Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Noncontrast magnetic resonance imaging (MRI) is standard of care imaging in the posttraumatic knee with clinical findings suggestive of ligamentous injury. MRI readily delineates injuries of the cruciate ligaments and offers a distinct advantage in preventing unnecessary arthroscopy by assessing the severity of the anterior cruciate ligament/posterior cruciate ligament (ACL/PCL) tear and other coexisting injuries. In addition, MRI is ideally suited for the evaluation of pain or instability in the postoperative patient by allowing assessment of graft integrity, graft ganglia formation, or hardware failure. MRI findings of partial and complete, and acute and chronic ligament tears throughout the knee are well described. With this in mind, MRI review should be systematic, with every effort made to identify the injury mechanism, and thus should focus on osseous, ligamentous, and cartilaginous structures at risk for acute trauma, while identifying chronic and degenerative lesions that might not be related to the recent injury.
The ACL arises proximally from the intercondylar notch of the lateral femoral condyle and inserts distally on the anteromedial (AM) tibial plateau in the anterior intercondylar region, which follows an oblique course with a mean sagittal angle of 54 to 55.5 degrees (angle measured between the ACL and the tibial plateau). The ligament is intra-articular but extrasynovial surrounded by a synovial layer separating it from the joint space, which contains a periligamentous arterial plexus that supplies the ACL with its own blood supply. The hemarthrosis that occurs with an acute ACL disruption is secondary to the disruption of this periligamentous plexus. Its fibers are distributed into two bundles with nomenclature according to their tibial insertions, known as the anteromedial bundle (AMB), which attaches proximally at the lateral femoral condyle more superomedially, and the posterolateral bundles (PLBs), which attaches at the lateral femoral condyle more laterally and distally. It measures approximately 38 mm in length and 11 mm in width. The AMB is longer and measures approximately 34 to 39.8 mm in length and 4.3 to 5.7 mm in width, whereas the PLB is shorter and measures 18 to 23 mm in length and 4.6 to 6 mm in width.
There is a reciprocal tension pattern shared between the AM and posteromedial ACL bundles. In flexion the AM band becomes taut while the posterolateral band is lax; however, during extension the opposite occurs when the posterolateral band becomes taut and the AM band is lax. This process maintains the ACL under tension throughout the different phases of normal biomechanics by activating the different ligamentous bundles, allowing for knee stability; especially during flexion, the stronger AM band provides the necessary stability.
There is a natural tendency of anterior tibial translation, which is prevented by both bundles of the ACL based on the position of the knee. In flexion, the main stability against anterior tibial translation is provided by the AM band. The anterior drawer tests for deficiency of this bundle, which is performed at 90 degrees of flexion—the knee position that places most tension on the AM bundle. Conversely, with the knee in extension, the PLB becomes “activated,” preventing anterior tibial translation; thus posterolateral band deficiencies are more commonly identified by the Lachman test and the pivot shift exam. Furthermore, the PLB plays a pivotal role in maintaining rotational stability during terminal extension of the knee, allowing tibial external rotation relative to the femur and aiding to “lock” the knee in extension.
The most important sign of an ACL tear is disruption or discontinuity of the fibers. ACL tears can be classified as partial or complete. Partial tears represent less than a third of the cases and can be further described as minor tears involving just a few fibers, a low-grade partial-thickness tear (involving less than 50% of the ligament thickness), or a high-grade tear (involving more than 51% of the ligament thickness but not the entire width). An attempt should be made to describe the degree of involvement based on ligamentous thickness affected. A partial tear can involve both or only a single bundle to varying degrees. Sometimes ACL insufficiency can be caused by plastic deformity without fiber discontinuity. Visualization of distal partial tears near the tibial insertion may be somewhat challenging, but presence of diffuse, high signal intensity with nonvisualization of the normal, linear, high signal intensity of the distal stripes qualifies as a partial distal tear of one or both bundles depending on the anatomic distribution of signal alteration.
An acute, complete ACL tear presents as ligament discontinuity with abnormal high signal intensity and complete ligamentous disruption (direct signs of ACL tear). The tear can occur proximally, at its midsubstance, or distally and may present with a mechanical block caused by the stump with resultant surrounding inflammation and fibrosis. Complete disruption most often occurs in the middle of the ACL and often leads to an abnormal slope or posterior bowing of the distal fibers. Secondary signs may be seen in the majority of complete ACL tears and include lateral tibiofemoral compartment contusions like the ones present in “pivot-shift” injuries involving the terminal sulcus of the lateral femoral condyle and the posterior aspect of the lateral tibial plateau, less than 45-degree angles between the lateral tibial plateau and a buckled course of the PCL with indentation of the distal part of the PCL and anterior displacement of the tibia. These indirect signs lack sensitivity, and the absence of these signs does not exclude presence of an ACL tear.
