Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The entities described in this section are a select group taken from the large number of diseases that affect the skin. They have been chosen to encompass the types of non-neoplastic material generally seen in surgical pathology laboratories. Many of the infrequently biopsied, histologically nonspecific, and rare dermatoses are excluded. Their characteristics are described in texts devoted wholly to dermatopathology and in the dermatologic literature.
The fact that isolated histopathologic analysis has distinct limitations becomes more evident in the evaluation of the reactive processes associated with diseases of the skin than in most other organs. It is imperative that the clinical differential diagnosis be correlated with the gross and microscopic observations to render a clinically meaningful diagnosis.
Skin biopsies are often small and have minimal gross changes. Ideally, the lesion should be examined by the pathologist on the patient, but, in lieu of this, an accurate clinical description and differential diagnosis should accompany each biopsy. With the ease of digital photography, the inclusion of a clinical image can be extremely useful in the interpretation of the biopsy findings. All biopsies should be taken from grossly characteristic areas. It is a waste of time and money to biopsy ruptured bullae, secondarily infected or heavily scratched areas, or the incipient or involuting lesion. Multiple biopsies may be advisable when the lesions present differing forms and stages. In diseases in which the expected changes are quantitative rather than qualitative (i.e. hyperkeratosis, acanthosis, increase in dermal thickness), the evaluation of these changes is best made by taking a punch biopsy also of clinically normal skin nearby, which represents the best possible control. Formalin, 10% buffered, is an adequate and widely available fixative. Bouin and Zenker fixatives may be used but have no unique merits. Incisional and punch biopsies can be kept from curling during fixation by placing them on a piece of file card prior to immersion. When the specimen is 0.3 mm or less in diameter, it is best processed into paraffin in one piece. It may then be sampled at various levels in the block. This prevents loss of tissue during the facing-up of the block and allows more adequate sampling. These technical niceties prevent delays, mishaps, and some mistakes.
The skin or integument is a complex organ with many functions and with three main anatomic components: epidermis and skin adnexa, melanocytic system, and dermis and subcutis.
The epidermis is a stratified squamous epithelium that differentiates to form the outer protective layer of keratin. It is composed of keratinocytes arranged in four layers: basal, squamous (prickle, malpighian), granular, and cornified (horny). The basal cells are the mitotically active cells that give rise to all other keratinocytes; they contain low-molecular-weight keratin and are separated from the dermis by a continuous basal layer, to which they are attached by hemidesmosomes. The basal membrane is a complex antigenic structure that plays an important role in many cutaneous diseases. The dermoepidermal junction is thrown into undulating folds of interlocking ridges of epidermis (rete ridges) and dermal papillae. Thus the undersurface of the epidermis seen in whole mounts presents an anastomosing and reticulated pattern of ridges and valleys. The pattern and size of these ridges vary from area to area. With age, they diminish in size, and the dermoepidermal junction becomes flattened.
The squamous layer is composed of several layers of cells, which become larger, more flattened, and more eosinophilic as they approach the surface. This correlates with the intracytoplasmic accumulation of filaments, which are the precursors of keratin, and a diminution of ribosomes. Some cells in the squamous layer exhibit a clear, vacuolated cytoplasm (sometimes resulting in nuclear indentation), which should not be confused with melanocytes or Paget cells. Melanocytes and Paget cells, unlike vacuolated keratinocytes, have cytoplasm clinging to their nuclei. When the cells are separated, as a result of fixation and dehydration or intercellular edema, these areas of attachment are seen via the light microscope as fine spiny (“intercellular”) bridges, with a dot-like structure at their center (Bizzozero nodule), representing the desmosome. The epidermal cells are not a syncytium, and true intercellular bridges do not exist. Destruction of these attachments causes the cells to lose their cohesion. This process, termed acantholysis, is seen in pemphigus vulgaris and related diseases. The granular layer is composed of one to three layers of flattened cells containing keratohyaline granules. These coarse, intensely basophilic granules are rich in histidine and represent the precursors of the protein filaggrin, which is responsible for the aggregation of keratin filaments. The cornified layer contains multiple layers of polyhedral cells that have lost their nuclei and that are arranged in a basket-weave pattern (except for the acral regions, in which this layer is thick and compact). The skin from the palms and soles features an additional layer—the stratum lucidum—located between the granular and the cornified layers and appearing as a homogeneous eosinophilic zone.
The major proteins of basal keratinocytes are keratins 5 and 14, which form an extensive network of 10-nm cytoskeletal filaments. As keratinocytes differentiate, they downregulate this pair of keratins and switch on expression of other pairs, the nature of which is dependent on the site. In the epidermis, terminally differentiated keratinocytes express keratins 1 and 10.
The keratinization cycle usually takes 30–45 days. Many dermatoses result in alterations in the pattern and speed of this process. Abnormal keratinization may be manifest by hyperkeratosis, in which the stratum corneum is thickened, usually in association with a more prominent granular layer, or by parakeratosis, in which the cells of the stratum corneum retain their nuclei and the granular layer is diminished or absent.
Certain descriptive terms are applied to alterations in the pattern of the epidermis. It may become atrophic or thinned with age or disease. It may be thickened, and as it proliferates the rete ridges extend deeper into the dermis, a process known as acanthosis . Outward overgrowth of the epidermis accompanied by elongation of the dermal papillae is papillomatosis . A degenerative process in which the basal cells become vacuolated, separated, and disorganized is called liquefactive or hydropic degeneration . Various combinations of these changes are seen in the dermatoses, and this descriptive jargon allows succinct communication.
