Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
As many as 15 million people suffer from some level of dysphagia during their lifetime, with 1 million receiving a new diagnosis of dysphagia every year.
More than 60,000 Americans die from complications associated with dysphagia, most commonly aspiration pneumonia. Aspiration pneumonia is one of the leading causes of death among the elderly.
The average cost of managing a patient with a feeding tube is reported to be more than $31,000 per patient per year. PEG tubes increase the length of hospital stay and increase patient expenses.
A variety of conditions, both acute and chronic, can influence the safety and efficiency of the swallow response, resulting in dysphagia.
Dysphagia profoundly affects patients and often leads to depression due to changes in lifestyle and overall decreased quality of life.
Which cranial nerves are involved in swallowing? There are six cranial nerves that contribute to both swallowing and speech, including the following:
CN V: Trigeminal nerve
CN VII: Facial nerve
CN IX: Glossopharyngeal nerve
CN X: Vagus nerve
CN XI: Spinal Accessory nerve
CN XII: Hypoglossal nerve
Keeping a cuff inflated on a tracheostomy tube does not mechanically prevent aspiration; it merely contains aspirated material at the level of the cuff, which will leak further into the airway upon cuff deflation unless subglottic suction is in place.
The less viscous the food material (e.g., liquids), the more likely it is to be aspirated. This is why the 3-oz water test has been successful in identifying aspiration risk.
Normal swallowing is divided into phases: (a) the pre-oral anticipatory phase, (b) the oral preparatory phase, (c) the oral transport phase, (d) the pharyngeal phase, and (e) the esophageal phase.
Pre-oral anticipatory phase: This phase begins with seeing, smelling, and tasting food. When these senses are triggered, we produce saliva that contains enzymes that start the process of digestion when food is manipulated in the mouth.
Oral preparatory phase: After food enters the oral cavity, it mixes with saliva and is manipulated by the tongue, lips, cheeks, palate, and jaw via mashing and rotary chewing motion. The masticated food is formed into a cohesive bolus by the tongue in preparation for swallowing.
Oral transport phase: The transport phase of a swallow involves propelling the bolus back between the tongue and palate until the bolus reaches the anterior tonsillar pillars. At this point, a swallow response is initiated and the oral phase of swallow is concluded. The normal oral phase lasts approximately 1 second, even with differing food consistencies, ages, or sex of the individuals.
Pharyngeal phase: The pharyngeal phase of a swallow is initiated after the swallow response is triggered. The pharyngeal phase of a swallow involves four main neuromotor components: (a) velopharyngeal closure to prevent oral contents from entering the nasal cavity; (b) sequential contraction of the superior, medial, and inferior pharyngeal constrictors to assist propulsion of the bolus through the pharynx and assist with epiglottic deflection; (c) laryngeal closure via approximation of the true vocal folds and false vocal folds, approximation of the arytenoids to the base of the epiglottis, and epiglottic deflection to prevent aspiration; and (d) opening of the pharyngoesophageal segment (PES), otherwise known as the upper esophageal sphincter. PES opening occurs as a result of three mechanisms: the superiorly directed mechanical tension from laryngeal elevation, signals from the vagus nerve to relax the muscular segment, and the contact pressure exerted by the bolus on the PES.
Esophageal phase: The esophageal phase of a swallow occurs when the bolus passes through the PES. The bolus is then carried through the esophagus via peristaltic movements of the esophagus to the lower esophageal sphincter, which relaxes to allow material to pass into the stomach.
Dysphagia is the symptom of difficulty in swallowing that can occur within any phase or combination of phases of swallowing as described above.
Dysphagia is most commonly caused by neurologic pathology and/or structural trauma. Neurologic pathologies include diseases affecting the cerebral cortex and brainstem, cranial nerves, and/or muscles of swallowing. Cerebral vascular accident (CVA) is the most common cause of dysphagia, followed by neurogenic diseases and head and neck cancers. If only a single cerebral hemisphere is affected by CVA, swallowing may be preserved because the brainstem still receives input from the noninjured hemisphere.
