Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Numerous pharmacologic agents may adversely affect the musculoskeletal system. Radiographic manifestations of these pathologic effects may often be apparent in the advance of clinical symptomatology. Therefore, the radiologist may be the first physician to raise the possibility of a drug-related musculoskeletal disorder. The scope of drug-related disorders with radiographic abnormalities involving the musculoskeletal system is reviewed in this chapter.
The spectrum of bone and joint abnormalities that may arise in patients on long-term corticosteroid therapy is wide and includes osteoporosis, pathologic fractures, osteonecrosis, neuropathic-like articular destruction, tendinous and soft tissue injury, periarticular and capsular calcification, and abnormalities in the distribution of fat. Musculoskeletal infection may also result from immunosuppression.
The two most probable mechanisms for osteoporosis in those undergoing long-term corticosteroid treatment are (1) direct inhibition of bone formation and (2) indirect activation of bone resorption related to diminished intestinal calcium absorption and parathyroid hormone upregulation. Women, the elderly, and patients on high-dose therapy may be particularly susceptible to corticosteroid-induced osteoporosis ( eFig. 89-1 ). The process is at least partially reversible on termination of treatment.

As in the case of osteoporosis, the mechanism by which osteonecrosis results from corticosteroid use is not definitively known. Although an association between osteonecrosis and corticosteroid use is well accepted, a causal relationship has not always been directly established. The two most commonly cited mechanisms in the pathogenesis of corticosteroid-induced osteonecrosis are (1) mechanical microfractures resulting in osseous collapse and (2) vascular compromise due to marrow accumulation of fat cells, fat embolization, vasculitis, and hyperviscosity. Findings related to osteonecrosis typically appear at least 2 or 3 years after the initiation of treatment. Reports on the incidence of these findings have been highly variable and contingent on the underlying disease, dose, and duration of treatment ( eFigs. 89-2 to 89-7 ).
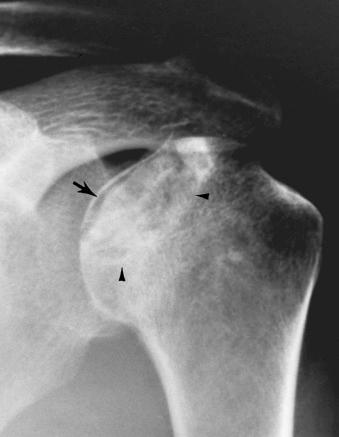


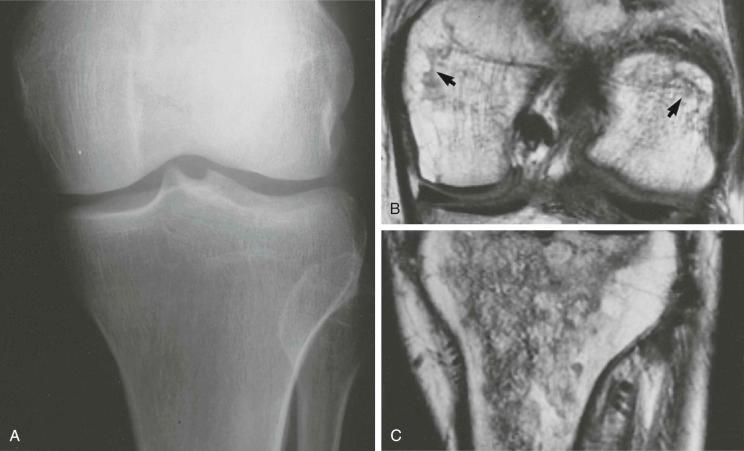
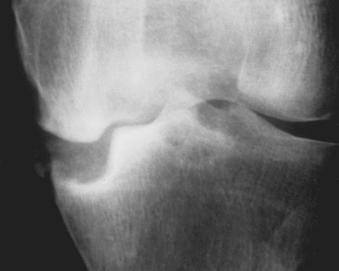
Intraarticular corticosteroid administration is believed by many, but not all, to be a cause of joint disease that mimics the neuropathic joint. This entity is most frequently seen in the hip and the knee. As in cases of neuropathic joint, recurrent trauma in the context of diminished pain sensation results in joint space narrowing, fracture, and fragmentation, leading eventually to severe osseous and cartilaginous collapse ( eFigs. 89-8 and 89-9 ).