In addition to keratinocytes, the normal epidermis contains melanocytes, Langerhans cells, and Merkel cells. Melanocytes are described in more detail in the chapter on cutaneous neoplasms. Langerhans cells are bone marrow–derived dendritic cells whose function is to present antigens to immunologically competent T cells. They are scattered throughout the upper part of the squamous layer and are difficult to identify in routinely stained sections. Ultrastructurally, they have a characteristic organelle—the Birbeck granule—a rod-shaped structure with zipper-like striations and sometimes a bulbous end. Immunohistochemically, they express CD1a, langherin, and S-100 protein; they have receptor sites for the Fc portion of the immunoglobulin G (IgG) molecule and the third component of complement.
Merkel cells, also extremely difficult to identify in hematoxylin and eosin (H&E) sections and even with special stains, are concentrated in the glabrous skin of the digits, lips, outer root sheath of hair follicles, and tactile hair disks. Ultrastructurally, they contain cytoplasmic dense core (neurosecretory-type) granules, often arranged beneath the cell membrane or located within unmyelinated neurites. Spinous processes projecting from the cytoplasm anchor these cells to adjacent keratinocytes. Immunohistochemically, Merkel cells are reactive for neuron-specific enolase (NSE), neurofilaments, keratin (including CK20), chromogranin, and synaptophysin.
The skin adnexa are represented by the hair follicles, sebaceous glands, sweat (eccrine) glands, and apocrine glands. The hair follicle, sebaceous gland, erector pili muscle, and (in certain regions) the apocrine gland constitute a functional complex known as the pilar unit .
The hair follicle is responsible for the formation of hair, a cyclic process that proceeds in three phases: anagen or growing phase, catagen or involuting phase, and telogen or resting phase. The mitotically active cells of the hair follicles lining the dermal papilla are the matrix (generative) cells. These cells give rise to the hair shaft and the inner root sheath . The outer layer of the latter structure is surrounded by a layer of large clear (glycogen-rich) cells known as the outer root sheath . At the level of the isthmus, these cells undergo an abrupt type of keratinization, which occurs without the interposition of a granular layer; this is referred to as trichilemmal keratinization and, by extension, the layer itself is known as the trichilemmal sheath . By contrast, the keratinization in the infundibular portion of the follicle is similar to that of the adjacent epidermis. It is not unusual to find Demodex folliculorum mites, clumps of Staphylococcus epidermidis , and yeasts of Malassezia (formerly Pityrosporum ) inside the pilar infundibulum.
The sebaceous glands are lobulated structures containing an outer layer of germinative cells that, as they differentiate, move toward the inside and accumulate intracytoplasmic lipid droplets. These result in a typical multivacuolated appearance, with multiple indentations of the centrally located nucleus. The excretory duct of the sebaceous glands opens into the infundibulum of the hair follicle.
Sweat glands are of three types: eccrine (responsible for thermoregulation and therefore the only “true” sweat glands), apocrine , and mixed (apoeccrine glands). Eccrine sweat glands are tubular structures with a secretory and an excretory portion. The secretory coil, located in the deep dermis or sometimes in the subcutis, is composed of secretory cells (further divided into clear and dark cells) and myoepithelial cells. The excretory portion is composed of a dermal (straight) and an intraepidermal (spiral) portion, the latter also known as the acrosyringium .
Although the apocrine glands are concentrated in the axillae, groin, and perineum, they also occur in small numbers on the face and elsewhere. Like eccrine glands, they have a secretory and an excretory component. It is the former that gives them their highly characteristic appearance. The cells have an abundant acidophilic cytoplasm, which may contain lipid, iron, and lipofuscin.
Immunohistochemically, the various epithelial components of eccrine and apocrine glands stain for carcinoembryonic antigen (CEA), epithelial membrane antigen (EMA), keratin, S-100 protein, the enzyme carbonic anhydrase, ferritin, secretory immunoglobulin, and pregnancy-specific β-I-glycoprotein (SPI). In addition, apocrine glands express the marker known as gross cystic disease fluid protein (GCDFP)-15. The myoepithelial cells stain for actin, calponin, caldesmon, S-100 protein, and Sox10.
The epidermal adnexa are seldom the sites of primary changes. However, diagnostic changes do occur: heterotopias as in nevus sebaceous of Jadassohn, in which apocrine glands are found in the scalp; pigmentation of eccrine gland basement membranes in argyria and hemochromatosis; atrophy, as in scleroderma; duct obstruction with subsequent retention, as in the various forms of miliaria; and deposition of aggregates of granules of mucoprotein in the eccrine gland cells in myxedematous patients.
The dermis is a connective tissue structure composed of collagen and elastic fibers bathed in ground substance and containing adnexal structures, vessels, and nerves. It is divided into two layers: adventitial and reticular. The adventitial dermis comprises the superficial layer located immediately beneath the epidermis—the papillary dermis—and that located around adnexal structures—the periadnexal dermis.
The adventitial dermis is largely composed of a delicate network of collagen fibers (mainly type I, with a scattering of type III or “reticulin” fibers), whereas the reticular dermis is made up of thick bundles of type I collagen intermixed with thick elastic fibers.
The thickness of the dermis varies considerably from area to area; it is particularly thick in the back, a feature that is sometimes misinterpreted as being abnormal in biopsies.