The main mechanism of injury of the ACL includes internal rotation of the femur relative to a fixed tibia with the foot planted beyond the stretching ligamentous capability in a sudden deceleration and rotation maneuver common in contact sports, such as football, or while skiing. Partial ACL tears most commonly involve the AM band of the ACL. Injury mechanisms as a whole are the same for partial tear and complete tear. The most common contact-related injury is the “clipping” type injury sustained in football. Pivot shift is a low-energy noncontact injury common in such sports as basketball, football, or rugby that can occur with the knee in flexion while the foot is fixated, by applying a valgus (lateral) force to the knee, causing internal rotation of the tibia or external rotation of the femur, which can produce an O'Donoghue unhappy triad comprised of an ACL tear, a medial collateral ligament (MCL) tear/sprain, and a medial meniscal tear. The pivot-shift mechanism of injury is one of the most common mechanisms resulting in tear of the ACL. This type of injury occurs during rapid deceleration combined with simultaneous sudden change of direction. After the ACL tears, it allows the tibia to translate anteriorly relative to the femur, resulting in impaction of the tibia against the femur, giving rise to the reciprocal bone bruise pattern in the lateral femoral condyle and posterolateral tibial plateau, known as the “pivot-shift” marrow edema pattern.
Hyperextension injuries can occur during jumping or high kick maneuvers with or without a varus force can result in ACL disruption and frequently occur without associated collateral ligament or meniscal injury. This kissing contusion pattern associated with this type of injury results from impaction of the anterior tibia against the anterior femur. The third mechanism is external rotation of the tibia relative to the femur with a varus (medial) stress leading to impaction/bone bruise in the medial knee compartment and distraction laterally resulting in avulsion of the lateral tibial rim (Segond fracture) and injury/tear of the lateral collateral ligament (LCL).
