Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Cells exist in, and must adapt to, an environment that is continually changing, reflecting not only physiological processes but also external influences such as drugs or toxins. As briefly discussed in Ch. 2 , if the stimulus is overwhelming, the cells undergo degeneration or cell death. However, many less noxious stimuli cause cells to adapt by altering their pattern of growth. This may occur in three main ways:
alteration in the size of cells
hypertrophy : increase in size of existing cells
atrophy : decrease in size of existing cells
increase in the number of cells (hyperplasia)
change in the differentiation of cells (metaplasia) .
In an organ composed of different types of cell, only one of the cell types may be affected, leading to a marked change in tissue appearance and function.
In all tissues, there is a population of undifferentiated cells (stem cells) that differ from mature cells throughout the body in three ways:
they are capable of dividing and renewing themselves (self-renewal)
they are unspecialised
they can give rise to specialised cell types.
Extrinsic to the cell, factors such as blood supply, innervation, hormonal stimulation, physical stress or biochemical alterations will determine the normal pattern of cell growth in an organ or tissue. Depending on the intrinsic characteristics of a particular cell type, a change in environment may result in a change in the growth pattern. Such responses are now recognised as being under the control of various growth factors that act upon specific cell surface receptors. Alterations in the concentrations of growth factors or the expression of growth factor receptors will result in altered cell growth.
Stem cells are undifferentiated cells with the capacity for self-renewal and differentiation into other specialised types of cells. Harnessing the regenerative/reparative characteristics of stem cells in treating disease is the subject of a large field of clinical research.
Stem cell therapy involves transferring intact, whole cells into a patient either from their own body (autologous) or from another person/donor (allogeneic) . Gene therapy involves transfer of DNA or RNA into a patient via a vector such as a virus or carrier cell. Gene and stem cell therapies are often used in combination to target diseases by altering the genetic structure of the cell before transfer into the patient.
The most common clinical application of stem cell therapy is bone marrow transplantation for the treatment of a variety of haematological diseases including forms of leukaemia, lymphoma and myeloma. However, the therapeutic repertoire of stem cell therapy is expanding to include treatment of diseases such as Parkinson’s disease, myocardial infarction and other types of cancer.
