Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Meningiomas are one of the most common primary intracranial brain tumors. They represent 34% of all primary brain tumors and originate from the arachnoid cells in the brain and spine.
The brain convexity is the most frequent site of these lesions (19–34%), followed by the parasagittal region (18–25%), sphenoid wing and middle cranial fossa (17–25%), anterior skull base (10%) and posterior fossa (9–15%).
Convexity meningiomas are those attached solely to the dura that covers the brain convexity.
Parasagittal meningiomas, in their turn, involve the superior sagittal sinus (SSS), with the potential of invasion and obstruction of this venous structure.
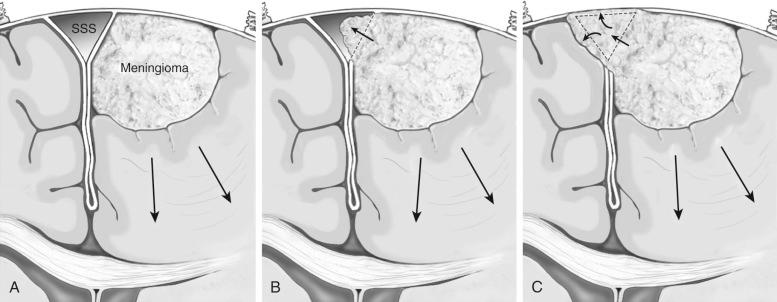
Parasagittal meningiomas are classified according to the relationship with the SSS in anterior, middle or posterior parasagittal meningiomas. These lesions can also be classified according to the degree of SSS invasion into three types, which has important implications for surgical planning. Type I lesions attach to the external layer of the SSS; type II visibly invade the SSS and narrow its lumen, but do not cause complete obstruction of the sinus; and type III are tumors that cause complete obstruction of the SSS ( Figure 10.1 ).
Convexity meningioma can present with a variety of signs and symptoms depending on its location. With the increasing use of MRI and CT scans, a significative proportion of these lesions (10–15%) are discovered incidentally. Incidental convexity meningiomas that are small, asymptomatic and/or without surrounding vasogenic edema may be followed clinically with serial MRI. Surgery is considered when there is significant enlargement of the lesion, development of neurologic signs, or in the presence of new surrounding vasogenic edema. Patients presenting with neurologic deficits related to tumor mass effects are typically candidates for surgical treatment.
The main objective in the surgical treatment of meningiomas is to obtain gross total resection of the lesion and removal of its dural attachment and the surrounding involved bone. Often, in cases of parasagittal meningiomas, gross total resection is not possible because of extensive involvement of the SSS.
The evaluation of convexity meningiomas must include:
Location of the lesion and its relation to the SSS, transverse sinus and other draining veins, including the vein of Trolard and the vein of Labbé.
Bone invasion.
Invasion of adjacent cortex.
Preoperative imaging evaluation is basically composed of:
CT scan, for evaluation of bone hyperostosis and intratumoral calcifications.
MRI with contrast, which will demonstrate the homogeneous contrast enhancement of the lesion, as well as aid in the evaluation of venous system anatomy.
CT angiography, magnetic resonance angiovenography (MRA/MRV) and conventional angiography are useful for preoperative evaluation of arterial feeders, superficial veins and SSS.
Preoperative embolization is not usually necessary because the arterial feeders of convexity meningiomas are usually located at the tumor surface and can be controlled with cautious hemostasis.
The head must be positioned above the heart level and in such a way that tumor location at the convexity of the brain is parallel to the ground. Ideally the tumor must be located at the highest point of the operative field in order to minimize brain retraction.
Supine position with head neutral or slightly flexed is used for frontal convexity meningiomas. Patients with temporal convexity meningiomas are placed in the lateral or supine position with a bolster under the shoulder and head turned about 60° to the contralateral side. In cases of parietal and occipital lesions, park bench, prone and Concorde position can be employed.
For parasagittal meningiomas, the positioning depends on its location of the tumor in relation to the SSS. For anterior lesions, a supine position with gentle head flexion is recommended. In cases located at the middle third of the SSS, semi-sitting and lateral positions are useful; and in cases of posterior lesions it is generally best to use a park bench, prone, or Concorde position with slight flexion and 45° ipsilateral rotation of the head. With this technique, the falx will act as a natural retractor of the contralateral hemisphere and the ipsilateral hemisphere will fall away by gravity, enhancing the exposure of the lesion.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here