Careful observation and assessment of osseous contusions about the knee should serve as a guide for interrogation regarding suspect soft tissue structures likely to be injured based on specific mechanisms. Osseous contusion patterns often elucidate the mechanism of injury and guide the evaluation for subsequent pathology. Five dominant osseous contusion patterns described by Sanders and associates play a key role in diagnostic MRI interpretation of knee ligament trauma. These include pivot-shift injury, dashboard injury, hyperextension injury, clip injury, and lateral patellar dislocation. MRI evaluation for osseous contusion is facilitated by the use of T2 fat-saturated sequences. Contusions appear as subcortical or subchondral regions of increased T2 signal and decreased T1 signal, often with a flame-shaped configuration, without a discrete fracture line.
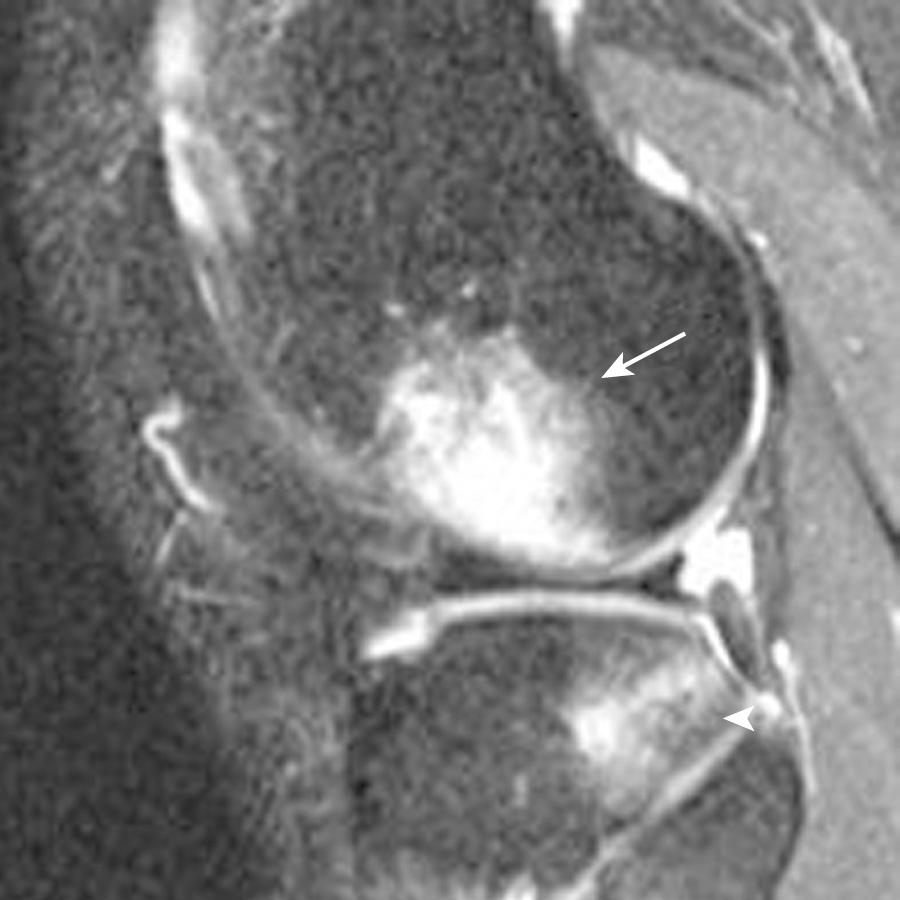
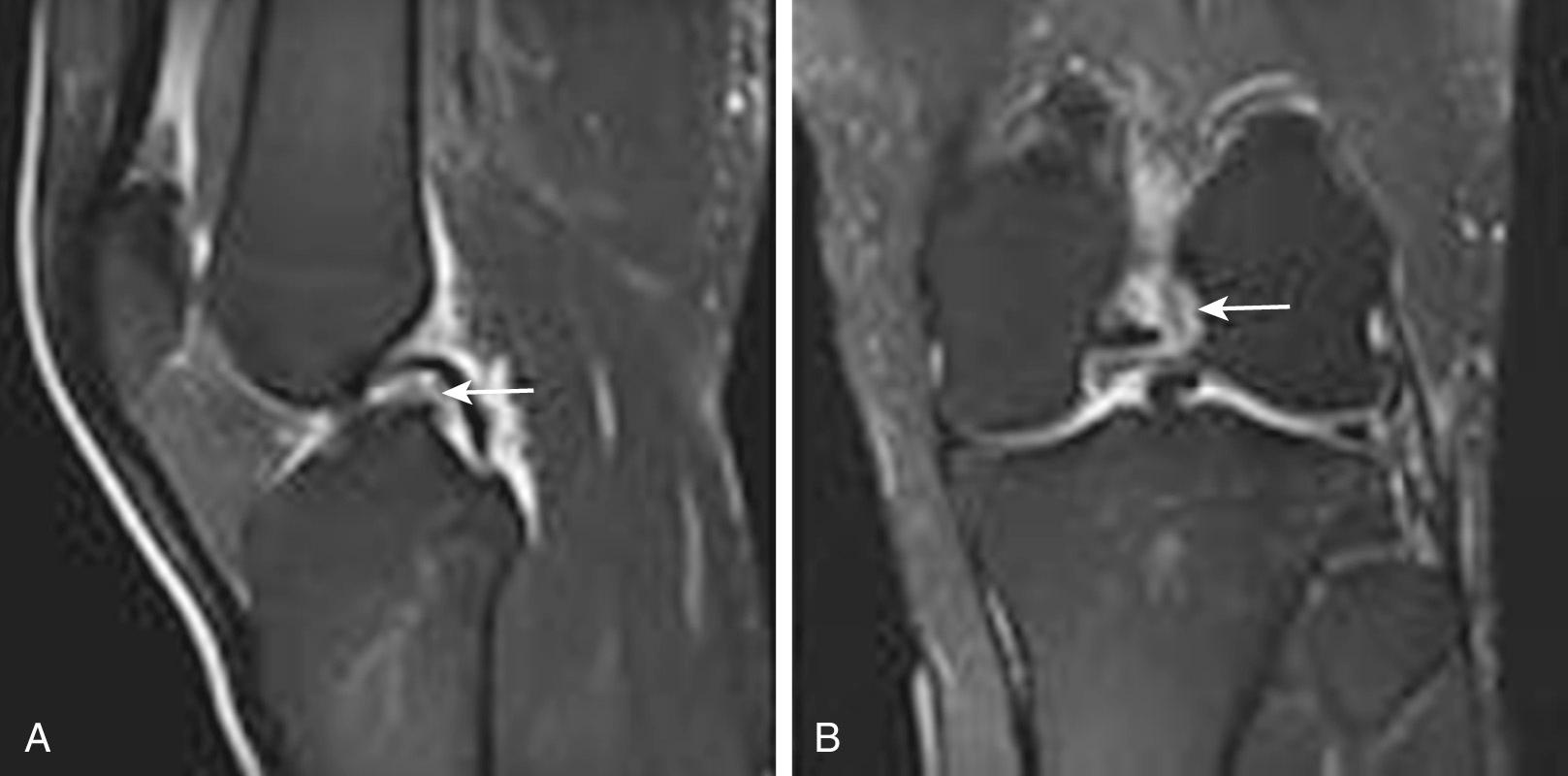
Following a pivot-shift injury, osseous contusions most commonly involve the posterolateral tibial plateau and the lateral femoral condyle ( Fig. 8.1 ). The presence of this contusion pattern indicates acute or chronic ACL disruption because it is failure of this ligament that leads to tibial subluxation and impaction. Other associated pathology includes posterolateral corner injury and subsequent instability. Osseous contusion of the medial tibial plateau has also been described with a pivot-shift mechanism of injury, present in approximately 20% of cases and associated with posteromedial peripheral tears of the medial meniscus.
The dashboard injury is related to a direct blow to the knee, often during an automobile accident. This mechanism manifests as contusions involving the anterior tibia and posterior subchondral patella. Concomitant soft tissue injury with a dashboard contusion pattern often includes PCL and posterior capsule disruption. Hyperextension injury results in impaction of the anterior tibia and anterior femoral condyle and subsequent osseous contusions ( Fig. 8.2 ). Associated ligamentous pathology with this mechanism can include ACL or PCL injury.

