Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
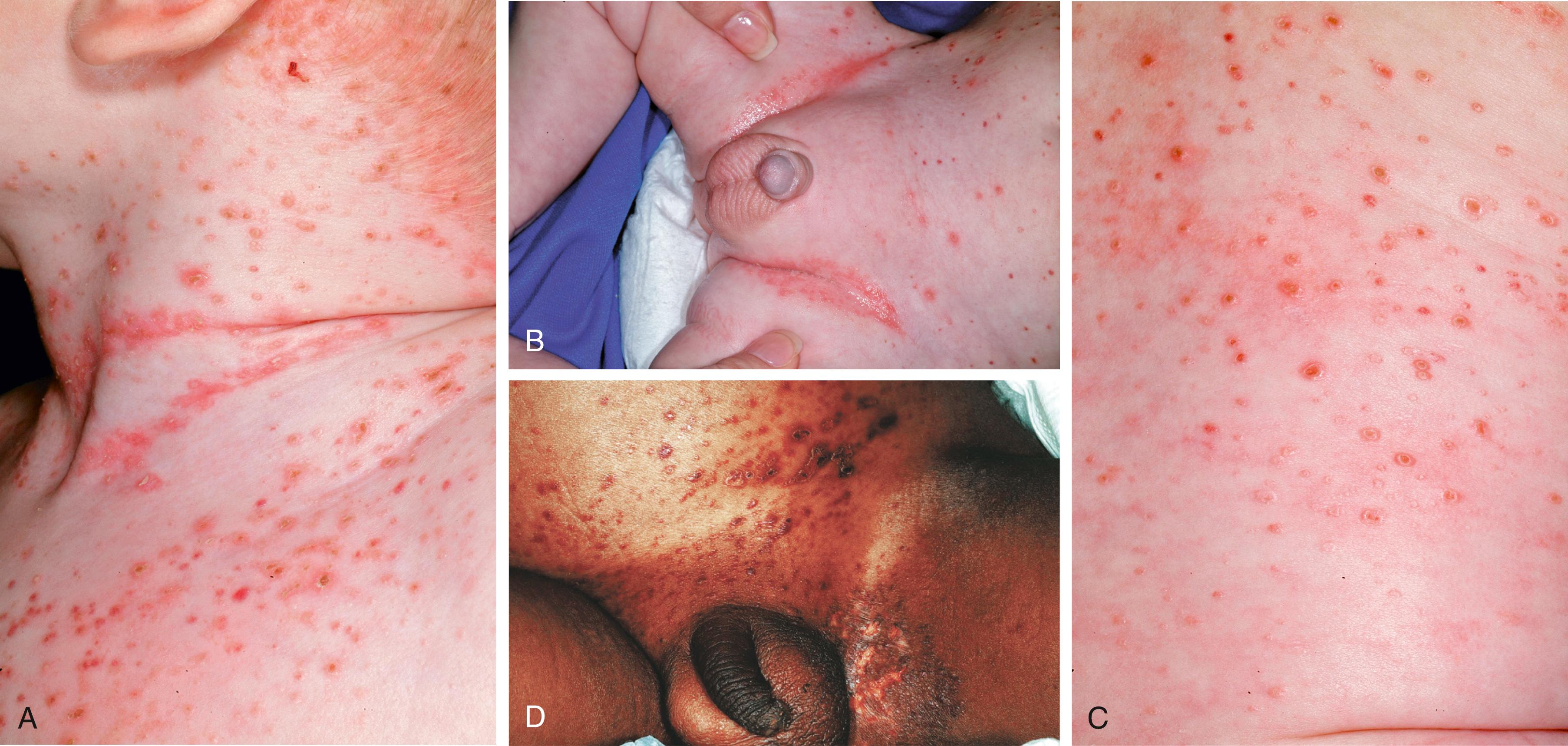
Erythema toxicum is a benign condition that occurs in 30–70% of White full-term infants. Erythema toxicum occurs less frequently in premature infants. The eruption is characterized by blotchy, erythematous macules or patches with central papules, pustules, or vesicles that give the infant a “flea-bitten” appearance ( Fig. 60.1 ). The lesions develop most commonly between the second and fourth days after birth; however, they may appear during the first 2–3 weeks. They are self-limiting and usually resolve within several days. Typical sites of involvement include the face, trunk, and proximal extremities. There may be very few to hundreds of lesions.

A Giemsa or Wright stain of the intralesional contents reveals sheets of eosinophils with a relative absence of neutrophils. Peripheral eosinophilia may be present in up to 20% of affected infants. Erythema toxicum is occasionally confused with transient neonatal pustular melanosis, congenital cutaneous candidiasis, impetigo neonatorum, milia, herpes simplex, or miliaria rubra (prickly heat).
Transient neonatal pustular melanosis , seen in up to 4% of neonates, occurs more often in Black infants. Typically present at birth, the initial lesions are 2- to 5-mm pustules distributed over the face, neck, and upper chest and, less often, on the sacrum, trunk, thighs, palms, and soles ( Fig. 60.2 ). In contrast to the lesions of erythema toxicum, there is no erythema surrounding each pustule, and a Wright stain of pustular contents reveals many neutrophils. In both disorders, the pustules are sterile and should be distinguished from those seen in potentially serious infections caused by herpes simplex virus (HSV), Staphylococcus aureus , or Candida species.

The superficial pustules of transient neonatal pustular melanosis rupture spontaneously within the first few days after birth, leaving hyperpigmented macules that have collarettes of fine scale. It is common to see only the hyperpigmented macules at birth. These brown spots slowly fade over several weeks to months.
Miliaria results from sweat retention and is exacerbated by heat and humidity. Affected newborns are frequently in incubators or receiving phototherapy. Keratinous plugging of the eccrine ducts and subsequent release of eccrine sweat into the surrounding skin produces two distinct clinical manifestations with different sites of eccrine duct obstruction. In miliaria crystallina, obstruction occurs just below the stratum corneum, resulting in superficial, noninflammatory 1- to 2-mm vesicles. In miliaria rubra, or “prickly heat,” obstruction occurs in the mid-epidermis. This is associated with an inflammatory response exhibited by vesicles, papules, or papulovesicles surrounded by a rim of erythema. The lesions occur in clusters on the trunk, face, scalp, and intertriginous regions. Neither type of miliaria warrants therapy, but improvement occurs with cooling of the skin and avoidance of excessive warmth and moisture.
