Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Trauma is a leading cause of death for those aged 1 to 46 years and the third overall leading cause of death for all ages in the United States. Trauma accounts for nearly 10% of all deaths and 16% of disabilities worldwide and is the most common cause of life-years lost before 75 years of age. Hemorrhage used to be the most common cause of death in trauma patients; however, improved and advanced management of hemorrhage with balanced perfusion has improved the outcome and a zero preventable death target might be achieved following the recommended guidelines. Over the years, deaths due to exsanguination have decreased and deaths due to CNS injury and sepsis with systemic inflammatory response syndrome (SIRS) and multiorgan failure (MOF) have increased. Multiorgan failure and sepsis in trauma patients are a result of the systemic response of the body to trauma consisting of the secretion and activation of a series of cellular and humoral factors ( Fig. 1 ). The metabolic and hormonal response adds to the complications of the hemorrhagic and immune response to trauma. The interlinked abnormalities of the inflammatory response, coagulopathy, microcirculatory compromise, suppression of defense ability, immunoparesis, and ischemia-reperfusion injury increase the risk of multiorgan failure and mortality. Immunoparesis also increases the risk of infection during initial surgery and later reconstructive surgery in major trauma patients. Thus, it is important to modulate the immune response for a better outcome. Early diagnosis and treatment of sepsis improve the clinical outcome. Increased understanding of the pathophysiology of systemic immune response and biology of organ damage with a panel of biomarkers for early diagnosis and intervention to modulate inflammatory response may improve outcomes. The role of various pro- and anti-inflammatory cytokines (interleukin [IL[-1, IL-2, IL-4, IL-6, IL-8, IL-10, IL-12, tumor necrosis factor alpha [TNF-α]), C-reactive protein (CRP), and growth factors (transforming growth factor beta), complement fragments (C3a, C5a), procalcitonin (PCT), and N -terminal C natriuretic peptide (NT-CNP) as biomarkers in trauma has been discussed; however, careful investigation on newer biomarkers is warranted to further improve the survival in polytrauma patients. Laboratory research and clinical trial may play an important role in understanding the inflammatory signaling and to investigate the newer biomarkers. In this chapter, we will first discuss the pathophysiology of SIRS followed by the role of research in the advancement of the care in trauma patients focusing on investigating novel biomarkers.
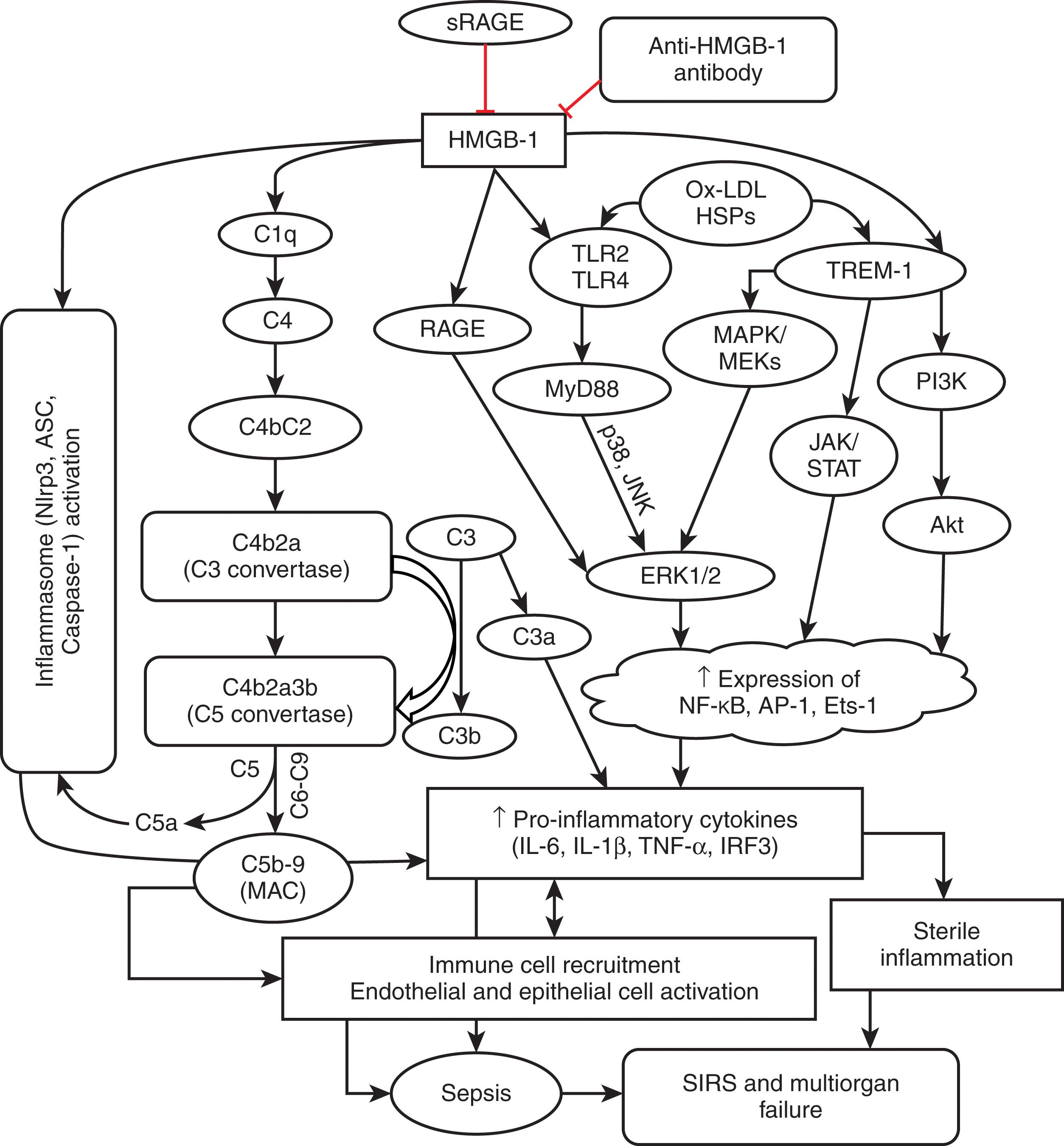
Traumatic injury results in the release of endogenous factors termed “damage-associated molecular patterns” (DAMPs) such as mitochondrial DNA, histones, high mobility group box protein-1 (HMGB-1), S100 proteins, and heat shock proteins (HSPs) from necrotic cells or by activated immune cells such as neutrophils. The secreted DAMPs act as sterile stimuli/signals and activate immune cells including neutrophils and monocytes and induce inflammation. Inflammation after trauma may also be rendered by activation of the complement system. Both reduced and disulfide forms of HMGB-1 activate the classical complement pathway (C3 and C4) leading to the generation of C3a and C5a. This results in the production and release of inflammatory cytokines such as IL-1β, IL-6, IL-8, interferon-gamma (IFN-γ), and TNF-α, etc., and evokes an immune response and sterile inflammation to restore the hemostasis. Increased secretion of proinflammatory cytokines and the formation of membrane attack complex (MAC) results in immune cell recruitment and epithelial and endothelial cell activation. Exposure of the endothelium to proinflammatory cytokines makes it more porous and allows increased access to the mediators of tissue damage resulting in increased concentration of these mediators in intercellular space. These events lead to SIRS, an inflammatory response to exsanguination, and tissue damage after an injury ( Fig. 2 ).