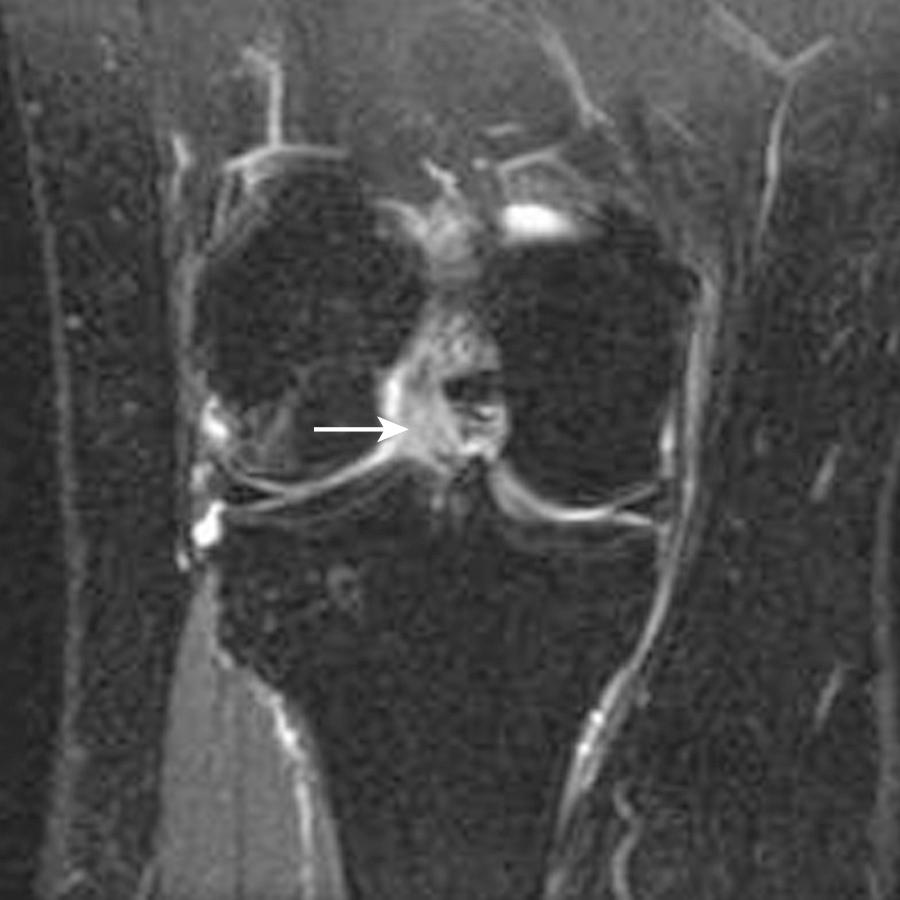
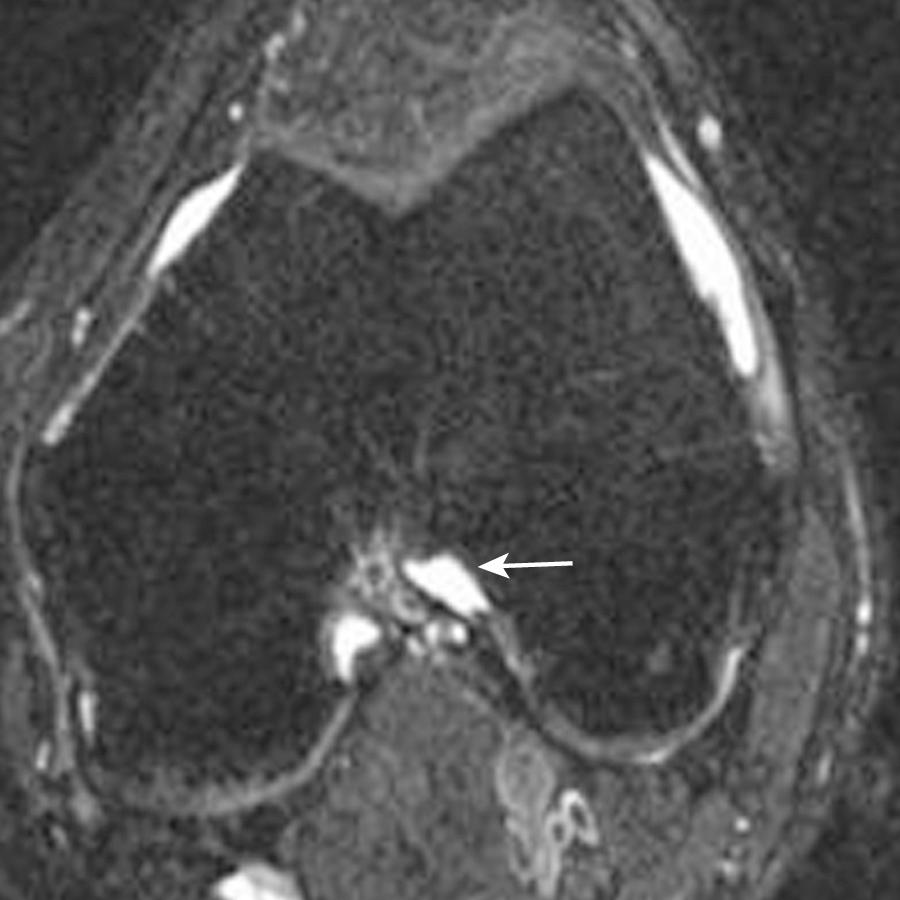
A clip injury is related to valgus stress to the knee and results in a dominant contusion within the lateral femoral condyle from direct impaction, along with a smaller focus of bone marrow edema within the medial femoral condyle related to avulsive force at the origin of the MCL. Injury to the MCL is common with this mechanism, ranging from low-grade sprains to frank disruption. In addition, ACL injury and medial meniscal injury have been described with clip injuries. Osseous contusions following lateral patellar dislocation involve the lateral, nonarticular portion of the lateral femoral condyle, as well as the medial patellar facet ( Fig. 8.3 ). Associated soft tissue injuries include medial patellar retinaculum and medial patellofemoral ligament (MPFL) sprain or disruption. Cartilaginous injury has also been reported with transient lateral patellar dislocations, with delamination of cartilage at the medial patellar facet or at the anterolateral margin of the lateral femoral condyle, sometimes leading to intra-articular cartilaginous bodies.