Eosinophilic pustular folliculitis is another disorder of infancy characterized by recurrent crops of vesicles and pustules, beginning in the first year of life. Lesions are often present on the forehead and scalp. The condition tends to occur in a cyclic pattern and is very pruritic. Scraped material from the pustules subjected to Wright stain demonstrates a large number of eosinophils but no evidence of infectious organisms. A CBC may show peripheral eosinophilia. In rare cases, skin biopsy may be necessary. Histopathologic study demonstrates a perifollicular and dermal infiltrate of eosinophils, as well as lymphocytes and histiocytes. Because the clinical condition is very similar to infantile acropustulosis, some authors contend that eosinophilic pustular folliculitis may be part of the same clinical spectrum. This condition is not associated with systemic disease, and the first-line treatment is symptomatic with topical corticosteroids and antihistamines. Oral and topical indomethacin has been effective in recalcitrant cases. Eosinophilic pustular folliculitis usually resolves spontaneously by 2–3 years of age.
Acropustulosis of infancy is a condition that may present at birth or during the first few weeks or months afterward. The disorder is characterized by recurrent eruptions of pruritic pustules or vesicles involving the hands and feet ( Fig. 60.3 ). On occasion, involvement includes other sites such as the trunk or abdomen. The lesions frequently begin in crops, which typically last approximately 1 week, and resolve with desquamation, followed by postinflammatory hyperpigmentation.

Acropustulosis is often confused with infantile scabies . Family history and examination of scrapings of the involved area may help differentiate between these two diagnoses. However, there is some thought that it may occur after a previous scabies infection. Scrapings of lesions in acropustulosis often demonstrate neutrophils. Bacterial infection should also be ruled out by wound cultures. Treatment is symptomatic and consists of control of pruritus with low- to mid-potency topical corticosteroids and antihistamines. Parents should be advised that lesions tend to occur episodically until approximately 2–3 years of age.
Neonatal cephalic pustulosis (neonatal acne) develops in approximately 20% of newborns. Typically, it is not present at birth but appears during the first few weeks after birth. Characterized by papules and pustules located on the face or trunk, this condition usually resolves within the first several months of life ( Fig. 60.4 ). Neonatal acne is a misnomer as neonatal cephalic pustulosis is likely caused by Malassezia yeast species. Therapeutic intervention is rarely required, but ketoconazole 2% cream may be of some use.

Langerhans cell histiocytosis (LCH) is a rare disorder, affecting about 5 per 1 million children, which is characterized by a proliferation of clonal dendritic cells, called Langerhans cells. There are four main types, two of which are most frequently seen in neonates and infants, though there is substantial overlap among the types.
Congenital self-healing reticulohistiocytosis ( Hashimoto-Pritzker disease ) typically presents at birth or within the first few days of life and is limited to the skin. There is a diffuse eruption of red to purple-brown papules and nodules that will crust and remit after several weeks. While it is considered a benign, self-limited condition, it can rarely progress to other, more aggressive forms of LCH.
Letterer-Siwe disease is the more acute, diffuse form of LCH that has multisystem involvement. It commonly presents before 1 year of age with the majority of patients having skin findings of small 1- to 2-mm papules, pustules, and vesicles, typically on the scalp, intertriginous areas, and trunk ( Fig. 60.5 ). The lesions are often crusted and may have secondary bacterial infections. Fissures and confluence of papules can be seen. It can be confused with seborrheic dermatitis and other forms of diaper dermatitis ( Table 60.2 ).
Patches are confluent, flat lesions over 1 cm in size, while plaques are slightly raised lesions over 1 cm in size. Many of these conditions have overlapping features but can often be distinguished by their location, distribution, and response to certain treatments (see Table 60.1 ).
| Rashes | |
| Papules and Pustules | |
| Erythema toxicum | Occurs first few days of life Blotchy red macules with central papule, pustule, or vesicle |
| Transient neonatal pustular melanosis | Present at birth More common in African-American infants Pustules resolve with hyperpigmented macules |
| Miliaria | Associated with overheating Vesicles and pustules in occluded areas |
| Eosinophilic pustular folliculitis | Onset during infancy Pruritic pustules on the head and neck |
| Acropustulosis of infancy | Onset during infancy Pruritic pustules on the hands and feet |
| Neonatal cephalic pustulosis (neonatal acne) | Pink papules, predominately on face |
| Langerhans cell histiocytosis | Crusted papules, predominately on the scalp and intertriginous areas |
| Herpes simplex virus | Onset from birth to 2 wk Grouped vesicles and papulopustules favor scalp and trunk |
| Varicella | Diffuse vesicles and papules Associated with sepsis, fever/hypothermia |
| Scabies | Pruritic papules, vesicles, and pustules Can be widespread in infants, but concentrated in intertriginous areas |
| Syphilis | Widely scattered scaly red-brown papules and plaques |
| Patches and Plaques | |
| Neonatal lupus | Bright red annular patches and plaques distributed on cheeks and periorbital skin Heart block is most common extracutaneous finding |
| Seborrheic dermatitis | Pink patches on the scalp, face, ears, and intertriginous areas May have yellow, greasy scale Erosions and fissures can be seen |
| Diaper dermatitis | Pink patches with erosions in the groin and buttocks Can be multifactorial |
| Fixed Lesions | |
| M acules, Papules, and Pustules | |
| Milia | Pinpoint white-yellow papules without erythema Typically on face, gingiva, or palate Resolves with time |
| Sebaceous gland hyperplasia | Skin-colored to yellow tiny papules on cheeks and nose Secondary to maternal androgens Resolve in first few months |
| Subcutaneous fat necrosis | Firm, indurated, tender plaques on back, arms, shoulders of newborns Due to perinatal trauma, hypothermia, or hypoxemia Monitor for hypercalcemia |
| Macules, Papules, and Pustules—cont’d | |
| Juvenile xanthogranuloma | Solitary yellow-pink plaques on the face and scalp May ulcerate and usually resolve spontaneously |
| Mastocytoma | Yellow to pink solitary plaques Can urticate or swell with friction or rubbing Composed of mast cells Can be seen in infants but typically more common with toddlers |
| Urticaria pigmentosa | Condition with several mastocytomas Rare in infants Typically presents with lesions that will urticate Over time, they become hyperpigmented Rarely associated with systemic symptoms |
| Spider angioma | Rare in infants Small blanching capillaries with “feeder vessel” on the trunk and face |
