Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acknowledgment: The author would like to acknowledge Brian W. O’Doherty, coordinator of visual media services. His photographic and video excellence was necessary for completion of this chapter.
Thumb hypoplasia is considered part of radial deficiency even with normal forearm architecture. Hence, associated anomalies need to be considered during the initial evaluation. The workup must include entities such as VACTERL association, thrombocytopenia–absent radius syndrome, Holt-Oram syndrome, CHARGE ( c oloboma of the eye, h eart defects, a tresia of the choanae, r etardation of growth and/or development, g enital and/or urinary abnormalities, and e ar abnormalities and deafness) syndrome, and Fanconi anemia ( Table 37.1 and Fig. 37.1 ). An evaluation of all possibly affected organ systems can be lifesaving. The workup should include renal ultrasound, echocardiography, spine radiographs, a complete blood count, and a chromosomal challenge test.
| Syndrome or Association | Characteristics |
|---|---|
| Holt-Oram syndrome | Heart defects, most commonly cardiac septal defects |
| Thrombocytopenia–absent radius syndrome | Thrombocytopenia present at birth (may require transfusions) but improves over time |
| VACTERL association | Vertebral abnormalities, anal atresia, cardiac abnormalities, tracheoesophageal fistula, esophageal atresia, renal defects, radial dysplasia, lower limb abnormalities |
| Fanconi anemia | Aplastic anemia not present at birth; develops at about 6 years of age |
| CHARGE syndrome | Coloboma of the eye, heart defects, atresia of the nasal choanae, retardation of growth and/or development, genital and/or urinary abnormalities, and ear abnormalities and deafness |

Failure to ascertain the diagnosis of an associated syndrome will have lifelong ramifications for the child, family, and physician. This consequence is particularly evident in children with Fanconi anemia that can be diagnosed early with a chromosomal challenge test before the onset of bone marrow failure. Timely diagnosis allows for years of searching for an appropriate bone marrow match that may prevent the child from dying from aplastic anemia. Patients with thumb hypoplasia and other physical findings, specifically café-au-lait spots and short stature, have an increased risk of having Fanconi anemia. Innovative techniques, such as preimplantation genetic determination (PGD), allow the parents to have another child with matching blood characteristics and without Fanconi anemia. At birth, the cord blood can be harvested and used as donor blood for the affected Fanconi anemia child. Numerous hand surgeons and pediatricians fail to consider the diagnosis of Fanconi anemia in children with thumb hypoplasia, leaving the child and the family to suffer the consequences of a painful terminal illness that could otherwise have been treated.
The diagnosis of thumb hypoplasia is dependent on the degree of deficiency and the presence or absence of any associated anomalies. The combination of thumb hypoplasia and profound radial deficiency is typically diagnosed shortly after birth because the infant’s forearm is foreshortened and the hand deviated in a radial direction. Substantial thumb hypoplasia is also recognized early in infancy because there is marked asymmetry between the thumbs. In contrast, mild thumb hypoplasia may go unidentified for years, and the patient may not present to the physician until adolescence. This late presentation is often perplexing to the patient and disconcerting to the parents. The parents cannot understand how they failed to recognize the child’s hypoplasia before adolescence. They often relate the thumb hypoplasia to some recent trauma and question the diagnosis. Our explanation is quite simple: “As one gets older, the activities of daily of life become more complicated, and therefore subtle differences are not recognizable until the child is older.” For example, buttoning, keyboarding, and tying shoes are tasks performed as the child becomes older and are not performed during infancy and early childhood. This explanation removes any guilty feelings and allows the family to focus on the treatment to correct the problem.
The diagnosis is based on the physical examination findings and corresponding x-rays. The determination of length, girth, motion, and stability are important parts of the examination. If there is unilateral involvement, the length and girth are usually compared with the thumb on the contralateral side. A thumb of normal length reaches the point just proximal to the proximal interphalangeal (PIP) joint of the adjacent index finger. On x-ray, a normal thumb is approximately 70% as long as the proximal phalanx of the adjacent index finger. The thumb girth and nail width are approximately 133% and 105%, respectively, of the index finger girth and nail width. The overall thumb motion is assessed along with specific movement at the carpometacarpal (CMC), metacarpophalangeal (MCP), and interphalangeal (IP) joints. Similarly, the stability of each of these joints is assessed by clinical examination and stress testing. Instability of the MCP and/or CMC joints is commonly associated with thumb hypoplasia and directly influences the surgical treatment algorithm. An assessment of present and absent intrinsic and extrinsic muscles is necessary in order to formulate a surgical plan.
The Blauth classification of thumb hypoplasia (circa 1967) modified by Manske (circa 1995) truly guides management ( Table 37.2 ). , , Type I hypoplasia is minor generalized hypoplasia usually affecting the thenar muscles. As stated beforehand, this slight degree of hypoplasia may present later in life as hand function becomes more intricate and demanding. Type I thumb hypoplasia may or may not warrant treatment, depending on the functional impact. If the lack of opposition is causing functional difficulties, a tendon transfer is recommended.
| Type | Findings | Treatment |
|---|---|---|
| I | Minor generalized hypoplasia | No treatment |
| II | Absence of intrinsic thenar muscles First web space narrowing Ulnar collateral ligament (UCL) insufficiency |
Opponensplasty First web release UCL reconstruction |
| III | Similar findings as type II plus: Extrinsic muscle and tendon abnormalities Skeletal deficiency A: Stable carpometacarpal joint B: Unstable carpometacarpal joint |
A: Reconstruction B: Pollicization |
| IV | Pouce flottant or floating thumb | Pollicization |
| V | Absence | Pollicization |
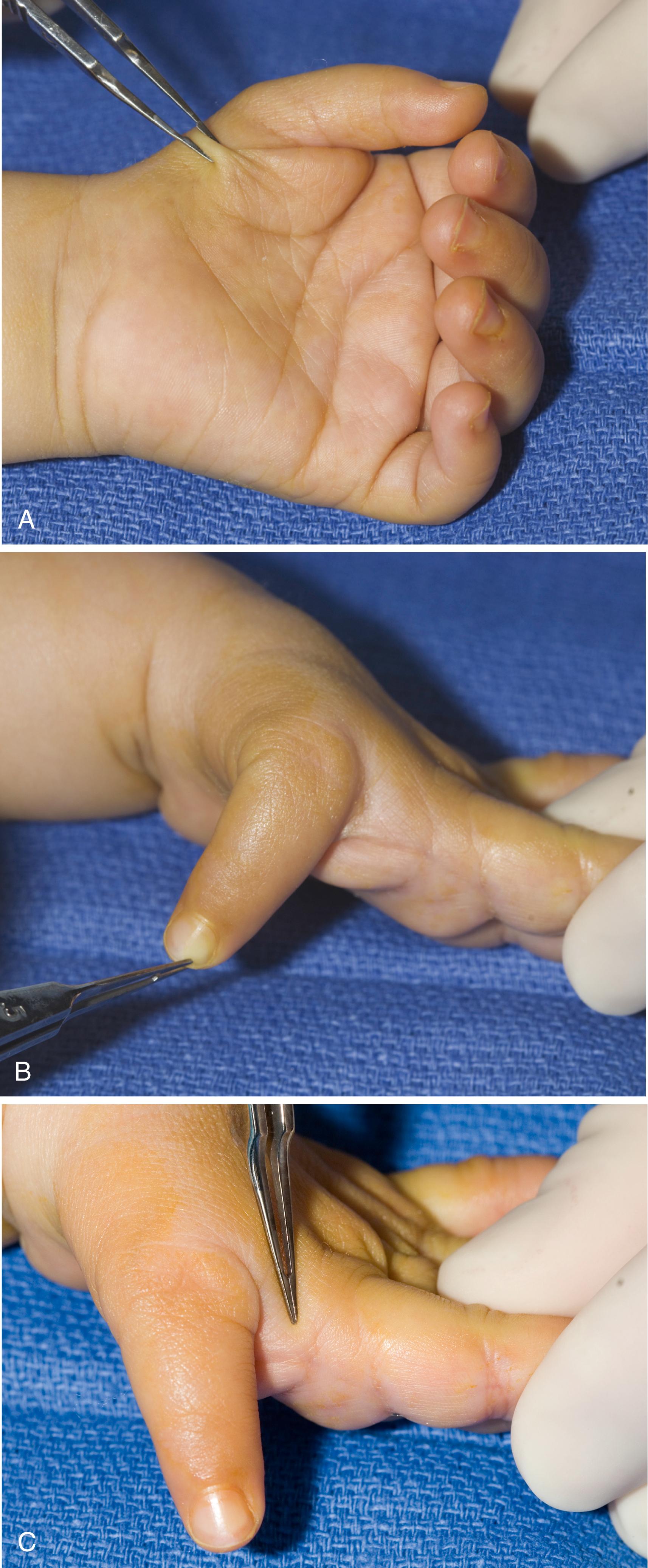
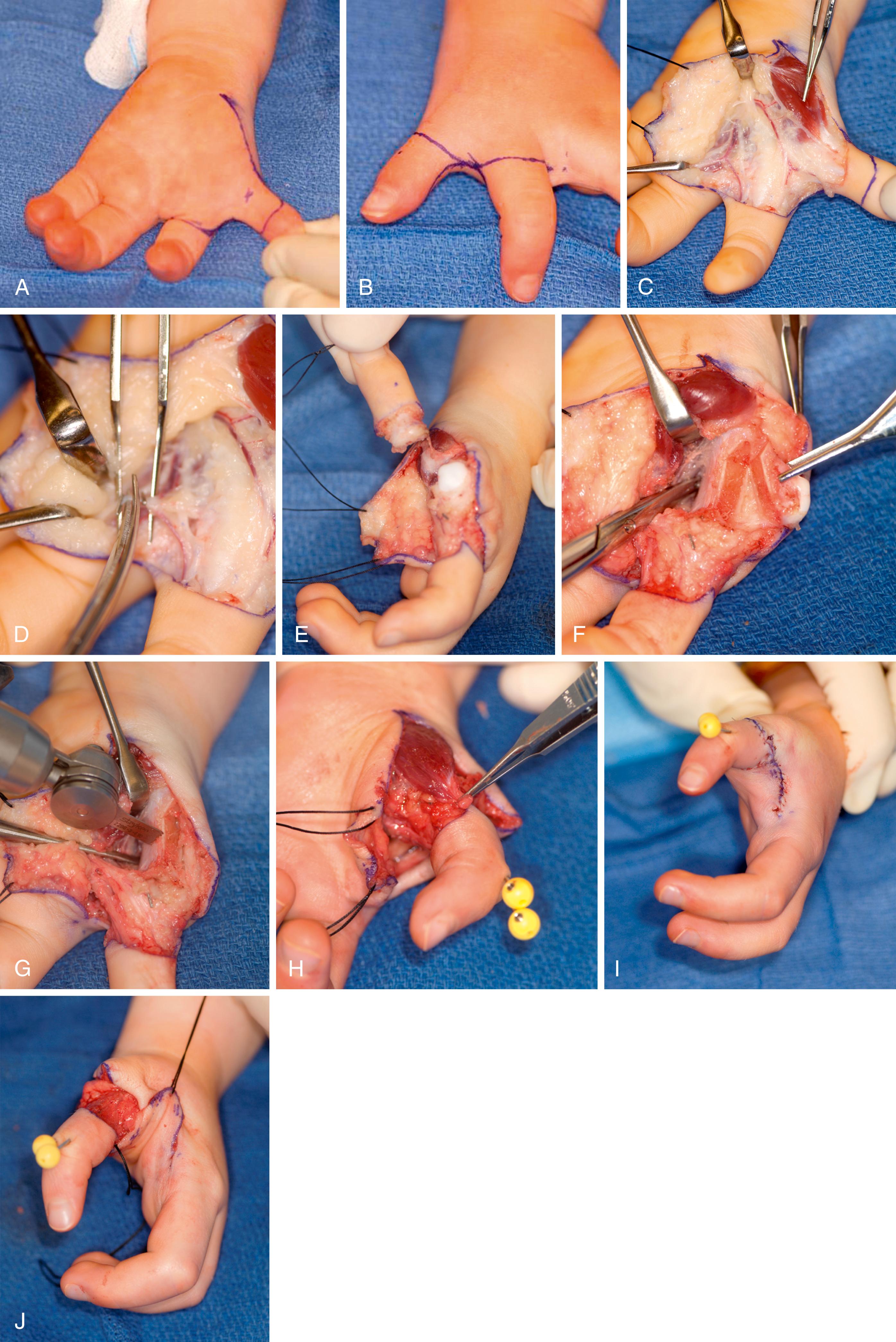
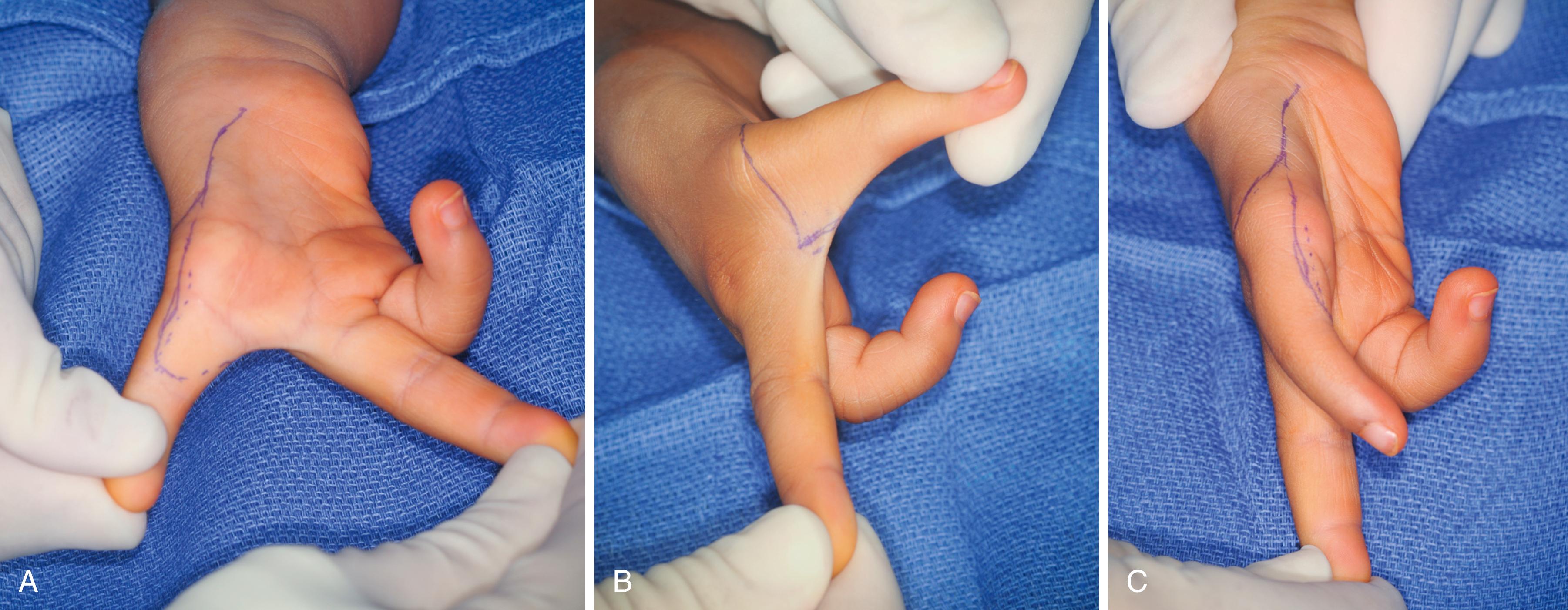
Type II hypoplasia has distinct findings that guide treatment ( Fig. 37.2 and Case Study 37.1 ). There is absence of the thenar muscles innervated by the recurrent branch of the median nerve (the abductor pollicis brevis, opponens pollicis, and superficial head of the flexor pollicis brevis) (see Fig. 37.2A ). The deep head of the flexor pollicis brevis, innervated by the ulnar nerve, is usually present, and it provides MCP joint flexion. The MCP is usually unstable, with laxity or incompetency of the ulnar collateral ligament (UCL) (see Fig. 37.2B ). The MCP joint can also be globally unstable, with incompetency of both the ulnar and radial collateral ligaments. The thumb/index finger or first web space is narrowed and the intervening skin is taut (see Fig. 37.2C ). The web space can appear to be less narrow because the unstable MCP joint drifts into valgus, masking the narrow web space. However, careful examination and imaging typically reveal an adducted metacarpal.
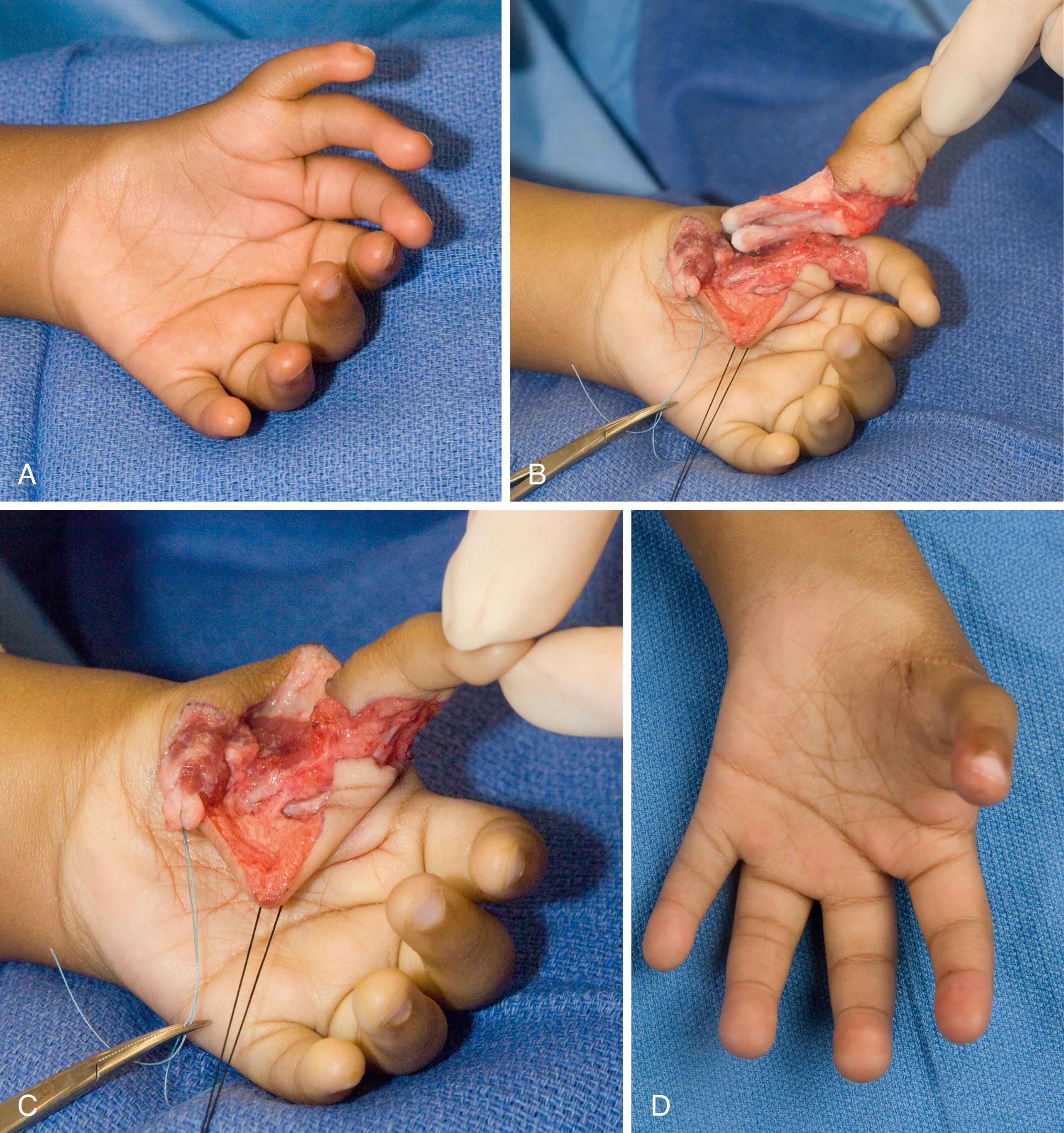
Andres was a 9-year-old with type II thumb hypoplasia ( eFig. 37.1 ). Thumb reconstruction was planned using the present CMC and thumb of adequate girth.
The surgical technique is displayed in eFig. 37.2 and ![]() . The long-term outcome is shown in eFig. 37.3 and
. The long-term outcome is shown in eFig. 37.3 and ![]() , .
, .
Type III hypoplasia has the same characteristics as type II hypoplasia with the addition of extrinsic muscle and tendon deficiencies. Absence or hypoplasia of the extrinsic extensors (extensor pollicis longus and extensor pollicis brevis) or flexors (flexor pollicis longus) requires an observant examination of the active movement at the MCP and IP joints. Type III hypoplasia is subdivided into types IIIA and IIIB, which is a crucial differentiation in the treatment paradigm. A type IIIA thumb has a stable CMC joint that is worthy of reconstruction and can provide a worthwhile prehensile thumb. A type IIIB thumb has an unstable CMC joint that is better served by ablation and index pollicization. The unstable CMC joint precludes successful reconstruction because the surgery cannot overcome the basal joint instability. A simple explanation to parents is that this effort would be similar to “trying to build a house without a stable foundation.” Multiple valiant surgical attempts including free vascularized second metatarsophalangeal transfer to reconstruct the CMC joint have yielded inferior results (outcome and function) compared with a successful index finger pollicization. A complicating factor is cultural philosophies that require and even sometimes demand five digits. In these circumstances, we prefer to treat the child nonoperatively, keeping the unstable thumb for cultural reasons. Valiant attempts using nonvascularized or vascularized basal joint reconstruction jeopardizes any future pollicization. Our practice has always remained that “function trumps form,” avoiding societal pressures to reconstruct an unusable thumb.
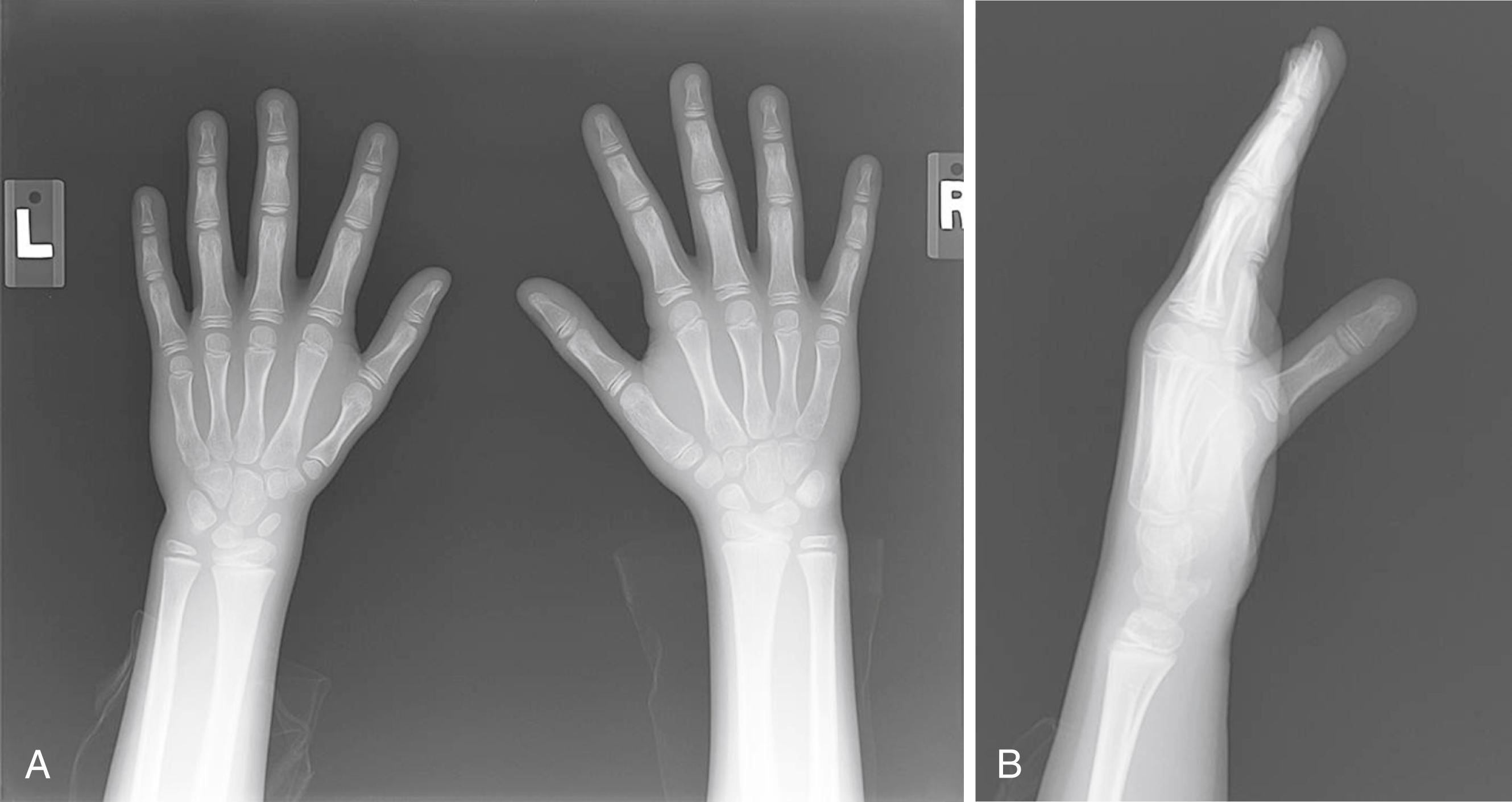
Differentiating between a type IIIA (stable) and a type IIIB (unstable) thumb can be difficult in some cases, but it is fundamental to formulation of a treatment plan. The first metacarpal base and the trapezium do not ossify until about 6 years of age. Therefore plain radiographs are often unreliable for evaluation of the CMC joint architecture. In a grossly hypoplastic CMC joint, the metacarpal base tapers to a point and the proximal metacarpal is absent ( Fig. 37.3 ). However, this plain x-ray finding is not present in milder type III hypoplasia. Advanced imaging studies, such as ultrasound or magnetic resonance imaging (MRI), can be helpful to visualize and evaluate the integrity of the cartilaginous metacarpal base and the trapezium. Repeat examinations, however, are equally as reliable to detect a thumb unworthy of reconstruction. A child with an unstable CMC joint usually completely ignores the thumb and uses the index finger and long finger for scissor pinch. In addition, the index finger pronates and the long finger/index finger web space widens. In these circumstances, thumb reconstruction is contraindicated and index pollicization is preferred.