The subcutaneous tissue (subcutis) is composed of lobules of mature adipose tissue separated by thin bands of connective tissue interlobular septa. The dermal blood vessels are divided into a deep plexus (located in the reticular dermis) and a superficial plexus (located in the papillary dermis), with communicating vessels in between. From the superficial vascular plexus, capillary loops extend into the dermal papillae. The acral skin contains specialized arteriovenous anastomoses—the Sucquet–Hoyer canals —surrounded by a row of modified smooth muscle—the glomus cells —which have a round shape, clear cytoplasm, and well-defined cytoplasmic borders. The lymphatics of the skin are also divided into a deep and a superficial plexus.
Specialized nerve end organs present in the skin are the Wagner–Meissner corpuscles (with a tactile function; mainly located in the papillary dermis of the palms and soles) and Pacinian corpuscles (sensitive to pressure; mainly located in the deep dermis and subcutis of weight-bearing areas). With age, and more so in areas exposed to sunlight, the collagen and elastica undergo structural and tinctorial changes called solar (actinic) elastosis . These changes should not be attributed to some suspect disease and should be distinguished from pathologic connective tissue changes, such as increased dermal mucin deposition.
The dermis is the site of inflammatory reactions. In normal skin, a few fibroblasts, macrophages, mast cells, lymphocytes, and dermal dendrocytes are present. The latter represent a population of mononuclear dendritic cells located in the papillary and upper reticular dermis and are thought to function as antigen-presenting cells. They express the coagulation factor XIIIa (also known as fibrin stabilizing factor) and are known to increase in number in a large number of inflammatory and neoplastic disorders.
The perivascular and periadnexal spaces and the papillary layer of the dermis are the usual sites in which inflammatory cells aggregate. Certain dermatoses, such as lichen planus and chronic discoid lupus erythematosus, have distinct patterns of inflammatory reaction. Others, such as urticaria pigmentosa, have a specific cellular population. Changes in the nerves, visible in sections stained with H&E, are infrequent but when present are of note (see section on leprosy ).
As previously mentioned, a thorough and detailed discussion of inflammatory dermatoses is beyond the scope of this text and the reader should seek texts devoted to dermatopathology for a complete discussion of inflammatory diseases of the skin. Nevertheless, biopsies of inflammatory diseases are still encountered with relative frequency by surgical pathologists. Therefore some familiarity with these entities is necessary. Approaching inflammatory dermatoses based on the pattern of inflammation is a rational approach that results in more refined diagnoses. Multiple different patterns exist. For the purposes of this text, a simplified approach will be used. Broadly speaking, the inflammatory reaction patterns can be divided into five groups: (1) dermatoses with significant epidermal changes, (2) dermatoses with dermal inflammation without significant epidermal change, (3) sclerosing diseases, (4) panniculitis, and (5) immunobullous/vesiculobullous disease. These will be discussed in turn. There are also a variety of diseases with specific etiologies (e.g. infections) and miscellaneous disorders that will be described separately at the end of the chapter.
There are three primary patterns within this group: spongiotic, psoriasiform, and interface dermatitis. Spongiotic dermatitis is characterized by the accumulation of edema fluid within the epidermis, resulting in the epidermal keratinocytes being pulled apart by hydrostatic forces. The psoriasiform pattern is characterized by epidermal acanthosis (hyperplasia) without significant spongiosis. There is often overlap between these patterns. The interface pattern is characterized by a dermal infiltrate, either lichenoid or perivascular, that is associated with damage to the epidermis along the dermoepidermal junction with basal vacuolization and dyskeratotic keratinocytes. Select entities within these groups will be discussed.
Spongiotic dermatitis is a reaction pattern that is most commonly seen in the clinical spectrum of eczematous dermatitis, including allergic contact dermatitis, nummular dermatitis, atopic dermatitis, dyshidrotic eczema, stasis dermatitis, and eczematous drug reactions. All of these dermatoses are characterized by the presence of intraepidermal edema (spongiosis). Histologically, these entities resemble one another and differentiating them relies on knowledge of the clinical presentation rather than histologic features in most cases. That being said, this group of clinical disorders is frequently biopsied and have common histologic features.