In bone marrow transplantation, the bone marrow must first be cleared of cells through a process known as myeloablation using a combination of both chemotherapy and radiotherapy. This process removes any remaining, diseased marrow and reduces the likelihood of transplant rejection. As above, stem cells can be sourced from the patient’s own marrow or blood (autologous transplant) or from a donor (allogeneic transplant) . The harvested haematopoietic stem cells can then be introduced to the patient through an intravenous infusion. Allogeneic transplants use stem cells collected from a donor with a tissue type that closely matches that of the recipient, often a family member. This reduces the risk of transplant rejection, known as graft versus host disease , where donor immune cells mount a response to the recipient’s tissues, particularly the skin, gastrointestinal tract and liver.
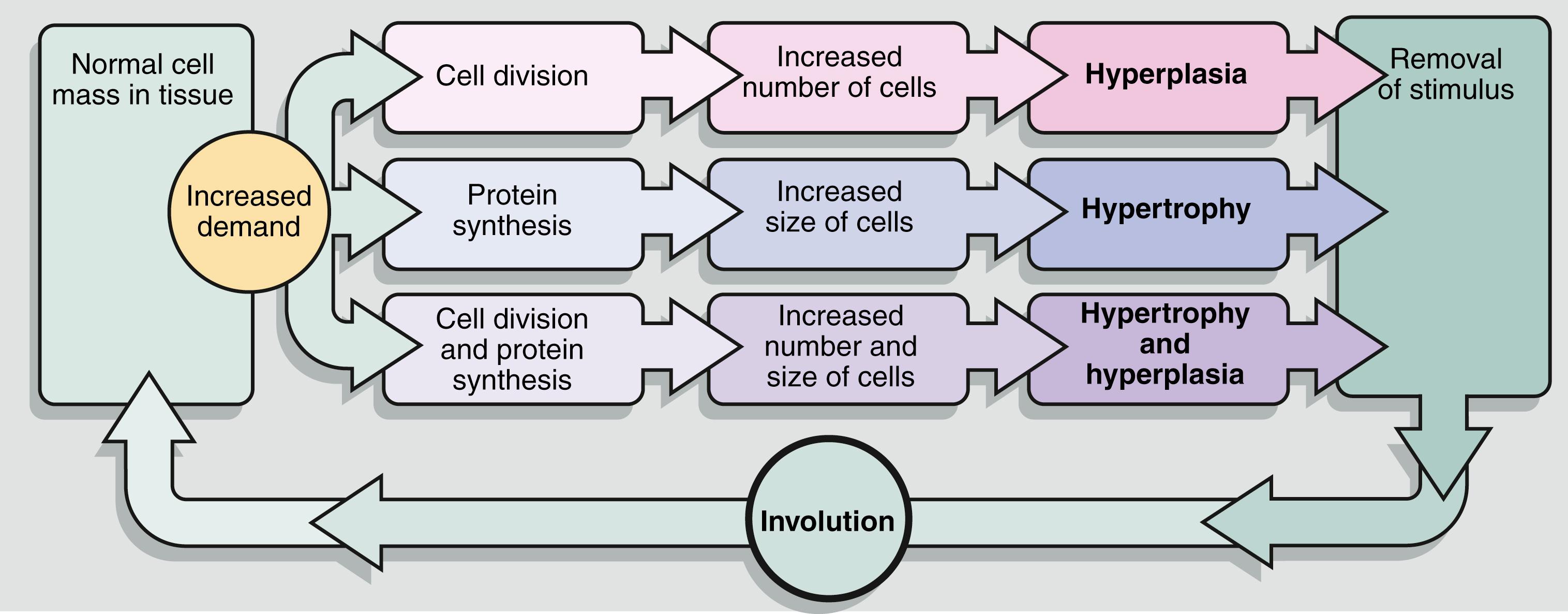
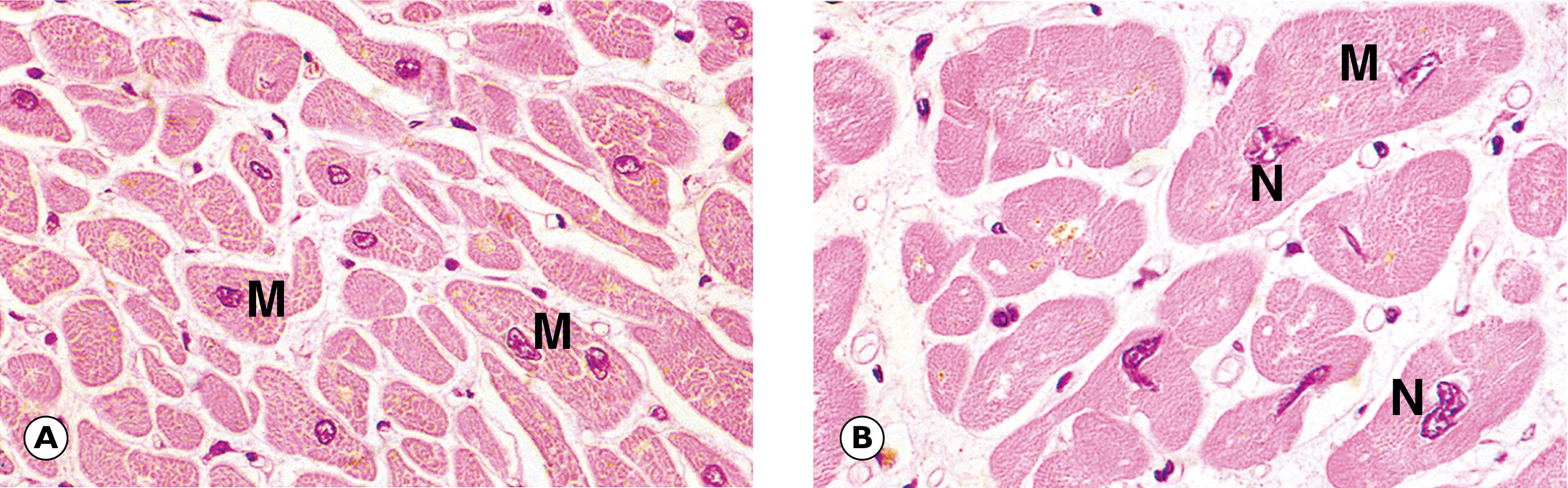
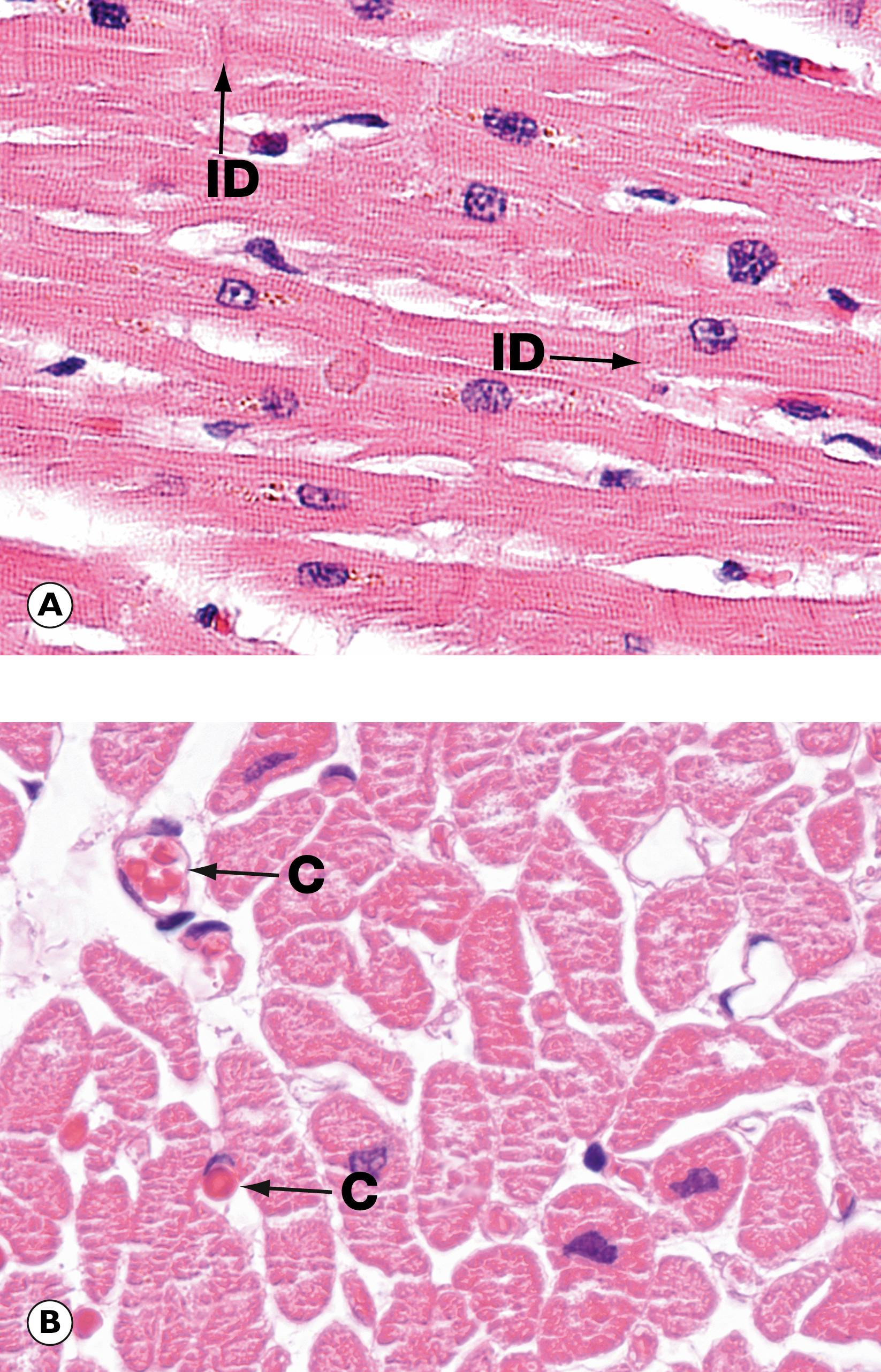
Organs may respond to environmental stimulation by an increase in functional cell mass through hyperplasia and/or hypertrophy ( Fig. 6.1 ). Hyperplasia occurs where cells are capable of dividing to generate an increased number of cells. In contrast, hypertrophy is typified by increase in cell size without an increase in cell number ( Fig. 6.2 ). An important feature of these forms of increased cell mass is that, following removal of the environmental stimulus, the altered pattern of growth ceases and the tissue may revert to its former state. Hypertrophy and hyperplasia can, in many circumstances, be regarded as normal physiological adaptations, as exemplified by exercise-induced skeletal muscle hypertrophy and the hyperplasia and hypertrophy of the myometrium during pregnancy.