| Pyogenic granuloma | Solitary, small vascular papules that develop rapidly and bleed profusely Typically seen in toddlers and occasionally infants |
| Patches and Plaques | |
| Pink (Vascular or Other) | |
| Hemangioma | Benign vascular tumors, typically present in first month of life Grow rapidly for first several months and then involute slowly over a couple of years |
| PHACE/PELVIS | Syndromes associated with hemangiomas in particular locations on the face or back |
| Capillary malformation | Stable, pink, vascular patches; typically unilateral In V1 distribution, can be associated with Sturge-Weber syndrome |
| Nevus simplex | Pink patches on glabella, eyelids, nape of neck, typically Usually fade over first couple of years |
| Cutis marmorata telangiectasia congenita | Lacy, reticulated vascular patches Do not resolve with rewarming of infant May have atrophic changes or ulcerate |
| Kaposiform hemangioendothelioma | Rare vascular tumor Firm, violaceous, and tends to proliferate Can lead to consumptive coagulopathy (Kasabach-Merritt syndrome) |
| Venous/lymphatic malformation | Slow-flow vascular malformations Typically present at birth May be associated with atrophy or overgrowth |
| Hyperpigmented or Darker Pigment | |
| Congenital melanocytic nevus | Pigmented macules, papules, patches, and plaques Present in 2–3% of population |
| Neurocutaneous melanosis | Defined by a giant melanocytic nevus or greater than two CMNs Associated with melanocytic infiltration of leptomeninges Clinically symptomatic lesions have worse prognosis |
| Café-au-lait macules | Well-demarcated tan macules or patches Seen in 10–20% of population Multiple lesions can be associated with neurofibromatosis |
| Dermal melanocytosis | Large, poorly demarcated, slate-gray to blue patches on buttocks and lumbosacral region Occurs normally in darker skin tones Typically fades over time |
| Hypopigmented or Depigmented | |
| Nevus depigmentosus | Hypopigmented patch that persists through life |
| Ash leaf spots | Hypopigmented macules that present in first few months to years of life Typically seen with tuberous sclerosis |
| Piebaldism | Well-circumscribed areas of depigmentation on the skin Tends to be symmetric and stable in size |
| Waardenburg syndrome | White forelock, white patches on skin Can have heterochromia of irides and hearing loss |
| Albinism | Diffuse congenital hypopigmentation of skin Usually involves eyes and hair Should be monitored closely by ophthalmologists Evaluate for hearing loss Patients need lifelong photoprotection |
| Other | |
| Nevus sebaceus | Sebaceous gland hamartoma, usually present at birth Yellow-orange and smooth plaque Thickens during puberty |
| Dermoid cyst | Typically found in head/neck region Potential for intracranial connection |
| Aplasia cutis | Congenital absence of skin, typically on scalp Can resemble scars when child is older |
| Hair collar sign | Ring of dense, darker hair encircling a scalp lesion Can be a sign of spinal dysraphism |
| Hypertrichosis of lumbar area | Normal variant in certain ethnicities Can be indicator of spinal dysraphism |
| Sacral dimples | Commonly seen Large dimples along gluteal crease need to be evaluated for spinal dysraphism Can be associated with hypertrichosis |
| Transient/Changing Lesions | |
| Patches | |
| Segmental | |
| Cutis marmorata | Lacy, reticulated vascular patches, often bilateral Resolve with warming of infant and disappear over time |
| Diffuse | |
| Harlequin color change | Marked erythema on dependent side Simultaneous blanching on nondependent side Transient |
| Distal Extremities | |
| Acrocyanosis | Bluish-purple discoloration of hands, feet, and lips Occurs with crying and cold stress |
Neonatal lupus erythematosus is a unique annular erythematous eruption during the neonatal period. It affects 1 in 12,000–20,000 live births. Congenital cases are even more uncommon. Lesions of neonatal lupus are often scaly, annular plaques that usually occur on the face and scalp and may affect the periorbital and malar areas, creating a “raccoon eyes” appearance ( Fig. 60.6 ). Other manifestations may include transient hypopigmentation with epidermal atrophy or telangiectasia. Cutaneous lesions may be present at birth but often appear within the first 2–4 months of life. The lesions are usually exacerbated by sun exposure and are typically photodistributed. The majority of skin findings are transient, lasting up to 6–9 months.

Cutaneous findings and congenital heart block are each present individually in approximately 50% of affected infants; some studies have shown congenital heart block to be much less common. An overlap of both is present in approximately 10% of affected infants. The major morbidity and mortality of neonatal lupus result from congenital heart block.
The diagnosis of neonatal lupus includes examination of anti-Ro, anti-La, and anti-U1RNP autoantibodies in both the infant and mother. Ninety-five percent of mothers of infants with neonatal lupus have anti-Ro antibodies. Skin biopsy is usually not necessary. Work-up should include an ECG, platelet count, and liver function tests because approximately 35% of affected infants have liver disease or thrombocytopenia. Rare reports of multisystem involvement, including neurologic and respiratory findings, have been reported.
Mothers with high titers of anti-Ro antibodies or with systemic lupus erythematosus have a higher risk of delivering an infant with neonatal lupus and should be counseled appropriately. Mothers with positive anti-Ro or anti-La antibodies will have an approximately 2% risk of their baby having neonatal lupus. Despite high antibody titers, fewer than half of mothers of affected infants are symptomatic at the time of delivery. In most of these mothers, evidence of connective tissue disease, usually Sjögren syndrome or subacute cutaneous lupus, develops over time.
Differential diagnosis should include annular erythema of infancy, tinea corporis, and cutis marmorata telangiectatica congenita (CMTC). Treatment consists of photoprotection and topical steroids. Most cutaneous changes resolve spontaneously by 6–9 months of age as a result of a gradual decrease in maternal antibodies.
Seborrheic dermatitis , common during infancy, typically manifests within the first several weeks after birth. Characterized by erythema and a yellow, greasy scale, it usually resolves spontaneously within several months. The eruption occurs at sites where sebaceous glands are concentrated, such as the face, chest, posterior auricular scalp, and intertriginous areas ( Fig. 60.7 ). Malassezia colonization plays a part in the development of seborrheic dermatitis. “Cradle cap” is seborrhea that is confined to the scalp. Involvement of the diaper area is characterized by salmon-colored patches that arise in skinfolds and spread to the genitalia, suprapubic area, and upper medial thighs. Scale may not be as apparent in intertriginous areas. Unlike atopic dermatitis, this eruption is not very pruritic. Secondary candidal or bacterial infection is common, particularly if erosions or fissures are seen.
