Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Puberty is defined by both biologic and social standards. Puberty is the time when there is an increase in sex steroid production, resulting in physical changes such as breast development in females and testicular enlargement in males, as well as maturation of processes required for future fertility. Puberty, also known as adolescence, is the time when children make the transition to adult patterns of behavior, which involve maturity, responsibility, and sexuality.
Various terms are used to discuss puberty ( Table 55.1 ). Bone age refers to the degree of epiphyseal calcification, width, and proximity to adjacent metaphyses and is a marker of physical maturity that normally corresponds to chronologic age. Dental age generally correlates with bone age. Bone age is derived by comparing a radiograph of the left hand and wrist to gender-appropriate standards in Greulich and Pyle’s bone age atlas. In infants and toddlers, a more accurate assessment of bone age can be determined from a radiograph of the hemi-skeleton, with primary attention to epiphyses of the long bones. Delayed or advanced bone age occurs in many conditions; bone age is strongly influenced by sex steroid production. The timing of the onset of puberty is usually more closely linked to the bone age than to the chronologic age when the two are significantly discordant. Regardless of chronologic age, linear growth ceases when the bone age reaches 15 years in females and 18 years in males.
|
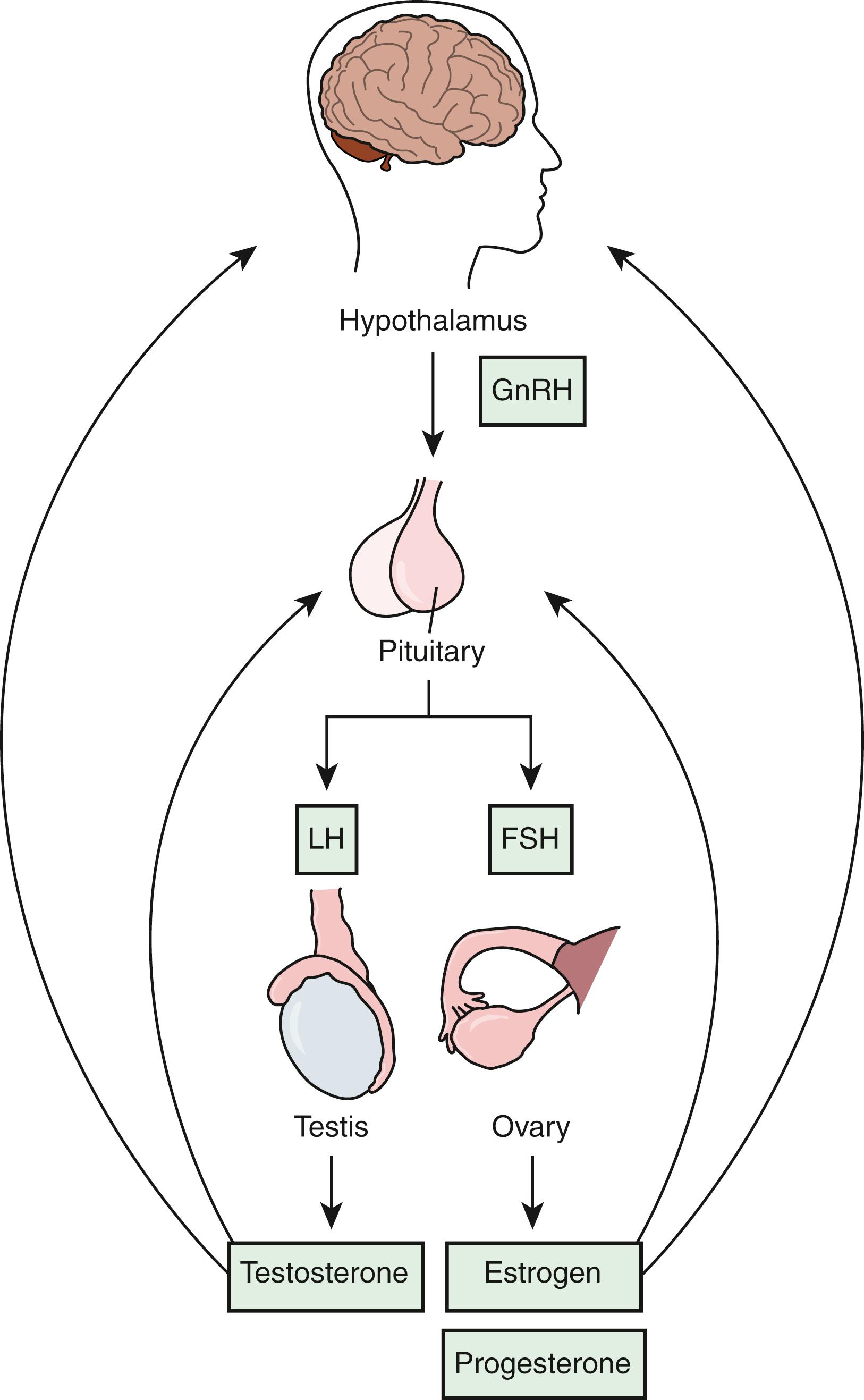
Puberty is controlled by the production of gonadotropin-releasing hormone (GnRH) in the anterior hypothalamus. GnRH-containing cell bodies project axons to the median eminence, where they terminate on the hypothalamic portal vessels. This system is referred to as the GnRH pulse generator . After GnRH reaches the anterior pituitary gland via the portal vasculature, it stimulates the production of both follicle-stimulating hormone (FSH) and luteinizing hormone (LH) by the gonadotroph cells. In females, both FSH and LH are required for estrogen production by ovarian granulosa cells. The regulated secretion of FSH and LH is also required for follicle growth, ovulation, and maintenance of the corpus luteum. In males, FSH regulates spermatogenesis by Sertoli cells within the seminiferous tubules, and LH activates Leydig cells to produce testosterone ( Fig. 55.1 ). Androgens cause development of male internal and external reproductive organs and secondary sexual characteristics in both sexes by binding to receptor proteins in the cells of target tissues. Sex steroids also exert a negative feedback effect on the pituitary gland and hypothalamus.
Maternal estrogens stimulate breast development in both male and female fetuses. Maternal estrogens also stimulate uterine developmental and endometrial growth; at birth, withdrawal of the high levels of maternal estrogen and placental progesterone causes the infant endometrium to regress or even slough and manifests as vaginal bleeding.
