Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
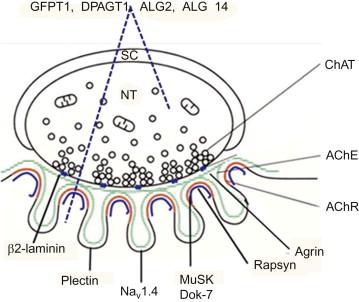
Congenital myasthenic syndromes (CMS) are heterogeneous disorders in which the safety margin of neuromuscular transmission is compromised by one or more specific mechanisms. These syndromes are neither new nor uncommon. They were recognized by Rothbart, who in 1937 described four brothers with myasthenia younger than 2 years of age in one family, and by Sarah Bundey, who in 1972 collected 97 familial cases with onset in early childhood. After the discovery of the autoimmune origins of myasthenia gravis in the 1970s and of the Lambert-Eaton syndrome in the 1980s, it became apparent that myasthenic disorders occurring in a familial or congenital setting must have a different etiology. Since then, clinical, ultrastructural, in vitro microelectrode, and molecular genetic studies of CMS patients have revealed a phenotypically and genetically heterogeneous group of disorders. To date, no fewer than 19 CMS disease genes have been identified. Most disease proteins reside in presynaptic, synaptic basal lamina, or postsynaptic endplate (EP) compartments, but recently it has become apparent that proteins distributed in many tissues, such as those providing cytoskeletal support or subserving glycosylation of nascent peptides, are also CMS targets ( Figure 26.1 ).
A generic diagnosis of a CMS can be made on clinical grounds from a history of fatigable weakness involving ocular, bulbar, and limb muscles since infancy or early childhood, a history of similarly affected relatives, a decremental electromyographic response, and negative tests for antibodies against the acetylcholine receptor (AChR) and the muscle specific receptor tyrosine kinase (MuSK). In some CMS, however, the onset is delayed, the electromyography (EMG) abnormalities are not present in all muscles or are present only intermittently, and the weakness has a restricted distribution. Box 26.1 lists the differential diagnosis of CMS.
Spinal muscular atrophy
Congenital myopathies (central core disease, nemaline myopathy, myotubular myopathy)
Congenital muscular dystrophies
Limb-girdle muscular dystrophy
Infantile myotonic dystrophy
Mitochondrial myopathy
Brain stem anomaly
Möbius syndrome
Infantile botulism
Seropositive and seronegative forms autoimmune myasthenia gravis a
a Not reported in the first year of life.
Limb girdle or facioscapulohumeral dystrophy
Seropositive and seronegative forms of autoimmune myasthenia gravis
Mitochondrial myopathy
Chronic fatigue syndrome
Motor neuron disease
Peripheral neuropathy b
b This diagnosis was made in some slow-channel CMS patients.
Syringomyelia b
Radial nerve palsy b
A direct approach to diagnosis is Sanger sequencing based on available phenotypic clues (see Box 26.2 ). However, many CMS patients lack phenotypic clues. In that case mutation analysis can be based on frequencies of heretofore identified mutations in different proteins as shown in Table 26.1 . In large kinships, linkage analysis followed by Sanger sequencing of genes at the candidate chromosomal locus can be helpful. The use of microarray chips designed to detect variants in currently identified CMS disease genes will likely increase in the near future. Exome sequencing has now become a powerful tool for obtaining a genetic diagnosis when other approaches fail. However, this approach presently captures close to only ~85% of the entire exome and reads a smaller proportion of the exome at a high coverage. It also misses changes in noncoding DNA and large deletions or duplications, is less efficient at detecting dominant than recessive mutations, and is still very expensive. DNA from both parents, and whenever possible from other affected family members, should be analyzed. The bioinformatics analysis of the enormous amount of generated data remains challenging, and the putative pathogenic mutations must be confirmed by Sanger sequencing. The effects of novel nontruncating mutations can be assessed by available software programs, but the accuracy of these tools is not currently validated. Ideally, pathogenicity of novel variants should be evaluated by expression studies. Finally, pathogenic mutations may reside in novel genes whose function is yet unknown. Sequencing the whole genome is also feasible but the interpretation is even more expensive and complicated than that of exome sequencing.
Ptosis, oculoparesis, weakness of limb muscles
Repetitive CMAPs
Refractoriness to cholinesterase inhibitors
Delayed pupillary light reflexes in some cases
Unresponsive to/worsened by cholinergic agonists; improved by ephedrine or albuterol
Repetitive CMAPs
Selectively severe involvement of cervical and wrist and finger extensor muscles in most cases
Dominant inheritance in most cases
Worsened by cholinergic agonists; improved by long-lived AChR channel blockers
Recurrent apneic episodes, spontaneous or with fever, vomiting, or excitement
Variable myasthenic symptoms between acute episodes
Stimulation at 10 Hz for 5 min causes marked decrease of the CMAP amplitude followed by slow recovery over 10 minutes. Rapid recovery in 2 to 3 minutes is not diagnostic
EMG decrement at 2 Hz can be absent at rest but appears after stimulation at 10 Hz for 5 min, then disappears slowly over 10 minutes. Rapid recovery in 2 to 3 minutes is not specific
Multiple congenital joint contractures in one fourth of patients
Increased weakness and respiratory insufficiency precipitated by intercurrent infections
EMG decrement can be mild or absent
Ophthalmoparesis in ~25%; strabismus relatively common
Predominantly limb-girdle and axial distribution of weakness; mild facial weakness, and ptosis are common; normal ocular ductions in most patients
Significant bulbar muscles involvement in some patients
Worsened by cholinesterase inhibitors; responds to ephedrine or albuterol
Can present with stridor and vocal cord paralysis in neonates and infants
Predominantly limb-girdle and axial distribution of weakness.
CK elevation in about one fourth
Tubular aggregates in muscle in most patients; autophagic myopathy in some patients
Improved by cholinergic agonists
Limb-girdle or diffuse weakness; ocular ductions spared
Can be associated with congenital malformations and cognitive deficits
Abnormal isolelectric focusing pattern of serum transferrin in some patients
Tubular aggregates in muscle in most patients; autophagic myopathy in some patients
Improved by cholinesterase agonists
Nephrotic syndrome, ocular abnormalities (Pierson syndrome)
Refractoriness to cholinesterase inhibitors
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here