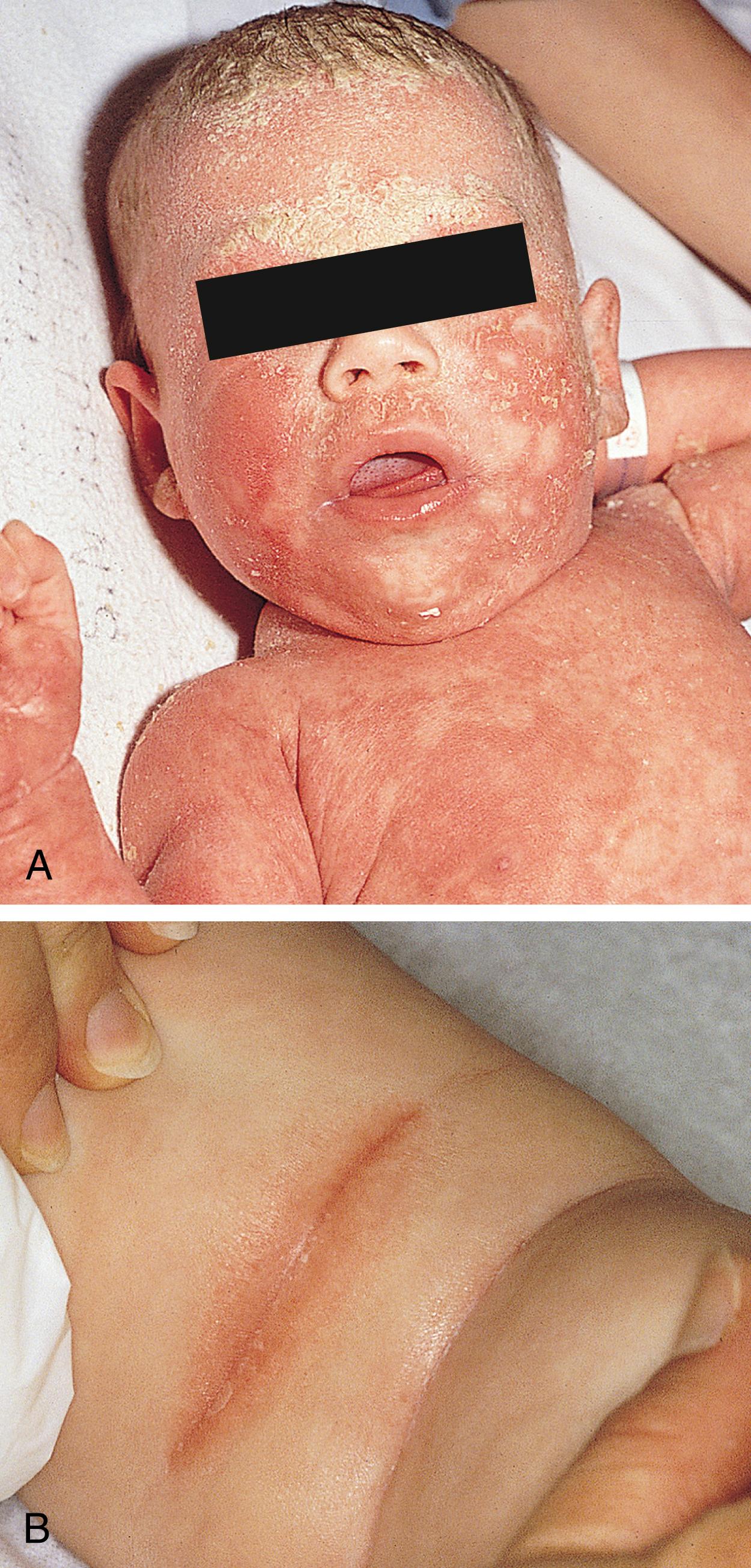
The diagnosis is established clinically. The presence of greasy yellow scales and salmon-colored patches, involvement of the scalp and intertriginous areas, early onset, and lack of pruritus or atopic history help distinguish seborrheic from atopic dermatitis. However, some infants have an overlap of seborrheic dermatitis and atopic dermatitis. Seborrheic dermatitis should also be differentiated from LCH, in which the lesions are typically purpuric, erosive, or crusted, and from psoriasis (see Chapter 61 ). Skin biopsy findings, as well as hepatosplenomegaly, purpura, lymphadenopathy, anemia, thrombocytopenia, external otitis, interstitial pneumonia, and osseous lesions, further distinguish LCH from seborrheic dermatitis.
Treatment of the scalp consists of mild keratolytic shampoos, such as those containing selenium sulfide or zinc pyrithione. Ketoconazole 2% shampoo can be efficacious, particularly with controlling overgrowth of the yeast. Mineral oil may be helpful in removing thick, adherent scales. The scalp and diaper dermatitis may be treated with low-potency topical corticosteroids and barrier ointments. Topical antifungal or antibacterial agents should be used for coexisting candidiasis or impetigo.
Diaper dermatitis is one of the most common dermatologic disorders of infants and toddlers (see Table 60.2 ). It comprises a group of inflammatory conditions that involve the lower abdomen, genitalia, upper thighs, and buttocks. Clinical manifestations include erythema, edema, erosions, vesicles, and pustules. Secondary changes of postinflammatory hyperpigmentation or hypopigmentation are common.
| Disease | Clinical Manifestation | Other Features | Treatment |
|---|---|---|---|
| Friction | Inner surface of thighs, genitalia, buttocks, abdomen | Course waxes and wanes Aggravated by talc |
Responds well to diaper changes Avoidance of diapers |
| Irritant | Mild erythema with shiny surface and occasional papules Confined to convex surfaces Spares intertriginous areas |
Exacerbated by heat, moisture, and sweat retention | Gentle cleansing Regular diaper changes Barrier creams (zinc oxide, Vaseline) Low-potency topical steroids can help |
| Allergic contact | Typically confined to convex surfaces Skin involved is in direct contact with offending agent Mild cases: diffuse erythema, papules, vesicles, scaling Severe cases: papules, plaques, psoriasiform lesions, ulcerations, infiltrative nodules |
Often related to topical antibiotics (neomycin, bacitracin) Certain emulsifiers in topical products Preservatives in wet wipes can be an offender |
Remove offending agent Judicious use of low-potency topical steroids Barrier creams/ointments |
| Seborrheic dermatitis | Salmon-colored patches Often have yellow, greasy scale Fissures, erosions, maceration, and weeping can be seen |
Axillae, ear creases, and neck are often involved “Cradle cap” on scalp Hypopigmentation often seen in patients with darker skin tones |
Low-potency topical steroids If coexistent infection—antifungal or antibacterial agents |
| Candidiasis | Usually involves intertriginous areas and convex surfaces Bright-red papules and plaques Satellite lesions on abdomen and thighs |
Oral thrush may be present Often occurs after treatment with systemic antibiotics or local topical steroid use |
Topical anticandidal agent, including nystatin |
| Intertrigo | Well-demarcated, macerated plaques with weeping Gluteal cleft and fleshy folds of thighs |
May be associated with miliaria | Avoiding excessive heat Cool clothing |
| Psoriasis | Bright red, scaly, well-demarcated plaques Can persist for months Less responsive to topical treatment |
Red, sometimes scaly Can be present on extremities or trunk Nail changes seen Family history |
Low-potency topical steroids Moisturizers |
| Staphylococcal infection | Many thin-walled pustules with pink-red base Collarette of scale after rupturing |
Antistaphylococcal therapy | |
| Acrodermatitis enteropathica (zinc deficiency) | Early lesions are vesicular and pustular Become confluent, pink, dry, scaly, crusty plaques |
Perioral skin typically also involved Irritability or listlessness Failure to thrive, alopecia, diarrhea |
Secondary to zinc deficiency or inborn error of zinc transporter Treat with zinc replacement |
| Langerhans cell histiocytosis | May mimic candidiasis or seborrheic dermatitis Persistent, does not improve with standard treatments Clusters of infiltrative, crusted, hemorrhagic papules Ulceration can be seen |
Involvement of groin, axillae, periauricular skin, hairline, and scalp Anemia, thrombocytopenia, hepatosplenomegaly, and osseous lesions |
Chemotherapy |
Diaper dermatitis is often multifactorial, including irritation from feces/urine, skin breakdown from maceration, and bacterial or fungal components. Although urinary ammonia was thought to be the primary factor in the development of diaper dermatitis, feces now appear to play a more important role. Fecal ureases, by converting urea to ammonia, cause the elevation of skin pH, which in turn increases fecal protease and lipase activity. These proteases and lipases cause the disruption of the epidermal barrier. Skin wetness, friction, maceration, and contact with feces, urine, and microbes further compromise epidermal integrity. This results in increased permeability of the skin to irritants such as soaps, powders, and detergents. Diaper dermatitis may begin as early as 1–2 months of age and may become a chronic or recurrent problem in older infants as well.