Rarely, corticosteroid administration may predispose a patient to bone and joint infections owing to immunosuppression. The most commonly involved joint is the knee, but any joint is susceptible, and multiple joints may be simultaneously affected. Bacteria, particularly Staphylococcus aureus , are typically the causative organisms.
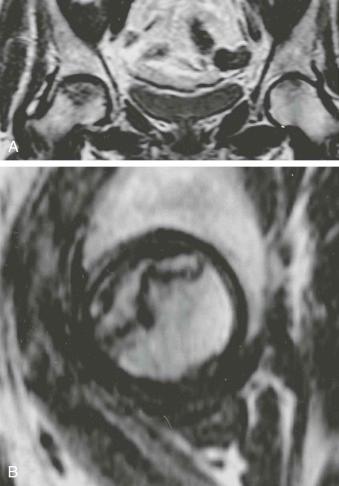
Tendon rupture may occur in the setting of systemic corticosteroid therapy or local injection. Corticosteroids are believed to induce changes in healthy tendons and inhibit normal healing of diseased tendons. Subcutaneous tissue atrophy and calcification may also be present in the region of local application of corticosteroids. Calcification due to hydroxyapatite deposition has been reported in synovial membranes, joint capsules, periarticular tissues, and cartilage ( eFig. 89-10 ). Finally, systemic corticosteroid treatment, as in Cushing disease, may result in abnormal accumulation of fat. This may manifest in the mediastinum, paraspinal region, and epidural spine. Epidural lipomatosis may have neurologic manifestations.

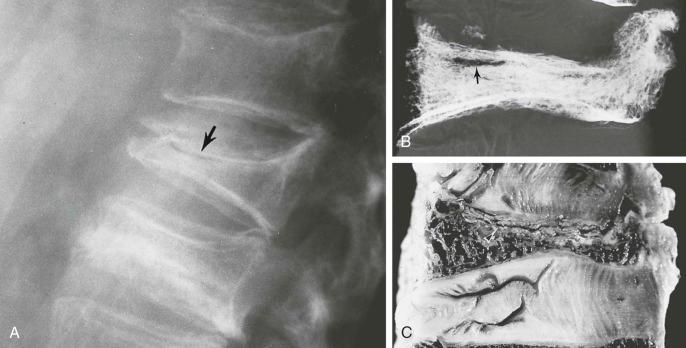
Gonadotropin-releasing hormone used in the treatment of endometriosis, premenopausal breast cancer, male breast cancer, and prostatic cancer is associated with loss of trabecular bone in lumbar vertebrae. Heparin, in large doses, is associated with osteoporosis that may be complicated by rib fractures and vertebral collapse. These findings are attributed to a collagenolytic property of heparin.
Phenytoin and phenobarbital are commonly prescribed antiepileptics that may result in generalized abnormalities of bone formation indistinguishable from rickets and osteomalacia. The associated radiographic changes were present in 20% of patients on long-term anticonvulsant treatment in one study. The biochemical basis of these changes is reflected in an elevation in serum alkaline phosphatase level present in an even larger fraction of patients early in the course of therapy. Although the mechanism underlying the altered bone metabolism remains unclear, the most compelling implicated pathway involves the induction of hepatic microsomal hydroxylase activity and consequential inactivation of vitamin D and 25-hydroxyvitamin D. Phenytoin has also been demonstrated to impair intestinal absorption of calcium. Data attempting to define the dose and treatment duration necessary to enact bony changes are inconclusive.
Radiographic changes, first described in 1968, include diffuse osteopenia, joint space widening, and the development of “Looser zones” ( eFig. 89-11 ). These findings are nonspecific and indistinguishable from other causes of osteomalacia and rickets.

