Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The preferred noninvasive test for evaluating patients with suspected chronic lower extremity ischemia depends upon individual circumstances. Doppler-derived ankle-to-brachial systolic blood pressure indices (ABIs) provide an accurate and reproducible measure of overall blood supply to the foot in patients without extensive mural calcification, but they do not define the location of the occlusive disease. Four-cuff segmental blood pressures can grossly localize hemodynamically significant lower extremity arterial stenosis, but their accuracy is reduced by multilevel disease, is suboptimal for detecting iliac occlusive disease, and cannot distinguish between long- and short-segment occlusions or identify vessels that remain patent but highly stenotic. Many of these limitations can be overcome by using color duplex scanning.
Lower extremity arterial color-flow duplex imaging is performed with a variety of ultrasound transducers. For iliac vessels, 3-MHz transducers are optimal, whereas a 5-MHz transducer suffices for most infrainguinal vessel examinations. Distal tibial arteries occasionally are best examined with a 7.5- or 10-MHz transducer. Angle correction is necessary because not all lower extremity arteries can be readily insonated at the ideal Doppler angle of 60 degrees. Results obtained within a 30% to 70% range of Doppler angles in lower extremity arterial duplex mapping provide information sufficiently accurate for clinical purposes, provided velocity waveforms obtained at similar angles are compared.
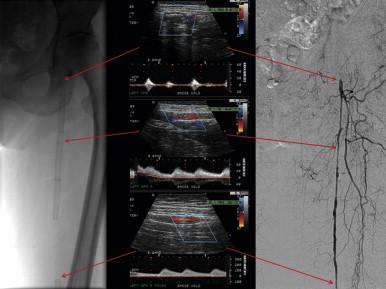
Color flow greatly aids duplex examination of lower extremity arteries, particularly the iliac and tibial arteries. It facilitates establishing vessel location, helps identify points of turbulence associated with stenoses, and can determine the length of arterial occlusions while identifying reconstitution of occluded vessels ( Figure 1 ). Measurements of diameter from the color-flow image are less accurate than spectral analysis in quantifying stenoses. As a result, spectral analysis is required to accurately quantify stenoses. It is important to remember that color is a display of average, not peak, velocity shifts and that it changes with changes in the angle of insonation. Clinical application of duplex mapping to the lower extremity arteries, therefore, begins with color flow to identify the arteries and ensure a reliable Doppler angle. Depending on the color settings, it CAN help localize areas suspicious for stenoses, but only elevated peak systolic velocities are a reliable indication of a significant stenosis. Points within a vessel that do not fill on color flow and do not have an associated Doppler signal indicate occlusion.
A complete lower extremity arterial duplex examination extends from the aorta to the ankle and is best performed the morning after an overnight fast. The amount of intraabdominal gas is less at that time, which facilitates evaluation of the iliac arteries. Most arteries are examined moving proximal to distal with the patient supine. The femoral bifurcation is most easily visualized with the leg slightly externally rotated. The popliteal artery is best insonated in the prone position to avoid confusion with large geniculate collateral vessels. Tibial arteries, when occluded proximally, are examined by identifying the vessel at the ankle and moving cephalad. With persistence, adhering to this protocol, and using well-trained, experienced vascular technologists, adequate visualization of the lower extremity vessels to the level of the ankle is almost always possible. Complete examination of both legs requires about 1½ hours. Difficult examinations take more time. However, in many cases examinations are shortened by focusing on only clinically suspicious areas.
Lower extremity arterial velocity waveforms are triphasic in the absence of a significant upstream stenosis. Systolic forward flow is followed by a short reverse flow component, and then diastolic forward flow declines to zero, or near zero, at the end of diastole. Peak systolic velocities in normal lower extremity arteries gradually decrease from the aortic bifurcation to the knee and remain relatively constant in the peroneal, anterior, and posterior tibial arteries.
