Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Constipation is defined symptomatically as the infrequent passage of hard stools, straining while passing a stool, or pain associated with the passage of a hard stool. The range of normal defecation patterns in children is widely variable, though in general, formula-fed infants may have four to five stools per day in the first weeks of life, while breast-fed infants usually pass softer and more frequent stools. Stool frequency in both gradually decreases to one to two per day by 1 year of age. Most children aged 1–4 years have one or two daily bowel movements, with a range of three daily bowel movements to one bowel movement every other day.
Constipation is classified broadly either as functional or as secondary to underlying conditions, such as anatomic abnormalities, metabolic disorders, neurologic dysfunction, or medication effects ( Table 19.1 ). Most childhood constipation is functional. The Rome IV Criteria for Functional Gastrointestinal Disorders defines functional constipation in two age groups as noted in Tables 19.2 and 19.3 .
| Functional |
|
| Anatomic |
|
| Endocrine |
|
| Genetic/Metabolic |
|
| Infectious |
|
| Intrinsic Intestinal Neuronal or Myopathic Disorders |
|
| Neurologic/Spinal Cord Lesions |
|
| Psychologic |
|
| Medications/Toxins |
|
| Other |
|
|
|
Changes in diet, such as formula changes or the addition of solid foods, may lead to transient constipation in infants, with up to 40% of constipation starting during this time period. Minor illnesses, including infectious diarrhea, can subsequently result in episodic constipation as well. More long-standing constipation is often secondary to inadequate intake of dietary fiber, fluid, or both. The evaluation of constipation involves first determining whether the change in the frequency or consistency of stools is secondary to functional constipation or is related to an underlying organic disorder. This determination is based on identifying historical features and examination findings that suggest an underlying disorder and prompt further investigation.
Fecal continence and physiologic defecation are dependent on the anal inhibitory reflex , which is in turn dependent on the proper structure and function of the internal and external anal sphincters and the pelvic floor. The internal anal sphincter is an involuntary muscle that is contracted at rest. When a bolus of stool distends the rectum, the internal anal sphincter relaxes. This process generally results in the child sensing the need to defecate. The external anal sphincter and the puborectalis muscle of the pelvic floor, under voluntary control, contract upon rectal distention, respectively closing the anus and decreasing the rectoanal angle, thus allowing the child to hold stool until it is socially convenient to defecate. Voluntary relaxation of the puborectalis muscle and the external anal sphincter straightens the anorectal angle and allows the child to stool. In situations where there is encopresis secondary to overflow incontinence , the child typically consciously withholds stool by refusing to relax the external anal sphincter in the setting of a relaxed internal anal sphincter. Over time, the child is not able to keep the external anal sphincter fully contracted and stool leaks out of the anal canal. The presence of overflow incontinence is an important indicator that the anal inhibitory reflex is likely intact, as patients with anatomic or neurologic abnormalities of the distal colon and internal anal sphincter, including Hirschsprung disease, are unable to reflexively relax the internal anal sphincter to allow for the passage of stool.
Patients with chronic constipation have abnormal anorectal manometry. The most consistent abnormality is blunted rectal sensation, rendering the patient unable to sense stool in the rectum. Other findings include incomplete relaxation of the internal anal sphincter and paradoxical contraction of the external sphincter during attempted defecation. Patients who have paradoxical anal contraction, also known as functional dyssynergia, are less likely to respond to routine medical therapy or may be more likely to have recurrent constipation if treatment is withdrawn unless the paradoxical contraction is addressed.
Functional constipation may be distinguished from secondary causes of constipation by assessing the age of symptom onset, the stool consistency, and the presence of associated signs or symptoms.