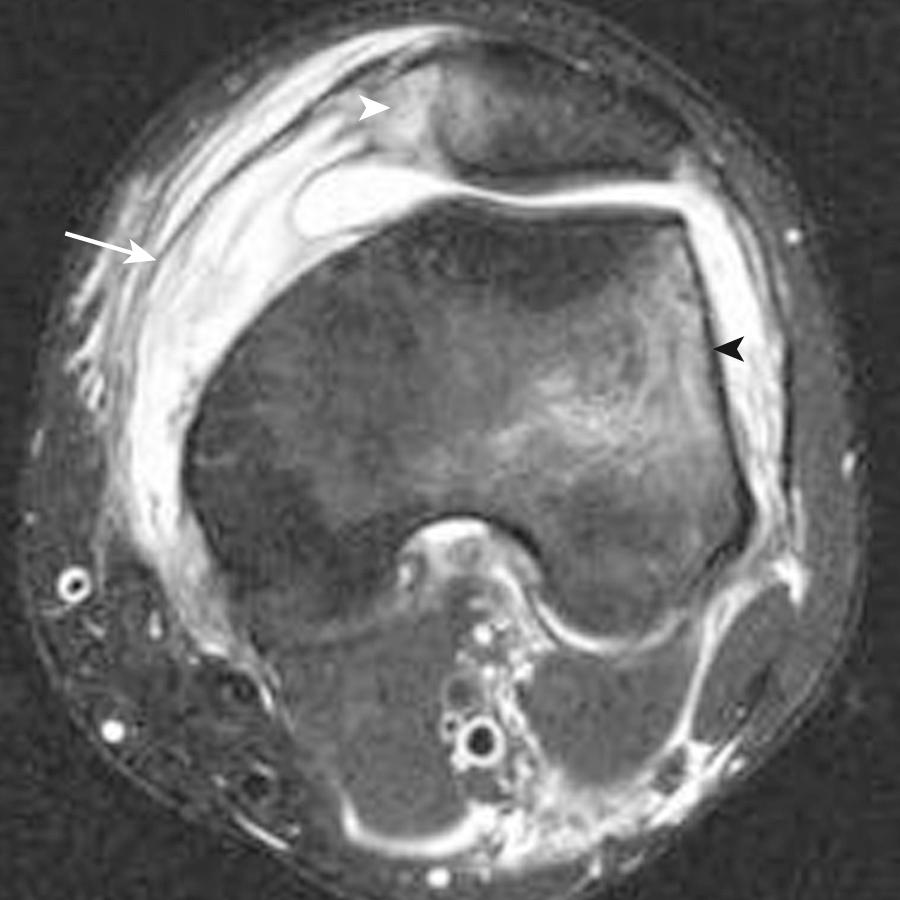
On MRI, the ACL is low in signal relative to muscle on all sequences and parallels the intercondylar roof on sagittal images (Blumensaat line). Proximally the ACL usually displays a homogeneous low signal intensity, whereas distally the ligament demonstrates a striated appearance with fat and synovium interspersed between the AMB and PLB. Familiarization with this appearance is key to avoid misinterpreting the distal ligament appearance for a tear ( Fig. 8.4 ). With the knee in full extension, the ACL should parallel the roof of the intercondylar notch (Blumensaat line). All three planes should be used for the most accurate assessment of the ACL. The sagittal sequence (see Fig. 8.4 ) is most useful and can be performed in an oblique sagittal plane parallel to the orientation of the ACL as prescribed from an axial localizer image with 3- to 4-mm image thickness to decrease volume averaging. The axial and coronal images ( Fig. 8.5 ) are useful in evaluating the ligamentous attachments and confirming abnormalities seen on the sagittal sequence. Axial images are particularly helpful for assessing the integrity of individual ACL bundles in the setting of sprain or partial tear.

The use of radiographs in the assessment of acute ACL injuries is limited to osseous abnormalities. There are several indirect findings that could indicate an underlying ACL injury, such as avulsion fractures of the ACL at the tibial insertion or femoral origin. Avulsion fractures of the intercondylar eminence more commonly occur in children than adult patients and usually come about because of extreme hypertension. There are three types of tibial avulsion fractures: type I describes a minimally distracted fracture; type II encompasses a partially displaced fracture fragment; and a type III is commonly associated with complete separation.