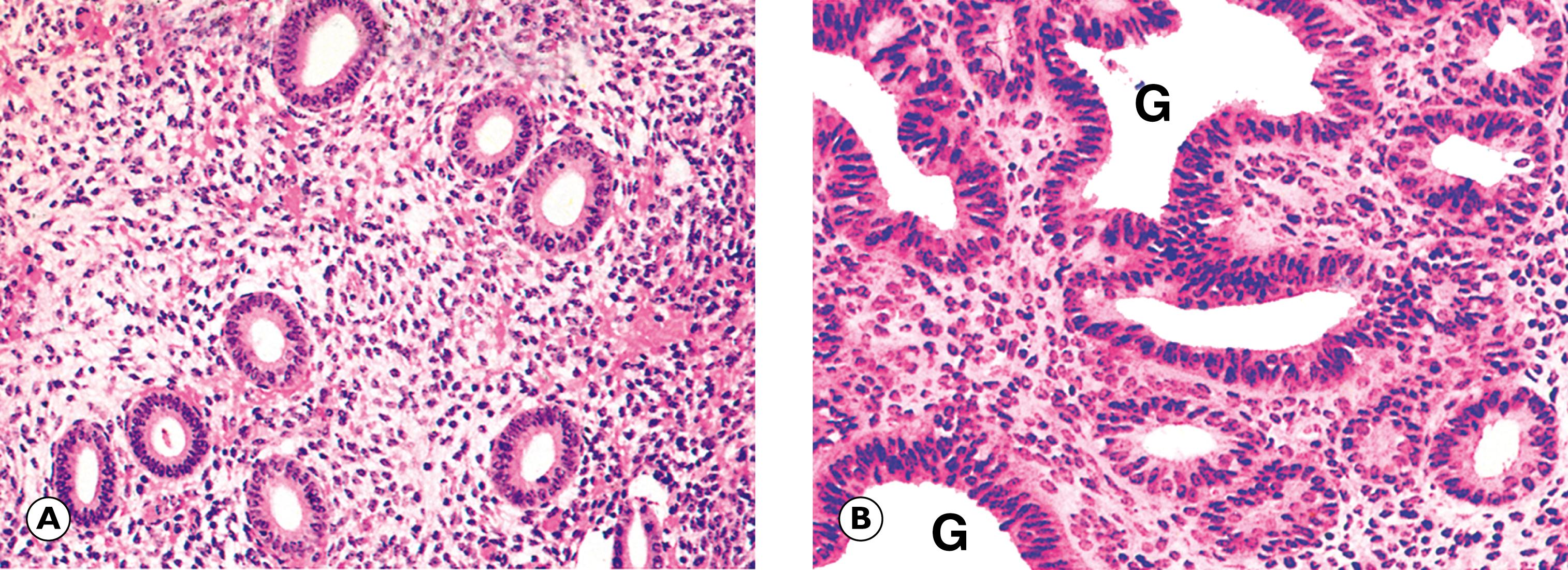
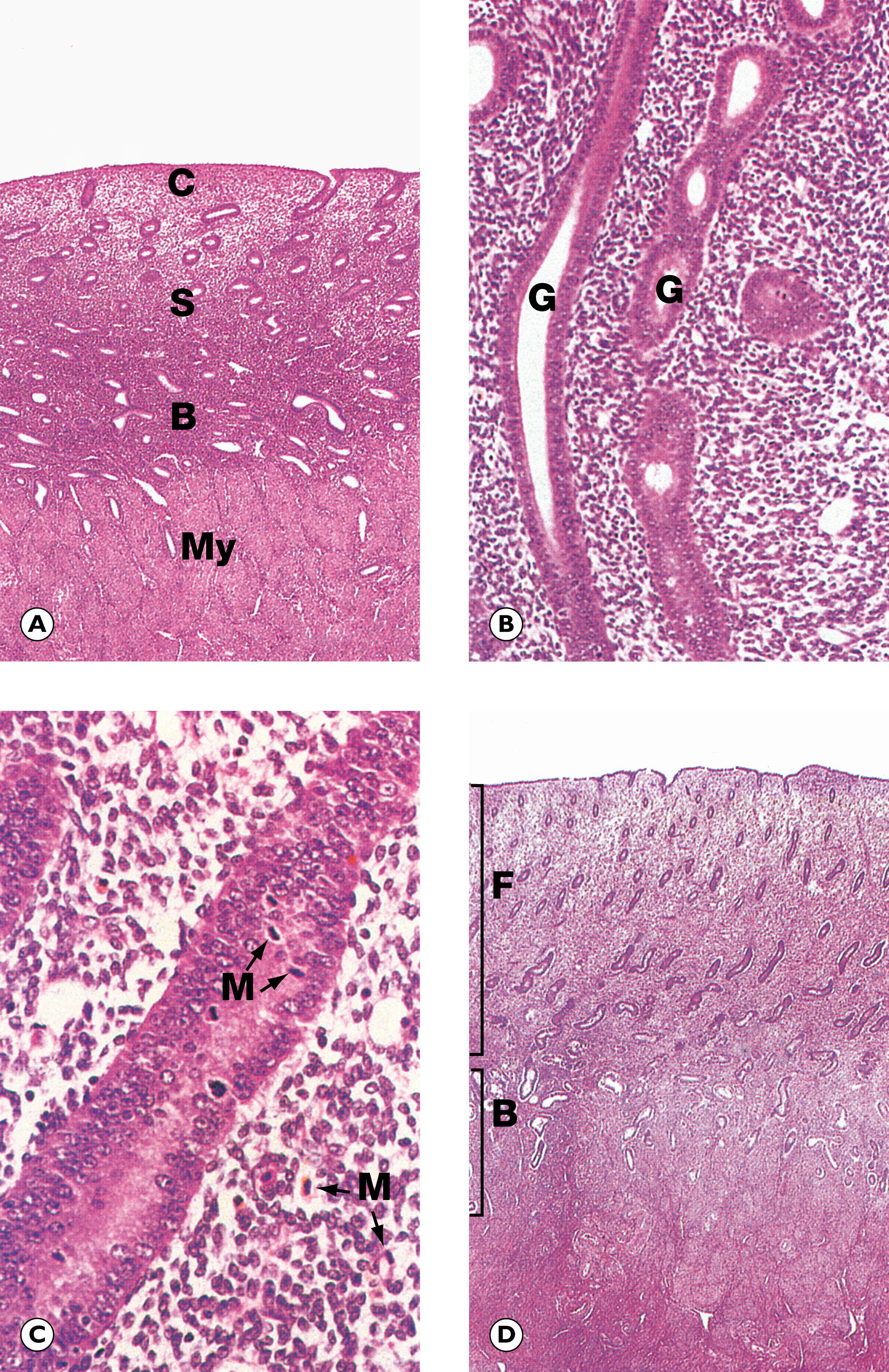
Many pathological stimuli invoke the responses of hypertrophy and hyperplasia and it appears these responses occur in many cases by the same mechanism that induces the normal physiological response ( Fig. 6.3 ). Thus, in the first part of the menstrual cycle, the endometrium proliferates with elongation of glands and increased numbers of epithelial cells. When an excessive concentration of oestrogen acts on the endometrium, such as during the menopause or owing to injudicious hormone replacement therapy, similar but more pronounced changes occur, leading to crowding of endometrial glands. Removing the stimulus to this excess growth can result in a regression. This contrasts with the abnormal, uncontrolled proliferation of cells associated with the development of cancers, referred to as neoplasia (see Ch. 7 ) where growth is independent of any external stimuli. Therefore, hyperplastic tissue is not of itself neoplastic but may carry with it an increased risk of neoplastic change. Thus, hyperplastic endometrium is more likely than normal endometrium to progress to cancer. This risk is increased further when the hyperplasia is combined with cytologic atypia (termed atypical hyperplasia ) ( E-Fig. 6.1 G ).