Type IV hypoplasia represents a profound deficiency known as a pouce flottant, or floating thumb ( Fig. 37.4 ). The thumb remnant is attached to the hand solely by a narrow bridge of skin containing a single neurovascular element. The thumb is floppy and is entirely ignored during prehension.

Type V hypoplasia is complete absence of the thumb. On occasion, there will be a small skin nubbin present ( Fig. 37.5 ).

Thumb hypoplasia can also be found in children with ulnar deficiency ( Fig. 37.6 ). The treatment for thumb hypoplasia in ulnar deficiency and radial deficiency is the same. Pollicization is indicated and is the preferred procedure for marked thumb hypoplasia. The surgical technique for pollicization is similar, with minor modifications, such as skin design.

The standard indications for pollicization can be expanded to include a thumb that is just too small to make a useful thumb despite having a stable CMC joint. This decision to ablate the small thumb and pollicize the robust index finger requires a prolonged conversation with the parents about the rationale for this recommendation. Parents generally come to understand that “function trumps form” and that thumb ablation and index finger pollicization will result in a thumb which is more functional than the small, scrawny thumb even after reconstruction. When in doubt, parents are given a list of other parents who have made a similar difficult decision regarding thumb ablation. This parent-to-parent communication is invaluable.
An experienced hand therapist is invaluable in the evaluation of the child with a hypoplastic thumb. Although there is little need for nonoperative management, the hand therapist’s input is essential and can provide support for the family and facilitate the decision-making process. Following surgery, the therapist becomes a primary care provider who directly affects the success of the procedure.
The classification schema guides treatment. Type I hypoplasia usually does not warrant surgical intervention because the functional impairment is negligible. Type II or IIIA hypoplasia diminishes function and often requires surgery to provide stability, improve motion, and enhance function. Type IV or V hypoplasia requires index finger pollicization if the index finger is “suitable” for becoming a thumb. A stiff index finger will be a stiff thumb and may not enhance hand function. Therefore determining the risk-benefit ratio of pollicization requires ample thought and consideration. The operation should follow the Peter Carter 2-4 rule: For some children, surgery can indeed be done “to” them, but it may not necessarily be “for” them. We have slightly modified the Carter 2-4 rule to state that the operation should be done “to” the patient and “for” the patient.
Thumb reconstruction for type II and IIA hypoplasia requires addressing all the deficient elements. The narrowed thumb/index finger web space, MCP instability, and thenar muscle absence all require treatment. Thumb/index finger web space narrowing is treated with skin rearrangement and soft tissue release. A four-flap Z-plasty lengthens the tight skin and provides a rounded contour to the web space. The theoretical increase in length is 150%. The deeper soft tissue release includes the investing fascia around the adductor pollicis. The princeps pollicis artery and its branches must be identified and protected before division of the fascia. An extremely tight web space may also require partial release of the adductor muscle and/or first dorsal interosseous muscle to obtain adequate breadth. An extremely tight web space may require more extensive skin rearrangement, such as a dorsal rotation flap or Ghani flap.
MCP instability necessitates stabilization. Unidirectional instability with an incompetent UCL is the most common finding. Ligament reconstruction can be performed with local tissue or preferably the residual length of donor tendon from the opposition transfer. Bidirectional or global instability is more challenging to manage. Reconstruction of both the radial and UCLs with a tendon graft is an option. MCP joint chondrodesis is preferred, however, to achieve firm stability and provide a stable platform for the opposition transfer to function. The details of MCP joint chondrodesis are discussed in Chapter 39 (Arthrogryposis). UCL insufficiency can be secondary to an anomalous connection between the flexor pollicis longus and extensor pollicis longus muscles (i.e., pollex abductus ). The pollex abductus attenuates the UCL over time and prevents active thumb IP joint motion. The key to determining its presence is the physical examination prior to surgery. During attempted thumb IP flexion, the MCP joint deviates into valgus rather than bending the IP joint. Surgery must release the pollex abductus during the surgery to reconstruct the UCL.