The age at symptom onset differentiates disease processes that are congenital versus those that are acquired. Failure to pass meconium in the first 48 hours of life suggests a diagnosis of Hirschsprung disease , though up to 50% of patients with Hirschsprung disease will pass meconium prior to this. Constipation in the first month of life or a history of constipation since infancy suggests organic causes, including and in addition to Hirschsprung disease ( Table 19.4 ). The onset of symptoms beyond infancy suggests acquired organic constipation or functional constipation.
|
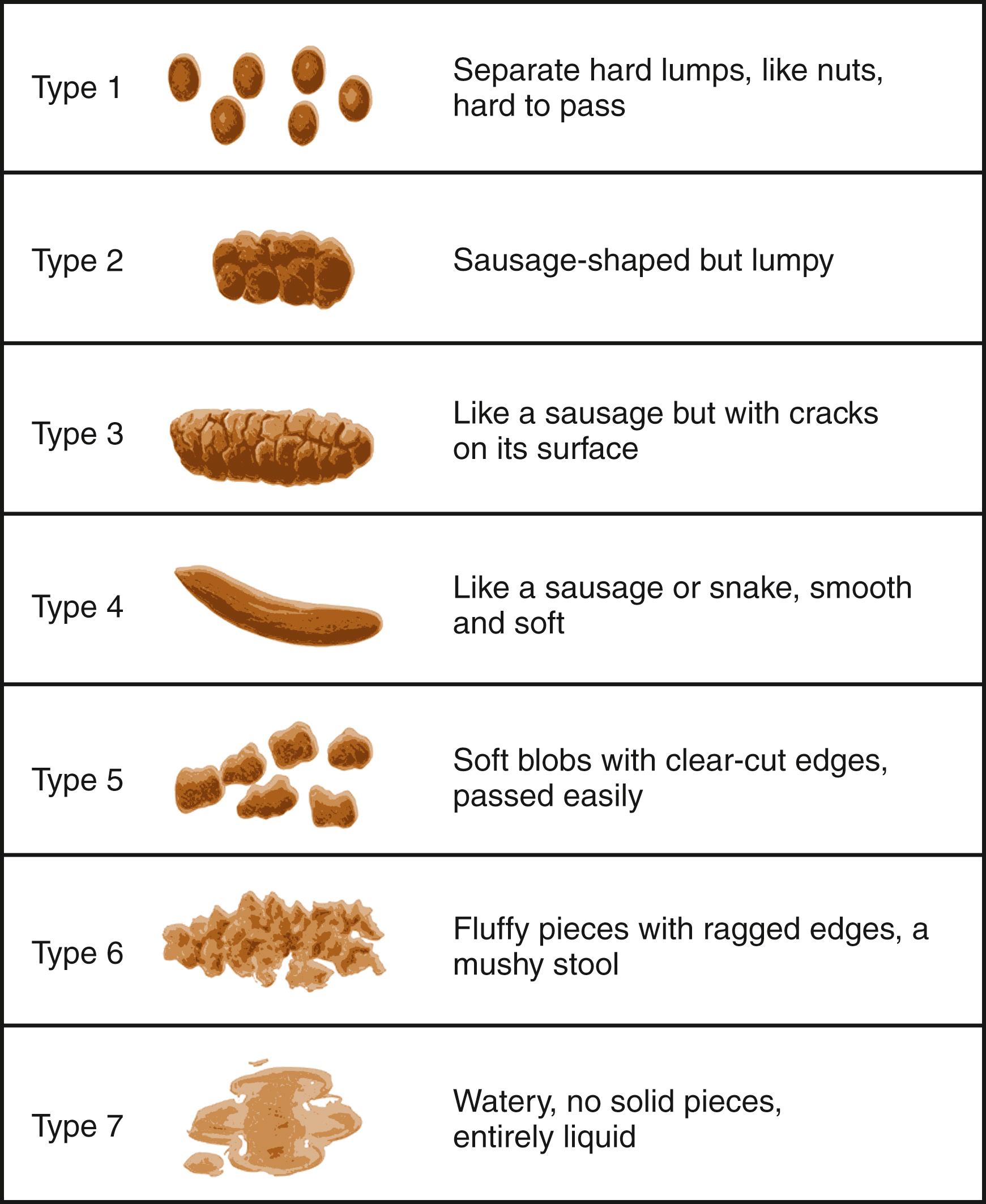
Stool consistency in constipation can differ by etiology. Functional constipation tends to produce painful, large, bulky stools, whereas constipation secondary to Hirschsprung disease or other organic etiologies tends to produce harder, pebble-like, or ribbon-like stools. Stool consistency may be objectively rated via use of the Bristol stool scale ( Fig. 19.1 ) and can be used to follow response to therapy.