For poorly understood reasons, the process of hyperplasia may not be uniform throughout an organ or tissue and, in these instances, nodules of excessive cell growth arise in between areas of unaltered cell growth. This phenomenon, known as nodular hyperplasia , is seen in the thyroid gland (see Fig. 20.5), the adrenal gland (see Fig. 20.9) and the prostate gland (see Fig. 19.8) .
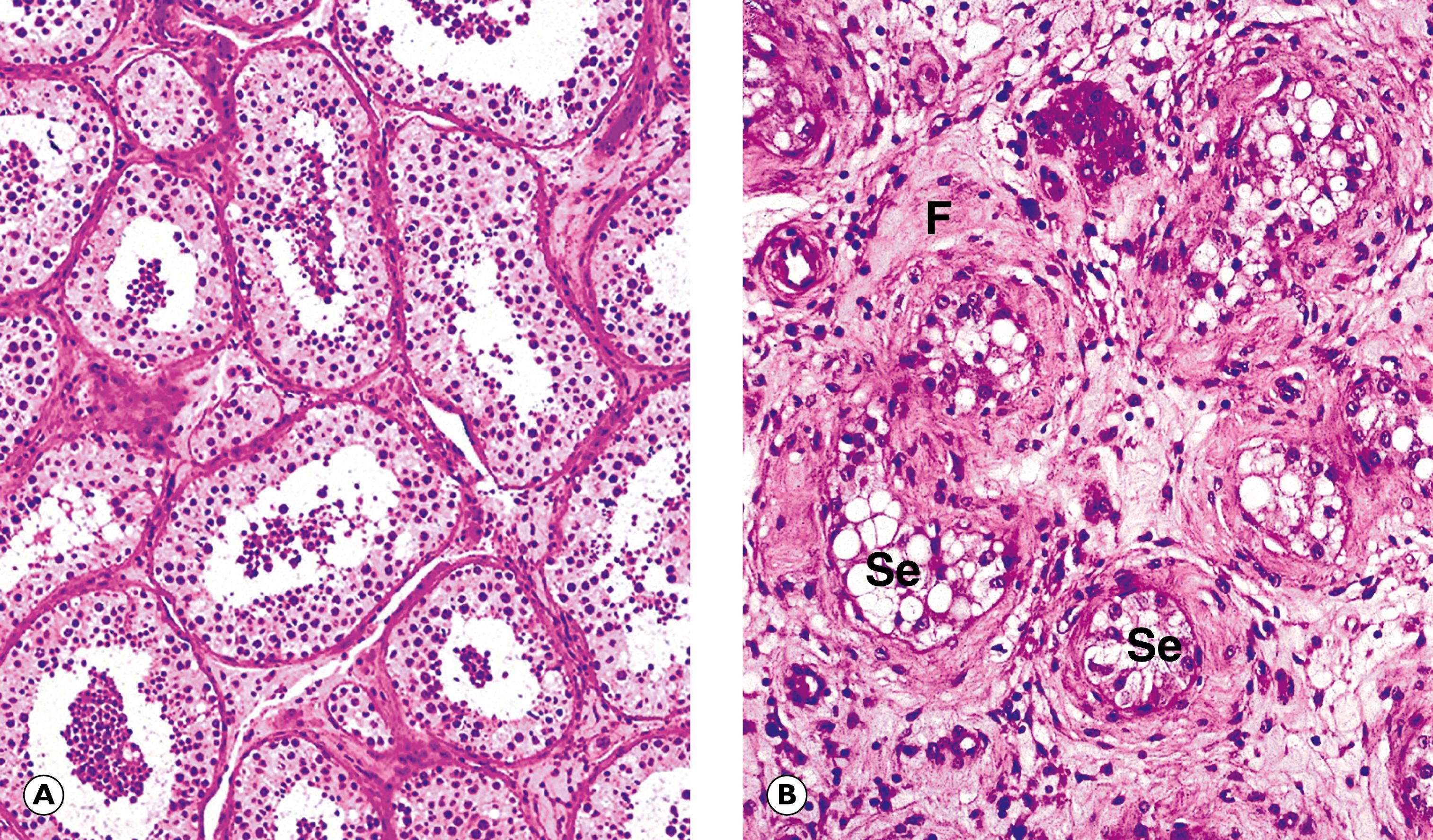
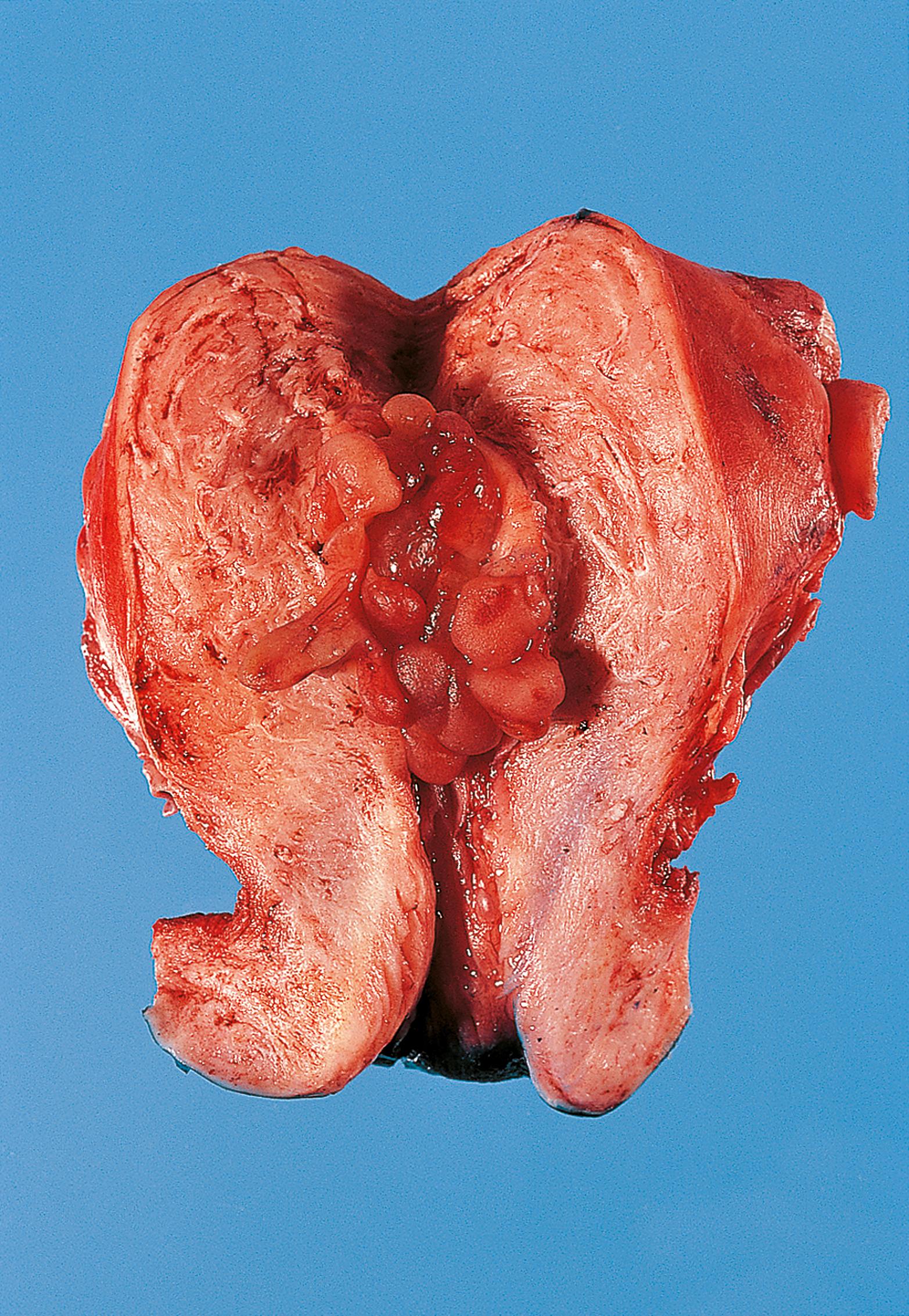
G gland M myocardial cell N nucleus
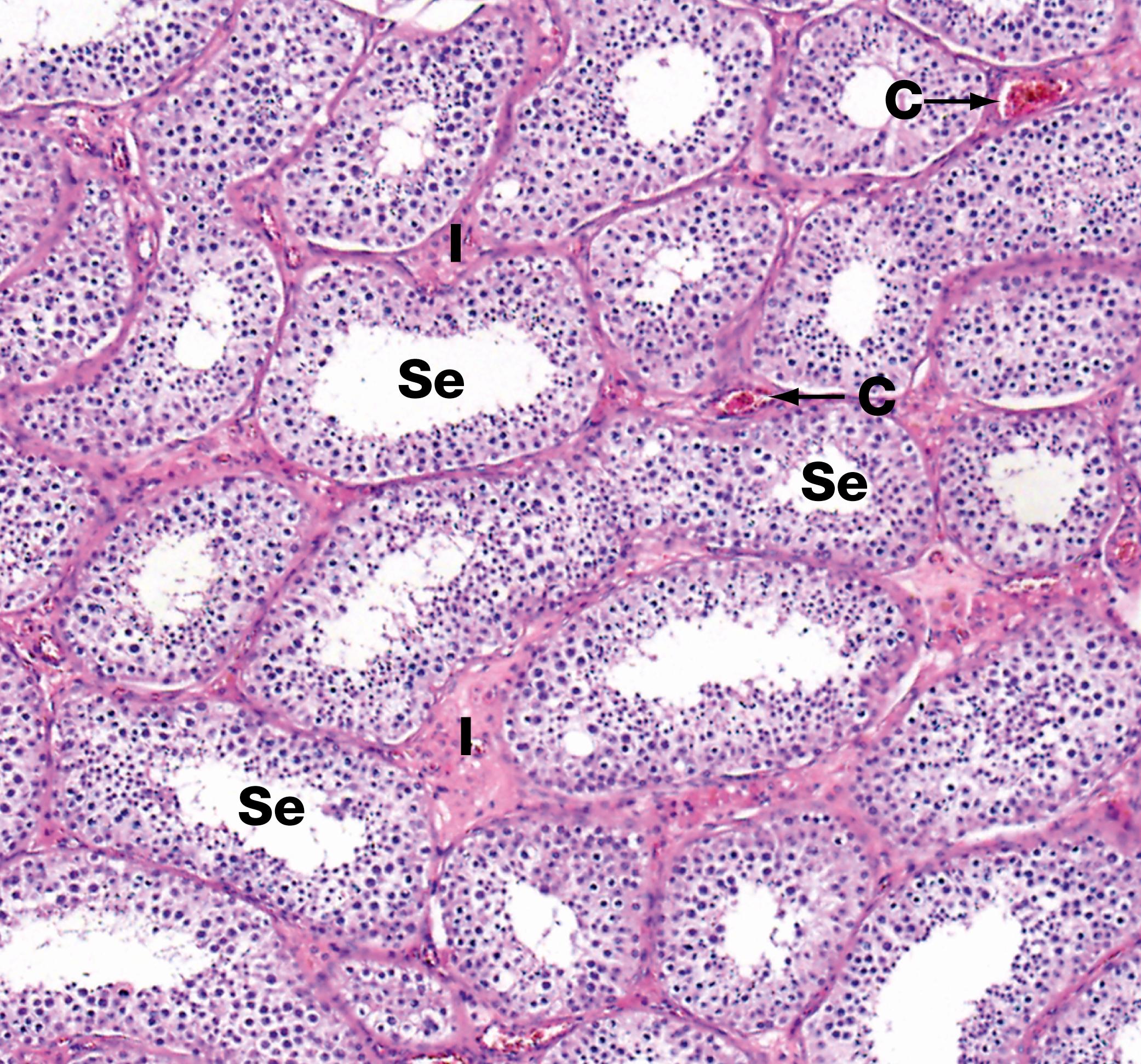
When the functional cell mass in a tissue is reduced, the tissue is said to have undergone atrophy . The mechanisms of atrophy may involve reduction in cell volume and/or in cell number, both leading to a reduction in functional capacity. Macroscopically, the appearance of the tissue depends on whether the functional cells lost are replaced by other tissue. Commonly, when atrophy occurs, the lost cells are replaced by either adipose or fibrous tissue, often maintaining the overall size of the organ. When adipose or fibrous replacement does not