Thenar absence requires a tendon transfer to provide thumb opposition. There are a variety of donor muscle-tendon units to choose from, including the flexor digitorum superficialis (FDS) (long or ring finger), abductor digiti minimi, extensor carpi ulnaris, and extensor indicis proprius. Each donor muscle-tendon unit has its advocates and its advantages and disadvantages. The long or ring finger FDS is preferred because of its length, power, expendability, and synergism and the technical ease with which it can be used. If the FDS is unavailable, the other donor options are considered.
The patient is placed supine on the operating room table ( Box 37.1 and see ![]() , ). The procedure is performed under general anesthesia. A single dose of intravenous preoperative antibiotics is administered. The limb is prepped and draped in sterile fashion. Chlorhexidine gluconate and alcohol prep (ChloraPrep, CareFusion, Leawood, KS) is preferred and may be more effective than Betadine prep in eliminating bacteria. Chlorhexidine avoids the use of iodine, which can migrate beneath the tourniquet and cause skin burns.
, ). The procedure is performed under general anesthesia. A single dose of intravenous preoperative antibiotics is administered. The limb is prepped and draped in sterile fashion. Chlorhexidine gluconate and alcohol prep (ChloraPrep, CareFusion, Leawood, KS) is preferred and may be more effective than Betadine prep in eliminating bacteria. Chlorhexidine avoids the use of iodine, which can migrate beneath the tourniquet and cause skin burns.
Limb is exsanguinated and the tourniquet is inflated
Four-flap Z-plasty of thumb index web space with release of tight fascia while protecting the princeps pollicis artery
Ringer FDS tendon is isolated at the base of finger and in the distal forearm
Ring FDS tendon pulled through the carpal tunnel and into the forearm
Radial one-half of the distal 2 to 3 cm FCU tendon made into a loop for the FDS tendon
Ring finger FDS tendon passed through the through FCU loop
Skin incision along the radial side of thumb MCP joint
Subcutaneous tunnel is made between the radial side of thumb and the volar forearm FCU loop
FDS tendon is passed under the skin to the radial side of the thumb
Metacarpal head is isolated and a 0.045″ Kirschner wire drilled across the metacarpal head parallel to the joint surface
Hole is enlarged with a drill bit to allow passage of the FDS tendon
MCP joint is reduced and stabilized with a longitudinal 0.045″ Kirschner wire drilled antegrade from the tip of the thumb across the MCP joint
FDS tendon is passed through the drill hole to ulnar side of thumb for ligament reconstruction
FDS tendon is sutured to the surrounding bone and periosteum along the radial side of the thumb while setting the appropriate tension in the tendon transfer
Remaining FDS tendon is directed to the base of the proximal phalanx and sutured directly into the bone to reconstruct the UCL
Skin is closed with absorbable suture and the limb is immobilized in a long-arm thumb spica cast for 3 weeks
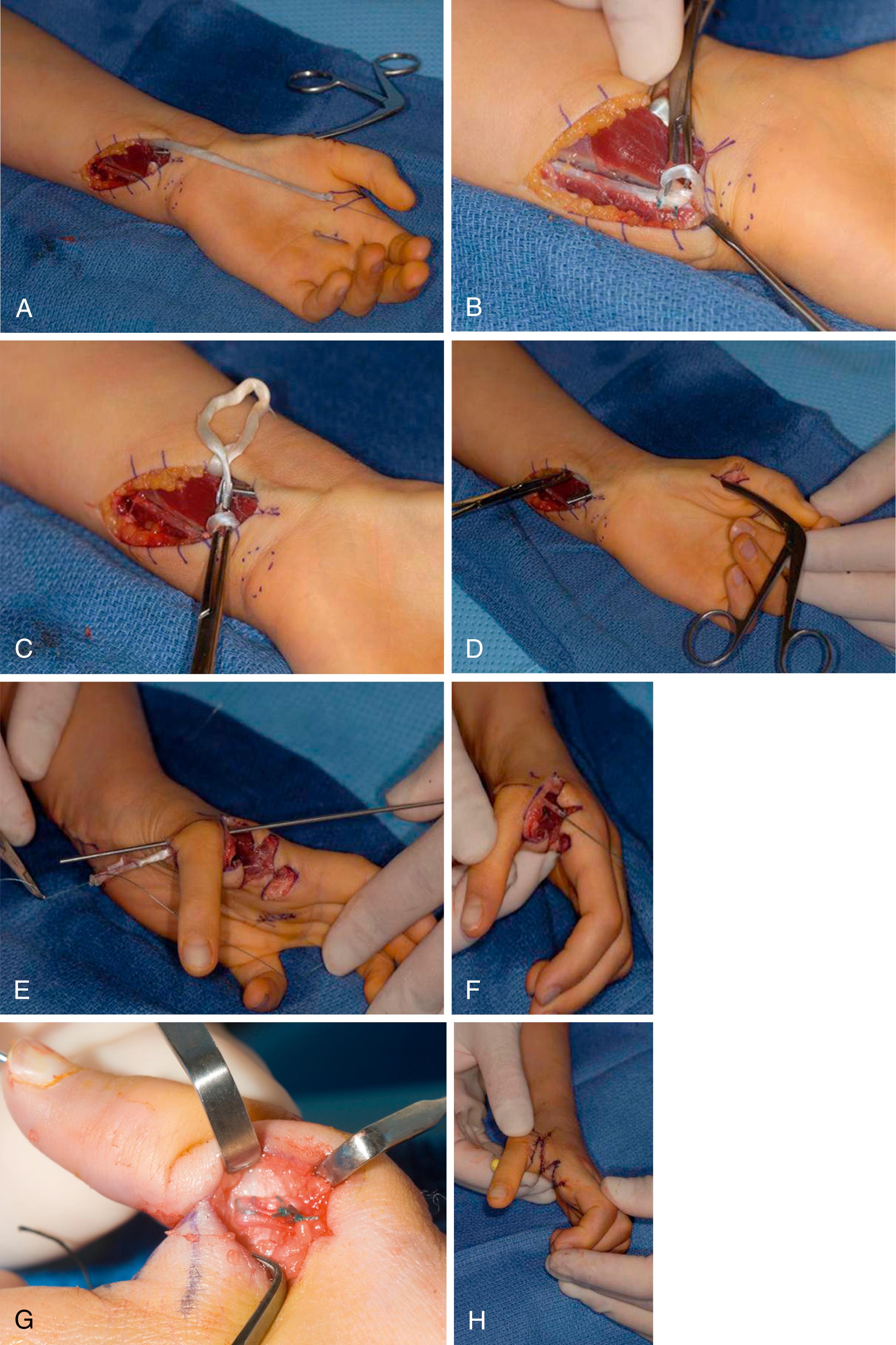
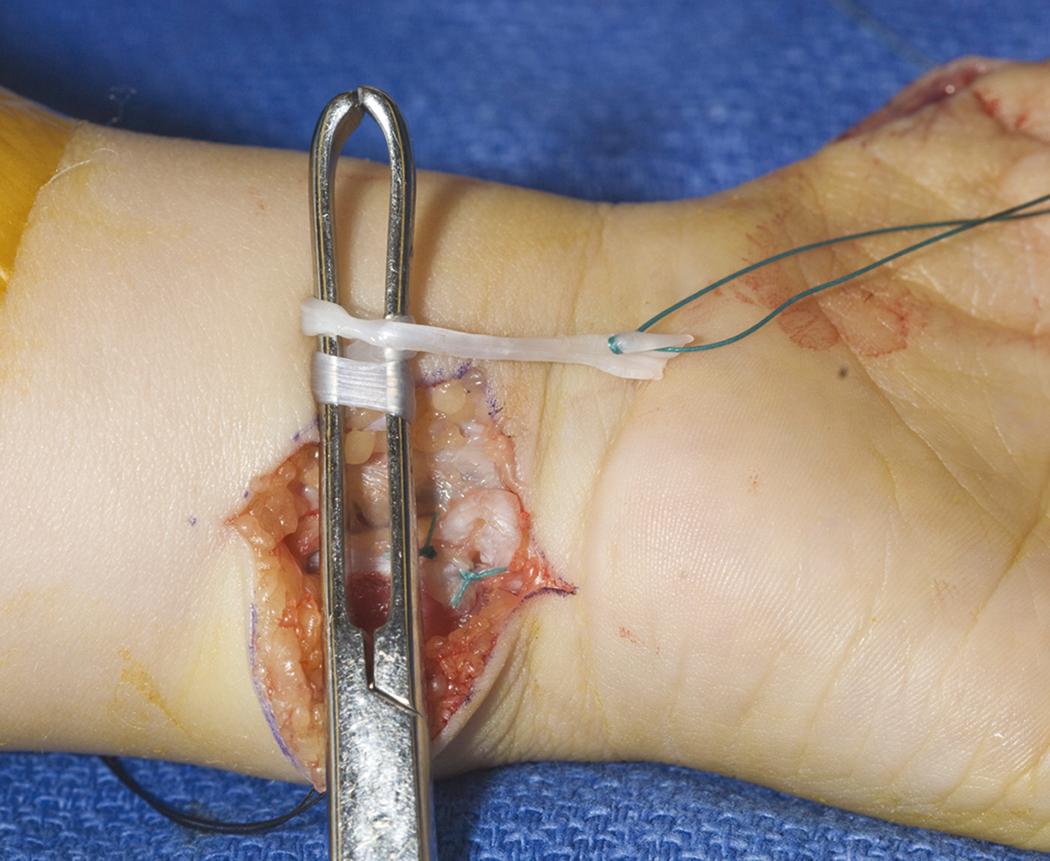
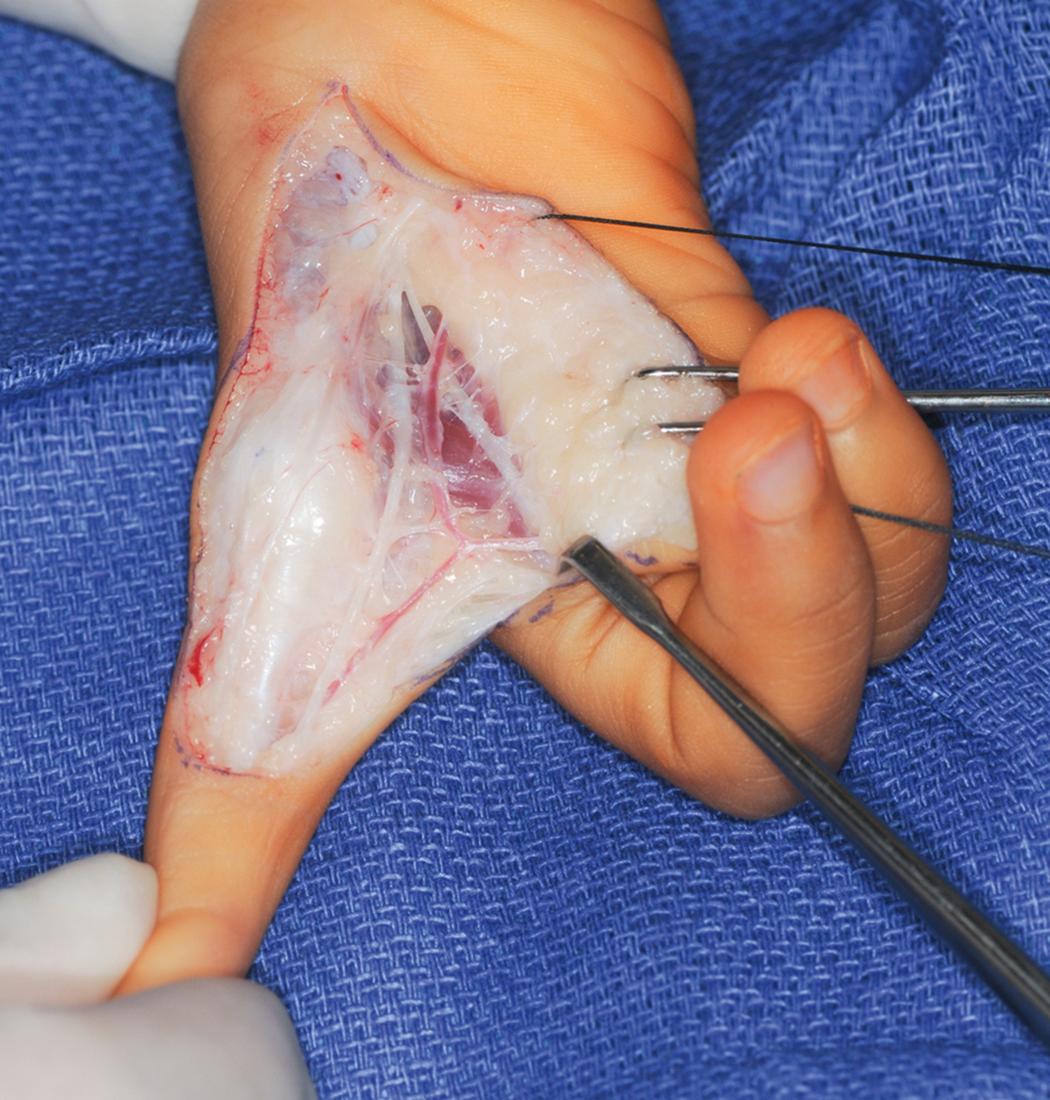
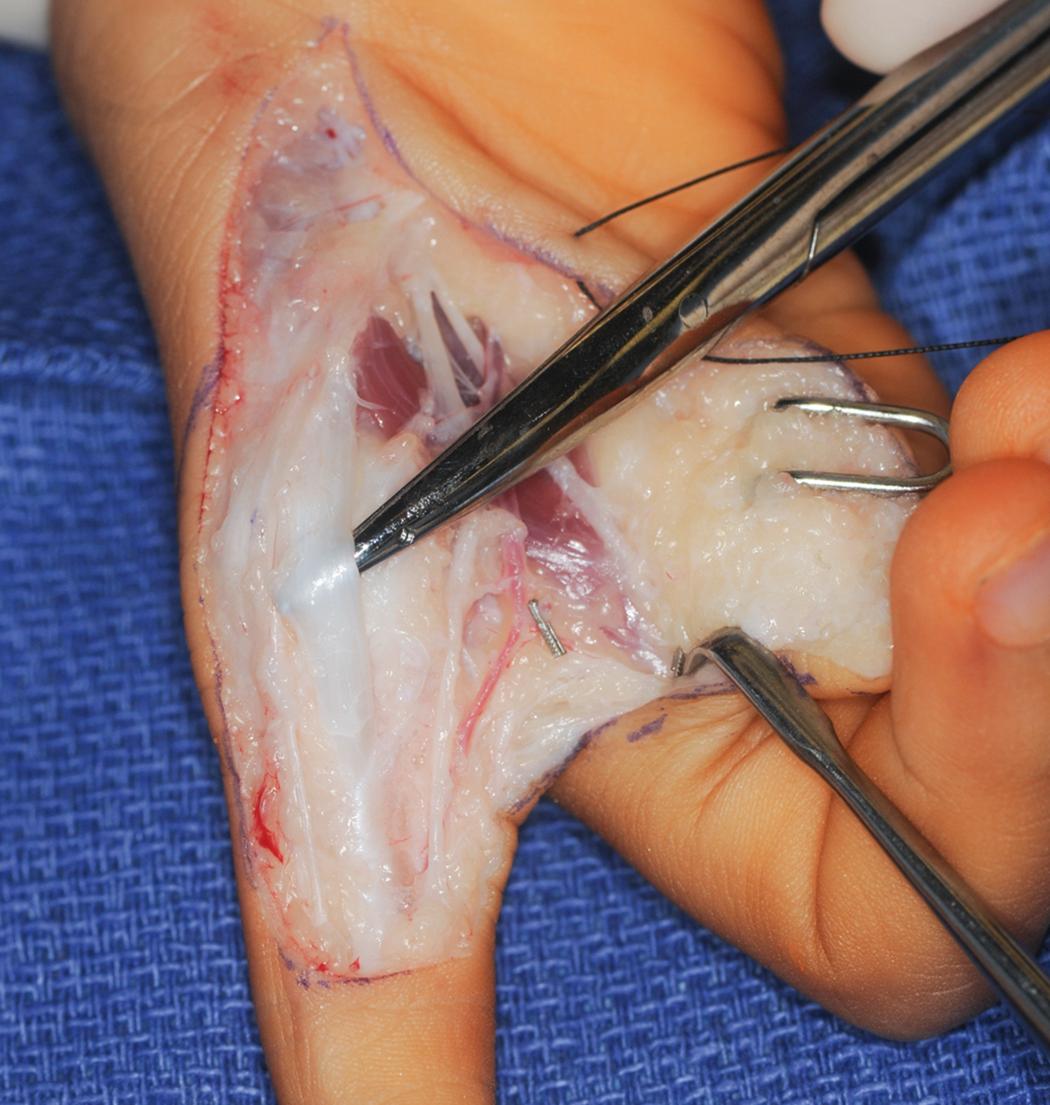
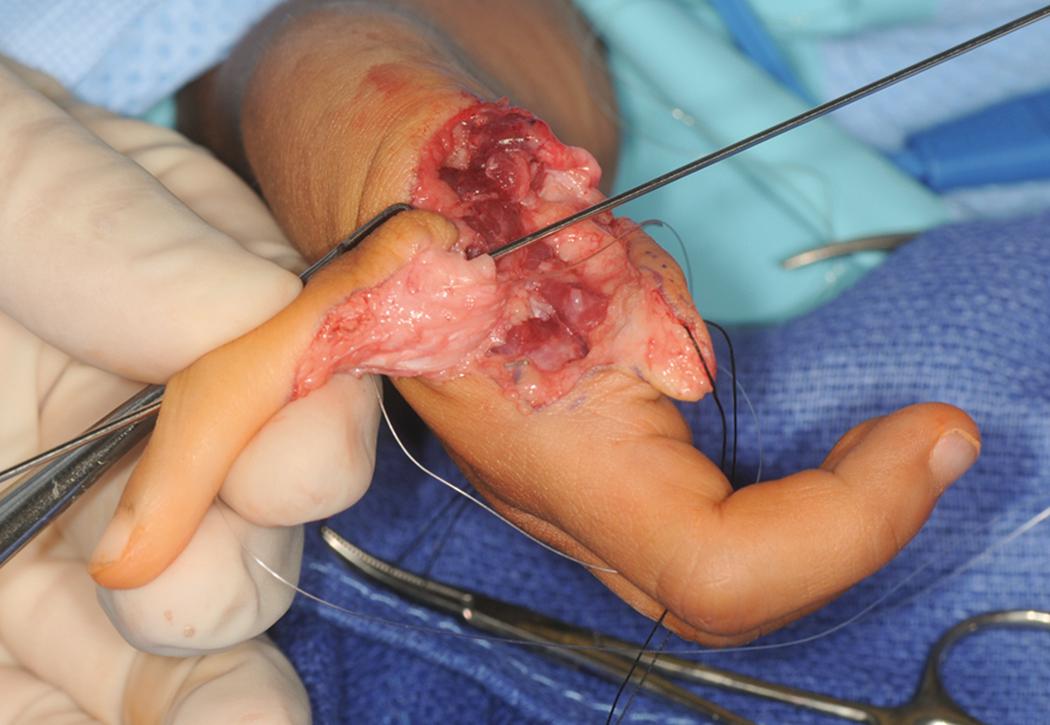
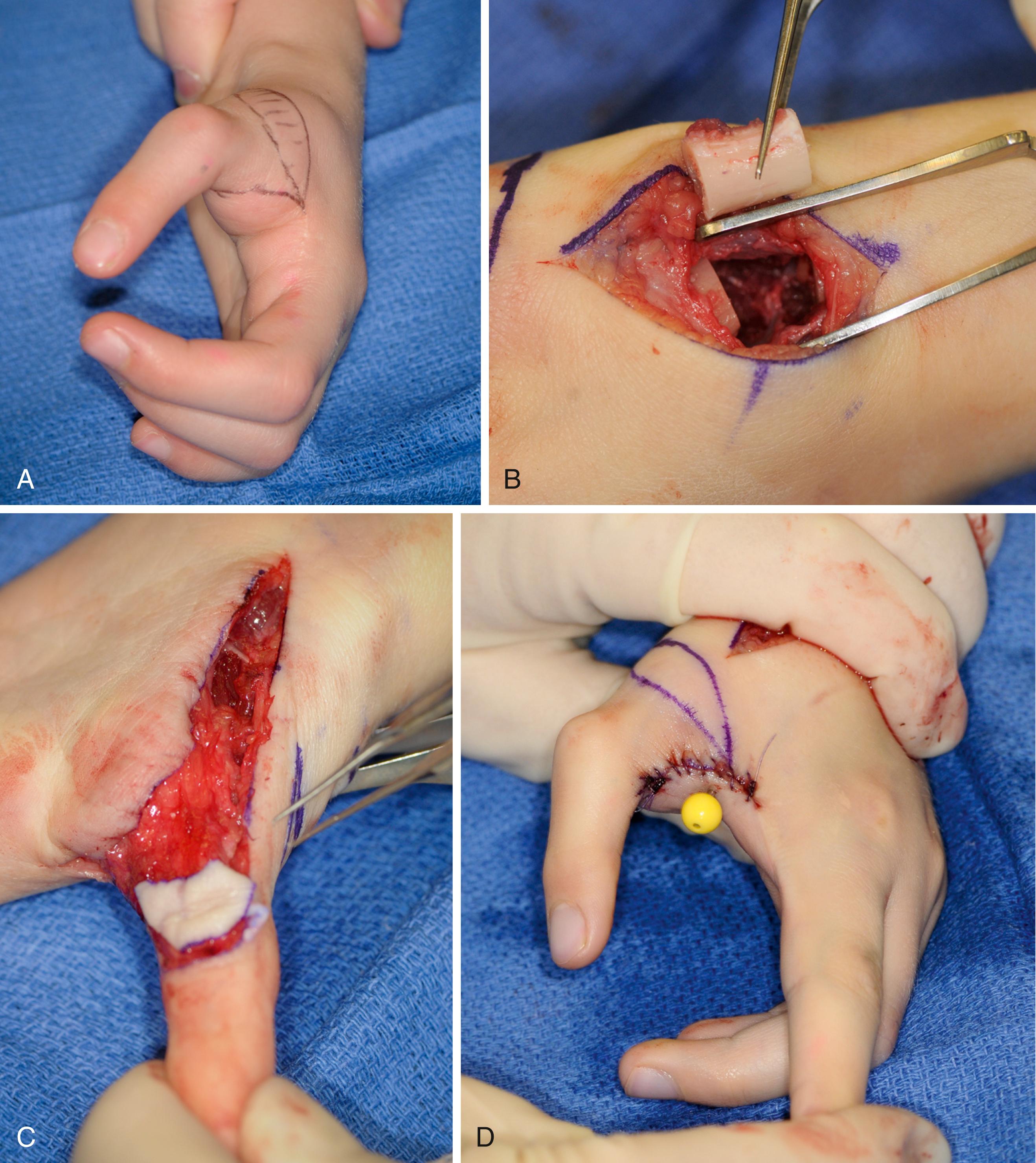
The limb is exsanguinated and the tourniquet is inflated. The incisions are carefully drawn ( Fig. 37.7 ). The narrowed thumb/index finger web space is widened via a four-flap Z-plasty. Each limb of the Z-plasty should be equal in length. The radial limb can be extended in a proximal direction to expose the UCL and the MCP joint. The ring finger FDS tendon is isolated at the base of the finger and in the distal forearm. A short oblique incision is made at the base of the ring finger along a skin crease, and a zigzag or oblique incision is made along the volar ulnar distal forearm. The flexor carpi ulnaris (FCU) tendon is also isolated. An additional skin incision is made along the radial side of the thumb MCP joint to expose the ultimate site for FDS tendon attachment. The FDS tendon is identified at the base of the ring finger and separated from the flexor digitorum profundus (FDP) tendon. The FDS tendon is also isolated in the forearm ( Fig. 37.8 ). The FDS tendon is tagged with a suture and cut at the base of the ring finger while the underlying FDP tendon is protected. An Allis tissue forceps (Jarit, Hawthorne, NY) is placed around the ring finger FDS tendon in the forearm and used to roll the tendon through the carpal tunnel ( Fig. 37.9 ). If the FDS tendon fails to roll into the forearm, it must be retrieved into the hand using the tagged suture. An additional release of FDP and FDS attachments and freeing any entrapment within the Camper chiasm is performed.