At birth, levels of LH and FSH in both sexes rise markedly and remain elevated for several months. In the female, FSH stimulates ovarian granulosa cells to produce 17β-estradiol sufficient to maintain prenatal breast development for up to 8 months of life. Estrogen-induced vaginal cornification is generally evident as abundant vaginal discharge at birth and is maintained as long as estrogens are produced. Ovarian size from birth to 3 months ranges from 0.7 to 3.6 cm 3 , decreasing to 2.7 cm 3 by 12 months and to 1.7 cm 3 by 24 months; this size persists until the onset of puberty. Ultrasound studies of the ovaries in normal infants show many microcysts.
Male breast development regresses rather quickly after birth. Elevated LH levels after birth stimulate Leydig cell production of testosterone for 6–12 months, leading to further genital development. Penis length increases from 3–5 cm in the full-term newborn to 4.5–6 cm by 2–3 years.
By 2 years of age, serum gonadotropin levels decrease, and thus serum sex steroid levels also decrease, frequently to levels undetectable by conventional assays.
Beginning approximately at ages 6–7 years in females and 7–8 years in males, adrenal androgen production begins to increase and can be detected by the presence of increasing concentrations of the weak adrenal androgen dehydroepiandrosterone (DHEA) and its sulfated derivative, DHEA sulfate (DHEAS). Despite these serum levels, there is initially no secondary sexual (pubic or axillary) hair development.
Beginning on average at about 10.5 years in females and 11.5 years in males, there is the return of activity of the hypothalamic GnRH pulse generator, leading to increased serum levels of FSH and LH. The kisspeptin ( KISS1 gene)/G-protein-coupled receptor (GPR54) (also called KISS1 receptor) system stimulates the GnRH neurons and is involved in the feedback regulation of the hypothalamic-pituitary-gonadal axis by gonadal steroids. The trigger mechanism for this resurgence is unknown, but it may be linked to attainment of a critical body mass or fat mass. Leptin, a hormone produced by fat cells, may be the connection between weight (fat mass) and pubertal events. In early puberty, the activity of the hypothalamic GnRH pulse generator is mostly evident overnight (sleep-entrained), with pulses increasing in number and amplitude and eventually occurring every 60–90 minutes. Over time, this process begins to occur during the daytime; there is always greater gonadotropin secretion at night. Because of the longer half-life of sex steroids, serum levels of estradiol and testosterone show little, if any, diurnal variation. Testosterone levels may be slightly higher in the morning with advancing puberty. There is central sensitivity to the negative feedback effects of sex steroids, leading to significant elevations of gonadotropins when sex steroid production is impaired. The function of the hypothalamic GnRH pulse generator can be accelerated in the setting of obesity, and LH and FSH secretion can revert to the prepubertal pattern in the setting of significant weight loss, as occurs in females with anorexia nervosa.