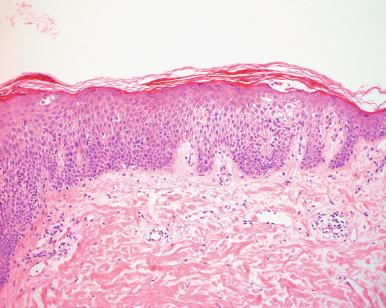
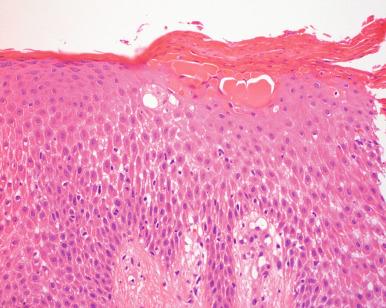
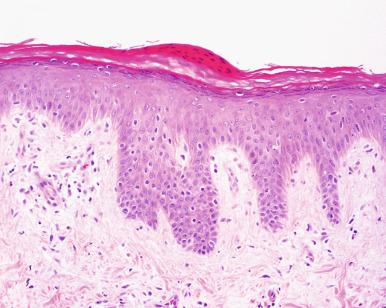
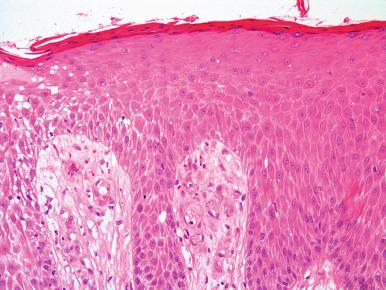
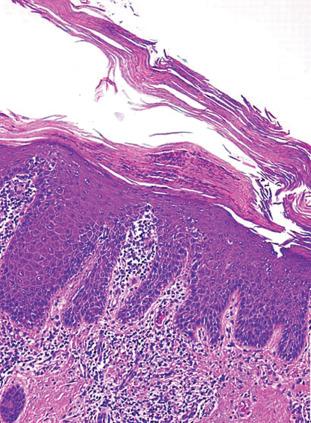
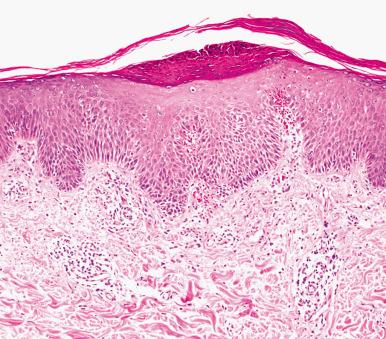
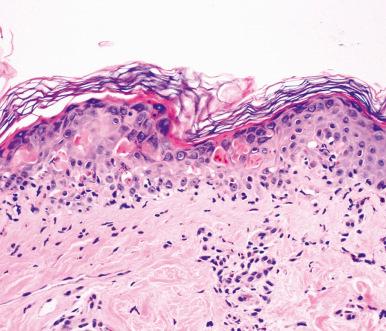
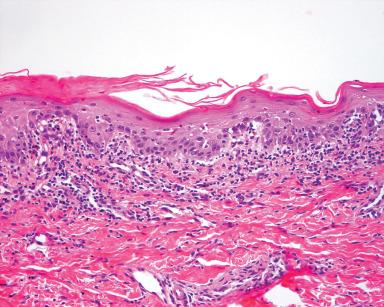
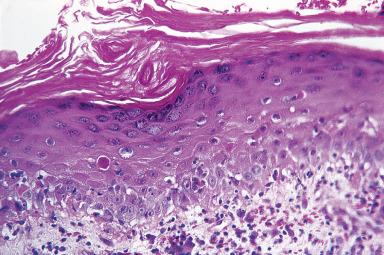
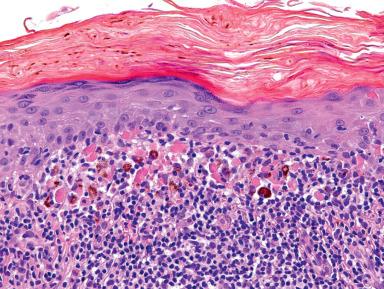
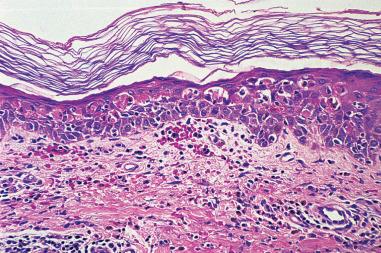
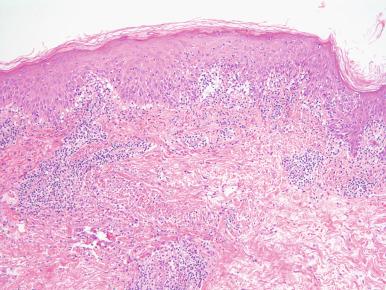
The histologic features are somewhat dependent on when the biopsy is taken during the disease process. The range of histologic features can be divided into three phases, although one should recognize that these phases exist along a continuum. In acute spongiotic dermatitis , there is accumulation of edema fluid in the epidermis, sometimes with spongiotic microvesicle formation. The stratum corneum often retains its normal basket-weave configuration or may have some focal parakeratosis. Acanthosis is absent or mild. Within the dermis there is a variable superficial perivascular infiltrate of lymphocytes often admixed with eosinophils ( Fig. 2.1 ). In the subacute form, there is associated parakeratosis, often with a diminished granular layer, acanthosis of the epidermis, variable spongiosis, and a similar superficial perivascular dermal inflammatory infiltrate ( Fig. 2.2 ). In the chronic phase, there is often compact hyperkeratosis, a thickened granular layer, acanthosis, minimal spongiosis, and mild superficial inflammatory infiltrate ( Fig. 2.3 ). The subacute and chronic phases can have significant histologic overlap with entities in the psoriasiform dermatitis category. In addition to spongiosis, there is variable parakeratosis, hyperkeratosis, and irregular acanthosis.
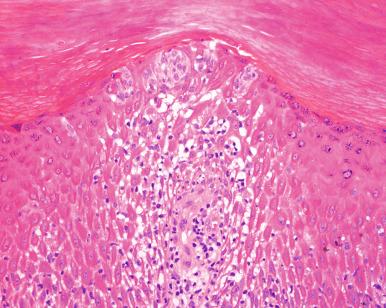
Allergic contact dermatitis is a common entity that is biopsied with some frequency. Typical examples of common allergens include detergents, nickel, and plants, such as poison ivy, but a whole host of potential allergens exist. Microscopically, it is a spongiotic dermatitis that is indistinguishable from other forms of spongiotic dermatitis. Some cases have Langerhans cell microabscesses in the epidermis ( Fig. 2.4 ). This is a clue to possible allergic contact dermatitis but is not entirely specific.