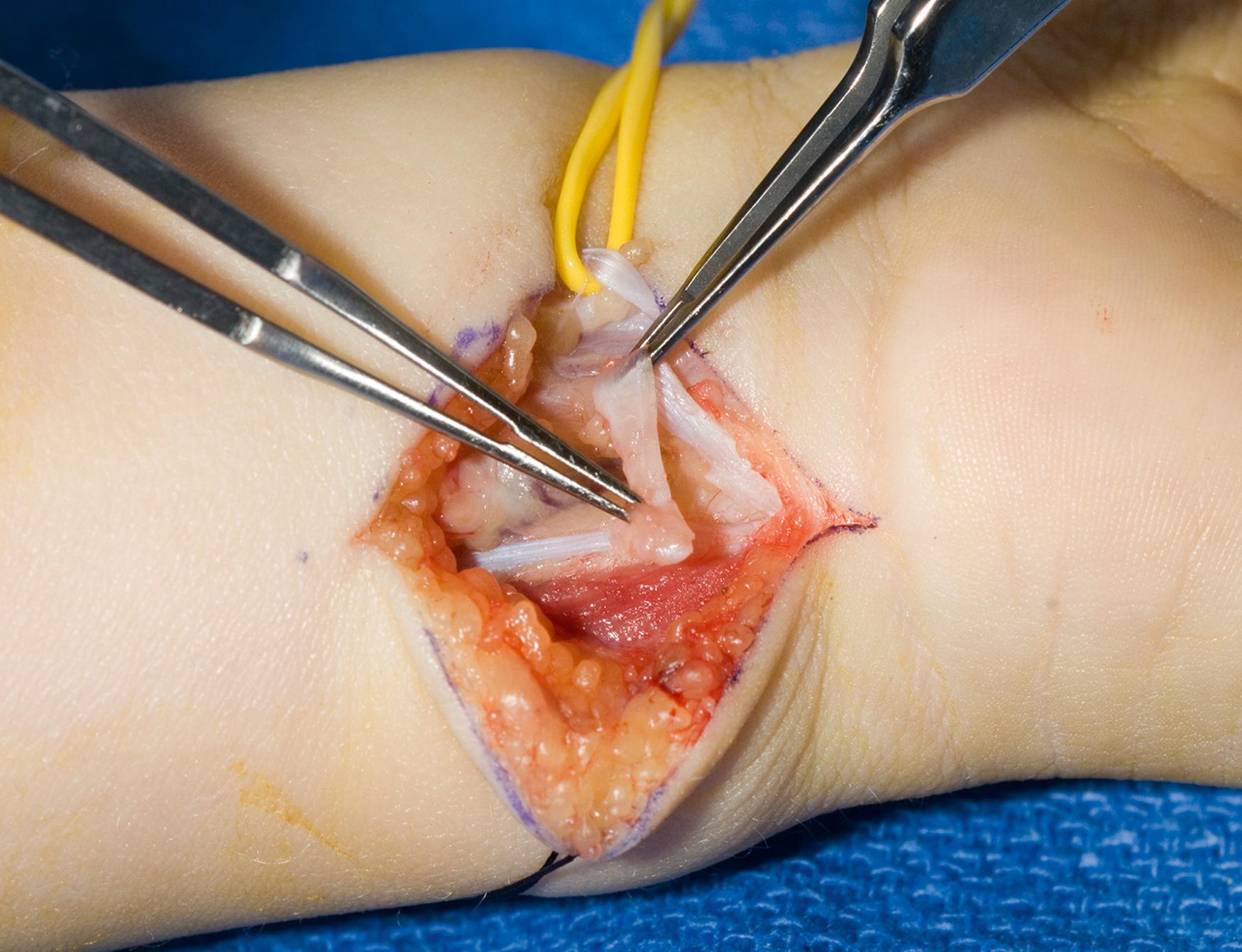
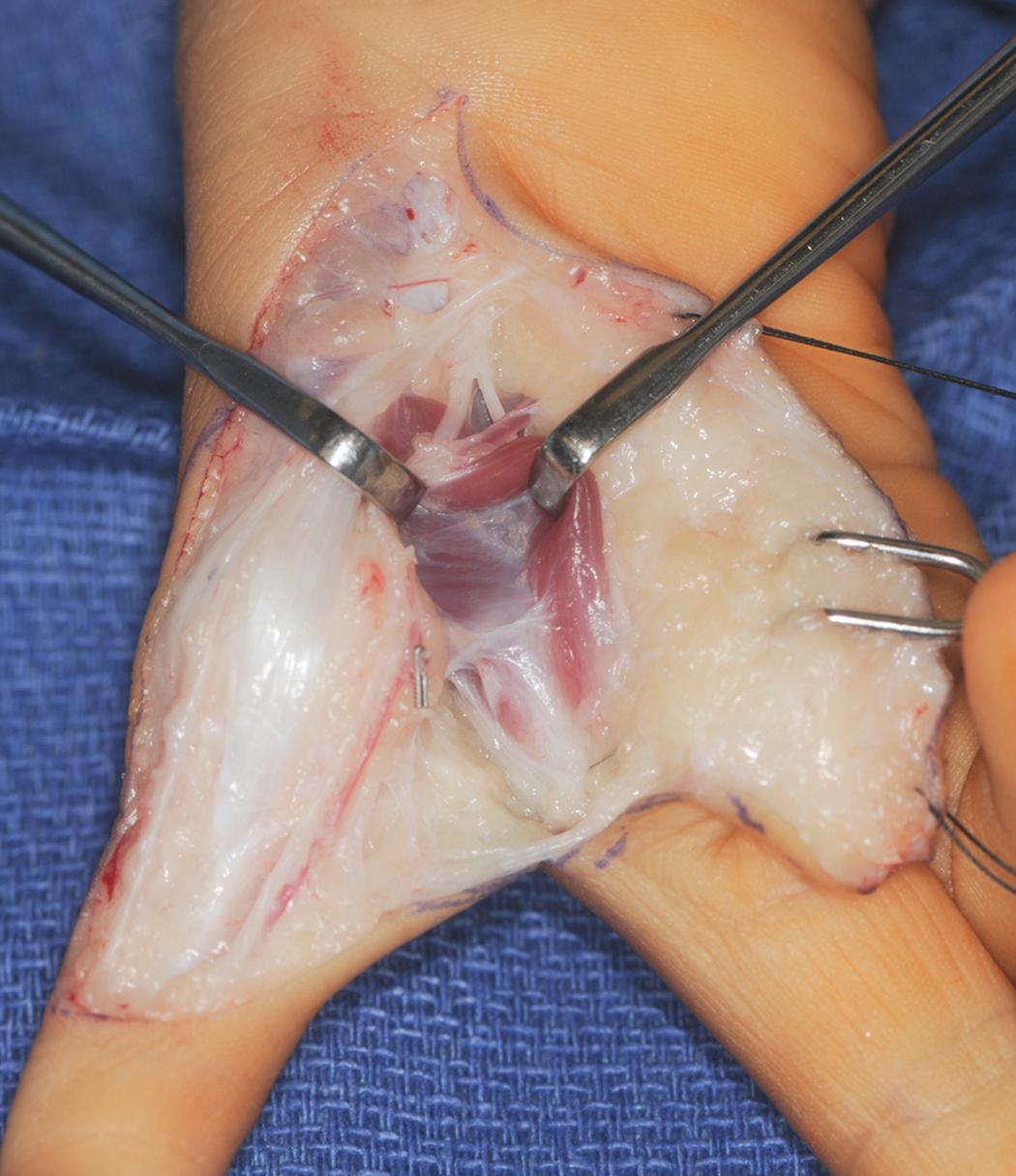
An FCU tendon loop is constructed as a pulley for the FDS tendon. The distal 2 to 3 cm of FCU tendon is isolated. The radial half of the FCU tendon is harvested, preserving its distal attachment into the pisiform ( Fig. 37.10 ). The radial half of the tendon is passed through the retained FCU at the pisiform and sutured to form a loop. The ring finger FDS tendon is passed through the FCU loop prior to transfer across the palm ( Fig. 37.11 ).
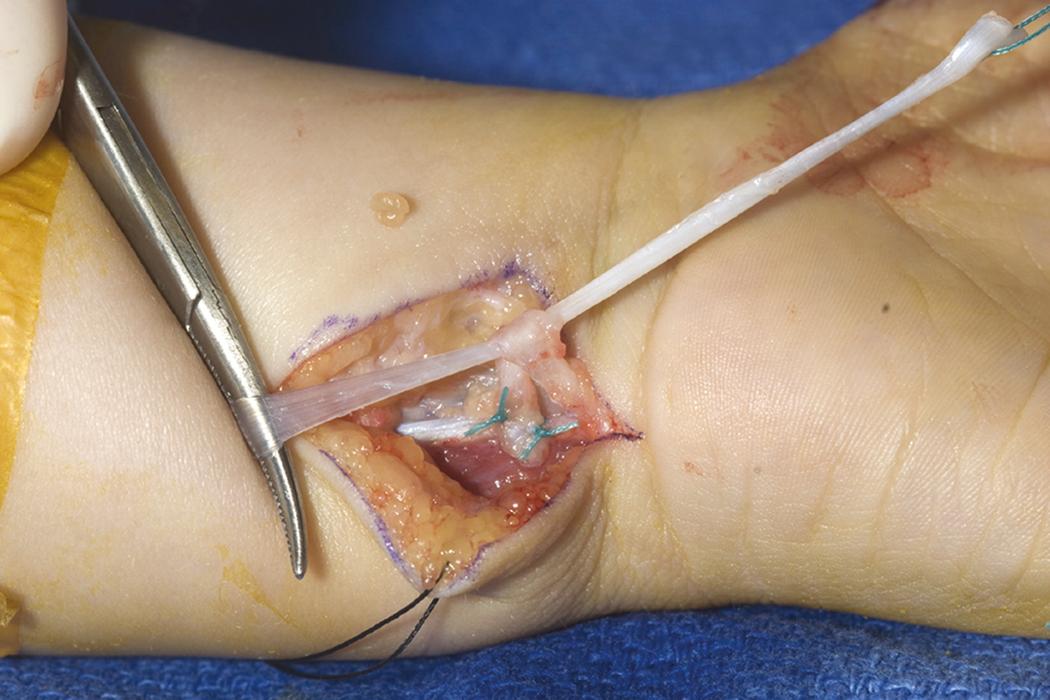
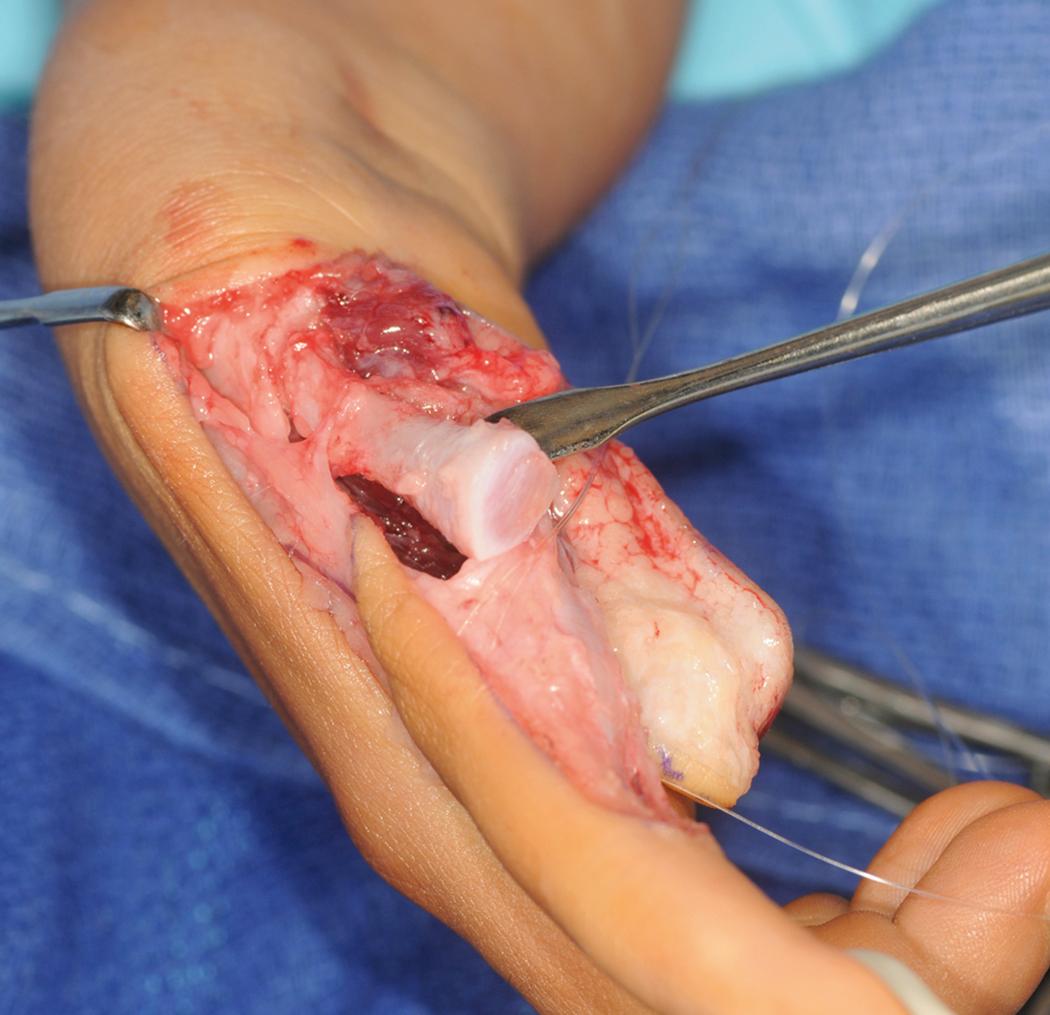
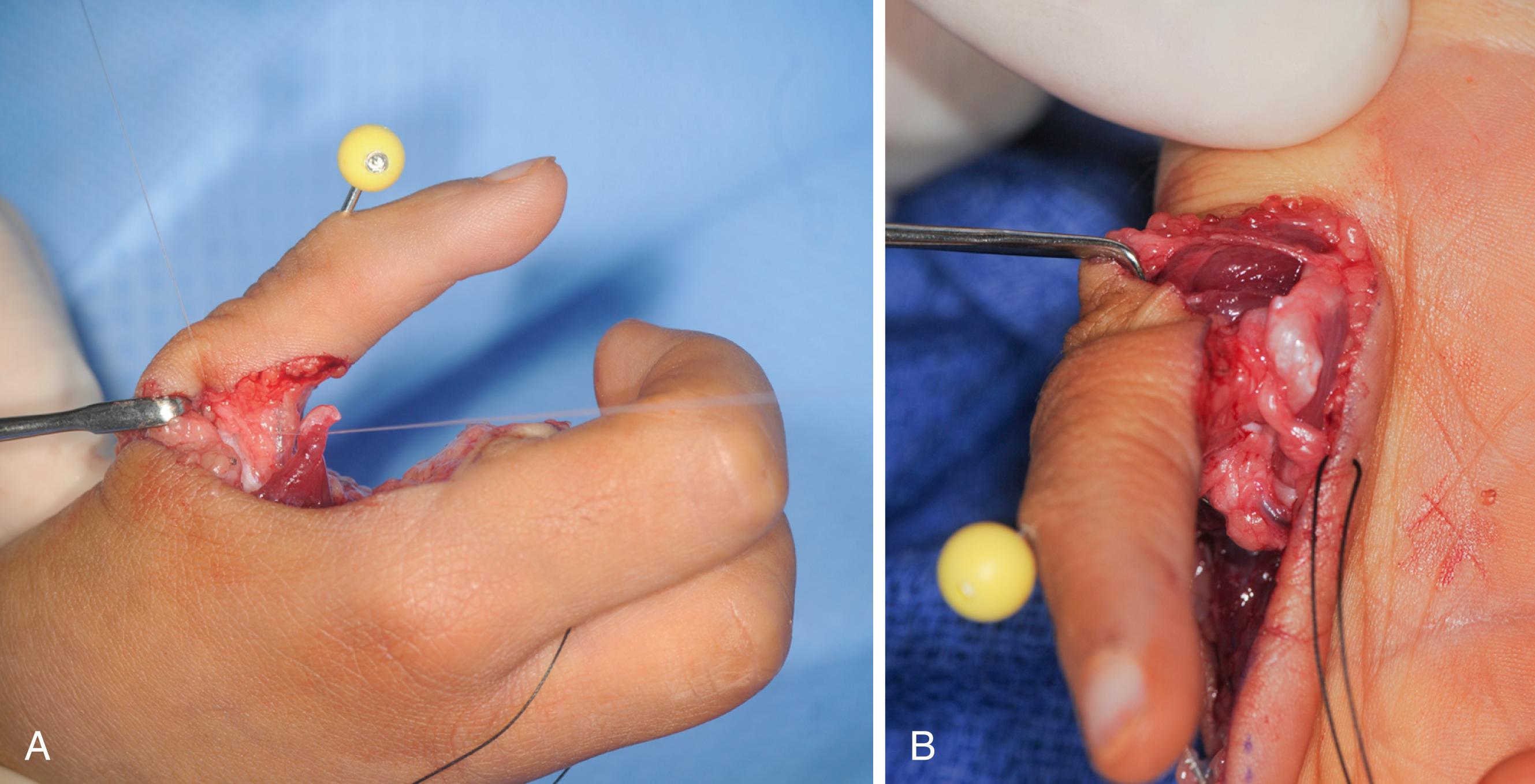
A subcutaneous tunnel is made between the radial side of the thumb and the volar forearm incision for channeling the ring finger FDS tendon. The FDS tendon is passed under the skin to the radial side of the thumb ( Fig. 37.12 ). The metacarpal head is isolated and a 0.045-inch Kirschner wire drilled across the metacarpal head parallel to the joint surface ( Fig. 37.13 ). Minifluoroscopy ensures appropriate Kirschner wire positioning. The hole is enlarged with a drill bit (cannulated if available) to allow passage of the FDS tendon. The MCP joint is reduced and stabilized with a longitudinal 0.045-inch Kirschner wire drilled antegrade from the tip of the thumb across the MCP joint. The wire is cut short and a Jurgan pin ball (Jurgan Development and Manufacturing, Madison, WI) applied. The FDS tendon is passed through the drill hole to the ulnar side of the thumb for ligament reconstruction ( Fig. 37.14 ). If the diameter of the tendon is too large, one slip of the FDS can be removed.