Allergic contact dermatitis is another component to consider, although it is more common in toddlers and children than neonates. Offenders can be dispersed dyes from disposable diapers and methylisothiazolinone in wet wipes. The differential diagnosis may also include seborrheic dermatitis, skin or perianal infections (particularly due to group A streptococcus), and psoriasis (see Chapter 61 ).
Milia are pinpoint white or yellow papules that are commonly present in 40–50% of neonates. Located predominantly on the face, they may also be seen in the oral cavity, where they are referred to as Epstein pearls (palate) or Bohn nodules (gingiva). The lesions represent keratin-filled epidermal inclusion cysts, which usually resolve spontaneously during the first few weeks of life. Unusually widespread or persistent lesions may be associated with defects such as hereditary trichodysplasia, oral-facial-digital syndrome, or particular subtypes of epidermolysis bullosa (EB). Milia may be present in several genodermatoses, including Bazex-Dupré-Christol, Rombo, and Brook-Spiegler syndromes; atrichia with papular lesions; and pachyonychia congenita type 2. Treatment is typically not needed, though topical retinoids have been used.
Sebaceous gland hyperplasia is characterized by the presence of multiple flesh- to yellow-colored tiny papules primarily on the nose and cheeks of full-term infants. The increased sebaceous cell size and number as well as sebaceous gland volume may result from maternal androgen stimulation. Spontaneous resolution occurs within the first 4–6 months of life.
Subcutaneous fat necrosis is a condition of otherwise healthy infants that is associated with preceding trauma, cesarean section, cold injury (including therapeutic hypothermia), or hypoxia. Over half of patients will develop lesions within the first week of life. This disorder occurs primarily in healthy full-term and postmature infants. It is thought to be due to the higher ratio of saturated to unsaturated fat in neonates, thereby predisposing the fat to crystallization with colder temperatures. Single or multiple erythematous to violaceous, indurated, tender nodules or plaques arise on the buttocks, thighs, back, cheeks, and arms. In rare cases, lesions liquefy, ulcerate, and drain an oily substance ( Fig. 60.8 ). The diagnosis can be confirmed by the histopathologic findings of fat lobules containing pathognomonic needle-shaped clefts surrounded by a mixed inflammatory infiltrate of lymphocytes, histiocytes, and foreign body giant cells. Intact lesions heal spontaneously within several months, whereas ulcerated lesions may heal more slowly and result in scarring. All patients should be screened for hypercalcemia, which may be present in nearly 70% of patients. Fortunately, hypercalcemia tends to be asymptomatic, without evidence of irritability, hypotonia, or weight loss, though life-threatening hypercalcemia may occur. The hypercalcemia may be delayed, with normal serum calcium early in the course of this disorder but elevated levels arising several weeks later. In most patients, the hypercalcemia resolves within 4 weeks of initial detection. Some recommend screening at 30, 45, and 60 days following resolution of skin lesions. The differential diagnosis includes cold panniculitis, cellulitis, and sclerema neonatorum.

Juvenile xanthogranulomas (JXGs) are rare, benign, solitary collections of non–Langerhans cell histiocytes, thought to be reactive in nature. They typically present during the neonatal and infantile period and usually resolve over subsequent months or years. Multiple lesions may exist and should raise suspicion for extracutaneous disease. The incidence of extracutaneous JXG is rare, and the eye is thought to be the most common site, occurring in 0.24% of patients. Multiple JXGs should trigger a thorough review of symptoms, as neurofibromatosis (NF)-1 is associated with multiple JXGs. Recommendations for ophthalmology examinations are somewhat controversial and are likely low yield, unless there are ocular or visual symptoms. A skin biopsy is diagnostic and shows collections of histiocytes and multinucleated giant cells called Touton giant cells.
A mastocytoma is a solitary skin-colored to light red or tan papule or plaque that is often located on the trunk, extremities, or neck. Some lesions may have a yellow or pink hue. The lesion may appear at birth or within the first few months of life. Histopathologic study reveals the dermis densely infiltrated with mast cells. The characteristic finding on physical examination is that stroking the lesion causes histamine release that results in tense edema within the lesion and an erythematous flare, known as the Darier sign. A skin biopsy and special stains for mast cells may confirm the clinical diagnosis. Symptoms such as pruritus or flushing, when present, are usually mild. Treatment is not usually necessary unless the patient has symptoms of excessive histamine release. The condition is self-limited and resolves spontaneously over several years. The lesions do not need to be excised.
Urticaria pigmentosa is characterized by the development of multiple mastocytomas, usually within the first 8–12 months of life ( Fig. 60.9 ). The lesions may vary in size from a few millimeters to several centimeters. Some lesions may not become pigmented until the child is approximately 6 months of age or older. Therefore, early lesions of urticaria pigmentosa may resemble recurrent urticaria until pigmentation is noted. The Darier sign, or urtication of the lesions upon rubbing, is seen in urticaria pigmentosa as well. Rarely, these lesions may produce enough histamine release to cause flushing, diarrhea, vomiting, tachycardia, and hypotension. Parents should be counseled about the avoidance of mast cell–degranulating agents.

Antihistamines should be used in any patient who experiences prominent histamine effects. Patients should be monitored closely for any symptoms that suggest systemic mastocytosis. In rare cases, other organs may be involved, including the intestines, bone, liver, spleen, and bone marrow. Intestinal involvement may be manifested by chronic diarrhea. The liver and spleen should be palpated for hepatosplenomegaly, and the patient should be monitored for any symptoms of bone involvement. Routine bone marrow and hematologic examinations are not required. Systemic manifestations are more common in adults; infants or children with significant systemic symptoms may require further evaluation. In most infants and young children, urticaria pigmentosa remits spontaneously by adulthood. Children who present at an older age tend to have a more persistent condition that is less likely to resolve.