Nummular dermatitis presents as round to oval plaques, commonly on the extremities. Clinically, it may get confused with psoriasis. Microscopically, most cases show features of subacute spongiotic dermatitis. Clues that help to distinguish it from psoriasis include serum in the parakeratotic scale, epidermal spongiosis, and, when present, eosinophils in the dermal infiltrate.
This is a chronic eczematous dermatitis that runs in families and is associated with allergic rhinitis and asthma. It is infrequently biopsied and typically shows features of a subacute to chronic spongiotic dermatitis.
Also called pompholyx, this is a recurrent dermatitis that affects the hands and feet, and many are in actuality an allergic contact dermatitis. Clinically, it often has a vesicular appearance. Microscopically, it resembles a typical spongiotic dermatitis. Spongiotic microvesicles are relatively common. It is important to exclude a dermatophyte infection, especially in lesions from the feet.
A small subset of drug eruptions may be eczematous in nature. Histologically, they are not distinguishable from other forms of spongiotic dermatitis. Rather correlation with onset related to a medication is required.
As a general rule, pathologists can render only a descriptive diagnosis of spongiotic dermatitis because the histologic features themselves are not specific. That being said, it is important to exclude more specific diagnoses, such as psoriasis and dermatophyte infection, which can have overlapping features and are discussed later. If information is known about the clinical presentation, a more specific diagnosis can be suggested in a comment.
A more distinct form of dermatitis that can have either a spongiotic or psoriasiform pattern is stasis dermatitis. Stasis dermatitis occurs on the lower legs of older and/or obese patients. Often it is bilateral but sometimes presents as an isolated lesion that can mimic a neoplasm clinically. Microscopically, it is associated with variable acanthosis and spongiosis. The key feature is the presence of a lobular proliferation of relatively thick-walled blood vessels in the papillary dermis ( Fig. 2.5 ). Frequently there are extravasated erythrocytes and siderophages. In longstanding cases there may be significant dermal fibrosis with an associated fibroblastic proliferation, called acroangiodermatitis , a condition that can superficially mimic Kaposi sarcoma. It should be remembered that other forms of eczematous dermatitis, such as contact dermatitis, can be superimposed on patients with underlying stasis change.
The most common entities in this group include psoriasis and lichen simplex chronicus/prurigo nodularis. This group is characterized by prominent epidermal hyperplasia. That being said, there may be considerable overlap with subacute to chronic spongiotic dermatitis, which also is associated with epidermal hyperplasia. In that regard, placing subacute to chronic spongiotic dermatitis in the spongiotic pattern is somewhat arbitrary.
Psoriasis is one of the more common dermatoses. Estimates of its incidence vary between 0.5% and 1.5% of the population. In its most common form, psoriasis vulgaris , it is a chronic, bilaterally symmetric, nonpruritic lesion formed by erythematous plaques covered by fine silvery scales. Typically, it involves the extensor surfaces, such as the elbows, knees, back, and scalp. Generalized lesions also occur. The morphologic characteristics are those of uniform acanthosis of the epidermis with prominent parakeratosis and attenuation of the epidermis overlying the dermal papillae, a feature known as “suprapapillary thinning” ( Fig. 2.6 ). Within the parakeratosis and sometimes the epidermis, there are collections of neutrophils. Within the dermal papillae, the capillaries are dilated and tortuous. There is also a polymorphic inflammatory infiltrate composed of lymphocytes, macrophages, and neutrophils. Psoriasis may also be induced by tumor necrosis factor-α inhibitors, typically in the setting of inflammatory bowel disease. In our experience, drug-induced psoriasis in this setting often has eosinophils, in contrast to conventional psoriasis in which eosinophils are typically absent. Eosinophils are usually absent with the exception of drug-induced forms of psoriasis, usually secondary to tumor necrosis factor-α inhibitors. The hyperproliferation appears to be caused by overexpression of cytokines (e.g. tumor necrosis factor-α, interferon gamma, and various interleukins), as well as chemokines and chemokine receptors (e.g. CCL2, CCL3, CCL4, CXCL1, CXCL8), suggesting a Th1 disorder.
Other variants of psoriasis lack the prototypical uniform hyperplasia but will be discussed in this section. Pustular psoriasis is a variant in which the subcorneal abscesses are particularly prominent. In pustular psoriasis, there is less prominent epidermal hyperplasia. Guttate psoriasis is a special type of psoriasis that is characterized by a rapid onset of small papules and plaques, typically after an antecedent streptococcal pharyngitis. It lacks the epidermal hyperplasia, and the granular layer is often retained. It is characterized by discrete mounds of parakeratosis with collections of neutrophils overlying the epidermis ( Fig. 2.7 ).