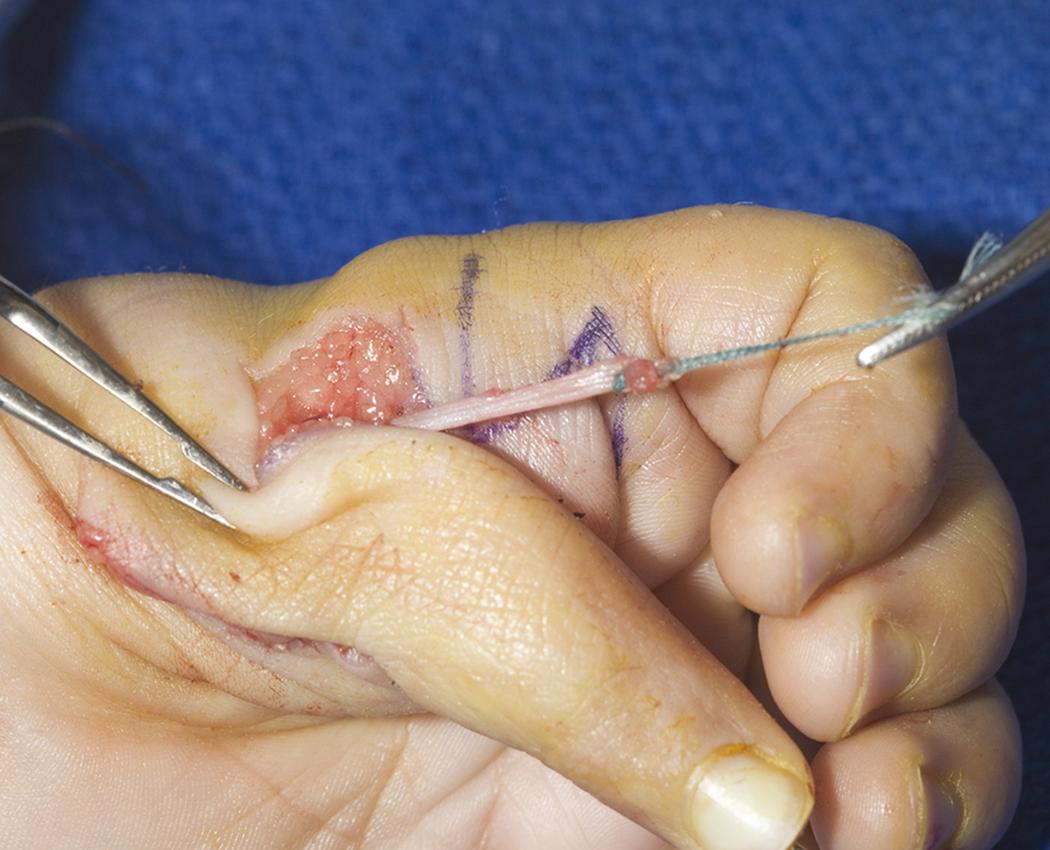
At this point, the wrist is placed into slight extension and the FDS tendon tensioned until the thumb is positioned in opposition. Tenodesis is used to assess tension, and typically the tendon can be seen tenting the palmar skin when the wrist is placed into extension. After correct tension is achieved, the FDS tendon is sutured to the surrounding bone and periosteum along the radial side of the thumb. This maneuver sets the tension in the opposition tendon transfer. The remaining FDS tendon that had been passed through the metacarpal head is used to reconstruct the UCL. The FDS tendon is directed to the base of the proximal phalanx and sutured directly into the bone. Usually, the FDS tendon is long enough that it can be passed back onto itself to complete a double-stranded repair ( Fig. 37.15 ).

The skin is closed with absorbable suture and the limb is immobilized in a long-arm thumb spica cast with the wrist in slight flexion and the thumb in opposition. After 3 weeks, the Kirschner wire is removed and a short-arm thumb spica splint is fabricated. Active motion and therapy are initiated. Protective splinting of the thumb is continued until 3 months after surgery.
Pollicization is indicated for types IIIB, IV, or V hypoplasia. The technique is similar for each type, with subtle variations depending on whether a hypoplastic thumb is present or absent. In type IIIB hypoplasia, vascularized fat from the ablated thumb can be used to augment the first web space or thenar eminence. , In type IV or V hypoplasia, there is insufficient vascularized fat, and this option is unavailable.
The current technique of pollicization represents a consolidation of contributions from surgeons over the past 100 years ( Box 37.2 , Case Study 37.2 , and ![]() ). , Following general anesthesia, the child is placed in the supine position. Preoperative antibiotics are routinely administered. The extremity is prepped and draped in sterile fashion. A sterile pediatric tourniquet (Delfi Medical Innovations, Vancouver, Canada) is placed on the upper arm. Exsanguination should be gentle so that some filling of the digital vessels can be maintained in order to facilitate visualization.
). , Following general anesthesia, the child is placed in the supine position. Preoperative antibiotics are routinely administered. The extremity is prepped and draped in sterile fashion. A sterile pediatric tourniquet (Delfi Medical Innovations, Vancouver, Canada) is placed on the upper arm. Exsanguination should be gentle so that some filling of the digital vessels can be maintained in order to facilitate visualization.
Limb is gently exsanguinated and the tourniquet is inflated
Skin incision proposed by Ezaki and Carter
Palmar skin is incised and the radial neurovascular bundle is isolated
Dissection proceeds in an ulnar direction to identify the common digital vessels to the index finger/long finger web space
Proper digital nerves to the ulnar side of the index finger and the radial side of the long finger are isolated
Proper digital artery to the long finger is ligated with a ligature clip
First annular pulley of the index finger is incised
Divide intermetacarpal ligament between index finger and long finger
Dorsal skin incision is sharply elevated with preservation of dorsal veins
Incise dorsal fascia between index and long metacarpals
The first dorsal and palmar interossei muscles are released with a portion of the hood
Metacarpal index finger is shortened by a saw cut at the metaphyseal flare and a knife cut through the physis leading to an epiphysiodesis
Index metacarpophalangeal joint is fixed into hyperextension using nonabsorbable suture material passed through the epiphysis and dorsal capsule
Kirschner wire drilled antegrade through the metacarpal epiphysis, into the proximal phalanx, and out the proximal interphalangeal joint
Kirschner wire used as a joystick to align the index metacarpal into 45 degrees of abduction and 100 to 120 degrees of pronation
Kirschner wire is drilled retrograde across the metacarpal base into the carpus
Transfer the first dorsal interosseous to the radial lateral band and the first palmar interosseous to the ulnar lateral band about the PIP joint
Skin is closed with absorbable suture with resection of any redundant skin and Kirschner wire is cut short
Emma is a 4-year-old with ulnar deficiency and marked left thumb hypoplasia ( eFig. 37.4 ). Treatment included bone and joint reorganization and muscle reorganization.

Bone and joint reorganization:
Distal interphalangeal (DIP) joint → Interphalangeal (IP) joint
Proximal interphalangeal (PIP) joint → Metacarpophalangeal (MCP) joint
MCP joint → Carpometacarpal (CMC) joint
Metacarpal → Trapezium
Muscle reorganization:
First palmar interosseous (PI) → adductor pollicis
First dorsal interosseous (DI) → abductor pollicis brevis
Extensor indicis proprius → extensor pollicis longus
Extensor digitorum communis → abductor pollicis longus
The surgical procedure is demonstrated in ![]() and eFig. 37.5 .
and eFig. 37.5 .
The challenging rehabilitation requires communication and experience ( eFig. 37.6 ) to achieve a successful outcome ( eFig. 37.7 and ![]() ).
).