Vascular birthmarks can be classified into two groups: tumors and malformations ( Table 60.3 ). Infantile hemangiomas are the most common of the vascular tumors, and their behavior is characterized by a growth phase (endothelial proliferation), followed by a plateau or stabilization phase and then an involutional phase. Vascular malformations are usually apparent at birth and tend to be relatively stable developmental abnormalities of vessels, including any combination of capillaries, veins, arteries, and lymphatic vessels ( Table 60.4 ).
| Vascular Tumors | Vascular Malformations |
|---|---|
| Hemangioma Kaposiform hemangioendothelioma Tufted hemangioma Noninvoluting congenital hemangioma (NICH) Rapidly involuting congenital hemangioma (RICH) |
Capillary malformation Venous malformation Lymphatic malformation Arteriovenous malformation (AVM) Mixed |
| Infantile Hemangioma | Vascular Malformations |
|---|---|
| Up to 55% present at birth | 90% recognized at birth |
| Rapid postnatal growth and slow involution | Static malformation of dysplastic vessels that grows proportionally with child |
| Rapid endothelial cell turnover | Normal endothelial cell turnover and proliferation |
| Increased incidence in female-to-male ratio (3:1–5:1) | Female-to-male incidence ratio 1:1 |
Infantile hemangiomas are the most common benign tumors occurring in children. These lesions develop in approximately 4% of White infants by 1 year of age. Females are affected approximately 3 times as often as males. The incidence is higher in premature infants. Other risk factors for hemangiomas include low birthweight and multiple gestations. The natural course of infantile hemangiomas includes proliferative and involutional phases that end in complete, spontaneous regression in most cases. There is some thought that infantile hemangiomas may be triggered by hypoxia, either through maternal events or the infant factors.
There are three types of infantile hemangiomas:
Superficial hemangiomas, once referred to as strawberry marks, are the most common type (60%). They are bright red with well-demarcated borders ( Fig. 60.10 ). Often, a pale pink stain or bruiselike patch is noted at birth before taking its more characteristic form.

Deep hemangiomas, previously known as cavernous hemangiomas, are the least common of the three types (15%). They typically have a blue-violaceous to skin-colored surface. These lesions involve the deep reticular dermis and subcutaneous tissue. These may not be noted until the infant is a few months old.
Mixed hemangiomas (25%) possess both superficial and deep components ( Fig. 60.11 ).

Most infantile hemangiomas occur on the head and neck, but any area of the body may be involved. Infantile hemangiomas may be indistinguishable from port-wine stains in the early weeks of life. Lesions must be followed closely during the first few weeks after birth to determine whether a proliferative phase is present. Although the cause of infantile hemangiomas is not clear, their natural course has been well documented. The initial lesion may be a white macule with central threadlike telangiectases or a red macule resembling a port-wine stain. A peripheral zone of pallor representing vasoconstriction may be noted at this stage. Within the first few months of life, the macule becomes raised and enlarges. During the first 6 months of life, infantile hemangiomas proliferate at a rapid rate, and after 6 months, the lesions grow at a slower rate. Deep hemangiomas (and to a lesser extent mixed hemangiomas) have a slightly delayed onset of growth but also have sustained growth when compared to superficial hemangiomas. Involution may begin as early as the first year of life and is heralded by a color change from bright cherry red to dull red violet. Deep hemangiomas start to lose their blue-violet hue. In time, the central portion of the superficial hemangioma develops a grayish-white color that eventually extends to the periphery of the lesion. Lesions on the lips and nose and deep hemangiomas usually involute more slowly. It is not possible to predict precisely how long an infantile hemangioma will take to involute. Statistically, 50% of lesions are gone by 5 years of age, 70% by 7 years, and more than 90% by 9 years. Once resolved, residual skin changes such as hypopigmentation, atrophy, and telangiectases may be present in up to 10–20% of affected patients. If infantile hemangiomas have grown rapidly during their proliferative phase or were very exophytic, residual fibrofatty tissue may also be seen.
Infantile hemangiomas have many potential complications and associations ( Table 60.5 ). For most, no treatment is needed. Management of infantile hemangiomas is based on a variety of factors. These include the size of the lesion, location of the lesion, age of the patient, rate of growth/involution at the time of presentation, and risk or presence of complications. β Blockers, such as oral propranolol or topical timolol 0.5% solution, are the initial treatment of choice. The most common adverse events are sleep changes and cool extremities, but more serious concerns are hypotension, bradycardia, and hypoglycemia, though these are rare. A pretreatment screening should include clinical examination to identify patients who are at risk for cardiac or pulmonary abnormalities.
| Location | Complication |
|---|---|
| Lips/perineal/lumbosacral area | Seen in rapidly growing lesions, especially of oral mucosa and genital area Risk for infection, scarring, hemorrhage; can be very painful |
| High output, extensive lesions | Congestive heart failure; hypothyroidism Extensive lesions with a large vascular supply may compromise cardiac function |
| “Beard” distribution | Symptomatic subglottic hemangiomas may occur in 50–60% of patients with extensive “beard” involvement Refer for laryngoscopy to evaluate risk for respiratory or airway compromise Often manifests within first 2–3 mo of life |
| Periorbital distribution | Associated ocular complications in up to 80% of patients Screening by an ophthalmologist to rule out astigmatism or amblyopia |
| Ear lesions | Location can cause the obstruction of auditory canal or decreased auditory conduction Monitor for otitis media or speech delay |
| Lumbosacral hemangiomas | High risk for spinal dysraphism; imaging of all midline lumbosacral hemangiomas should be considered Increased risk with other lumbosacral abnormalities (e.g., hypertrichosis, dimple, tags) Associated urogenital/anogenital anomalies may be present |
| Large, extensive cervicofacial hemangiomas | PHACE syndrome |
| Benign neonatal hemangiomatosis | Multiple cutaneous hemangiomas without evidence of visceral hemangiomatosis History taking/physical examination should be performed thoroughly to rule out systemic involvement Consider liver ultrasound for infants with five or more cutaneous hemangiomas Benign clinical course with involution of hemangiomas within first year |
| Disseminated neonatal hemangiomatosis | Multiple cutaneous hemangiomas with evidence of visceral hemangiomatosis Liver most commonly affected; can affect lungs, gastrointestinal tract, eyes, mouth, and tongue Work-up necessary to determine the extent of systemic involvement; aggressive treatment usually needed |
Lesions that may need to be treated include those on the midface, labial, periorbital, genital, or diaper area. These lesions warrant close clinical observation during the rapid growth phase of early infancy. Additional therapeutic modalities that are more rarely used include intralesional steroids, pulsed dye laser therapy, surgery, embolization, and sclerosing agents.