The assessment of associated signs and symptoms should include evaluating for a history of blood in the stool, as well as for the presence of urinary symptoms. Bright red blood on the surface of the stool suggests an anal fissure indicative of straining, which is seen in approximately 25% of patients with constipation. Blood mixed in the stool suggests a more remote source, and thus less likely an anal fissure. Urinary symptoms may take the form of either retention or incontinence. Retention may be secondary to congenital or acquired abnormalities in the neurologic regulation of bladder voiding and may be associated with similar abnormalities in the regulation of defecation. Megacystic megaureter intestinal hypoperistalsis syndrome is often detected in utero or after birth with massive bladder distention and failure to pass meconium. In some patients, it is an autosomal dominant disorder due to variants in the ACTG2 gene. Patients with primary chronic intestinal pseudoobstruction may also have bladder distention.
Alternately, retention may be secondary to urinary tract outflow obstruction caused by a large stool burden. Incontinence may be due to a large stool mass distending the rectum and placing pressure on the posterior bladder wall or may indicate overflow incontinence in the setting of a neurogenic bladder.
Abdominal pain is common in constipated patients; when present, it is often mild, nonspecific, and periumbilical. Older children may describe discomfort in the lower abdomen and a history of pain relief after passing stool. Appetite is often diminished. A diary recorded over a period of several days to weeks noting the passage of stools, the timing of meals, and the onset of abdominal pain can aid in the diagnosis of constipation and in monitoring therapy. The personal medical history and the family history may reveal illnesses and conditions associated with constipation ( Table 19.5 ; see Table 19.1 ).
| Symptoms or History | Physical Findings |
|---|---|
Acute Signs
Chronic Signs
|
|
The child’s behavior during defecation should be noted. A history of straining, as an index of difficulty in defecation, can be misinterpreted by parents, who often view a child’s efforts to withhold stool as efforts to pass a bowel movement. Parents often describe a toddler who hides in a corner, with stiffened straight legs, or who may lean into the wall or hold onto a table while “straining.” More often, these actions represent attempts at withholding stool. The young child, having become constipated, passes a painful stool, which, if large, may be associated with an anal fissure. If a fissure is present, a small amount of blood is usually passed with the stool and may create additional worry if noticed by the child. The child associates the passage of stools with pain and tries to prevent further painful episodes by withholding fecal matter. This behavior results in the formation of even larger, harder stools, which are painful to pass, thus establishing a link between pain and defecation that perpetuates the cycle. Children with stool retention may go 3–5 days without defecating. Enuresis and encopresis may occur in this setting. Fecal incontinence is one of the most common presentations of functional constipation and can be misinterpreted by the parent as diarrhea by virtue of constant smearing of stool in the gluteal cleft.
Abnormal growth patterns should alert the physician to the possibility of underlying organic disease, such as hypothyroidism or celiac disease (see Table 19.5 ). Abdominal examination is usually benign; there may be some mild tenderness in the left lower quadrant on palpation of a segment of bowel that is full of stool. Stool may be palpable through the abdominal wall in the sigmoid and descending colon. On occasion, a large, firm fecal mass extends from the symphysis pubis to the umbilicus, which may mimic findings of an abdominal malignancy.
The spine and sacral area should be examined closely. A tuft of hair, a dimple, or a palpable defect or mass in this area should prompt consideration of spina bifida occulta or a tethered spinal cord . Sensory and motor function should be assessed. A normal anal wink , as elicited by gentle stroking of the perianal skin with a sharp object, such as a wooden tongue blade or the corner of a small package of lubricant, gives evidence of intact lumbosacral innervation. A normal cremasteric reflex in males also gives evidence of intact lumbosacral innervation. The cremaster muscle, innervated by the genitofemoral nerve of the lumbar plexus, typically contracts when the observer brushes a finger along the upper surface of the inner thigh, resulting in withdrawal superiorly of the ipsilateral testis.
