this population, with patient age and size factored into the decision. Animal studies suggest lesion growth when ablations are undertaken in immature animals, and risks have been shown to be increased in children weighing less than 15 kg. Postponing an ablation allows time for substrate resolution as well as the patient's somatic growth, which can decrease the risk of the procedure. Ablation is not without risk, but the risk is small. Thus the small and immediate risk of the ablation must be weighed against the lifetime symptom burden, ease of SVT management, and—in children with WPW syndrome—the lifetime risk of sudden death.
PJRT is an accessory pathway–mediated tachycardia with a long RP interval; it occurs predominantly in infants and children ( Fig. 22.15 ). The pathway can be located anywhere in the AV junction but is usually located in the posteroseptal region. This is a tachycardia with a long VA interval, called a long RP′ tachycardia. The typical ECG of PJRT is that of negative P waves in leads II, III, aVF, given the typical inferior location of this unique accessory pathway. Because the AV node constitutes the anterograde limb of this tachycardia, it will likely terminate with adenosine; most often, however, it quickly recurs. Pathways are tortuous and slow conducting; thus the tachycardia is often incessant, and PJRT is the second most common cause of arrhythmia-induced cardiomyopathy in children. In a large review of children with PJRT, 27% presented in fetal life, 7% of these with hydrops, which is a fetal manifestation of arrhythmia-induced cardiomyopathy. Isolation of the AV junction is a continuing process that may not be complete at birth, and the presence of accessory connections crossing the annulus fibrosus could result in persistent perinatal SVT. Although most children with PJRT present with palpitations or are noted to have rapid heart rates, in this series of 194 children, 18% presented with cardiomyopathy. Cardiomyopathy was more likely to occur in children with longer RP interval/cycle length ratios, consistent with an accessory pathway with slow retrograde conduction and a wide, excitable gap. PJRT is often incessant, and those with incessant PJRT had longer RP intervals, were younger at diagnosis, and more often had cardiomyopathy. The clinical course of PJRT is not benign and spontaneous resolution is unlikely.
A number of antiarrhythmic medications have been used to treat PJRT, and a single most effective agent has not emerged. β-blockers are the common first choice, likely reflecting physician comfort rather than proven efficacy. Caution should be exercised when β-blockers are being given to neonates as they may cause hypoglycemia and sleep disturbances; moreover, occasionally infants do not eat as well while on antiarrhythmic medications. Complete tachycardia suppression with medications varies from 25% in the recent series to more than 80% in a study using regimens that included amiodarone. Medical therapy is commonly employed in neonates and infants, whereas older children typically undergo ablation. Catheter ablation is the primary treatment for PJRT in older children or small children who fail medical management or have frequent bouts tachycardia with echocardiographic evidence of ventricular dysfunction or clinical signs of heart failure. Success rate for catheter ablation of PJRT is 90% (Kang).
Although atrial flutter is uncommon in children with structurally normal hearts, neonatal atrial flutter does occur ( Fig. 22.16 ). This can be seen in utero; in the neonate, it usually occurs in the first 48 hours of life. Unrecognized, this can result in an arrhythmia-induced cardiomyopathy. Cardioversion is effective and the arrhythmia usually does not recur. Most neonates do not require antiarrhythmic medications. There is an association between atrial flutter in the fetus and the newborn and the subsequent development of AVRT.