Duplex criteria for grading isolated stenoses in the iliac, femoral, and popliteal arteries were first proposed by Jäger and colleagues ( Table 1 ). These early criteria depended heavily on analysis of spectral broadening for detecting stenoses of less than 50% reduction in diameter. Because spectral broadening is difficult to quantify in clinical studies and can be increased by increasing sample volume size and/or the gain control of the duplex scanner, spectral broadening for clinical purposes is not particularly useful in quantifying lower extremity arterial stenoses less than 50%. However, the criteria for 50% to 99% stenosis have proved quite accurate in prospective blinded clinical studies ( Table 2 ).
| Percentage of Stenosis | Criteria |
|---|---|
| 0 | Normal waveforms and velocities |
| 1–19 | Normal waveforms and velocities Spectral broadening primarily on the down slope of the systolic portion of the velocity curve |
| 20–49 | Normal triphasic waveform with marked spectral broadening There is at least a 30% increase in peak systolic velocity |
| 50–99 | Loss of end systolic reverse flow 100% or more increase in peak systolic velocity |
| Occluded | No detectable Doppler signal in an adequately visualized vessel |
| ILIAC | COMMON FEMORAL | DEEP FEMORAL | SUPERFICIAL FEMORAL | POPLITEAL | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author | No. of Patients | Sens | Spec | PPV | NPV | Sens | Spec | PPV | NPV | Sens | Spec | PPV | NPV | Sens | Spec | PPV | NPV | Sens | Spec | PPV | NPV |
| Kohler et al. | 32 | 89 | 90 | 75 | 96 | 67 | 98 | 80 | 96 | 67 | 81 | 53 | 88 | 84 | 93 | 90 | 88 | 75 | 97 | 86 | 93 |
| Moneta et al. | 150 | 89 | 99 | 94 | 97 | 76 | 99 | 93 | 96 | 83 | 97 | 83 | 97 | 87 | 98 | 97 | 89 | 67 | 99 | 93 | 94 |
| Cossman et al. | 61 | 81 | 98 | 94 | 92 | 70 | 97 | 78 | 96 | 71 | 95 | 56 | 97 | 87 | 85 | 86 | 72 | 84 | 97 | 93 | 93 |
| Aly et al. ∗ | 90 | 89 | 99 | 92 | 99 | NA | NA | NA | NA | 100 | 99 | 95 | 100 | 95 † | 99 † | 94 † | 99 † | 95 † | 99 † | 94 † | 99 † |
∗ Segments analyzed as aortoiliac, femoral artery, femoropopliteal region, and run-off vessels (not represented in table).
† Superficial femoral and popliteal arteries combined for data analysis.
In addition, color flow duplex scanning is very reliable in distinguishing stenosis from occlusion in iliac and femoropopliteal arterial segments, with accuracies of 98% to 100%. Furthermore, pooled data from multiple investigations suggest that overall sensitivity and specificity of duplex imaging to distinguish stenosis from occlusion is 86% and 97% for aortoiliac, 80% and 96% to 98% for femoropopliteal, and 83% and 84% for infragenicular disease, respectively (see Table 2 ). In addition, the fact that data across numerous study sites are relatively consistent for imaging the arterial tree from the aortoiliac to popliteal segments suggests that duplex scanning yields reproducible results across centers.
Imaging the infragenicular arteries has not been as consistent. Our early studies sought to predict patency of a tibial artery from the popliteal trifurcation to the ankle rather than attempt to quantitate tibial artery stenoses. Sensitivities and specificities for duplex scanning in predicting interruption of anterior and posterior tibial artery patency are 90% to 93%. Those for the peroneal artery are 82% and 74%, respectively. Aly and colleagues attempted to identify significant (>50%) stenoses in the infrapopliteal vessels, noting overall sensitivity and specificity of 82% and 99%, respectively. However, patient-to-patient variability in below-knee disease might still require angiography to definitively determine the location and extent of occlusive disease.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here