Location of infantile hemangiomas (segmental on face or beard distribution) as well as on the spine and lower back should raise concern for PHACE syndrome or PELVIS/SACRAL syndrome, respectively.
Posterior fossa malformations, hemangiomas, arterial anomalies, cardiac defects, and eye abnormalities (PHACE) syndrome is a rare syndrome that affects a subgroup of infants with infantile hemangiomas. It is likely the most common vascular neurocutaneous disorder. The cutaneous findings tend to be larger hemangiomas (>5 cm) and also tend to be segmental, rather than arising from one point. These hemangiomas can be more confluent, have a telangiectatic appearance, or be composed of grouped papules. They are nearly always located on the head or face. It is important to distinguish them from capillary malformations. Approximately 20% of all infants with segmental facial hemangiomas have extracutaneous anomalies.
Criteria for PHACE syndrome include one segmental hemangioma of the head (>5 cm in diameter) plus one major criterion or two minor criteria. Major and minor criteria involve a group of cerebrovascular, structural brain, cardiovascular, ocular, and ventral/midline defects.
Cerebral vascular anomalies are the most common extracutaneous manifestation. The changes tend to be arterial, unlike Sturge-Weber syndrome, which involves capillaries. Imaging (MRI/magnetic resonance angiography [MRA] of the head and neck) greatly aids in the work-up of a patient with a segmental hemangioma on the face/head, looking for arterial changes, as a subset of patients are at increased risk for vasculopathy and ischemic stroke, though this remains a poorly understood complication.
Many congenital brain abnormalities have been noted in patients with PHACE syndrome: The most common ones are malformations of the posterior fossa and cerebellum. Most patients with congenital lesions will have normal neurologic examinations during infancy, and, thus, screening should not be based on abnormalities with the neurologic examination.
Cardiovascular anomalies may be seen on echocardiogram in up to 40% of patients and include coarctation of the aorta (most common), aberrant subclavian aneurysm, ventricular septal defect, and arterial aneurysms. Ocular abnormalities are somewhat rare in PHACE syndrome but include microphthalmia, optic nerve hypoplasia, persistent fetal vasculature, and morning glory disk anomalies. Midline defects including sternal cleft, supraumbilical abdominal raphe, and subtle changes such as sternal pits, dimples, or papules can be seen. A screening echocardiogram should be done for children who are at risk for PHACE syndrome.
Treatment typically is propranolol, and for patients with life-threatening hemangiomas, it can be initiated prior to obtaining imaging results. Propranolol is typically well tolerated in patients with PHACE syndrome, though it is recommended that they undergo a physical exam and echocardiogram prior to initiation, to make sure there is not coarctation of the aortic arch.
PELVIS, LUMBAR, and SACRAL syndromes are all different acronyms to describe disorders that include a segmental hemangioma of the perineal area or midline lower back with underlying abnormalities. The acronyms PELVIS (perineal hemangioma, external genitalia malformations, lipomyelomeningocele, vesicorenal abnormalities, imperforate anus, and skin tag) and SACRAL (spinal dysraphism, anogenital anomalies, cutaneous anomalies, renal and urologic anomalies, associated with angioma of lumbosacral localization) have been used to describe associations with occult spinal dysraphism. The risk of a spinal anomaly is ∼35% with a solitary lumbosacral hemangioma. MRI is more sensitive than ultrasound in evaluating for underlying spinal abnormalities in lumbosacral lesions, such as tethered cord.
Capillary malformations (also known as port-wine stains or nevus flammeus) occur in 0.3% of all newborns. They are present at birth and represent progressive ectasia of the superficial vascular plexus. These lesions do not undergo spontaneous resolution. They are usually unilateral and segmental but can be bilateral ( Fig. 60.12 ). The face and neck are the most commonly affected sites. Capillary malformations are typically pink to red during infancy and darken to reddish-purple hues with advancing age. Affected adults frequently have thickened, nodular port-wine stains that may be associated with soft tissue hypertrophy. Capillary malformations occur as isolated cutaneous lesions or in conjunction with other abnormalities.

Sturge-Weber syndrome includes ipsilateral association of a facial capillary malformation, almost always involving the V1 distribution of the trigeminal nerve, eye abnormalities (primarily glaucoma), and vascular malformations of the ipsilateral leptomeninges and brain. The incidence of Sturge-Weber syndrome is approximately 5–10% in infants with a capillary malformation of the V1 distribution of the trigeminal nerve. Consequences of Sturge-Weber syndrome may include seizures, developmental delay, hemiplegia, and glaucoma. Neuroimaging may be helpful in demonstrating the characteristic calcifications of the leptomeninges and the abnormal cerebral cortex, although these changes may be quite subtle with early studies. Having MRI findings to diagnose Sturge-Weber syndrome prior to developing symptoms does not necessarily result in better outcomes. Newborns at risk for Sturge-Weber syndrome should have careful clinical follow-ups, including monitoring eye pressure for glaucoma. Early referral to a pediatric neurologist for education of parents to help monitor for neurologic symptoms is also recommended.
Other syndromes associated with capillary malformations include Klippel-Trenaunay syndrome and Parkes-Weber syndrome. Klippel-Trenaunay syndrome is characterized by a capillary malformation, venous and/or lymphatic malformation, and soft tissue and/or bone overgrowth of the affected limb. Parkes-Weber syndrome is the association of arteriovenous malformations, limb overgrowth, and the variable presence of lymphedema and multiple arteriovenous shunts. Klippel-Trenaunay syndrome is a slow-flow capillary-venous malformation, whereas Parkes-Weber syndrome is a fast-flow arterial-venous malformation. Both entities can result in overgrowth and hypertrophy of the affected limb; however, Parkes-Weber syndrome usually results in increased morbidity and clinical consequences.
Treatment of a capillary malformation is best accomplished with the pulsed dye laser. Several treatments are generally required over months to years to achieve desired fading. Depending on the location of the capillary malformation, the response to the pulsed dye laser may be limited. Many experts believe that early initiation of pulsed dye laser therapy results in superior cosmetic results.
Nevus simplex (salmon patch) is the most common vascular lesion in infancy. These lesions consist of ectatic capillaries and are present at birth in about 40% of infants. These pink to red macules can be located on the nape of the neck, glabella, forehead, upper eyelids, and nasolabial regions. More atypical locations include the lateral forehead, nose, upper and lower lip, and back. Unusually persistent or prominent nevus simplex can be associated with Beckwith-Wiedemann syndrome, Nova syndrome, nevus simplex with odontodysplasia, macrocephaly-capillary malformation syndrome, and Roberts-SC syndrome.