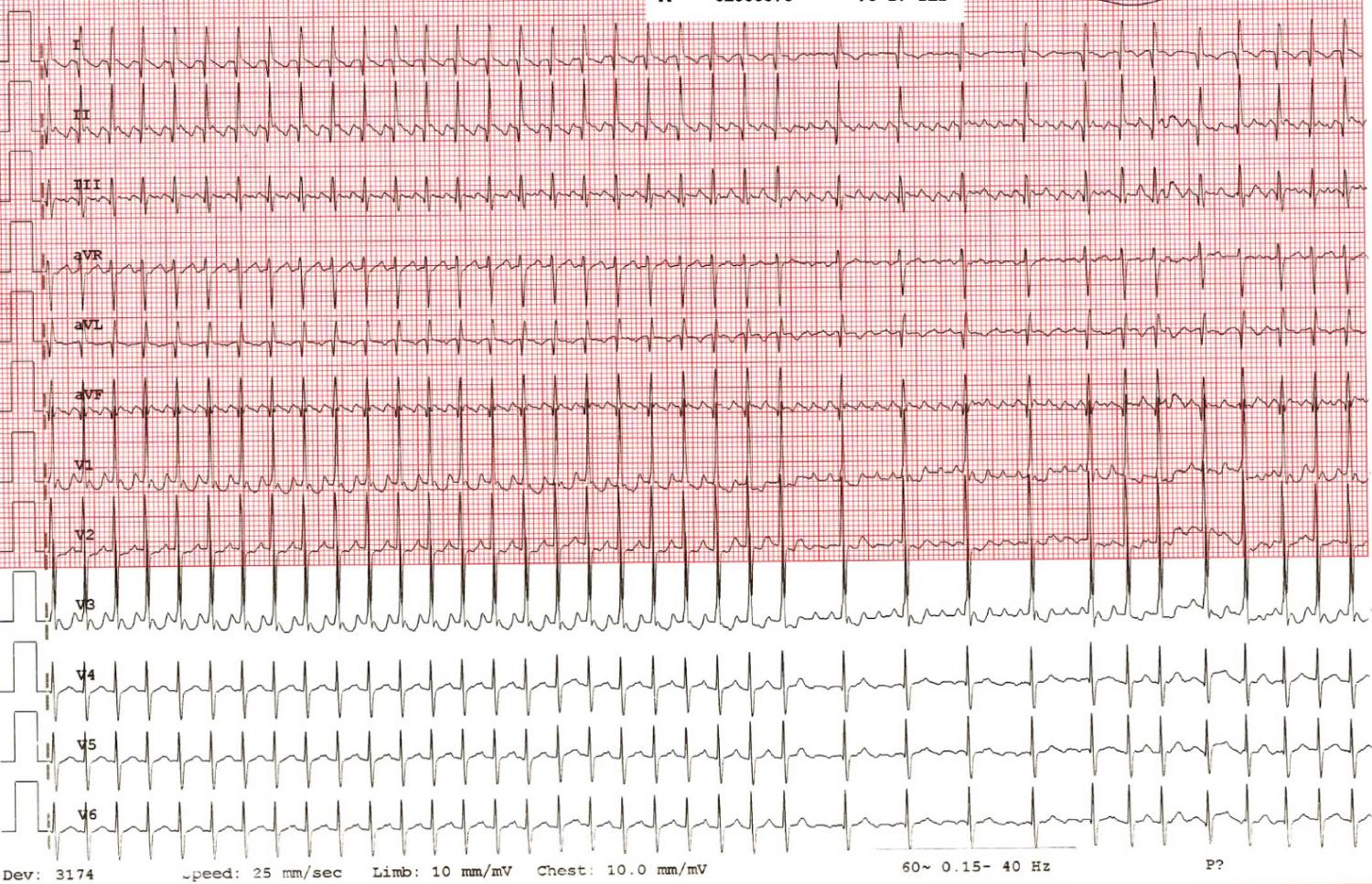
Unlike reentrant tachycardias, automatic tachycardias are rapid discharges from an automatic focus distinct from the sinus node. Typically these tachycardias have a “warm up and a cool-down” phase and respond to the autonomic tone of the individual. Distinct from reentrant tachycardia, automatic tachycardias often cannot be initiated or terminated with programmed electrical stimulation and are less likely to terminate with cardioversion. They do not use the AV node as part of the tachycardia circuit so do not routinely terminate with adenosine, although the use of this medication may allow for AV block and unmask an atrial tachycardia.
