Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Disseminated intravascular coagulation (DIC), also referred to as consumptive coagulopathy or defibrination, is caused by a wide variety of serious disorders ( Table 161-1 ). In most patients, the underlying process dominates the clinical picture, but in some cases (e.g., occult malignant neoplasm, envenomation), DIC may be the initial or predominant manifestation of the disorder. DIC never occurs in isolation, without an inciting cause.
| INFECTIONS |
| Gram-negative bacterial sepsis Other bacteria, fungi, viruses, Rocky Mountain spotted fever, malaria |
| IMMUNOLOGIC REACTIONS |
| Transfusion reactions (ABO incompatibility) Organ transplant rejection Hematopoietic stem cell transplantation Chimeric antigen receptor (CAR) T-cell therapy |
| OBSTETRIC COMPLICATIONS |
| Amniotic fluid embolism Retained dead fetus Abruptio placentae Toxemia, preeclampsia Septic abortion |
| MALIGNANT NEOPLASMS |
| Pancreatic carcinoma Adenocarcinomas Acute promyelocytic leukemia Other neoplasms |
| LIVER FAILURE |
| ACUTE PANCREATITIS |
| ENVENOMATION |
| RESPIRATORY DISTRESS SYNDROME |
| TRAUMA, SHOCK |
| Brain injury Crush injury Burns Hypothermia or hyperthermia Fat embolism Hypoxia, ischemia Surgery |
| VASCULAR DISORDERS |
| Giant hemangioma (Kasabach-Merritt syndrome) Aortic aneurysm Vascular tumors or malformations |
DIC is primarily a thrombotic process from a pathophysiologic perspective. However, its clinical manifestation may appear to be widespread hemorrhage in acute cases. The basic pathophysiologic mechanism ( Fig. 161-1 ), regardless of cause, is entry into the circulation of procoagulant substances that trigger systemic activation of the coagulation system and platelets. This results in disseminated deposition of fibrin-platelet thrombi within the microvasculature. In most cases, the procoagulant stimulus is tissue factor, a lipoprotein that is not normally exposed to blood. In DIC, tissue factor gains access to blood by tissue injury, its elaboration by malignant cells, or its expression on the surface of monocytes and endothelial cells by inflammatory mediators. Components of the inflammatory response and the coagulation system are reciprocally activated in some forms of DIC, such as sepsis. Tissue factor triggers generation of the coagulation protease thrombin, which induces fibrin formation and platelet activation. In some specific cases of DIC, procoagulants other than tissue factor (e.g., a cysteine protease or mucin in certain malignant neoplasms) and proteases other than thrombin (e.g., trypsin in pancreatitis, exogenous enzymes in envenomation) provide the procoagulant stimulus.
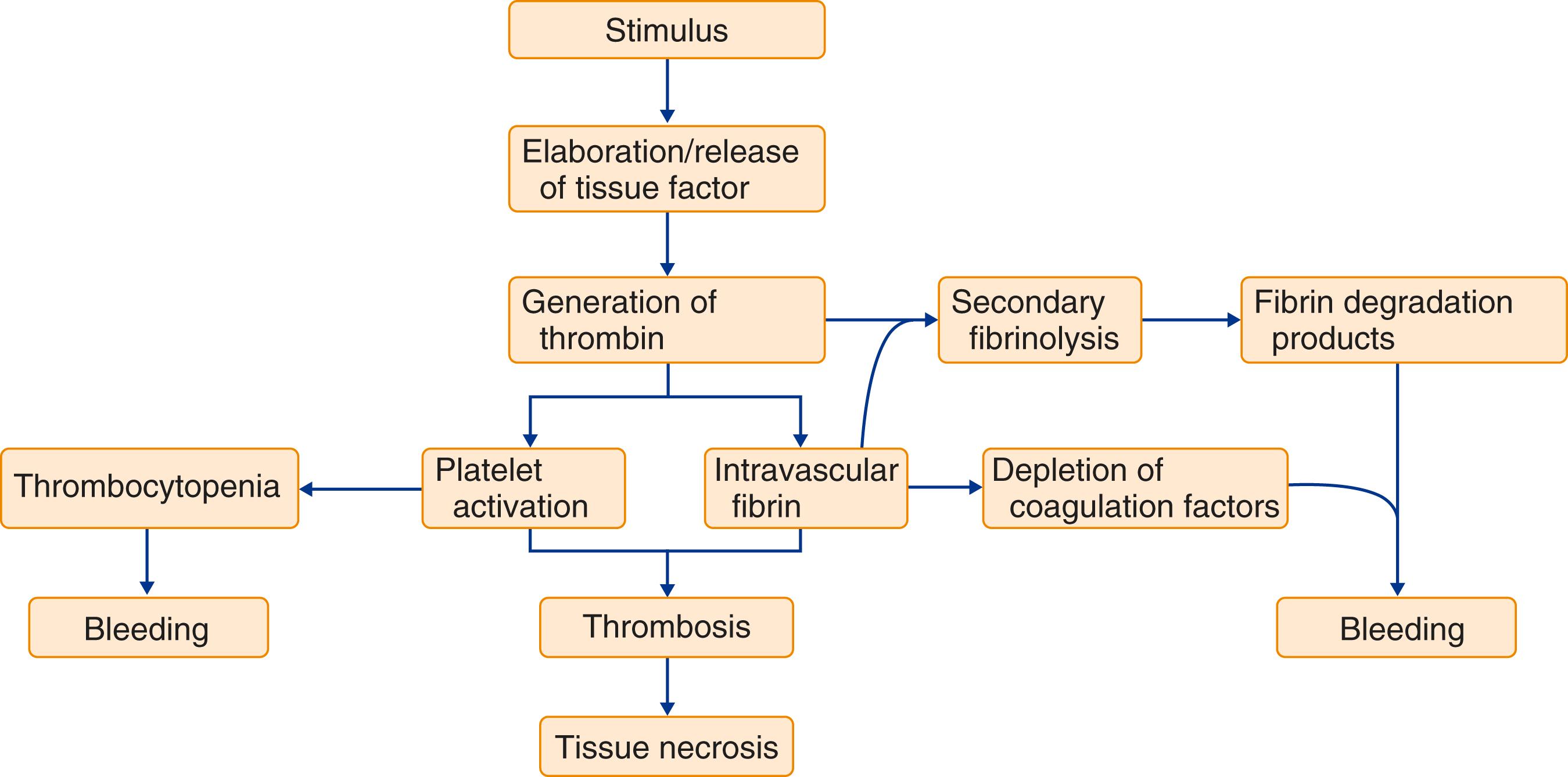
In acute, uncompensated DIC, coagulation factors are consumed at a rate in excess of the capacity of the liver to synthesize them, and platelets are consumed in excess of the capacity of bone marrow megakaryocytes to release them. The resulting laboratory manifestations under these circumstances are a prolonged prothrombin time (PT), a prolonged activated partial thromboplastin time (aPTT), and thrombocytopenia. Increased fibrin formation in DIC stimulates a heightened process of secondary fibrinolysis, in which plasminogen activators generate plasmin to digest fibrin (and fibrinogen) into fibrin(ogen) degradation products (FDPs). FDPs are potent circulating anticoagulants that further contribute to the bleeding manifestations of DIC. Intravascular fibrin deposition can cause fragmentation of red blood cells and lead to the appearance of schistocytes in blood smears (see Chapter 143 ); however, frank microangiopathic hemolytic anemia is unusual in DIC. Occlusive microvascular thrombosis in DIC can compromise the blood supply to some organs and lead to multiorgan failure, particularly when it is accompanied by systemic hemodynamic, inflammatory, and metabolic derangements.