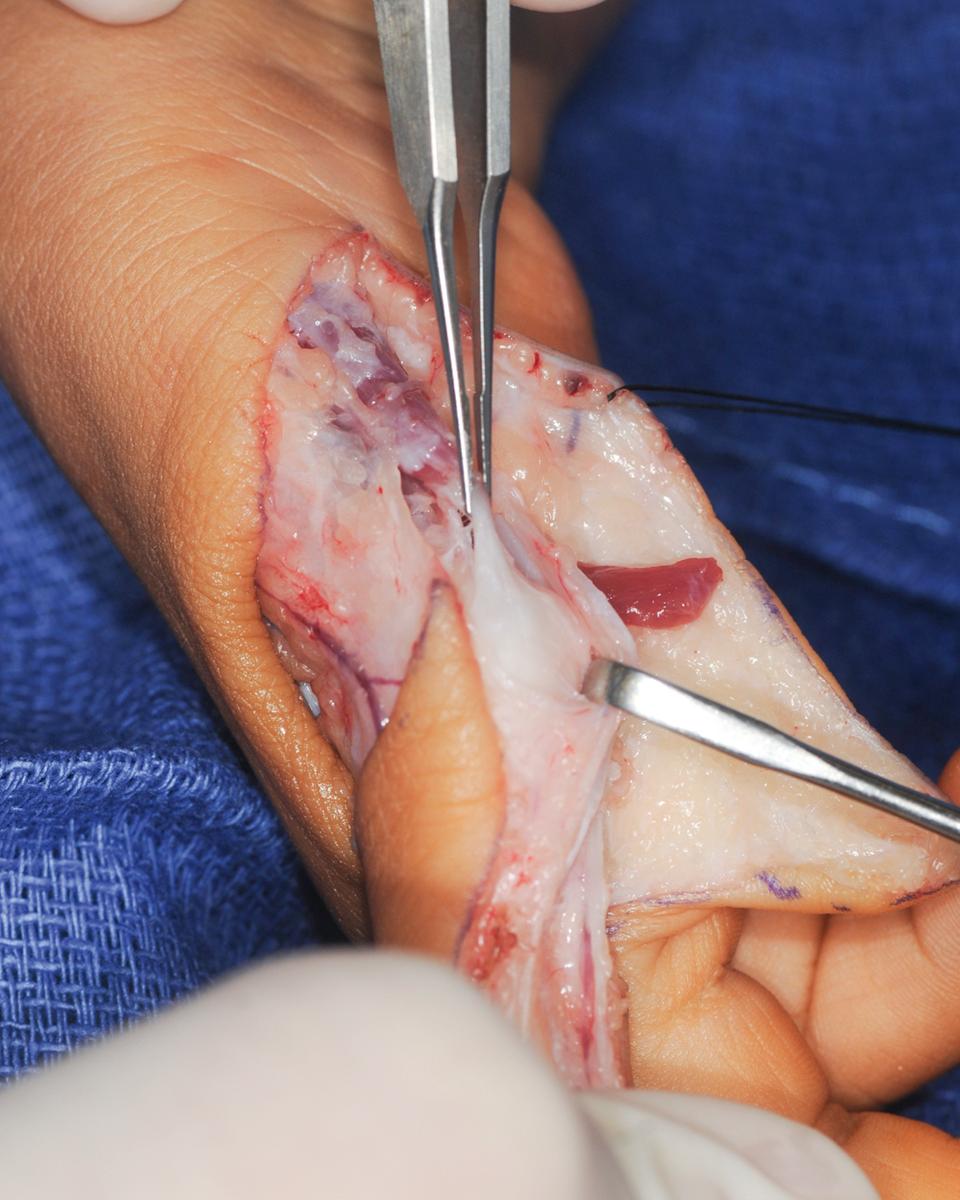
The skin incision must allow index finger transposition and reconstruction of an abundant thumb/index finger web space. The skin incision proposed by Marybeth Ezaki and Peter Carter is used because it allows more glabrous skin to be placed along the palmar aspect of the index finger ( Fig. 37.16 ). The palmar skin is incised first, and the radial neurovascular bundle is isolated, although the artery can be extremely small. In children with type IIIB or IV hypoplasia, the single vessel to the hypoplastic thumb can be traced to the radial neurovascular bundle of the index finger to ease identification ( Fig. 37.17 ). The dissection next proceeds in an ulnar direction to identify the common digital vessels to the index finger/long finger web space ( Fig. 37.18 ). The proper digital nerves to the ulnar side of the index finger and the radial side of the long finger are isolated. Proximal nerve microdissection is required to further separate the proper digital nerves prior to pollicization. On occasion, as the dissection of the digital nerve proceeds in a proximal direction, one will encounter a neural loop that encircles the artery. This loop must be addressed to prevent constriction of the artery during index finger transposition. The loop can be widened to avoid arterial compression or the smaller of the two nooses can be cut. The proper digital artery to the long finger is ligated with a ligature clip ( Fig. 37.19 ). This allows tension-free index finger pollicization vascularized by the radial digital artery and the common digital artery to the index finger/long finger web space. The ligature clip acts as a visual reminder of the location of the proper digital artery through the remainder of the surgery.

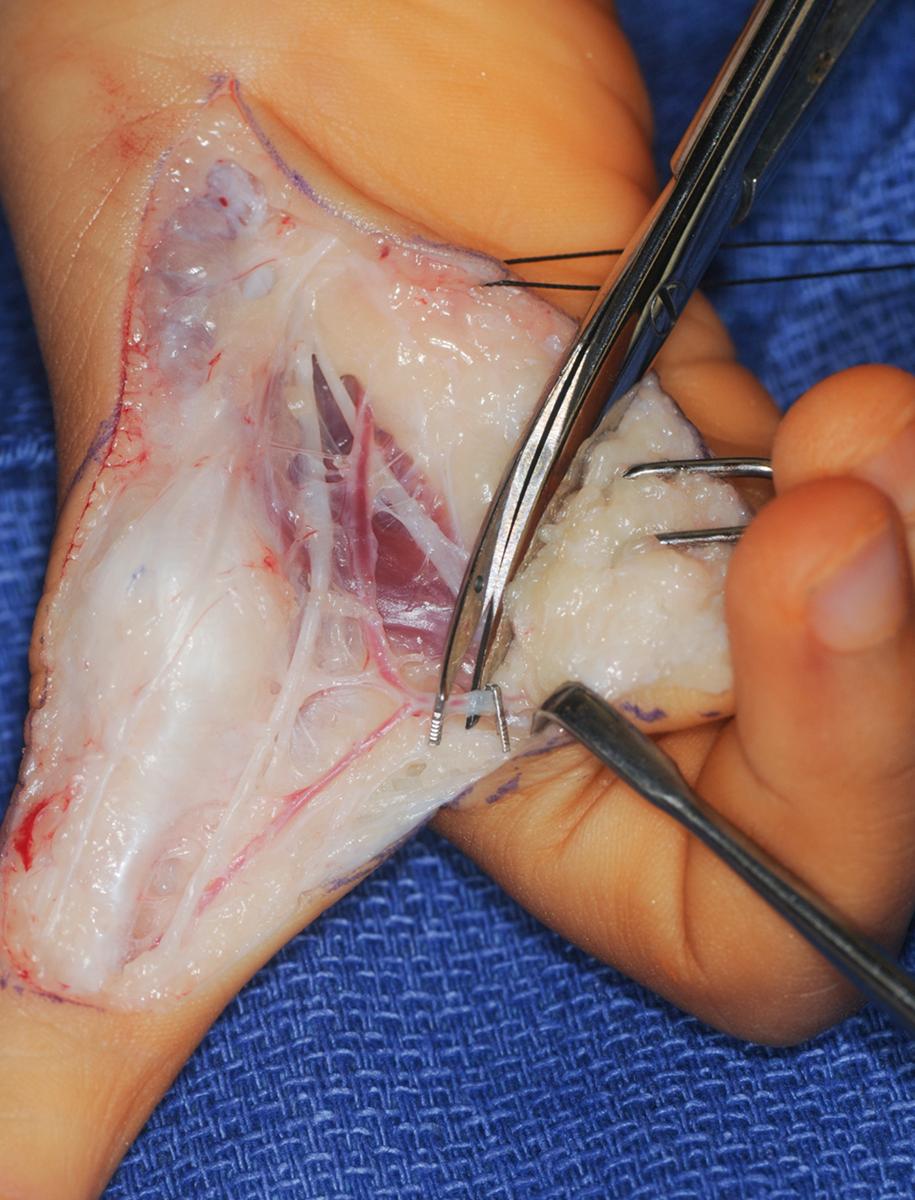
The first annular pulley of the index finger is incised to prevent buckling of the flexor tendons after index finger shortening ( Fig. 37.20 ). The intermetacarpal ligament is also divided ( Fig. 37.21 ). The dorsal skin incision is sharply elevated with preservation of as many dorsal veins as possible. The dorsal fascia between the index and long finger metacarpals is incised. The extensor or flexor tendons are not shortened because these musculotendinous structures adapt over time.
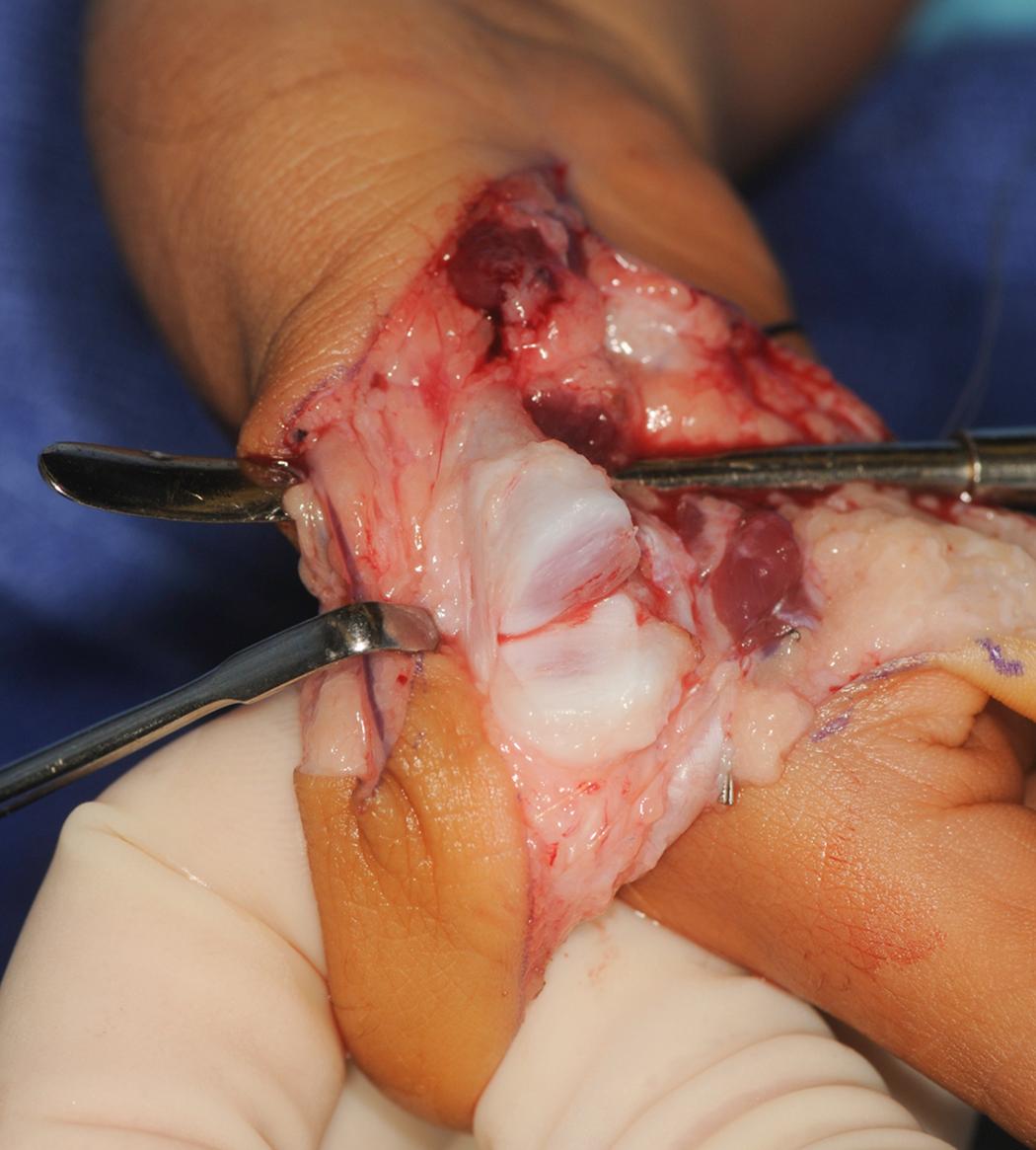
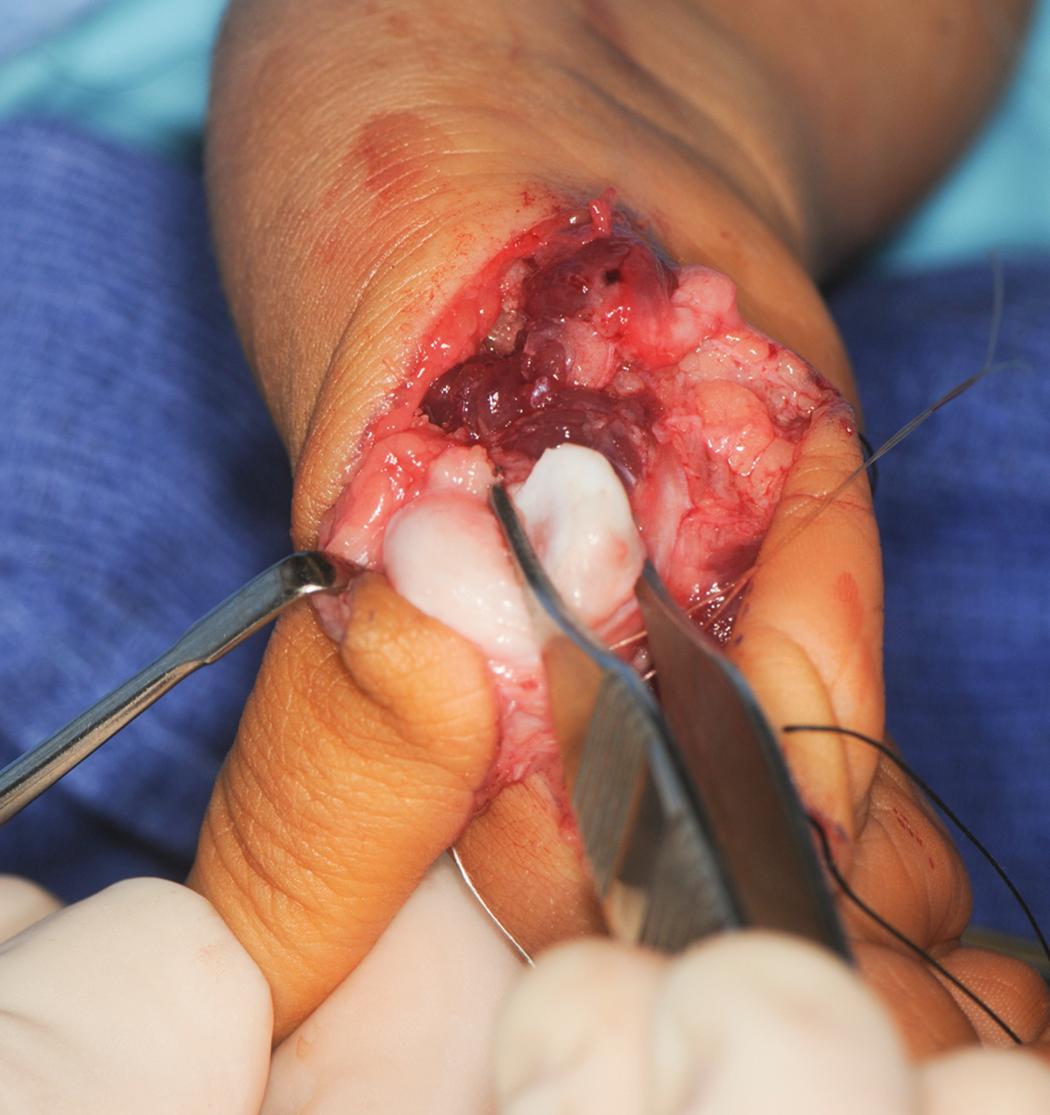
The first dorsal and palmar interosseous muscles are dissected to their attachments into the extensor hood ( Figs. 37.22 and 37.23 ). The interosseous muscles and tendons are released with a portion of the hood in expectation of transfer. The tendons must be carefully dissected from the MCP joint collateral ligaments to avoid entering the joint. The neurovascular bundles must also be shielded during elevation of the interossei. Prior to cutting the metacarpal, the eventual insertion sites for the tendon transfers are identified and tagged within the extensor mechanism over the PIP joint. This facilitates later transfer of the first dorsal and first palmar tendons into the radial and ulnar lateral bands, respectively.

The index finger must be shortened. The distal cut is made directly through the physis using a knife ( Fig. 37.24 ). This physeal cut leads to growth plate ablation (epiphysiodesis) to prevent unwanted growth of the index metacarpal. A fine-bladed saw is used to cut the metacarpal base through the metaphyseal flare in the plane of the intended thumb ( Fig. 37.25 ). The cut can be transverse or angulated to position the thumb in palmar and planar abduction. The index metacarpal bone is removed from its base to the epiphysis ( Fig. 37.26 ). A rongeur may be used to widen the base by opening or pedaling the surrounding cortex to promote healing ( Fig. 37.27 ).