The differential diagnosis of psoriasis typically centers on subacute forms of spongiotic dermatitis, usually nummular. In contrast to spongiotic dermatitis, the epidermis in psoriasis is more uniformly acanthotic and the parakeratosis is “dry,” lacking the serum present in the overlying crust scale in spongiotic dermatitis. Psoriasis also typically lacks eosinophils (with the exception noted previously), which are frequently present in spongiotic dermatitis. Dermatophyte infections can have similarity to psoriasis. Both have collections of neutrophils in the parakeratosis, but dermatophyte infections usually lack the uniform acanthosis and may have eosinophils in the infiltrate. A periodic acid–Schiff (PAS) or Gomori methenamine silver (GMS) stain can help with this differential diagnosis. Pityriasis rubra pilaris is a rare disorder that can closely resemble psoriasis with a similar pattern of acanthosis and parakeratosis. However, collections of neutrophils in the parakeratotic scale are not seen. Finally, partially treated psoriasis may lack some of the typical histologic features. The presence of dilated and tortuous papillary dermal blood vessels can be a clue in partially treated psoriasis. As in all inflammatory dermatoses, clinical correlation is essential.
Lichen simplex chronicus and prurigo nodularis , sometimes clinically referred to as neurodermatitis, are ends of a spectrum of a dermatosis that are the result of persistent excoriation rather than inflammation. They are often seen in patients with medical conditions that result in pruritus (e.g. renal failure) and in a subset of patients with psychiatric disorders. They present as plaques (lichen simplex chronicus) or nodules (prurigo nodularis). The clinical location is a clue to the diagnosis in that lesions are only seen in areas that can be readily reached. This condition is most commonly encountered on the extremities, abdomen, genitalia, and scalp, but they may present at any easily accessible location on the body. Lichen simplex chronicus involving perianal and genital skin is often biopsied with a clinical diagnosis of lichen sclerosus. These disorders can also be seen as a complication of a chronic eczematous process, such as a persistent contact dermatitis (see earlier).
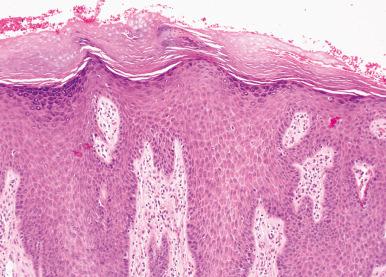
Microscopically, they demonstrate marked acanthosis of the epidermis, marked hyperkeratosis, a thickened granular layer, and vertical fibrosis of the papillary dermal collagen ( Fig. 2.8 ). Occasional cases may show pseudoepitheliomatous hyperplasia or focal parakeratosis. Typically, there is little inflammation unless it is superimposed on an underlying chronic eczematous process.
Interface dermatitis is characterized by basal vacuolization and dyskeratosis. The presence of dyskeratotic keratinocytes is important, as some cases of spongiotic dermatitis have basilar spongiosis that mimics vacuolar change. Broadly speaking, interface dermatitis can be grouped in two patterns: lichenoid and perivascular, although entities within this group may have overlapping features.
This group of disorders forms of spectrum of dermatoses that are histologically similar. Specific diagnosis requires knowledge of the clinical presentation. Erythema multiforme is a self-limiting episodic eruption that usually affects acral surfaces and oral mucosa of young adults. It is associated with herpes simplex virus and Mycoplasma infections, as well as a variety of medications.
Stevens-Johnson syndrome and toxic epidermal necrolysis involve both mucosa and epidermis. By definition, Stevens-Johnson syndrome affects ≤10% of the total body surface area and toxic epidermal necrolysis ≥30% of the body surface area, leaving an intermediate category between the two ends of the spectrum. Both Stevens-Johnson syndrome and toxic epidermal necrolysis are almost invariably triggered by adverse reactions to medications. They are considered true emergencies, and there is an associated mortality rate ranging from 10% to 40%. Recognition of Stevens-Johnson syndrome and toxic epidermal necrolysis is therefore critical because these patients may need to be managed in specialized burn units.
Microscopically, all of these entities show similar features. There is interface change characterized by basal vacuolization of the epidermis and frequent necrotic keratinocytes at all levels of the epidermis with exocytosis of lymphocytes into the overlying epidermis ( Fig. 2.9 ). In some cases there is complete necrosis of the epidermis. There is typically a relatively sparse to mild superficial perivascular lymphocytic infiltrate that may contain a few eosinophils. The infiltrate is typically disproportionately mild compared with the amount of epidermal damage. Reactive epidermal changes, such as acanthosis, parakeratosis, and hyperkeratosis, are notably absent, and this absence is a clue to differentiating this group from other dermatoses with interface change. Some cases may have a bullous appearance due to detachment of the epidermis secondary to the marked interface change.
Graft-versus-host disease is an important cause of morbidity and mortality following bone marrow transplantation. The acute form is characterized microscopically by vacuolization of the basal layer, spongiosis, and individual cell necrosis, associated with mononuclear cell infiltration of the upper dermis ( Fig. 2.10 ). Sometimes these epidermal changes occur in the absence of an inflammatory infiltrate. The amount of inflammation seems to be the most important prognostic determinator. This has been quantitated through the Lerner grading system, which has a high degree of interobserver concordance, but which is of limited use in predicting the likelihood of a skin rash progressing to a clinically more significant disease. In this system, grade 1 acute graft-versus-host disease is characterized by basal vacuolization with a superficial perivascular lymphocytic infiltrate without dyskeratotic keratinocytes. Grade 2 has the features of grade 1 graft-versus-host disease but with dyskeratotic keratinocytes and satellite cell necrosis. Grade 3 is associated with cleft formation between the epidermis and dermis, and grade 4 is characterized by complete loss of the epidermis. In general, most cases of acute graft-versus-host disease are grade 2.