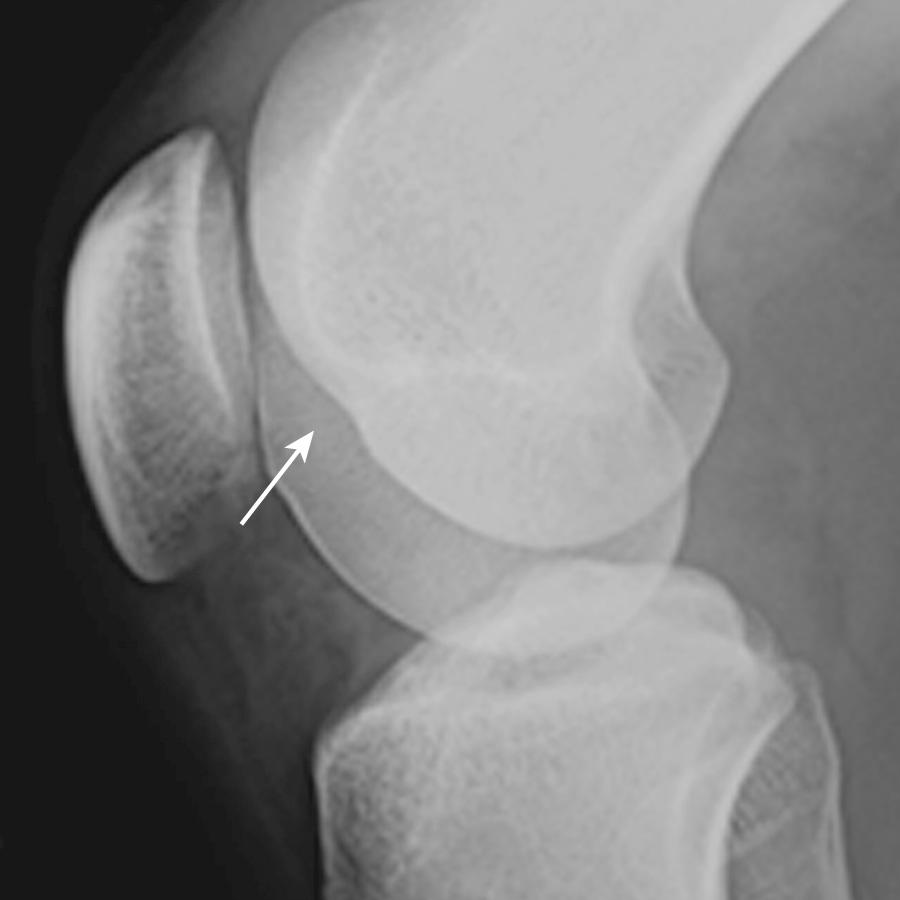
Other radiographic signs that correlate highly with disruption of the ACL include the deep lateral femoral sulcus sign, best seen on lateral radiographs of the knee, which is defined as deepening (more than 2 mm) and cortical irregularity of the lateral femoral sulcus ( Fig. 8.6 ). An avulsion fracture at the lateral aspect of the lateral tibial rim (Segond fracture; Fig. 8.7 ) can be associated in 75% to 100% of the time with ACL injury and occurs in approximately 9% to 12% of all ACL tears. It is characteristically secondary to an avulsion fracture of the iliotibial band (ITB), although the term has also been applied when there is avulsion of the anterior oblique band (AOB) of the LCL. Lastly, other less specific radiographic signs include a large joint effusion following an acute injury and cortical irregularity or fracture of the posterior aspect of the lateral tibial plateau.

The use of computed tomography (CT) in the assessment of ACL injury is limited as well. The gold standard imaging modality currently used in the setting of an ACL injury is MRI because it can diagnose or exclude a tear in patients with equivocal physical examination findings. An area in which CT imaging excels is in allowing more accurate characterization of comminuted fractures and in CT arthrography with sensitivities and specificities of 90% and 96% for the detection of ACL injury, respectively, at initial interpretation. These results are compatible to those previously published with MRI.
The ideal MR sequences for visualization of the ACL are two-dimensional (2D) fast spin echo (FSE) sequences either with or without fat suppression. The standard protocol typically includes a short echo time (TE) sequence (proton density [PD]) in the sagittal and coronal imaging planes. These images are best suited for detecting meniscal pathology. A preferred standard knee protocol comprises the following three sequences: (1) T2-weighted fat-suppressed sequence performed in the axial, sagittal, and coronal imaging plane; (2) FSE sagittal PD-weighted sequence; and (3) spin echo (SE) coronal T1-weighted with fat-suppression sequence. PD- or T2-weighted images with fat saturation are best suited for the evaluation of the articular cartilage. However, gradient echo (GRE) imaging is occasionally also used for this purpose.
MRI plays an important role in the assessment of suspected ACL injury. The majority of ACL tears are complete (approximately 80%) and most commonly occur at the midsubstance or middle third and less frequently occur proximally (near the femoral attachment in 7% of the time) or distally (near the tibial attachment with a frequency of almost 3%). The remainder 20% presents as incomplete tear demonstrating various degrees of involvement.