The onset of SIRS is associated with a compensatory anti-inflammatory response characterized by increased secretion of anti-inflammatory cytokines such as IL-10 and transforming growth factor beta. The compensatory anti-inflammatory response reduces the potentially harmful effects of acute inflammation but also increases the susceptibility to secondary infections, which leads to increased risk of sepsis and multiorgan failure. An initial inflammatory response (acute inflammation) is essential for healing by clearing the pathogens and wound debris through phagocytic immune cells, and this immune response is normalized in 3 weeks following trauma. A balance between pro- and anti-inflammatory mediators results in a return to baseline; however, an imbalance between pro- and anti-inflammatory mediators or a longer duration of inflammatory response results in chronic inflammation (see Fig. 1 ). Chronic inflammation leads to an increased risk of sepsis and multiorgan failure. Multiorgan damage and SIRS is also mediated by the activation and degranulation of polymorphonuclear neutrophils (PMNs) via circulating mitochondrial DAMPs after trauma. Ameliorating late inflammatory response or chronic inflammation may lead to improved outcomes. This might be achieved by regulating proinflammatory and anti-inflammatory responses in trauma patients, and therefore modulating immune response is important to improve the outcome. Additionally, targeting mediators of sterile inflammation could lead to the development of potential therapeutics.
Sepsis after a polytrauma increases the risk of multiorgan failure and overall morbidity and mortality. In the last two decades, the incidence of posttraumatic sepsis has decreased but the mortality is still high and is in the range of 19.5% and 23%. Higher mortality in posttraumatic patients may be attributed to delayed diagnosis because of the time needed for bacterial culture as well as negative bacterial culture. In polytrauma patients, early diagnosis and intervention with antibiotics can improve the prognosis and clinical outcome. There is a need to identify the factors involved in the development of sepsis and to develop a panel of biomarkers for early diagnosis and prediction of patient status, and in-depth research and large-scale clinical trials are warranted. An ideal biomarker should truly measure a molecular species or its relevant biological activity, should discriminate between patients with or without a disease, and should be able to facilitate a clinical decision to improve patient outcomes. For this, there is a need for a deep understanding of the pathophysiology of sepsis, well-planned research, and large-scale clinical trials. The probable role of potential biomarkers has been discussed in sepsis such as procalcitonin, C-reactive protein, IL-1, IL-6, IL-10, IL-18, neopterin, pancreatic stone protein/regenerating protein, NT-proCNP, polymorphonuclear elastase, lactate clearance, monocyte human leukocyte antigen DR (mHLA-DR), CD11b, toll-like receptor (TLR)-9, and soluble thrombomodulin (s-TM) level. Despite the presence of various biomarkers for sepsis, early diagnosis is still a challenge, and this may be attributed to the fewer clinical studies performed in polytrauma patients to elucidate biomarkers of sepsis or limited evidence for a biomarker in polytrauma patient and conflicting results of various studies. Further, complement activation plays a crucial role in the sepsis-induced multiorgan failure, targeting complements including sC5-9, and soluble complement regulators (C1 inhibitor, C4b-binding protein, factors H and I, clusterin, and S-protein, vitronectin) might be a potential therapeutic target. Inhibition of complement activation, improved motor function in acute spinal cord injury, and decreased number of C9- and CD59-positive cells with soluble complement receptor type 1 in rat model suggest the potential of targeting complement to improve the outcome. Since no clinical trials have been conducted targeting the complement activation and downstream signaling, well-organized large-scale clinical trials should be the focus of research.