DIC always has an underlying cause that must be identified and eliminated if the coagulopathy is to be managed successfully. The development of DIC in some of these disorders is associated with an unfavorable outcome. Infection is the most common cause of DIC. The syndrome is particularly associated with gram-negative or gram-positive sepsis ( Chapter 94 ), , although it can be triggered by a variety of other bacterial, fungal, viral, rickettsial, and protozoal microorganisms. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) with coronavirus disease 2019 (COVID-19) infection ( Chapter 336 ) can also be associated with a picture of DIC.
The placenta and uterine contents are rich sources of tissue factor and other procoagulants that are normally excluded from the maternal circulation; a spectrum of clinical manifestations of DIC may accompany obstetric complications when this barrier is breached, especially in the third trimester. These syndromes range from acute, fulminant, and often fatal DIC in amniotic fluid embolism to chronic or subacute DIC with a retained dead fetus. Other obstetric problems associated with DIC include abruptio placentae, toxemia, and septic abortion.
Chronic forms of DIC are caused by a variety of malignant neoplasms, particularly acute myeloid leukemia, pancreatic cancer ( Chapter 180 ), and mucin-secreting adenocarcinomas of the gastrointestinal tract ( Chapter 179 ), in which thrombotic rather than bleeding manifestations predominate. Treatment with all- trans -retinoic acid has greatly reduced the incidence of severe DIC in patients with acute promyelocytic leukemia ( Chapter 168 ). Up to 50% of patients develop coagulopathy following chimeric antigen receptor (CAR) T-cell therapy, often in the form of DIC. Likewise, coagulopathy with features of DIC can develop with hematopoietic stem cell transplantation ( Chapter 163 ). It is not known whether liver failure (see later) can cause DIC or whether its coexistence merely exacerbates intravascular coagulation because of impaired clearance of activated clotting factors, plasmin, and FDPs. Snake venom contains a variety of substances that can affect coagulation and endothelial permeability. Bites from rattlesnakes and other vipers can induce profound DIC by introduction of these exogenous toxins and release of endogenous tissue factor through tissue necrosis.
The likelihood and degree of DIC caused by trauma, surgery, and shock ( Chapter 92 ) are related to the extent of tissue damage and the organs involved. The brain is a particularly rich source of tissue factor, so traumatic brain injury ( Chapter 368 ) can precipitate acute DIC. Large aortic aneurysms ( Chapter 63 ), giant hemangiomas, and other vascular malformations can cause subclinical or clinical chronic DIC that is initiated locally within the abnormal vasculature but can spill into the systemic circulation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here