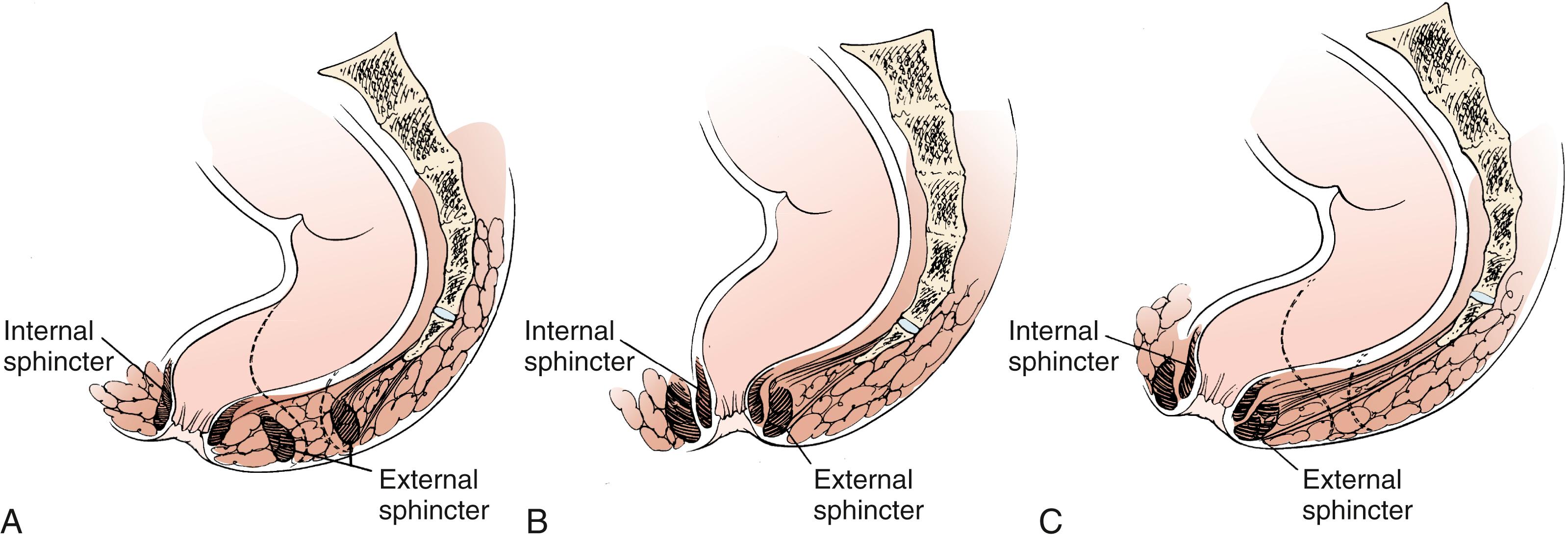
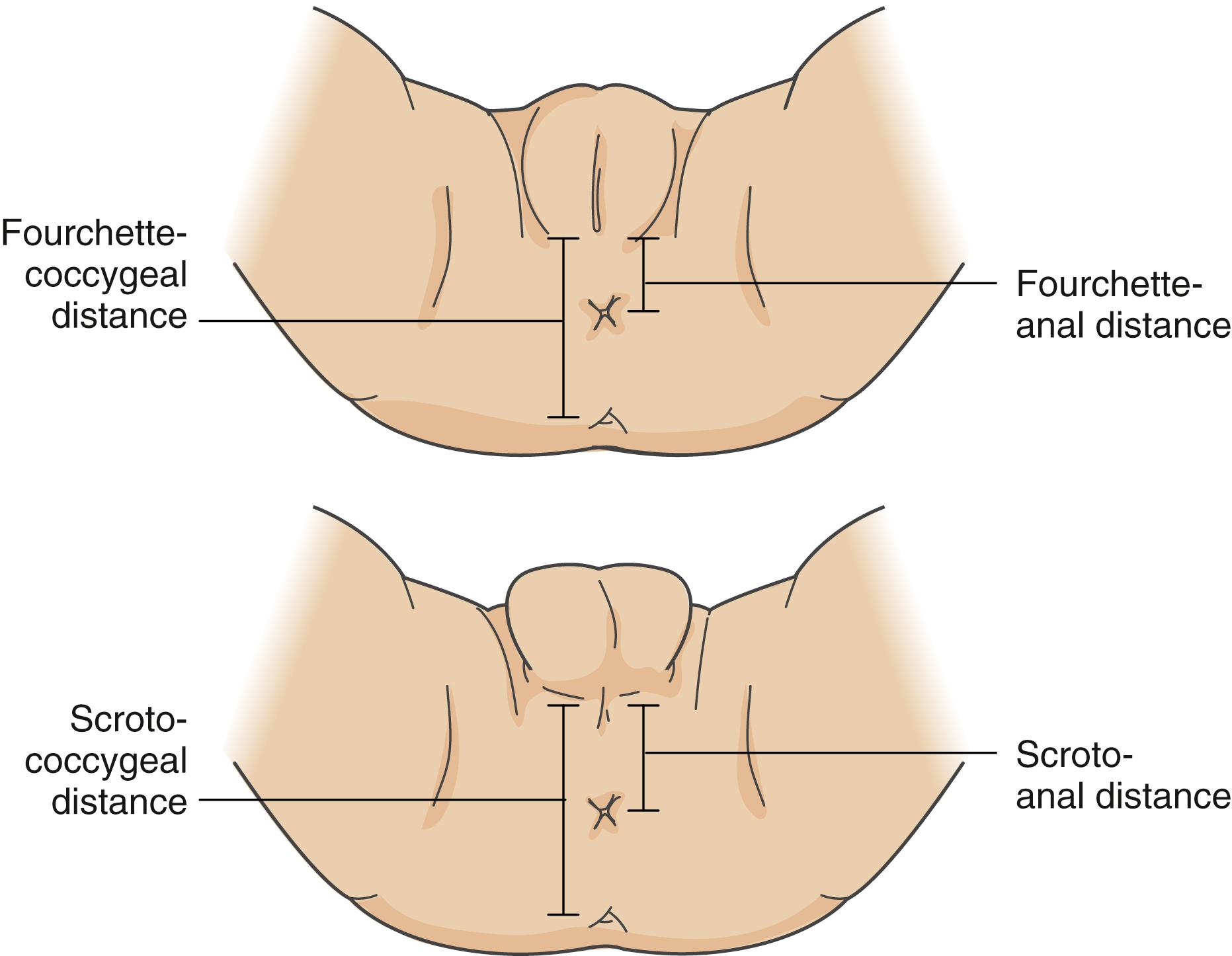
The perianal area should be examined for evidence of fissures suggestive of the passage of large, hard stools. The examination is facilitated if an assistant gently spreads the patient’s buttocks apart while the examiner illuminates the area. Soiling in the undergarments may indicate fecal impaction with overflow incontinence. The location of the anus in relation to the other perineal structures should be determined to assess for anatomic or structural anomalies, such as anterior displacement of the anus ( Fig. 19.2 ). The anus is typically situated in the center of the slightly hyperpigmented skin surrounding the anal sphincter. An anteriorly displaced anus is indicated by an abnormal anal position index (API) , which is defined as the ratio of the distance between the anus and the posterior aspect of the genitals (the fourchette in females and scrotum in males) to the distance between the coccyx and the posterior genitals ( Fig. 19.3 ). Measurements may be obtained using calipers or by placing clear plastic tape adjacent to the landmarks and marking with a pen, and then subsequently measuring the distance on the tape. The normal API for females is 0.45 ± 0.15, and for males it is 0.54 ± 0.14.