Dysphagia can occur during any phase of swallowing. In the oral preparatory phase, swallowing is controlled by both the cortex and brainstem and is voluntary (i.e., not a reflex). Dysfunction within the oral phase can lead to frequent spillage from the lips, inability to chew, and collection of food residue in the cheeks. These deficits result from decreased lip closure, decreased buccal tension, and decreased strength and/or coordination in the tongue and muscles during mastication. The pharyngeal phase of swallowing is an involuntary phase that is controlled by the brainstem. Pharyngeal phase impairments can include a delayed swallow reflex, decreased velopharyngeal closure resulting in pharyngonasal backflow, insufficient laryngeal closure, insufficient pharyngeal propulsion, and insufficient opening of the upper esophageal sphincter. Esophageal phase impairments include ineffective motility and failure of the lower esophageal sphincter to relax.
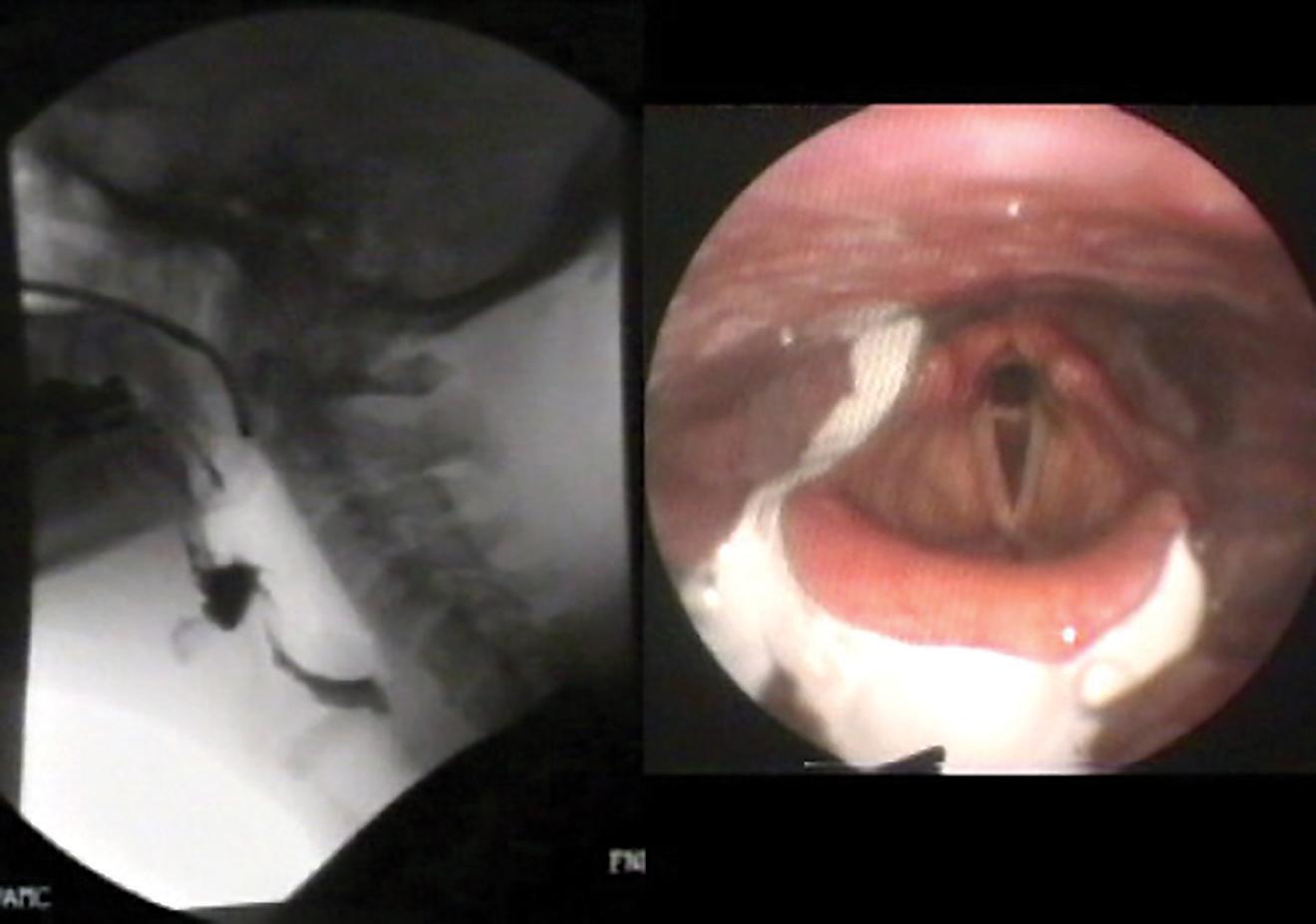
There are three techniques widely used to diagnose oropharyngeal dysphagia: (a) bedside swallow evaluation, also known as a clinical evaluation; (b) fluoroscopic examination called a modified barium swallow (MBS); and (c) fiberoptic endoscopic evaluation of swallowing (FEES). Esophageal phase dysphagia is commonly assessed via esophagram, manometry, and endoscopy. Bedside tests are noninstrumental assessments and are minimally invasive. This assessment involves merging clinical history, observation, and therapeutic trials to assess the risk factors of dysphagia. The Bedside evaluation has low sensitivity and interrater reliability. In addition, the bedside evaluation is poor in detecting silent aspiration. Modified barium swallow studies (MBSS) allow for an indirect view of the function. The MBS studies can also used to assess the effectiveness of compensatory strategies, which can decrease the presence of airway penetration or aspiration. Fiber-optic endoscopy is used to assess the pharyngeal phase without the use of radiation ( Fig. 76.1 ).