High mobility group box 1 (HMGB-1) is a highly conserved nuclear protein released by the injured or necrotic cells into the cytoplasm, and it plays a key role in sterile inflammation. Nuclear HMGB-1 maintains chromatin structure and regulates transcription; cytoplasmic HMGB-1 induces inflammasome activation, inflammation, autophagy, and apoptosis; and extracellular HMGB-1 regulates cytokine and chemokine production, tissue repair and angiogenesis, and immune response. This suggests that the role of HMGB-1 in inflammation and homeostasis is location dependent and can have both protective and detrimental effects. HMGB-1 secretion is regulated by a feed-forward loop through secreted HMGB-1 and by the exposure of the monocytes with apoptotic bodies. HMGB-1 secretion is also mediated by the exposure of the immune cells such as monocytes; macrophages; neutrophils; dendritic cells; endothelial cells; platelets to proinflammatory cytokines including TNF-α, IL-1β, IFN-γ; microbe-associated molecular patterns; and pathogen-associated molecular proteins. In the case of sterile inflammation, activation of exportin 1 or chromosomal maintenance 1 due to oxidative stress results in increased HMGB-1 secretion and is regulated by nuclear factor erythroid 2-related (Nrf2) (see Fig. 1 ). These results suggest that HMGB-1 plays a crucial role in inducing inflammation in polytrauma patients. Thus, an in-depth understanding of the downstream signaling and targeting them may improve the outcome.
The role of HMGB-1-mediated vital organ injury after trauma, including ischemia-perfusion-mediated solid organs injury including liver, heart, kidney, and nervous system via TLR4/receptor for advanced glycation end products (RAGE)-dependent reactive oxygen species production and the association with inflammation has been discussed. TLR4 is the primary target of extracellular HMGB-1, and the role of HMGB-1-TLR4 axis in trauma-induced inflammation and the sterile injury was evaluated by Levy et al. The study found increased levels of HMGB-1 after injury, and neutralizing HMGB-1 with antibodies to HMGB-1 lowers the levels of IL-6, IL-10, alanine aminotransferase and decreased hepatic and gut mucosal nuclear factor-kappa beta activation compared with the control mice, suggesting a critical role of HMGB-1-TLR4 axis in the initiation of systemic inflammation and end-organ injury. HMGB-1 levels significantly increase from 1 to 6 hours after a traumatic injury; investigating biomarkers of inflammation or SIRS and the time of surgical intervention for repair is very important. Increased HMGB-1 expression during the first 6 hours followed by a decline in association with a lower level of Nrf2 initially and then an increase, as found by Polito et al, suggests the role of HMGB-1 in inducing inflammation in traumatic patients as well as the relationship between the levels of HMGB-1 and Nrf2. The study documented that increasing levels of Nrf2 during the first 24 hours and a lower level of HMGB-1 after 6 hours suggest that Nrf2 might be controlling the release of HMGB-1, and this notion is supported by previous studies that Nrf2 regulates HMGB-1 release via modulation of ROS levels (see Fig. 1 ). The study suggested that along with HMGB-1, Nrf2 should be considered as a biomarker of SIRS to improve the outcome. Posttraumatic HMGB-1 release also results in the activation of inflammasomes including Nlrp3, ASC, and pro-caspase-1 which in turn increase secretion of proinflammatory cytokines (IL-1β, IL-18) resulting in sterile inflammation (see Fig. 2 ). Inflammasomes can also be activated by complement C5a. NIMA-related kinase 7 (NEK7) is another upstream factor involved in NLRP3 inflammasome activation and might be another potential therapeutic target. The role of NEK7 in neuroinflammation and NLRP3 activation causing brain injury after trauma is suggested by the reversal of neurological deficits, NLRP3 inflammasome activation, and neuronal apoptosis by NEK7 downregulation. Since complement pathways are involved in sterile inflammation after a trauma, the inflammasome complex might play a crucial role and may serve as a novel biomarker and therapeutic target. This notion is supported by a significantly decreased number of injury-induced degenerating neurons, recruited inflammatory cells, and cortical lesion volume and significantly decreased expression of NLRP3, ASC, IL-1β, TNFα, inducible nitric oxide synthase, and caspase-1 with JC124, an NLRP3 inflammasome inhibitor, in a mouse model with traumatic brain injury.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here