Usually within 6 months of the onset of this heightened GnRH pulse generator activity in females, there is also increasing production of androgens by the adrenal glands, the major source of androgens in females. In males, the testes are the main source of androgens, although male adrenarche also begins about 6 months after gonadarche.
In response to FSH, both testes and ovaries enlarge, starting gonadarche. Ovarian granulosa cells produce 17β-estradiol, which causes estrogen effects that generally occur in a fixed order ( Table 55.2 ). Growth increase is one of the early effects of estrogen. Growth is stimulated by estrogen-stimulated increased production of growth hormone and insulin-like growth factor 1. Estrogens along with growth hormone and thyroid hormones increase bone mineralization and growth.
|
In response to LH, testicular Leydig cells produce testosterone, which is converted to dihydrotestosterone (DHT), leading to androgen effects that generally occur in the same order ( Table 55.3 ).
|
Note that growth is not stimulated early in puberty by rising testosterone; in fact, during the phase when testosterone levels are beginning to rise, growth is usually slowed perceptibly from a prepubertal height velocity of perhaps 5 cm/yr to a velocity as slow as 4 cm/yr for 12–18 months. As levels of testosterone increase closer to 400 ng/dL and testis volume increases to between 10 and 12 mL, males make the transition to rapid growth. Rapid growth for males thus occurs for about 2 years in middle puberty, and slower growth continues for 2–3 more years.
Benign adolescent gynecomastia occurs in as many as 40–60% of normal males; enough estrogen relative to the amount of testosterone is produced so that breast development occurs. Gynecomastia usually starts in early to middle puberty (peak age, 13 years), before adult male concentrations of testosterone are achieved. It typically starts on one side and resolves within 2 years. Gynecomastia is more common in obese males, although true breast tissue in this setting is often difficult to distinguish from fat tissue (lipomastia).
Females begin puberty at an average age of 10.5 years (range, 8–13 years; mean ± 2.5 standard deviations [SD]). There are data suggesting that female puberty begins at an earlier age and that African-American females begin puberty about 1 year earlier than White females, but this is not universally accepted. In 85% of females, the first clinically detectable sign of puberty is breast development ( thelarche ), although ovarian enlargement, which is not clinically detectable in a strict sense, occurs first. Breast buds appear as small nodules either directly underneath the nipples or slightly off center, causing the areolae and nipples to be pushed out and sometimes cause minor, transient discomfort or itching as the skin around the nipple is stretched. Breast development may be unilateral and asymmetric in its earliest stages. Pubic hair usually begins to develop within the next 6 months; in approximately 15% of females, pubic hair precedes breast development. Such discordance has no clinical significance. The female adolescent growth spurt commences near the onset of thelarche, generally spanning a 2-year period between the ages of 11 and 13 years. Axillary hair generally begins, on average, between 12 and 13 years. Menarche, a rather late event in female puberty, occurs on average between 12.2 and 12.8 years, typically 2–2.5 years following thelarche. Menarche is often preceded by a whitish, non–foul-smelling vaginal discharge (physiologic leukorrhea) for up to 6 months. At the time of menarche, an adolescent female has reached 96.5% of her adult height potential. However, more linear growth may remain in clinical situations in which menarche occurs at a younger bone age than is typical for the average adolescent female. Menstrual cycles for the first 2 years after menarche are often anovulatory and irregular in frequency.
Males begin puberty at an average age of 11.5 years (range, 9–14 years; mean ± 2.5 SD). The first clinically detectable sign of puberty is testicular enlargement, a fact generally unknown to patients and their parents. From birth to the start of puberty, male testicular volumes range between 1 and 2 mL as determined by using an orchidometer, a series of ellipsoid models of varying volumes ( Fig. 55.2 ). Stretched penile length (measured with a rigid tape measure on the dorsum of the penis from the pubic symphysis to the tip of the nonerect penis without considering any foreskin tissue) averages about 3.5 cm (range, 2.8–4.2 cm) at birth and grows by an average of 2.5 cm until the start of puberty. The onset of male puberty is considered to have begun when at least one of the two testicles reaches 4 mL in volume. It takes approximately 5–6 years for the testicles to reach the average adult volume of 18 mL. Approximately 75–80% of the adult testicle consists of seminiferous tubules; testosterone-producing Leydig cells make up the remainder.