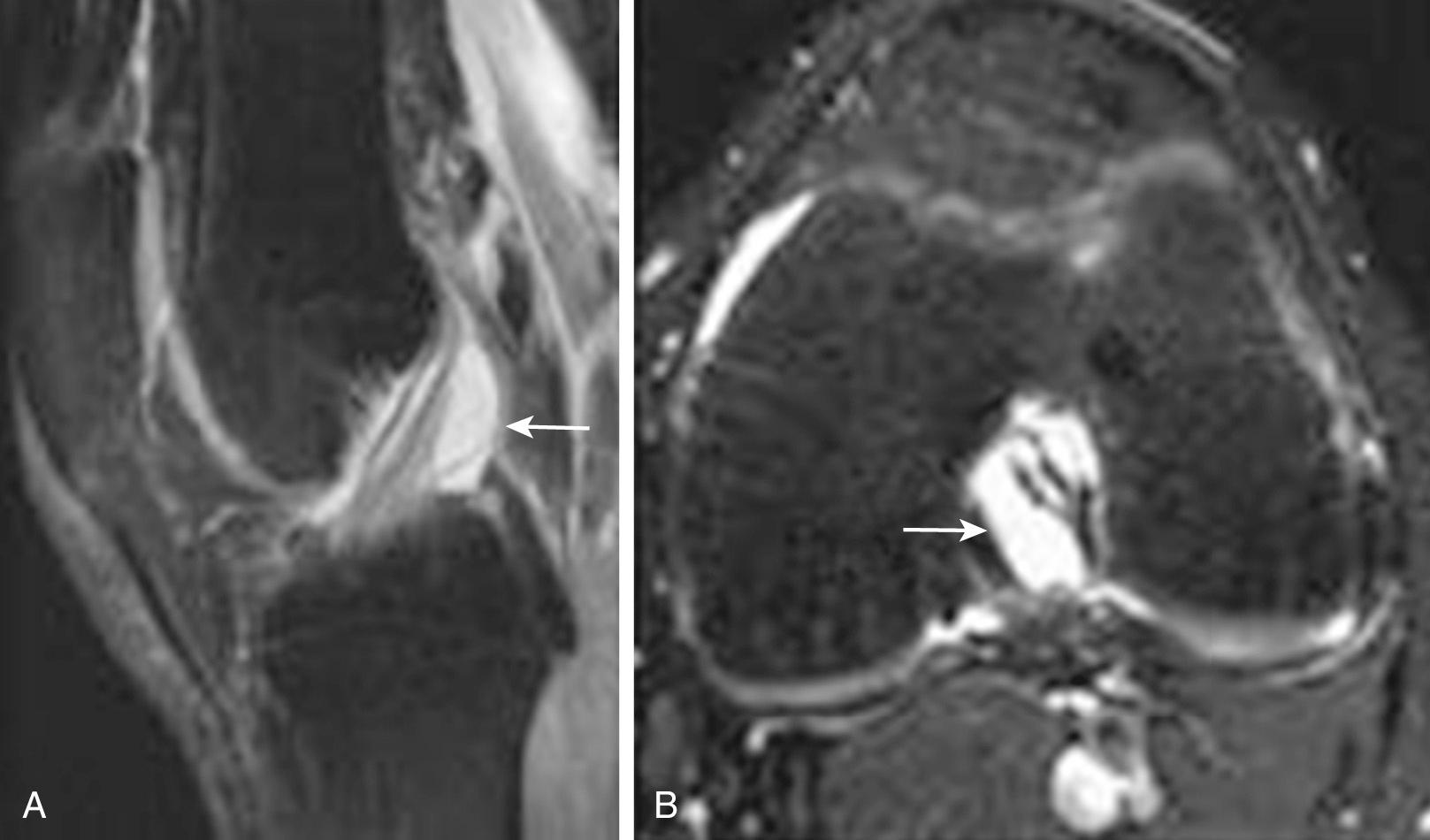
Both primary and secondary signs of ACL rupture have been seen on MRI. Primary signs of rupture include a discontinuous ligament or an abnormal course of the ligament, no longer paralleling Blumensaat line. With a discontinuous ligament, the fibers may appear wavy or horizontal in orientation ( Fig. 8.8A ). Often the ligament is replaced with amorphous increased signal related to edema and hemorrhage when tears are subacute; fibers appear as if they have been cut with scissors in more acute injuries (see Fig. 8.8B ). Secondary signs of ACL tear include buckling of the PCL, anterior translation of the tibia, uncovering of the posterior horn of the lateral meniscus, and characteristic osseous contusion patterns. Buckling of the PCL, uncovering of the posterior horn of the lateral meniscus, and anterior translation of the tibia are all related to anterior subluxation of the tibia relative to the femur secondary to ACL incompetence. Anterior translation of the tibia, referred to as the MRI equivalent of an anterior drawer sign, is assessed using the sagittal imaging plane ( Fig. 8.9 ). The distance between the posterior tibia and the femoral condyle is measured using lines parallel to the long axis of the image. With this method, Vahey et al. demonstrated high specificity (93%) and positive predictive value (95%) of subluxation of 5 mm or more for ACL disruption. A 7-mm or greater subluxation had 100% specificity and positive predictive value. The characteristic osseous contusion pattern for ACL disruption involves the posterolateral tibial plateau and the lateral femoral condyle. Contusion may also be seen at the posteromedial tibial plateau. Complete rupture of the ACL is often accompanied by joint effusion and hemarthrosis. A fluid-fluid level representing layering blood products may be identified in the suprapatellar recess as related to patient positioning during the examination. In skeletally immature patients, ACL injury commonly manifests as an avulsion fracture at its insertion onto the tibia. MRI will demonstrate an intact ligament with an associated displaced osseous fragment at the medial tibial spine or the intercondylar tibial eminence ( Fig. 8.10 ). Subchondral bone marrow edema may be seen within the proximal tibial epiphysis related to the fracture. With this injury, the immature epiphyseal bone is weaker than the mature ligament. Identification of the avulsed tibial fragment on radiography or MRI is essential because treatment options differ considerably from those used with a traditional ACL rupture.


Partial tears of the ACL are more difficult to detect with MRI and are defined as abnormal intrasubstance signal within an otherwise intact ligament or as discontinuity of some of the ligamentous fibers not involving the full width ( Fig. 8.11 ). Commonly, the most proximal portion of the anterolateral bundle of the ACL is disrupted with an intact posteromedial bundle. Although this type of injury can be confidently called a partial ACL tear on MRI, ligamentous integrity is not easily established without a dedicated and properly performed physical examination. MRI is not a sensitive tool for determining the integrity of a partially torn ACL, although secondary signs such as pivot-shift osseous contusions or an MRI anterior drawer can be helpful in suggesting ligamentous incompetence. In general, abnormal T2 hyperintense signal about or within a partially or completely intact ACL with a recent trauma history should be described as a partial tear of the ACL or low-grade ACL injury by MRI. This should be followed by a thorough description of the findings, the presence or lack of pivot-shift contusions, and other findings that might suggest ligament incompetence.