Other findings that have been reported in association with phenytoin include diffuse calvarial thickening; dental root abnormalities; gross enlargement of the lips, nose, and soft tissues of the face and scalp; and heel pad thickening. Finally, phenytoin is a known teratogen and is implicated in the formation of cleft palate deformity and syndactyly.
Although aluminum is usually efficiently eliminated from the body by renal filtration, it may accumulate in the serum of patients with chronic renal failure, patients on dialysis, and patients receiving total parenteral nutrition. Aluminum toxicity most dramatically involves the brain and the skeletal system, although deposits may occur in multiple organs, including liver, muscles, and gonads. In adults, aluminum intoxication manifests itself in the skeletal system as an osteomalacia resistant to vitamin D therapy. Radiographs may show evidence of osteomalacia and spontaneous fractures. Healing of these fractures results in only minimal callus formation. The radiographic features of aluminum toxicity are similar to those seen with renal osteodystrophy. The distinguishing clinical triad that accompanies aluminum intoxication consists of skeletal pain, proximal muscle weakness, and pathologic fractures. The pathologic basis for these effects of aluminum is probably the formation of insoluble complexes with phosphates and the inhibition of the deposition of calcium apatite.
Children with impaired renal function can develop aluminum toxicity from oral intake of aluminum alone, as well as from aluminum contents of vaccines. Radiographically, the effects of aluminum intoxication in these infants result in osteopenia with pathologic fractures, fraying of the metaphyses of the long bones, and widening of the physes.
Deferoxamine is administered for long-term chelation therapy in combination with the hyperperfusion regimen in the treatment of thalassemia. It has been demonstrated that subcutaneous administration of high doses of deferoxamine in children younger than 3 years is associated with a decrease in mean body length, joint stiffness, and a rickets-like syndrome. Short trunk, prominent sternum, genu valgum, and enlargement of the distal fibula and distal radius and ulna have been noted. Humerus, femur, and tibia may also be affected. Radiographs reveal widening of the metaphyses, followed by cupping, fraying, and eventually irregular mineralization with a jagged and thickened metaphyseal line. Genu valgum deformity occurs secondary to involvement of the proximal tibial metaphysis. Changes in the axial skeleton consist of loss of height in the thoracic and lumbar vertebrae.
Bisphosphonates such as elendronate (Fosamax) and zoledronic acid (Reclast) are currently in widespread use in the treatment of osteoporosis. The efficacy of these drugs is well established in the prevention of insufficiency fractures. One study demonstrated a 47% reduction of risk. However, recent reports have established small but significant risks of skeletal complications. They include atypical stress fractures of the proximal femur and osteonecrosis of the jaw.
The risk for atypical stress fractures of the proximal femur is more pronounced with prolonged use. The fractures characteristically become clinically evident in the setting of minimal trauma, such as a minor misstep, or in the absence of any trauma at all. Patients may experience a prodromal pain over weeks or months before presentation with a fracture.
Stress fractures that result from long-term bisphosphonate therapy have a characteristic radiologic appearance that is otherwise unusual in the setting of low-energy trauma. They include fractures of the proximal femur involving the subtrochanteric region or shaft. Before the development of a complete fracture, they may manifest as focal cortical thickening or beaking of the lateral aspect of the proximal femoral shaft ( eFig. 89-12 ). These eventually develop into transverse fractures oriented perpendicular to the shaft ( eFig. 89-13 ).


Another important musculoskeletal complication of bisphosphonate therapy is osteonecrosis of the jaw. This begins with incorporation of bisphosphonate within the mandible, a site where bone turnover is physiologically high. The resulting inhibition of osseous turnover leads to an accumulation of microdamage that occurs with mastication. Osteonecrosis of the jaw in those receiving oral therapy for bone demineralization is very rare. Most reported cases are seen in patients undergoing intravenous bisphosphonate therapy in the treatment of metastatic bone disease, where prevalence is between 6% and 10% as shown in one series.
Sodium etidronate, which is used in the treatment of Paget disease, may result in development of osteomalacia. Radiolucency may develop in the bones affected by Paget disease. Pathologic fractures at these sites may occur as a result. Effects of sodium etidronate have also been described in children with myositis ossificans progressiva, in whom it may cause widening/irregularity of the physis, generalized demineralization, and irregular sclerosis. There have also been reports of the development of pseudogout in patients treated with cyclical etidronate for osteoporosis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here