Within 6 months after the start of testicular enlargement, pubic hair can be found; pubic hair precedes testicular enlargement in approximately 15%. The presence of pubic hair is incorrectly considered the first evidence of puberty in males by both patients and parents. Pubic hair is followed by the development of axillary hair at approximately 14 years of age. During this time, penile enlargement also occurs, reaching a mean adult length of 12.4 ± 1.6 cm at 20 years of age. The male adolescent growth spurt typically occurs between the ages of 13 and 15 years, commencing when the testicular volumes reach 12 mL. By age 15 years, a male has attained 98% of his final adult height. The ability of adolescent males to produce sperm, as evidenced by detection of spermatozoa in urine samples, begins between 13.5 and 15 years.
Standardized staging of pubertal development in both sexes allows for comparison between children, as well as longitudinal monitoring of individual children ( Fig. 55.3 ).
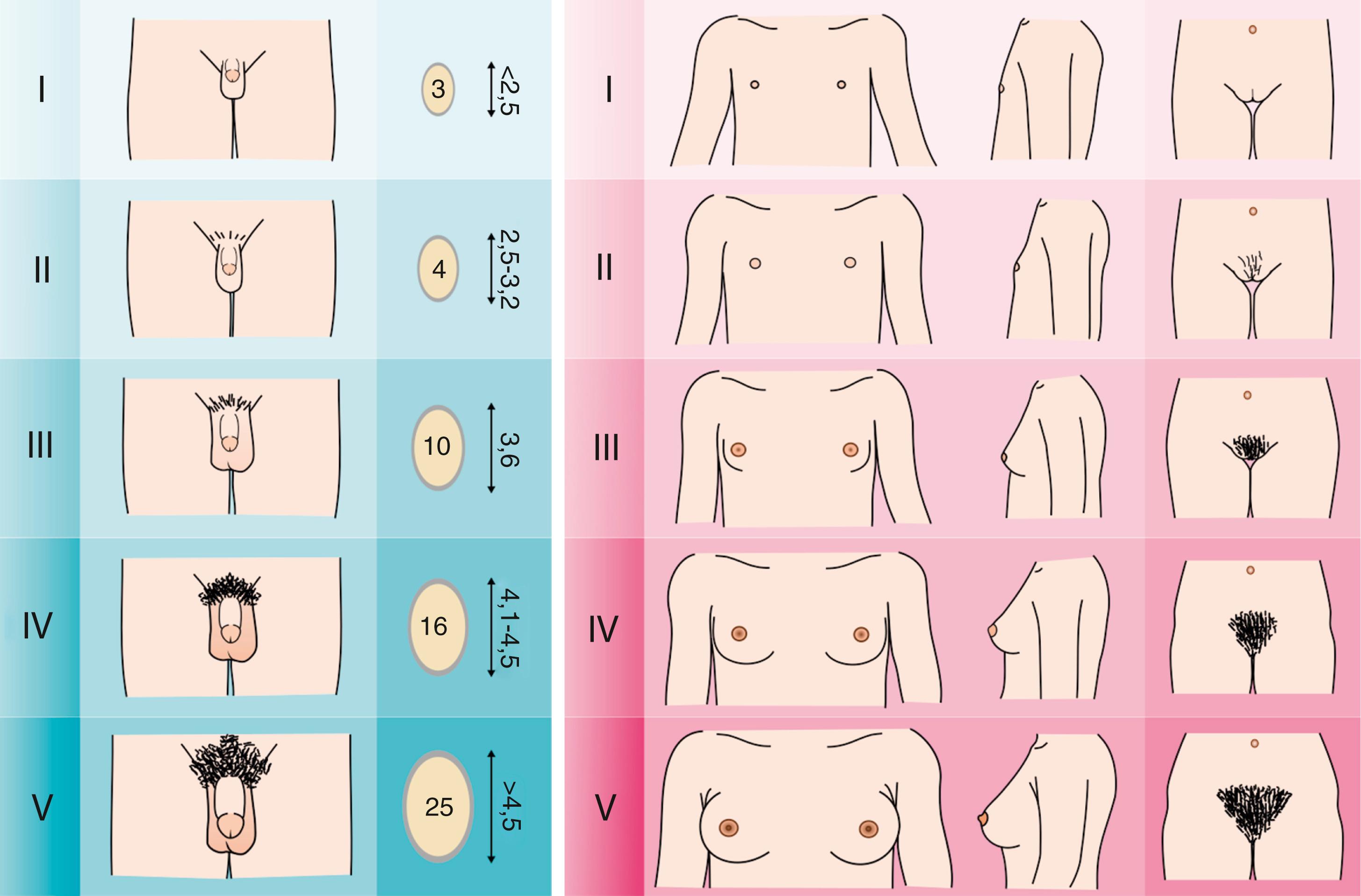
Breast development in females, genitalia in males, and pubic hair in both sexes are scored according to five-stage systems referred to as Tanner stages 1–5. Axillary hair in both sexes is rated by a three-stage system referred to as stages 1–3. Puberty itself is not staged because different components of puberty may occur at different stages.