occur, the overall size of the organ is reduced. Examples are the testis in the elderly ( Fig. 6.4 ) and the adrenal gland when suppressed by exogenous steroid administration (see Fig. 20.9). Atrophy may occur as a physiological event (termed involution ), such as in embryologic development or the normal involution of the thymus during adolescence.
A variety of causes of atrophy is recognised, in general conditions opposite to those causing hypertrophy or hyperplasia. Thus, disuse of skeletal muscle will result in a loss of cell mass (disuse atrophy) . Removal of endocrine stimulation causes atrophy in target organs. Reduction in blood supply to a tissue may result in loss of functional cells (ischaemic atrophy) , a situation commonly encountered in the kidney.
Atrophy must be distinguished from hypoplasia , a condition where there is incomplete growth of an organ, and agenesis , where there is complete failure of growth of an organ during embryological development.
In many atrophic tissues a granular, brown pigment (lipofuscin) , which is composed of degenerate lipid material in lysosomal granules, may accumulate within the shrunken cells. It is most readily identified in atrophic myocardial fibres of the hearts of elderly people, giving rise to the term brown atrophy .
Hyaline is a term used to describe replacement of tissue by an amorphous pink-staining material similar to basement membrane matrix. It is a common end result of atrophy or cell damage, being frequently accompanied by fibrosis.
Under certain circumstances, cells may undergo a change in differentiation to another, mature, differentiated cell type (metaplasia) . This is thought to be an adaptive response that produces cells better equipped to withstand an environmental change (usually pathological). For example, in the bronchi the specialised columnar respiratory epithelium may be replaced by squamous epithelium under the influence of chronic irritation by cigarette smoke (squamous metaplasia) . Similarly, in response to environmental changes during the reproductive cycle, the normal columnar endocervical epithelium is replaced by a stratified squamous epithelium ( Fig. 6.5A ).