The chronic form of graft-versus-host disease has been divided into a predominantly lichenoid form and sclerodermoid form. In lichenoid chronic graft-versus-host disease the epidermis shows thickening of the granular layer like lichen planus, but the inflammatory infiltrate is usually less dense. The sclerodermoid form is essentially indistinguishable from scleroderma/morphea with marked sclerosis of dermal collagen.
Cutaneous lupus erythematosus can be divided into the chronic/discoid, acute/systemic, and subacute forms. Chronic discoid lupus erythematosus is a relatively common condition with a distinct preference for women, presenting as delimited erythematous to hyperkeratotic to atrophic patches and plaques on the face, neck, scalp, and, less frequently, the arms and trunk ( Fig. 2.11 ). Systemic lupus erythematosus is an immune-mediated disease caused by antibodies to homologous and heterologous DNA. It manifests a protean symptomatology usually characterized by fatigue, fever, arthritis, various cutaneous lesions of which the erythematous bimalar “butterfly” blush is most common, signs of renal involvement, lymphadenopathy, and panserositis. Sunlight may cause exacerbations. Subacute lupus erythematosus usually presents as plaques, often annular, on sun-exposed skin of the extremities and trunk. The face is usually spared. Histologically, there is overlap between the subtypes. They all have basal vacuolization with interface change and scattered dyskeratotic cells associated with a superficial or superficial and deep perivascular lymphocytic infiltrate with increased dermal mucin. In the discoid form there is often follicular plugging, epidermal atrophy, a thickened basement membrane, and periadnexal inflammation ( Fig. 2.12 ). Eosinophils are absent, and their presence argues against the diagnosis. Tumid lupus erythematosus is a form of chronic lupus erythematosus without interface change and may represent the same process that has also been termed Jessner lymphocytic infiltration of the skin . Clusters of CD123-positive plasmacytoid dendritic cells are present in lupus erythematosus and their presence can support the diagnosis.

Direct immunofluorescence will show the presence of immunoglobulins (usually IgG and IgM) and so-called membrane attack complex (C5b, C6, C7, C8, and C9) in approximately 90% of specimens obtained from clinically involved skin of patients with either systemic or chronic discoid lupus erythematosus. The deposition consists of coalescing clumps along the dermoepidermal junction, resulting in the formation of an irregular band (so-called lupus band test ), a finding that is not entirely specific for this entity. Clinically uninvolved areas will show deposition of immunoglobulins in approximately half of the patients with systemic lupus erythematosus but no deposition of the membrane attack complex. Direct immunofluorescence may be helpful in selected cases but is generally not necessary to establish the diagnosis. Histologic examination and correlation with clinical history usually allows accurate diagnosis.
Dermatomyositis is an inflammatory disorder affecting skeletal muscle and skin, characterized clinically by proximal, symmetric muscle weakness, and cutaneous lesions. There are cutaneous forms without muscle involvement, termed dermatomyositis sine myositis. Microscopically, the skin changes may be those of a nonspecific chronic dermatitis or may acquire features very similar to those of systemic lupus erythematosus, although typically with less inflammation. By immunofluorescence, features favoring dermatomyositis over lupus erythematosus are a negative “lupus band test” and deposition of C5b–q (the membrane attack complex of complement). Biopsies of the afflicted muscles show distinct myositis with necrosis of myofibers, fragmentation, phagocytosis, and some sarcolemmal nuclear proliferation. In the later stages, fibrosis, fat infiltration, and fascicular atrophy appear.
Much has been written about the incidence or coincidence of adenocarcinoma with dermatomyositis. A review of the literature carried out by Williams many years ago found that 15% of dermatomyositis patients had neoplasms of the stomach, breast, ovary, lung, or colon. Remissions of the dermatomyositis have occurred following resection of the neoplasm. Therefore careful investigation of adults with dermatomyositis for undetected carcinoma is certainly worthwhile. However, in the majority none will be found.
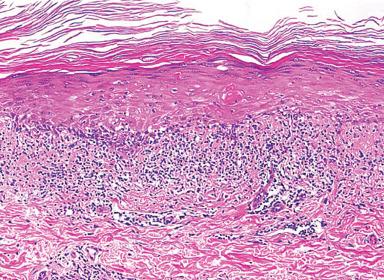
Lichen planus is a pruritic, violaceous, subacute to chronic, papulosquamous dermatitis of unknown etiology ( Fig. 2.13 ). It usually involves the flexor surfaces of the arms and the legs, but it may be found in many other sites. Lesions may be confined to the oral mucosa, or they may precede or accompany the skin changes. Histologically, the well-developed lesions are rather distinct ( Fig. 2.14 ). The epidermis is hyperkeratotic, the granular layer is prominent, and the hyperplastic epithelium forms irregular sawtooth acanthotic pegs. Within the dermis there is a dense band-like (lichenoid) lymphocytic infiltrate that may contain a few eosinophils and histiocytes. Dyskeratotic keratinocytes, also referred to as Civatte bodies , are often seen in the basal layer and sometimes also in the upper dermis and malpighian layer. On occasion, subepidermal cleavage occurs with the formation of bullae. In oral lichen planus, there is may be parakeratosis, subtle formation of keratohyaline granules. Prominent hyperkeratosis and hypergranulosis are absent in oral lichen planus . Histologically, the dyskeratotic cells and absence of atypia in oral lichen planus assists in distinguishing it from dysplasia (see Chapter 4 ). Clinicopathologic variants of lichen planus include bullous, pemphigoid, hypertrophic, atrophic, and follicular (lichen planopilaris) forms.