AET is the most common arrhythmia associated with arrhythmia-induced cardiomyopathy in children. Although a P-wave morphology and axis usually differ from sinus rhythm, an AET focus near the sinus node or right upper pulmonary vein is hard to differentiate from sinus tachycardia, especially in patients with heart failure, where sinus tachycardia is expected. Increased automaticity is the most likely mechanism; others include triggered activity and microreentry. AET usually occurs without structural heart disease but has been described after congenital heart disease surgery and in the setting of channelopathies. Arrhythmia-induced cardiomyopathy may occur in 1 in 4 children with AET; however, the presentation may vary from mild LV dysfunction to the need for heart failure medications; in rare cases it may require advanced mechanical heart failure therapies. Although β-blockers are often the first line of therapy in AET, drug failures are common and multiple antiarrhythmics may be utilized. Catheter ablation is effective in AET. In this procedure conscious sedation may be preferred to negate the potential that general anesthesia will suppress the tachyarrhythmia and reduce the likelihood of a successful ablation. The use of electroanatomic mapping for ablation has improved success and decreased recurrence. Spontaneous resolution of AET can occur, especially in those presenting within the first year of life, where 74% had resolution. Although ablation has proven safe and effective, a trial of medical therapy in the youngest patients, in whom ablation may have more risk and where spontaneous resolution, is prudent.
JET has two forms: occurring immediately after surgery (postoperative) or as a primary idiopathic arrhythmia (congenital). JET is due to abnormal automaticity in the region of the AV junction and is defined as a narrow QRS complex often with AV dissociation or retrograde atrial conduction in a 1 : 1 pattern. JET is most commonly seen in young children following complex congenital heart surgery ( Fig. 22.17 ) around the AV node with long cardiopulmonary bypass times and need for significant inotropic support. Postoperative JET is unique in that it is potentially life-threatening yet is self-limited. Because of the clinical context involving a small child after open-heart surgery, it is often a serious arrhythmia, associated with hemodynamic compromise and a high morbidity and mortality. Treatment is often needed and historically has included maximization of the patient's hemodynamics, correcting electrolyte abnormalities, minimizing inotropic agents when possible, and atrial pacing at rates exceeding the JET rate to provide AV synchrony when the JET rate will allow. A number of agents have been shown to be effective, including, magnesium, procainamide, esmolol, amiodarone, and dexemedetomidine. Although many treatment approaches exist, we advocate normalization of the electrolytes and acid base status, cooling to a temperature of 36°C to 37°C, and atrial pacing if JET rates are below 160 beats/min to reestablish AV synchrony. If this regimen is not adequate for control and hemodynamic improvement is not achieved, the addition of dexmedetomidine followed by intravenous amiodarone can be considered. If a bolus of amiodarone can be avoided and a drip instituted, this can prove effective over time and can avoid the risk of serious hemodynamic collapse, which has been described with the use of intravenous amiodarone in infants with acidosis, ventricular dysfunction, and prolonged tachycardia. If a bolus of amiodarone is required (2.5 to 5.0 mg/kg), it is prudent to give the bolus over a period of 45 to 60 minutes to reduce the possibility of cardiovascular collapse. The infusion rate for pediatric patients is 5 to 15 μg/kg per minute, using the lowest effective dose.
JET unassociated with cardiac surgery (congenital JET) can present at any age. In the past, when congenital JET presented in infancy, it was associated with high morbidity and mortality. In a more recent multicenter study of nonoperative JET, overall mortality was lower, with all deaths occurring in children 6 months of age or less. Although only 16% presented with heart failure, the tachycardia was incessant in more than 40%. JET can be incessant or paroxysmal, although infants below 6 months of age are more likely to have incessant tachycardia. Medical management is commonly undertaken (89%) as the first step, but it was variably effective, with a variety of drugs used. β-blockers were the most common first-line agent, but the majority of patients required two or more drugs for control, with complete suppression seen in only 11%. Amiodarone alone or in combination was cited as the most effective for rate or rhythm control. A newer agent, ivabradine, may prove useful in nonoperative JET. Catheter ablation for JET can be accomplished with the preservation of AV nodal conduction, and cryoablation has been associated with success rates similar to those of radiofrequency (RF) ablation but without AV block.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here