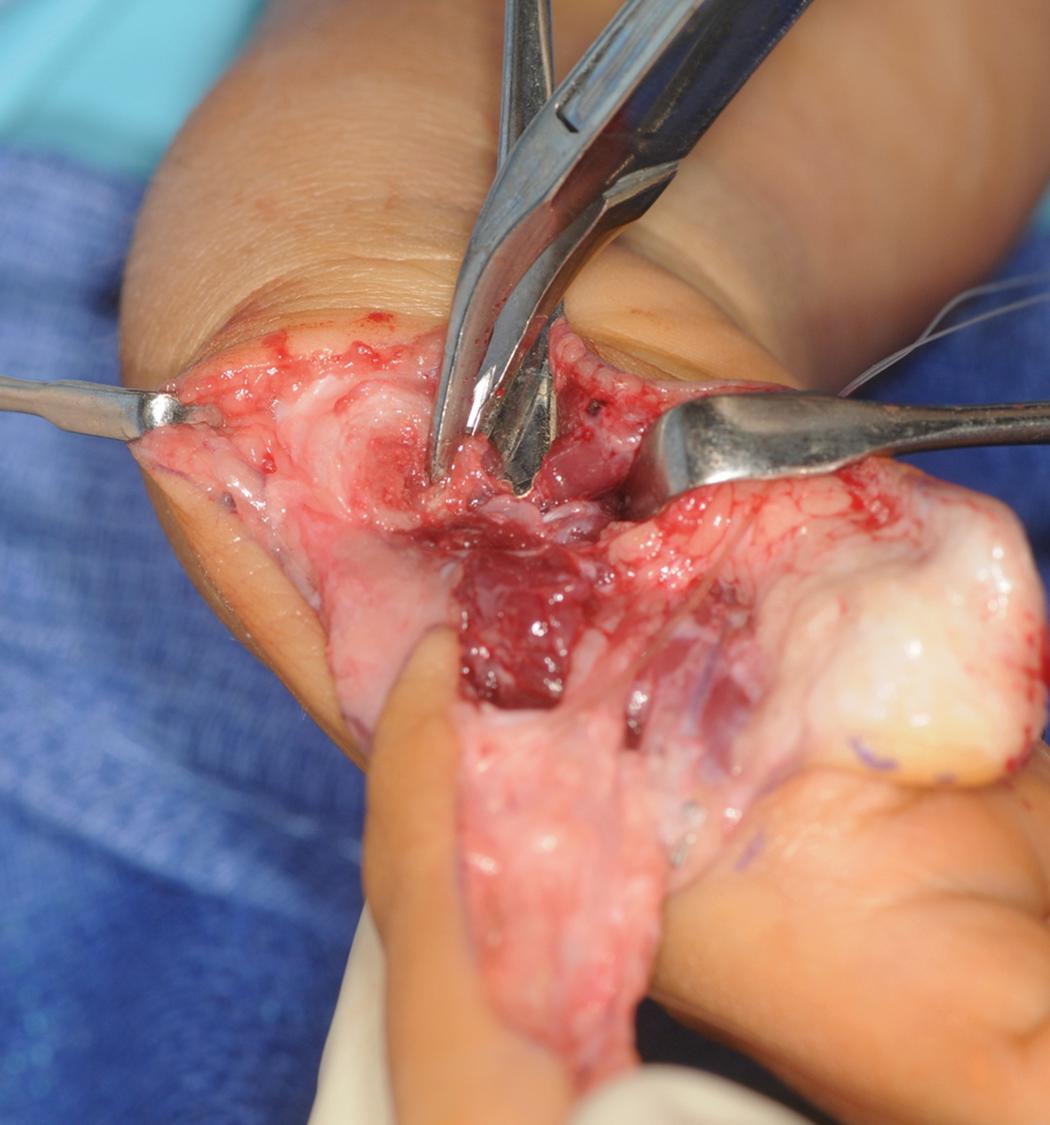
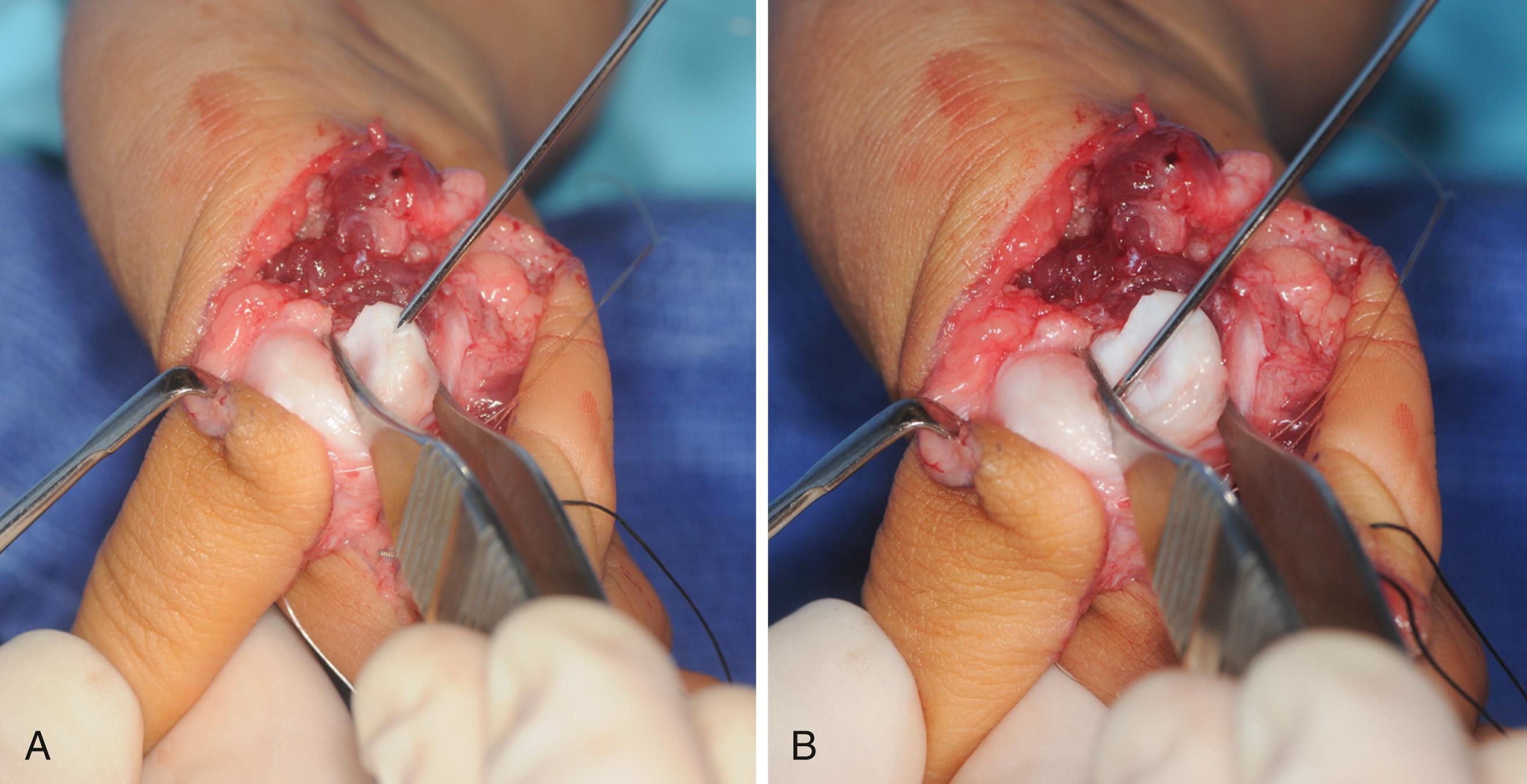
The normal index MCP joint hyperextends and the normal thumb CMC joint does not hyperextend. To correct this discrepancy, the index MCP joint is fixed into hyperextension, by placing the remaining metacarpal head into flexion ( Fig. 37.28 ). This metacarpal head position can be maintained with a Kirschner wire placed across the flexed metacarpal head or placed directly into the proximal phalanx blocking metacarpal head extension ( Fig. 37.29 ). The Kirschner wire is drilled through the proximal phalanx and out the PIP joint ( Fig. 37.30 ). This Kirschner wire is used as a joystick to facilitate index finger positioning ( Fig. 37.31 ). Interosseous sutures between the metacarpal base and index finger to augment fixation are rarely used. The index finger metacarpal epiphysis is aligned anterior to its metaphyseal base with meticulous positioning into 45 degrees of abduction and 100 to 120 degrees of pronation ( Fig. 37.32 ). Once the position is deemed satisfactory, the Kirschner wire is drilled retrograde across the metacarpal base into the carpus. The Kirschner wire is cut short and a Jurgan pin ball is applied. Further stability is achieved via tendon transfer of the first dorsal interosseous to the radial lateral band and the first palmar interosseous to the ulnar lateral band about the PIP joint ( Fig. 37.33 ). The skin is judiciously inset with absorbable suture. Any redundant skin is excised ( Fig. 37.34 ). Whenever possible, the first web space suture line is advanced dorsally to minimize any suture line within the commissure ( Fig. 37.35 ). The tourniquet is deflated and the “thumb” observed for 5 minutes. The arterial circulation typically returns rapidly, although vasospasm can result. Time, warm soaks, and patience routinely lead to resolution. Persistent lack of blood inflow requires exploration for arterial spasm that can resolve with lidocaine, arterial kinking, or iatrogenic injury. Venous congestion is a more common problem that requires reapplication of a looser dressing and/or release of any taut sutures.