For breast development, Tanner stage 1 refers to no breast development; Tanner stage 2, to the presence of just breast buds (one or two); Tanner stage 3, to the beginning of formation of the peripheral mound with elevation of the breast; Tanner stage 4, to a further increase in breast size, with the formation of the so-called “double contour,” in which the areola and papilla are both raised off the surface of the whole breast; and Tanner stage 5, to adult size, with a return to the single contour in which the surface of the areola is again flush with that of the breast. It may be difficult to differentiate between Tanner stages 3 and 5 because the only difference between these two stages is breast size (determined mostly by fat content). Thus, small breasts, especially in an older adolescent female, should not necessarily be construed as Tanner stage 3, especially if she has already menstruated, which typically occurs when the breasts have reached Tanner stage 4 and/or if women in the family typically have small breasts.
For external genitalia, Tanner stage 1 refers to the prepubertal state (testes <4 mL in volume); Tanner stage 2, to slight enlargement of the testes and scrotum; Tanner stage 3, to lengthening of the penis and further enlargement of the testes and scrotum; Tanner stage 4, to continued penile growth in both length and width with development of the glans; and Tanner stage 5, to adult appearance. An alternative, simplified, and equally accurate approach involves only sizing of the testicles, whereby 4 mL represents the start of puberty, 12 mL correlates with the start of the growth spurt, and 18 mL is the average adult size. In some cases, the appearance of pubic hair does not occur until the testicular volumes reach 12–15 mL. Testicular volumes may differ at all stages between sides but not usually by more than one size on a standard orchidometer. It is important not to confuse a hydrocele with an enlarged testis.
Tanner staging of pubic hair is similar in both sexes. Tanner stage 1 is defined by having no pubic hair. Tanner stage 2 is characterized by the presence of a few, countable strands of curly, coarse, pigmented hair along the labia minora in females or at the base of the penis and/or on the scrotum in males. Lighter and softer hair (lanugo) in the pubic region is not pubic hair. On occasion, especially in individuals from ethnic populations from Mediterranean countries or Northern India, there may be an extension of coarse body hair (hypertrichosis) to the pubic region that can be difficult to discern from pubic hair. Tanner stage 3 refers to the presence of coarser, darker, and curlier hairs, the number of which is no longer countable, which have spread more laterally. Tanner stage 4 refers to a thick, fully triangular pattern of hair growth, without spread to the thighs. Finally, Tanner stage 5 refers to the adult pattern in which there is spread of hair to the medial thighs. The designation Tanner stage 6 is used to describe hair growing up the linea alba, referring to the so-called male escutcheon.
Axillary hair is the simplest component of puberty to quantify. Stage 1 refers to the absence of any hair. Stage 2 refers to a countable number of curly, coarse, pigmented strands in at least one armpit. Stage 3 refers to the adult complement, which is merely more hair than is present in stage 2. For the individual with shaved axillae, it is safe to assume either stage 2 or stage 3 hair is present.
The timing of puberty is affected by familial patterns; both parents’ histories are important in assessing the child with early or late puberty. The following information is useful for establishing the parental effect:
Age of their mother’s menarche
Age their father began shaving on a daily basis
Age when their parents stopped growing
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here