ACL tears are often accompanied by other injuries of the ipsilateral knee. MCL sprain and meniscal tear are the most commonly associated injuries, with a particular prevalence of peripheral vertical tears in the posterior horn of either meniscus. Peripheral meniscus tears just above points of osseous contusion on the posterolateral or posteromedial tibial plateau are also commonly seen. Injuries to the posterolateral corner have also been described in association with ACL disruption. The Segond fracture, an avulsion fracture from the lateral tibia at the lateral capsular ligament insertion, is an indicator of ACL disruption that can be seen on MRI, as well as on plain radiographs ( Fig. 8.12 ).

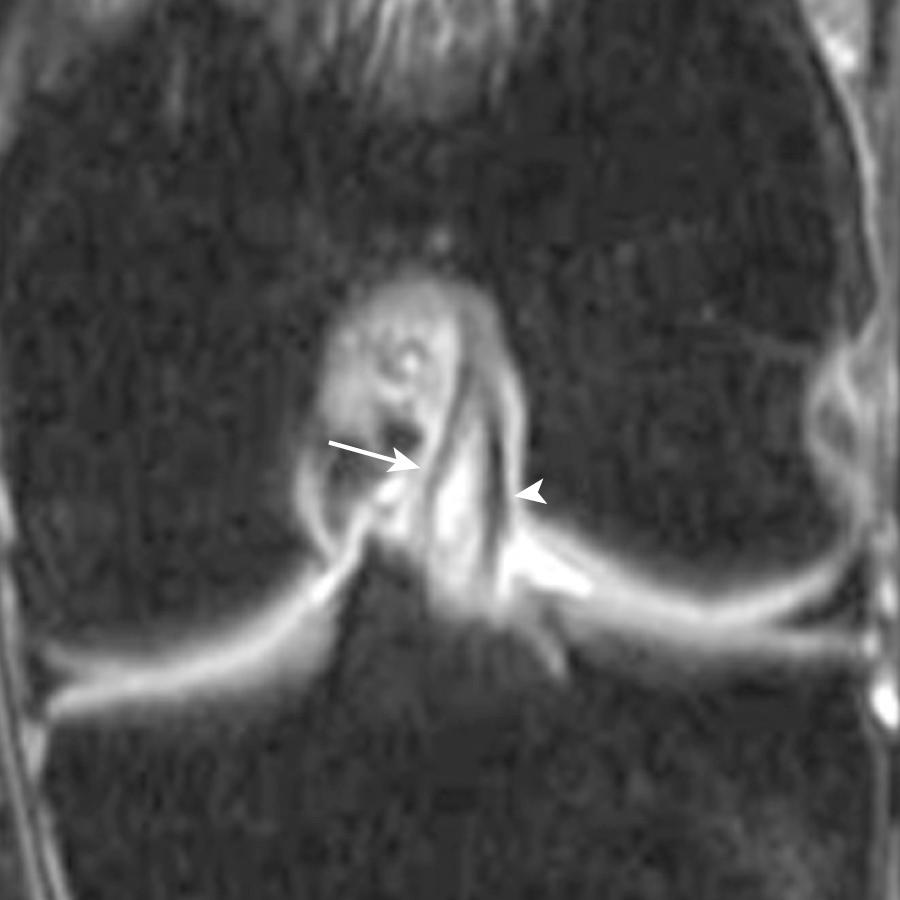
Nonvisualization of the ACL is the most common MRI presentation of a chronic tear. On axial images, fluid in the lateral intercondylar notch, where the normal ACL is found, described as the empty notch sign, can be seen in chronic ACL tears ( Fig. 8.13 ). The ligament may be attenuated or residual fibers may have a horizontal orientation. The chronically torn ACL may scar and adhere to the PCL and clinically may present with an endpoint on anterior drawer examination. Pivot-shift contusions suggest ACL incompetence but not necessarily an acute tear. A patient with a chronic and long-standing ACL tear can acutely pivot shift, leading to new contusions and a hemarthrosis, as well as injury to other ligamentous and cartilaginous structures. Therefore pivot-shift contusions and no visible ACL fibers at MRI should be interpreted as an age-indeterminate ACL tear, with a recent pivot-shift injury. In contrast, mucoid degeneration of the ACL manifests as increased T2 signal, enlargement, and ill definition of an otherwise intact ligament. This pattern of ACL abnormality at MRI should not show a pivot-shift contusion pattern and does not suggest the presence of acute ACL trauma but more likely chronic and repetitive abnormal ACL biomechanics related to meniscal tear or osteoarthritis. Mucoid degeneration of the ACL or PCL can be associated with osseous cystic formation at the cruciate attachments, distal more common than proximal. These intraosseous cruciate cysts are likely a variant of cruciate ganglion cysts, which show homogeneous increased T2 signal similar to that of fluid, insinuating between intact ligament bundles. They are loculated cysts often with lobulation and generally extending along the length of the ligament ( Fig. 8.14 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here