Once adequate arterial ingress and venous egress has been established, the postoperative dressings are applied. Adequate fluffy dressings are necessary to equalize the anterior-posterior and medial-lateral dimensions of the hand. This allows uniform compression without constriction. A long-arm soft cast (Scotchcast Soft Cast Casting Tape, 3M, St. Paul, MN) is applied with the elbow flexed to more than 100 degrees and a substantial supracondylar mold to decrease the chance of unintended removal. This fiberglass casting tape can be unwrapped in the clinic, avoiding the frightening cast saw. The child is admitted overnight with the arm elevated to promote venous drainage. The thumb can be covered the next day once vascularity has been observed overnight.
The Kirschner wire is removed 4 weeks after surgery and a short-arm thumb spica splint is fabricated. Occupational therapy is started with an emphasis on thumb usage. The initial goal is large object acquisition followed by acquisition of smaller objects and eventually fine pinch. Standard wound care is also performed consisting of scar massage and wound softening techniques. Active motion and therapy are initiated. Protective splinting of the thumb is continued until 3 months after surgery.
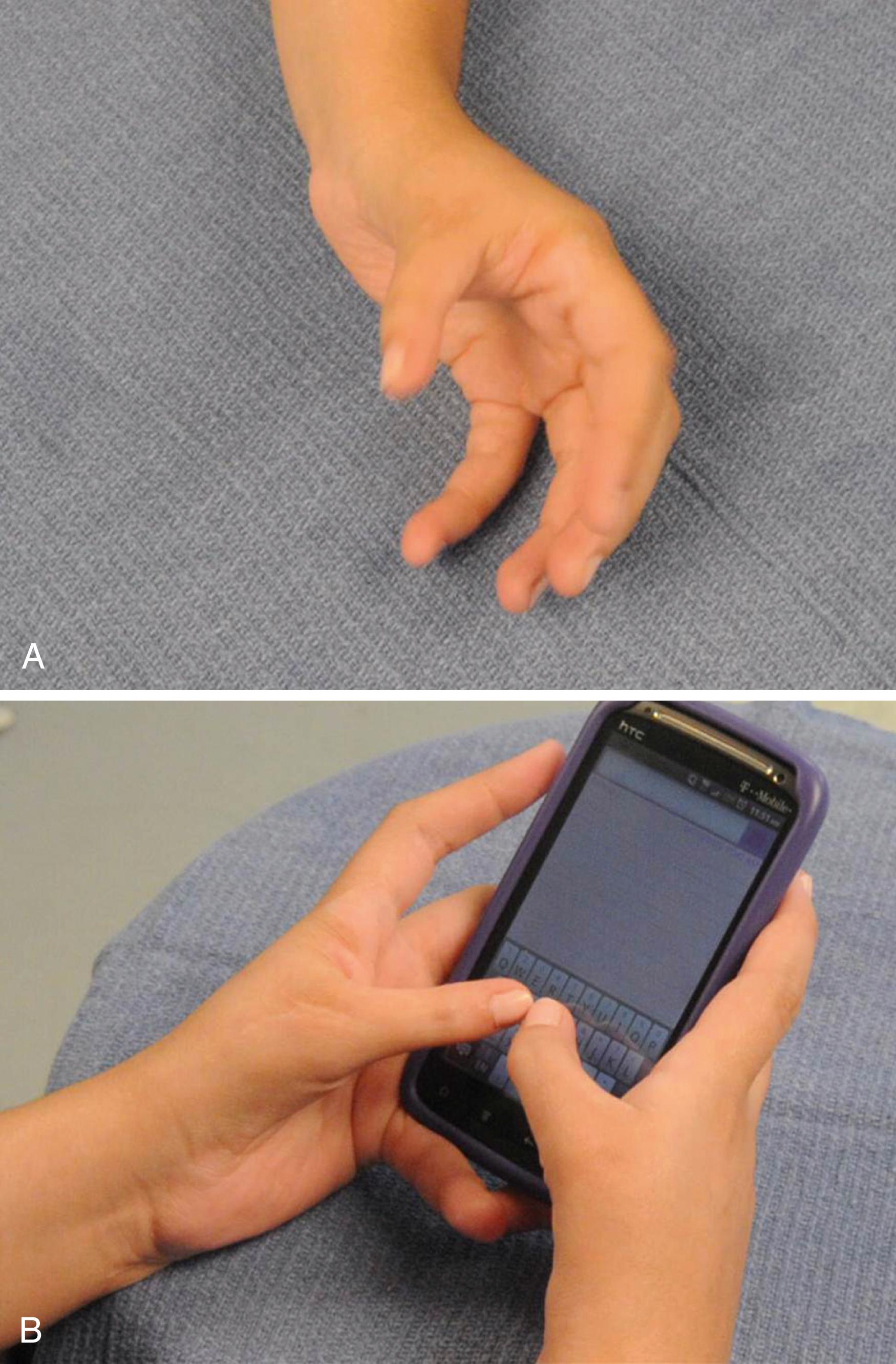
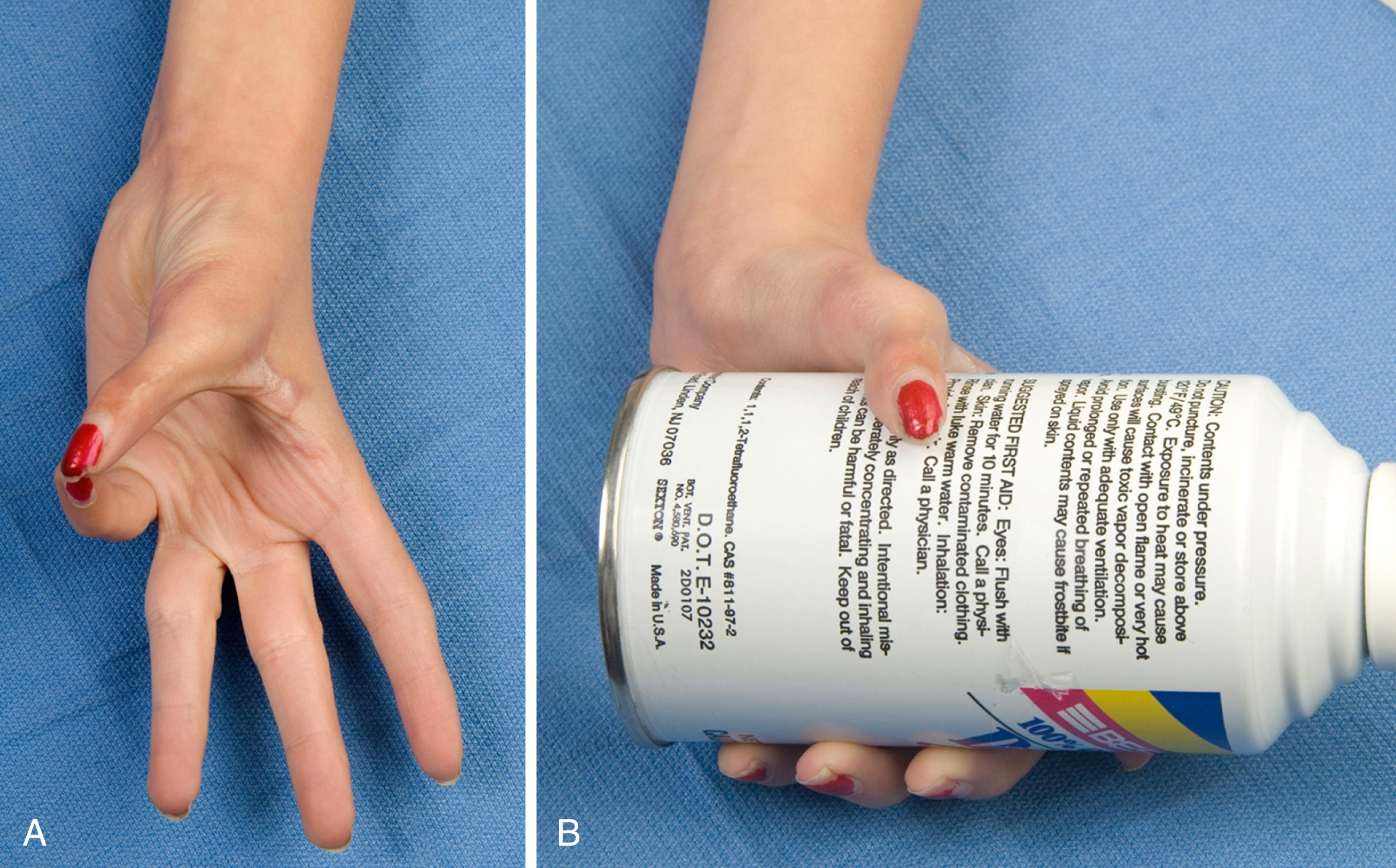
The results for thumb reconstruction for type II or IIIA hypoplasia are somewhat difficult to decipher because comparison among studies is confounded by the heterogeneity of the patient populations, severity of the hypoplasia, and reconstructive techniques used. Vuillermin et al. reported excellent function and Pediatric Outcome Data Collection Instrument (PODCI) scores in patients with ring FDS opposition transfer after 2 years of follow-up. No difference was found in the use of FCU or the transverse carpal ligament as a pulley. Wall et al. presented long-term outcomes after opposition reconstruction using the abductor digiti minimi muscle (Huber transfer). Patients had decreased range of motion and pinch strength compared with normal subjects but reported high PODCI and normal Patient-Reported Outcomes Measurement Information System (PROMIS) scores. If the surgical plan for reconstruction has addressed each deficient component of the thumb, the function following reconstruction is usually enhanced compared with the function present before surgery ( Fig. 37.36 ) (see ![]() , ). Some degree of MCP joint stiffness is inevitable after ligament reconstruction; however, this stiffness has little impact on functional outcome as long as the IP and CMC joints are supple.
, ). Some degree of MCP joint stiffness is inevitable after ligament reconstruction; however, this stiffness has little impact on functional outcome as long as the IP and CMC joints are supple.
The results of tendon transfers, bone lengthening, and joint stabilizations for higher-grade hypoplastic thumbs are poor compared with the results of pollicization. , , Children who require a five-digit hand for cultural reasons may gain some benefit from these procedures as long as the family has realistic expectations. ,
The results after pollicization depend mainly on the preoperative status of the index finger and surrounding musculature. Index finger pollicization provides better functional and esthetic results in isolated thumb hypoplasia than it does in patients with an associated hypoplastic or absent radius. A mobile index finger moved to the thumb provides stability for grasp and agility for fine pinch ( Fig. 37.37 ). Parents are extremely grateful and amazed at the results, often providing moving testimonials (see ![]() ). In contrast, a stiff index finger in the thumb position provides a stable thumb post for gross grasp but is unlikely to participate in fine pinch. Scissoring of adjacent digits is usually preferred for fine pinch in these cases. A pollicization that is stiff, weak, poorly positioned, and/or unstable will be bypassed in favor of scissoring pinch between adjacent long and ring fingers.
). In contrast, a stiff index finger in the thumb position provides a stable thumb post for gross grasp but is unlikely to participate in fine pinch. Scissoring of adjacent digits is usually preferred for fine pinch in these cases. A pollicization that is stiff, weak, poorly positioned, and/or unstable will be bypassed in favor of scissoring pinch between adjacent long and ring fingers.
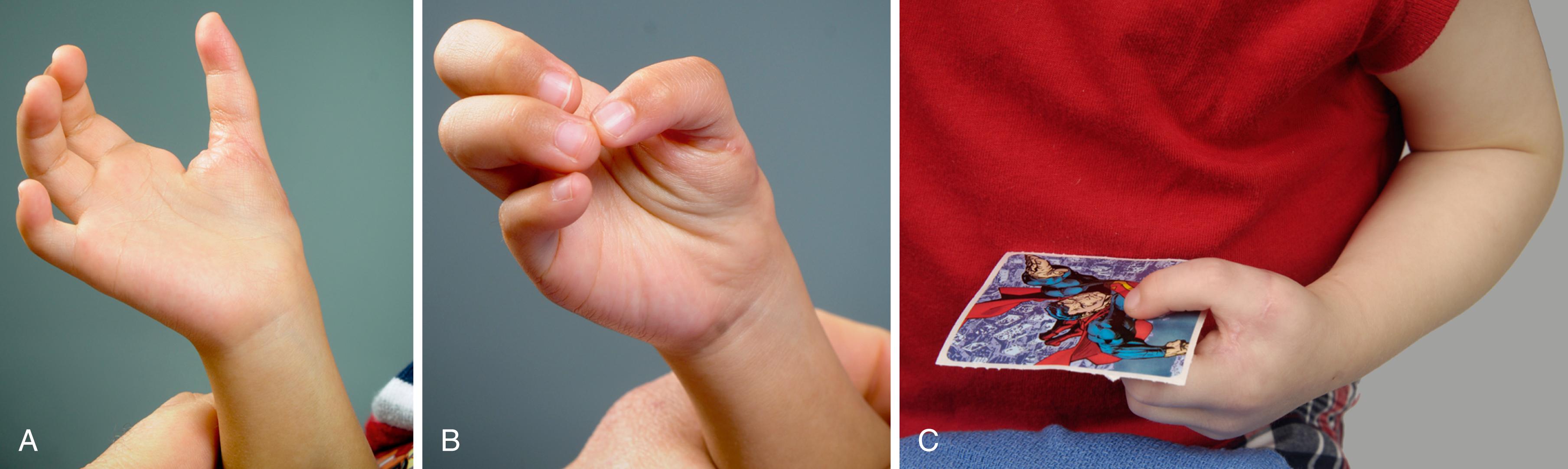
Zlotolow and colleagues correlated the primary caretaker’s subjective impressions of outcome to objective measures. A comprehensive subjective and objective measurement analysis was performed. The subjective results were correlated with objective data. The sticker test along with MCP joint and IP arcs of motion correlated best with children who preferred using their thumbs for small object acquisition instead of scissor pinch. Simply, the child’s ability to peel a sticker from its backing between the thumb and index correlated the strongest with the subjective interpretation of a digit that looked and worked like a thumb.
Tonkin et al. reported excellent/good functional outcomes in 77% of patients and excellent or good appearance in 94% after a mean of 5.7 years of follow-up. Worst outcomes were associated with patients with forearm and wrist anomalies. Lightdale-Miric et al. found that patients with pollicization had less strength but used different strategies to compensate and achieve normal dexterity. In their series, older patients at the time of surgery and more severely involved hands showed poorer results. Strugarek-Lecoanet et al. observed that 87% of pollicized thumbs maintained mobility of the reconstructed CMC joint after 8 years of follow-up. They also found a 40% of nonunion rate between the pollicized metacarpal epiphysis and its base that was not associated with higher rates of instability.
Kollitz et al. developed a new outcome measure for thumb use and incorporation into daily activities after pollicization, the Thumb Grasp and Pinch (T-GAP) assessment. This instrument uses a variety of tasks for three different age groups to assess grasp and pinch patterns. Scores correlated with pinch and grip strengths, opposition and grasp span, and parent and patient satisfaction. Further studies demonstrated excellent interrater and intrarater reliability. This same group longitudinally followed patients with pollicization across time and noted that improvement in dexterity and strength is the same rate as uninvolved children of the same age.
Children with a preoperative ulnar-sided grasp pattern secondary to perfect ulnar digit(s) finger mobility and stiff radial digits (often seen in patients with radial longitudinal deficiencies) will maintain their ulnar-sided grasp after pollicization and ignore the new thumb. Ulnar-sided grasp combined with a stiff index finger is a relative contraindication to perform pollicization ( ![]() ). Patients with mirror hands or five-fingered hands tend to have suboptimal results as well, although the reasons are unclear. One reason is the presence of forearm ulnar dimelia will negatively impact wrist and forearm motion. However, good results can be achieved with meticulous surgical technique combined with an experienced therapist ( Fig. 37.38 ;
). Patients with mirror hands or five-fingered hands tend to have suboptimal results as well, although the reasons are unclear. One reason is the presence of forearm ulnar dimelia will negatively impact wrist and forearm motion. However, good results can be achieved with meticulous surgical technique combined with an experienced therapist ( Fig. 37.38 ; ![]() ).
).
The results of pollicization continue into adulthood, with long-term studies showing sustained functional use of the thumb. In the majority of cases where the child used the index finger as a thumb prior to surgery, pollicization results in good to near-normal hand function in the long term ( ![]() ). With no associated conditions that could lessen the outcome, the child can expect about one-third of the strength of an unaffected thumb. Large object manipulation is typically better than small object manipulation, but overall approximately 95% of patients integrate the thumb into daily tasks. The objective and esthetic outcomes following pollicization have been compared with those of normal thumbs. Generally, the thumb created by pollicization was slightly longer than normal and smaller in girth. The most frequently cited negative perceptions of the thumb were decreased girth, excessive length, and angulation.
). With no associated conditions that could lessen the outcome, the child can expect about one-third of the strength of an unaffected thumb. Large object manipulation is typically better than small object manipulation, but overall approximately 95% of patients integrate the thumb into daily tasks. The objective and esthetic outcomes following pollicization have been compared with those of normal thumbs. Generally, the thumb created by pollicization was slightly longer than normal and smaller in girth. The most frequently cited negative perceptions of the thumb were decreased girth, excessive length, and angulation.
Timing of the surgery has not been demonstrated to affect functional outcomes, although most clinicians feel that operations done in younger patients better take advantage of cortical plasticity. Others have argued that social factors should be the impetus for surgery because the index finger already has cortical representation as a thumb and timing is less important. Pollicization simply makes the index finger appear and work more like a true thumb.
Cortical plasticity and motor relearning are hypothesized to play a critical role in functional development following pollicization. There is a large region of the sensorimotor cortex homunculus dedicated to the hand, and much of it is devoted to the thumb. Researchers are deciphering and understanding the changes in the sensorimotor cortex following injury, repair, and reconstruction. Techniques include transcranial magnetic stimulation, electroencephalography, magnetoencephalography, functional MRI, structural MRI, and positron emission tomography. Human cortical plasticity is a complex process that involves the unveiling of formerly quiescent connections and sprouting of active afferents from nearby cortical and/or subcortical regions.
Following hand transplantation, the original sensorimotor cortex map for hand activation is reestablished. The transplantation reverses the sensorimotor cortex loss that followed the hand amputation. Similarly, successful toe transfer to the hand produces temporal activation within the sensorimotor cortex consistent with cortical plasticity. Functional MRI has confirmed that when a patient learns to use the toe transfer there is an enlargement in the motor cortical representation. Practice amplifies the changes within the sensorimotor cortex. As the new motor skill is mastered, there is an ensuing decrease in the amount of cortical representation. , The precise effects of pollicization have yet to be studied; however, similar sensorimotor cortex changes are likely. Undoubtedly, essential alterations must occur in the sensorimotor cortex as the index finger becomes a thumb.
Another factor to consider when deciding on the timing of surgery is the size of the hand. Although the precise best age at which to perform surgery is unknown, the advantages of early surgery are lessened by the anatomic size of the neurovascular and musculocutaneous structures. We tend to perform surgery between 18 and 24 months of age, allowing the hand to grow, which eases the surgical procedure and still takes advantage of infant and toddler brain plasticity. However, other surgeons favor earlier intervention to promote a radial-sided (thumb-index) pattern of pinch. Late presentation, however, is not a contraindication for pollicization; the adolescent has less brain plasticity and is often astounded about the change in his or her hand. Preoperative discussion and review of pictures is mandatory to lessen the astonishment following the initial dressing removal.
Pollicization is a complex procedure with a host of big and small complications. Acute complications are related to vascular compromise. Arterial insufficiency results in failure of the thumb to “pink up” despite time, patience, and warm soaks. Immediate exploration is necessary for arterial kinking or injury. The principal problem needs to be rectified to preserve the arterial inflow into the thumb. The second vascular problem involves venous egress as the thumb turns blue. Rectification requires a series of steps, including loosening of the dressings or release of taut sutures. Subsequently, strict elevation is necessary to promote venous drainage. Loss of the index finger due to vascular compromise after pollicization is rare, with an estimated incidence of 0.2% when a skilled surgeon has performed the operation.
Long-term complications are related to scarring, stiffness, bony problems, and limited motion ( Table 37.3 ). First web space scarring and cicatrix require therapeutic modalities, such as silicone elastomer and massage. Dense recalcitrant scarring requires additional surgery to resurface the web space. Stiffness may be inherent in the index finger prior to pollicization and may not be amenable to treatment. Iatrogenic stiffness related to the surgery requires therapy to mobilize the thumb. Persistent stiffness may have a surgical solution, such as tendinous adhesions. Careful examination is necessary to determine the underlying cause. Bony problems can be related to joint instability, poor thumb positioning, or excessive thumb length. CMC joint instability is uncommon even with a fibrous union. Symptomatic instability, however, warrants revision surgery. A thumb positioned in excessive supination or pronation requires osteotomy and repositioning (see Fig. 37.39 ). A long thumb attributed to ongoing growth at the metacarpal physis requires epiphysiodesis and possible metacarpal shortening (see Fig. 37.40 ). Limited active motion in the presence of satisfactory passive motion is amenable to tendon transfer, such as an opposition transfer.
Thumb hypoplasia occurs in varying grades and is part of radial deficiency. Therefore appropriate workup for associated anomalies is mandatory.
The underdeveloped thumb has been classified into five types that guide treatment. The presence or absence of a stable CMC joint is the pivotal factor of retention and reconstruction versus ablation and pollicization.
Thumb reconstruction must address all the deficient elements including tight first web space, collateral ligament laxity, and absent thenar musculature.
Pollicization is the procedure of choice for type IIIB, IV, and V hypoplasia. Attempts at microsurgical joint transfer to restore the CMC joint in types IIIB and IV thumb hypoplasia have been reported; however, the results appear mediocre compared with those of index finger pollicization.
Pollicization requires a carefully designed skin incision and meticulous surgical technique. The neurovascular anatomy must be dissected with ligation of the radial digital artery to the thumb. The index finger metacarpal is removed from the physis to its base. The thumb is carefully positioned, and the intrinsic muscles (abductor pollicis brevis and adductor pollicis) are reconstructed with the first dorsal interosseous and first palmar interosseous, respectively.
Results after pollicization are related to numerous factors, including the status of the index digit, the surgical technique, and the ability to restore intrinsic muscle function. Early good results in childhood persist into adulthood.
| Complication | Causes | Management |
|---|---|---|
| First web space contracture | Insufficient web space reconstruction, loss of skin flap, scar formation | Therapeutic modalities Revision web space deepening via Z-plasty or dorsal rotational flap |
| Stiffness | May be attributed to preoperative condition of index finger or secondary to scarring related to surgery | Therapy; inherent stiffness not correctable; surgical adhesions can be treated by tenolysis |
| Excessive length | Failure to ablate index metacarpal growth plate | Epiphysiodesis and/or ostectomy of metacarpal |
| Malrotation | Technical error (underrotation or overrotation) or loss of fixation during postoperative care | Rotational osteotomy |
| Lack of opposition | Primary deficiency in intrinsic muscles or inability to reconstruct interossei | Opposition tendon transfer |

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here