Digital examination is indicated in the evaluation of infantile constipation, if the cause or degree of constipation is unclear, or if there are signs of organic disease. The examiner should note the patency and tone of the anus. High tone and an empty rectal vault may suggest Hirschsprung disease. If the aganglionic segment is short enough, withdrawal of the finger might result in an explosive release of stool as the finger acts as a dilator to reach the dilated, ganglion-containing segment. Conversely, a dilated rectal vault with a large stool impaction is more suggestive of functional constipation with withholding behavior. In a cooperative patient, the examiner can ask the patient to bear down against their finger as if attempting to push out stool, which should result in relaxation of the anal canal. Patients who have paradoxical contraction of their anal canal upon this request may have functional dyssynergia , a condition in which the patient’s pelvic floor fails to relax upon attempted defecation.
Routine laboratory evaluation is usually not helpful in the evaluation of constipation, though is indicated if an organic etiology is suspected on the basis of the history or physical examination. Endocrinologic disturbances, such as hypothyroidism, can be associated with constipation. If celiac disease (see Chapter 14 ) is a consideration, serum anti–tissue transglutaminase immunoglobulin A (IgA) antibody levels should be assessed. A total IgA level should be performed concomitantly to exclude IgA deficiency confounding interpretation. If the patient does have IgA deficiency, anti–tissue transglutaminase IgG levels or esophagogastroduodenoscopy with duodenal biopsies can be performed.
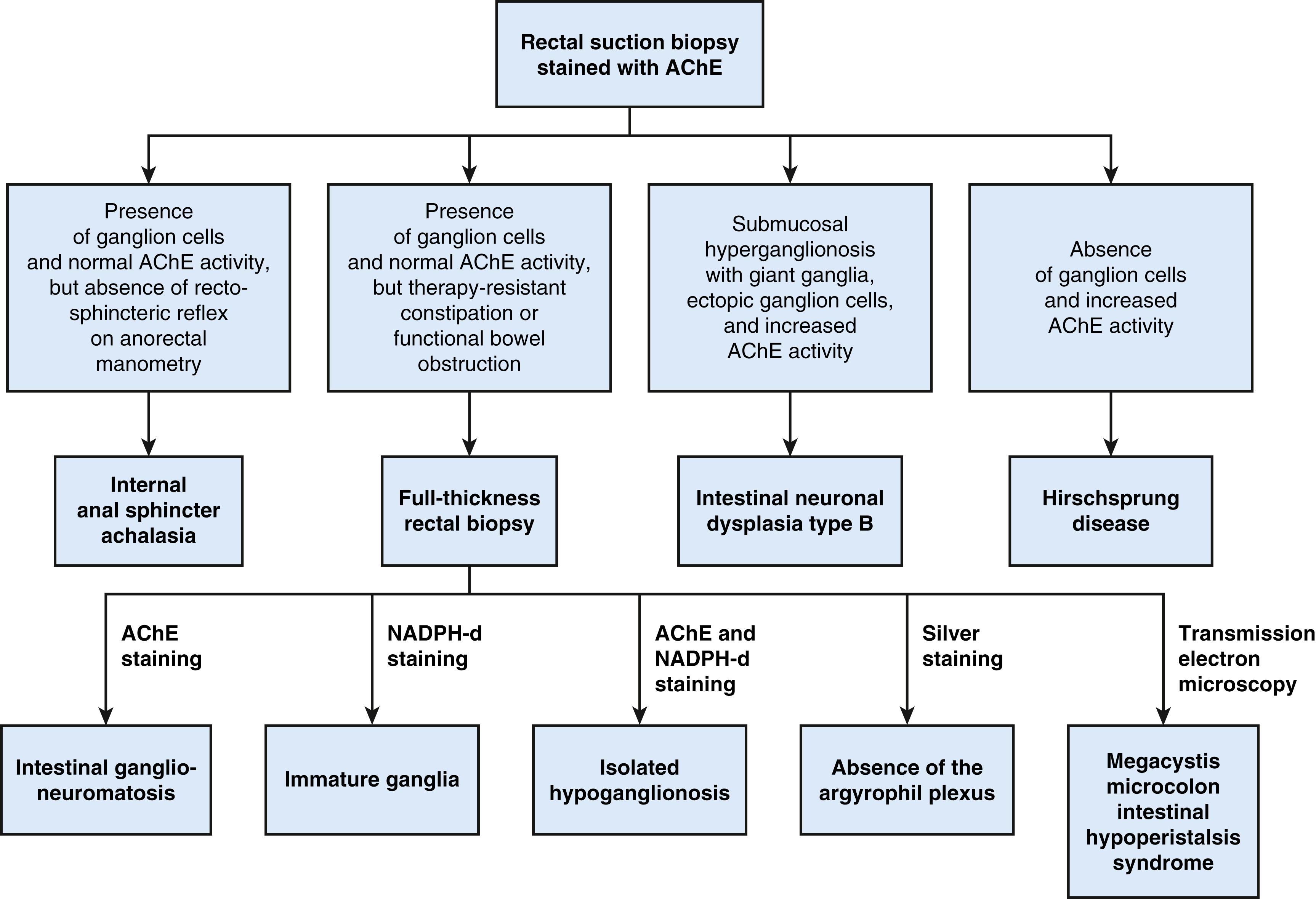
Plain films of the abdomen are rarely necessary, although if obtained may demonstrate stool in the large bowel. While this information is occasionally useful in the case of a child with complaints of diarrhea whose symptoms are due to fecal impaction and overflow of liquid stools, a digital rectal exam similarly can supply the information needed. In addition, there is poor correlation between stool burden on abdominal radiography and symptoms of constipation. However, abdominal radiography may be a useful initial study in the evaluation of suspected obstruction or pseudoobstruction, identifying possible transition zones and/or air-fluid levels. Suspected Hirschsprung disease is evaluated radiographically via a liquid contrast enema in children over 1 month of age in whom a transition zone is expected to have developed; in neonates, rectal suction biopsy is the test of choice ( Fig. 19.4 ). A contrast study in neonates may be useful to detect a meconium plug, microcolon, meconium ileus, or congenital anomalies (ileal atresia, colonic duplication).