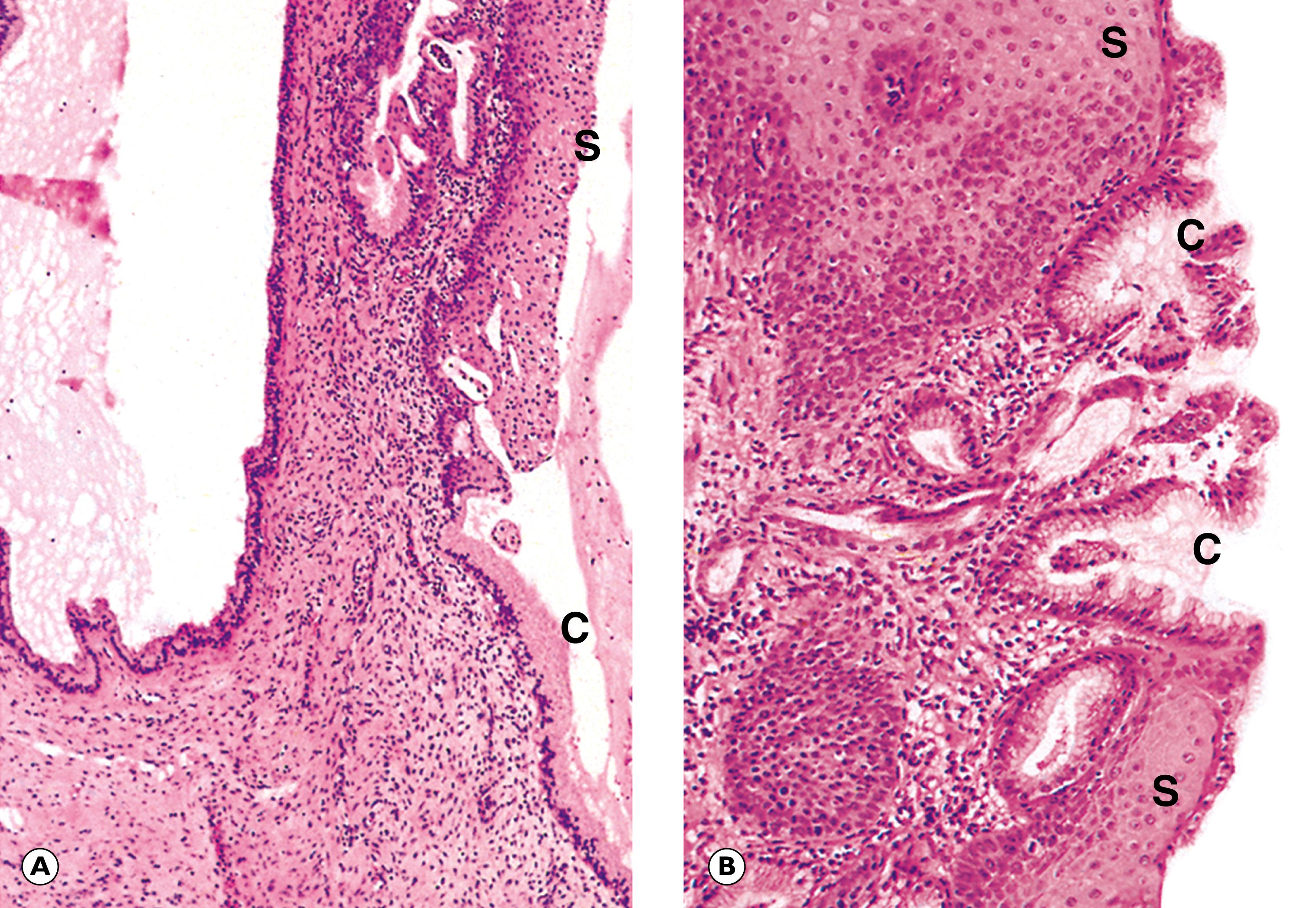
In the lower oesophagus, the normal stratified squamous epithelium may, in response to acid reflux from the stomach, be replaced by gastric (gastric metaplasia) or small intestinal (intestinal metaplasia) mucosa ( Fig. 6.5B ). In common with metaplasia at other sites, the basic alteration appears to occur in the stem cells of the tissue such that, rather than differentiating into a squamous cell, they mature instead into a mucus-producing columnar cell that is better able to protect itself from an acid environment. When the stimulus is removed, the stem cells may revert to producing differentiated cells of the original type.
Metaplasia most commonly occurs in epithelial tissues but may also be seen in mesodermal tissues; for example, areas of fibrous tissue exposed to chronic trauma may form bone (osseous metaplasia) . Metaplasia may co-exist with hyperplasia and, more importantly, dysplasia (see Ch. 7 ).
C columnar epithelium F fibrous tissue S squamous epithelium Se Sertoli cells
| Main features | Examples | Figure | |
|---|---|---|---|
| Hypertrophy | Increase in size of existing cells | Myocardium in hypertension | 6.2 |
| Skeletal muscle with exercise | |||
| Hyperplasia | Increase in number of cells | Endometrium under oestrogenic stimulation | 6.3 |
| Atrophy | Reduction in cell size and/or number | Ischaemic atrophy of kidney | |
| ‘Brown atrophy’ of myocardium | |||
| Testicular atrophy | 6.4 | ||
| Metaplasia | Change of differentiation in a cell | Squamous metaplasia of cervix | 6.5A |
| Gastric/intestinal metaplasia of lower oesophagus | 6.5B |

Cells continually adapt to physiological and pathological stimuli by a variety of mechanisms. Which of these adaptive responses will not resolve or reverse following removal of the stimulus? Choose ONE answer.
Hypertrophy
Hyperplasia
Neoplasia
Metaplasia
Atrophy
Which of the following is NOT characteristic of stem cells? (Select ONE answer)
They are undifferentiated cells.
They are capable of self-renewal.
They are specialised cells.
They can be used in the treatment of patients with haematological diseases.
They divide to give rise to specialised cell types.
Which of the following is NOT an example of involution? Select ONE answer.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here