A morphologic pattern akin to that of lichen planus and designated as lichenoid dermatitis, lichenoid tissue reaction or interface dermatitis can be seen in a variety of conditions, including lichenoid drug eruptions (see later), lichenoid actinic keratosis, benign lichenoid keratosis, solitary lichen planus, lupus erythematosus, acute graft-versus-host reaction, and several other conditions. A lichenoid reaction is the rule in regressing melanoma (a notorious pitfall) and can also be seen in the epidermis overlying a dermatofibroma.
Lichenoid drug eruptions present as widespread papular eruptions. A variety of agents can trigger lichenoid drug eruptions, including common agents, such as thiazide diuretics. The eruption can develop soon after ingestion of the drug or weeks after.
Microscopically, lichenoid drug eruptions are very similar to lichen planus. There is a lichenoid lymphocytic infiltrate with prominent epidermal damage. The epidermis has a thickened granular layer. The presence of parakeratosis and conspicuous eosinophils help to distinguish lichenoid drug eruption from lichen planus ( Fig. 2.15 ).
Fixed drug eruption is an unusual localized type of adverse medication reaction that recurs in the same location on subsequent exposures. Microscopically, it is an interface dermatitis with a lichenoid or perivascular infiltrate and basal vacuolization with dyskeratotic keratinocytes ( Fig. 2.16 ). The overlying stratum corneum usually has a normal basket-weave configuration but may have some parakeratosis. The infiltrate contains lymphocytes, histiocytes, and eosinophils. Melanophages are frequently present.
Pityriasis lichenoides occurs in two clinical forms: pityriasis lichenoides acuta et varioliformis acuta (PLEVA; also known as Mucha-Habermann disease ) and pityriasis lichenoides chronica (PLC). The etiology is uncertain but may be related to a hypersensitivity reaction to various infectious agents or drugs. It has also been associated with autoimmune disease. PLEVA is associated with the appearance of numerous, small papules that ulcerate and heal, leaving behind smallpox-like (varioliformis) scars. The eruption is predominately on the extremities but may also involve the trunk and buttocks. In PLC the eruption is characterized by brownish-red papules that typically do not result in scarring. Some patients may have overlapping features of both PLEVA and PLC.
Histologically, pityriasis lichenoides shows overlapping features of a lichenoid interface dermatitis and a perivascular interface dermatitis. The features somewhat depend on the timing of the biopsy during the evolution of the disease. In fully developed, nonulcerated lesions of PLEVA, there is a superficial perivascular to lichenoid infiltrate with an accompanying wedge-shaped perivascular infiltrate extending into the underlying dermis. There is interface change with basal vacuolization, dyskeratosis, and papillary dermal hemorrhage ( Fig. 2.17 ). The hemorrhage is likely due to a lymphocytic vasculitis, and vasculitic changes can sometimes be seen. In addition to interface change, the epidermis is spongiotic with parakeratosis-prominent exocytosis of lymphocytes and often exocytosis of erythrocytes. Although some authors prefer to classify this as a lymphocytic vasculitis, considering it in the family of interface dermatitis is prudent given the more consistent histologic findings of interface damage. In older lesions, the epidermis may be completely ulcerated. From a pathologic standpoint, ulcerated lesions are histologically nonspecific. Early lesions may show considerably less interface and epidermal change. PLC is similar to PLEVA but with less pronounced histologic features. There is less interface damage, less inflammation, and little to no hemorrhage. Again, a given patient may have lesions that histologically span the spectrum of both PLEVA and PLC.
The differential diagnosis includes other interface dermatitides, as outlined previously. PLEVA has a distinct clinical presentation, which aids in its diagnosis. PLEVA also typically has extravasation of erythrocytes, which is not a conspicuous feature of the aforementioned entities. The presence of spongiosis helps to distinguish it from chronic interface dermatitides, such as lupus erythematosus. Lichen planus and lichenoid drug eruptions have a lichenoid pattern without a deeper perivascular extension. Graft-versus-host disease has much less inflammation. As with all inflammatory diseases, knowledge of the clinical presentation is very helpful.
However, one entity may have a very similar clinical presentation to PLEVA: lymphomatoid papulosis (LYP). LYP is actually considered an indolent T-cell lymphoma. There are multiple different histologic types, ranging from type A to E. Types A, B, and C are the classic forms. Type A can show considerable histologic overlap with PLEVA but also has numerous large, atypical CD30 + lymphocytes that are not seen in PLEVA admixed within the infiltrate. Type B LYP resembles mycosis fungoides microscopically. Type C histologically resembles cutaneous anaplastic large cell lymphoma, with sheets of large atypical, CD30 + lymphocytes. The primary way to differentiate types B and C LYP from their mimics is knowledge of the clinical history of waxing and waning papulonecrotic lesions.
This section will encompass a wide variety of entities and by necessity is somewhat superficial, mostly concentrating on more common dermatoses. The patterns discussed will include perivascular, nodular and diffuse, palisading granulomatous and sclerosing dermatoses.
This pattern is typified by an inflammatory infiltrate that is predominantly in a perivascular distribution. Some entities in this pattern will have overlapping features with the nodular and diffuse pattern. This further highlights how inflammatory diseases and their patterns are on a biologic continuum that we by necessity categorize as discrete entities.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here