Neurologic symptoms, lower extremity or midline defects of the lower back or gluteal cleft, or examination findings suggestive of occult spinal dysraphism or tethered cord should be investigated with MRI of the spine and/or brain. MRI can be used if a disorder involving the lumbosacral spine is abnormal. Children with lower extremity and midline defects involving the lower back or gluteal cleft should have this imaging considered. Concerns for intestinal dysmotility may be evaluated with a colonic transit study , in which the patient swallows either a capsule of radiopaque circular markers once on day 1 or different-shaped markers on 3 consecutive days and undergoes serial abdominal radiographs to determine the distribution of the markers. After 3 days and by some protocols again after 7 days, any markers that have not yet been evacuated in the stool should be located in the rectum. The presence of markers more proximally in the gastrointestinal tract suggests enteric nervous system or neuromuscular pathology (e.g., pediatric intestinal pseudoobstruction).
A rectal motility evaluation may be helpful in the diagnosis and management of chronic constipation. Anorectal manometry can be used to evaluate the integrity of the muscles and the innervation of the defecatory mechanism. Determining the sensory threshold provides valuable diagnostic information: patients who cannot detect a balloon filled with 120 mL of air usually have encopresis. Hirschsprung disease is unlikely if reflexive relaxation of the internal anal sphincter occurs in the presence of rectal distention. Manometry and electromyography document the paradoxical contraction of the external anal sphincter on attempted defecation seen in functional dyssynergia. Anorectal manometry can also be used as a therapeutic modality in biofeedback therapy in patients with constipation and encopresis and in patients with paradoxical external anal sphincter contraction. Total colonic motility is performed by placing a catheter in the colon to monitor pressures from the rectum to the cecum. Motility tracings reveal information about the function of the colon that is useful in diagnosis and treatment, particularly if surgical options need to be explored.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here