The difference between laryngeal penetration and laryngeal aspiration is based on anatomical boundaries. Laryngeal penetration is defined as misdirected material at or above the level of the true vocal folds. If penetration into the laryngeal vestibule occurs during swallowing but clears with no residue once swallowing is complete, it is known as “transient” penetration. Aspiration is defined as material that passes below the level of the true vocal folds and enters the trachea. “Silent” aspiration is used to describe material that drops below the level of the true vocal cords, without any perception of the event (e.g., coughing, throat clearing, etc.).
A bedside swallow evaluation is a noninstrumental assessment. The purpose is to uncover any risk factors for dysphagia, signs of dysphagia, potential mechanisms, and treatment options and to determine if and what instrumental assessments are indicated. Speech-language pathologists (SLPs) look for signs or symptoms of possible oral or pharyngeal dysphagia when someone is eating or drinking. A thorough examination will include a comprehensive chart review, oral motor assessment, assessment of vocal quality, strength of cough, and administration of various food and liquid consistencies to monitor for signs of oral or pharyngeal deficits. If additional information is needed to define function and develop a corresponding treatment plan, an SLP will often perform an instrumental evaluation that allows visualization of swallow function, usually an MBS study or FEES.
For a patient with a tracheostomy tube, a bedside swallowing evaluation will begin by determining why the tracheostomy was placed. Some reasons for tracheostomy can render the beside swallow evaluation unreliable. For example, signs of pharyngeal dysphagia can be undiscernible in a tracheostomized individual with a large and obstructing laryngeal mass. If a bedside evaluation is indicated, it is best to check for cuff deflation and assess finger occlusion to determine the patient’s ability to move air around the tracheostomy tube and into the upper airway. If no difficulty is observed, the SLP proceeds with the clinical assessment, including food and liquid trials, if indicated. Signs of aspiration can be further assessed via endotracheal suctioning by trained personnel. Historically, food and liquid trials were dyed blue to make signs of aspiration more apparent. In some cases, a Passy Muir valve (PMV) can improve swallow comfort and safety by increasing subglottic pressure and enabling a more effective cough response to clear the upper airway. If a tracheostomized individual is at high risk of silent aspiration – for example, a stroke patient, an instrumental assessment is often best.
Indicators of penetration/aspiration include coughing upon a swallow, wheezing after intake, choking, chest congestion, tachypnea, noisy or wet breathing, wet vocal quality, throat clearing after a swallow, and rapid sequential swallows to clear a single bolus. Delayed signs of aspiration include infiltrates on a chest x-ray located in gravity-dependent locations, suctioning of postprandial material from the airway, coughing up food particles, and fever.
The modified Evan’s blue dye test (MEBDT) is a technique less commonly used today to assess for evidence of aspiration in the tracheostomized patient. Blue dye is placed in food and liquids provided to the patient during a bedside assessment. The patient is deeply suctioned to determine if any blue material has entered the airway. If nothing is recovered during the procedure and assessment, the SLP will wait 24 hours for evidence of delayed aspiration before allowing oral intake and notify both nursing and respiratory therapy that an MEBDT has been provided. The sensitivity and specificity of the MEBDT in predicting oropharyngeal dysphagia vary widely owing to inconsistent protocols and patient populations. A positive test merely shows evidence of aspiration, which requires additional instrumental testing to define the dysfunction. Because fiberoptic endoscopic evaluation of swallowing is more readily available at the bedside and provides more comprehensive information about structure and function, the MEBDT is not used as often.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here