No treatment is necessary because most of these fade by 1–2 years of age. Persistent lesions can be treated successfully with the pulsed dye laser if cosmetically disturbing.
Cutis marmorata telangiectatica congenita (CMTC) manifests as an erythematous to dark, bluish-purple, reticulated vascular patch that does not resolve with physiologic warming. This disorder is characteristically more segmental and asymmetric than physiologic cutis marmorata. The clinical findings are most often noted within the first few days of life. Associated features may include cutaneous atrophy and ulcerations of the skin. CMTC has also been reported to be associated with additional abnormalities, including body asymmetry (hypotrophy or hypertrophy of affected limb), other vascular malformations, developmental delay, and glaucoma (with lesions in the V1/V2 trigeminal nerve distribution). CMTC may be difficult to differentiate from a reticulated capillary malformation. The clinical course of CMTC is characterized by gradual fading within the first 1–2 years of life, and treatment is generally not required.
Kasabach-Merritt phenomenon is the presence of thrombocytopenia, hemolytic anemia, hypofibrinogenemia, and consumptive coagulopathy in association with a vascular tumor. Kasabach-Merritt phenomenon is associated with distinct vascular lesions: namely, kaposiform hemangioendothelioma (KHE) or tufted angioma, but not infantile hemangiomas. KHE and tufted angiomas are rare vascular tumors thought to exist on a spectrum. They can be locally destructive, infiltrating underlying soft tissue. Clinical examination findings, histologic findings, and the behavior of associated vascular tumors differ from those of conventional infantile hemangiomas. These lesions are often firm and violaceous with a shiny texture and may proliferate for several years. This condition can be life-threatening and may warrant aggressive multimodal therapeutic modalities. Treatment of choice is complete excision, if possible, but may not be feasible given location, size, or tissue infiltration. Other treatments include sirolimus, high-dose systemic corticosteroids, compression therapy, embolization, irradiation, low-molecular-weight heparin, and interferon alfa. Sirolimus has been used with promising results.
Venous and lymphatic malformations are slow-flow vascular malformations that are often present at birth. Venous malformations are bluish, poorly demarcated, compressible masses. The characteristic bluish hue is caused by the presence of ectatic venous channels in the dermis. Often there may be associated swelling with changes in position or activity. Venous malformations can be segmental or more generalized, and radiologic imaging may assist in determining the extent of the lesion. Evaluation for central nervous system abnormalities with cranial imaging is recommended for patients with venous malformations of the face, to rule out developmental intracranial venous abnormalities that usually are asymptomatic. Many lesions manifest with pain caused by muscle involvement or with episodes of thrombosis or hematoma. Other associated risks include bone abnormalities (thinning, demineralization, or hypoplasia) and chronic localized intravascular coagulation. Treatment is aimed at correcting disfigurement and functional impairments. Therapy can include sclerotherapy, deep laser surgery, compression, and surgical excision. In many cases, it may be best to not intervene and to treat symptomatically.
Lymphatic malformations , previously referred to as lymphangiomas, are usually skin-colored masses that may have superficial clear or hemorrhagic vesicles that occasionally leak lymphatic fluid. These lesions can be classified as macrocystic, microcystic, or mixed. Macrocystic malformations often occur on the head and neck and are frequently diagnosed by prenatal ultrasonography. When such a large lymphatic malformation occurs on the head and neck region, it is often referred to as cystic hygroma. Microcystic malformations are usually more superficial lesions with a “frog spawn” appearance (hemorrhagic and clear vesicles) that intermittently leak lymphatic fluid. This characteristic lesion was previously referred to as lymphangioma circumscriptum. These lesions usually become more evident in childhood rather than infancy. Large lymphatic malformations may impinge on vital structures and cause severe compromise in the neonatal period. Cellulitis is a potential complication of lymphatic malformations and may require prophylactic antibiotics if recurrent. Treatment includes sclerotherapy, sirolimus, and surgery in select lesions; surgical therapy of these lesions is often difficult and may result in recurrences and complications.
Several hyperpigmented or darker pigmented lesions can be seen during the neonatal period and infancy, while others can present later in childhood ( Table 60.6 ).
| Disorder | Congenital or Acquired | Clinical Features |
|---|---|---|
| Freckles (ephelides) | Acquired | Small tan to brown, 1- to 5-mm macules Increase in number and pigmentation in summer and spring due to sunlight Seen in fair-skinned individuals in sun-exposed areas |
| Lentigines | Acquired | Uniform, dark, brown/black 2- to 5-mm macules No seasonal variation or change with sun exposure Can be anywhere on the body, including mucous membranes |
| Café-au-lait spots | Congenital or acquired | May be seen at birth or later in life Tan to brown discrete macules or patches Round or oval Six or more lesions >5 mm in prepubertal persons meets diagnostic criteria for neurofibromatosis (NF) NF lesions are smooth and well demarcated McCune-Albright syndrome spots are larger and more jagged |
| Dermal melanocytosis (mongolian spots) | Congenital | Brown, blue-gray patches often seen on lower trunk Seen usually in African-Americans, Asians, or Native Americans Usually fades over time |
| Nevus of Ota | Congenital or acquired | 50% present at birth; 50% develop in second decade Unilateral, blue-gray pigmentation in trigeminal nerve distribution Commonly involves ipsilateral sclera May darken or enlarge over time |
| Nevus of Ito | Congenital or acquired | Patchy blue-gray pigmentation of shoulder, supraclavicular area May increase in size and color over time |
| Congenital melanocytic nevus | Congenital | Tan, brown, dark brown macules, patches, plaques, seen at birth or early infancy Variable color and texture Large, giant, or multiple nevi increase risk for neurocutaneous melanosis |
| Nevus spilus (speckled lentiginous nevus) | Congenital or acquired | Well-demarcated, hyperpigmented patch with smaller, darker macules and papules within larger patch May be extensive and segmental in distribution Small risk for malignant transformation |
| Acquired melanocytic nevi | Acquired | May start as hyperpigmented macules (junctional melanocytic nevi) Over time, can become elevated papules (compound melanocytic nevi) Peaks in number during second and third decade of life Abnormalities in color, borders, size, symmetry may suggest malignancy |
| Melanoma | Acquired | Variegation in color, texture, or border of congenital or acquired melanocytic nevi Rare in childhood or infancy Risk correlated with family history and sun exposure in childhood |
Congenital melanocytic nevi (CMN) are pigmented macules, papules, patches, or plaques that are present at birth or early infancy in approximately 2–3% of children. The lesions are often tan at birth and become darker and hairier during infancy and childhood. Congenital nevi can be divided into small (<1.5 cm), medium (1.5–20 cm), large (20–40 cm), and giant (>40 cm) lesions on the basis of their projected adult size. In neonates and infants, lesions larger than 9 cm on the head and larger than 6 cm on the body constitute giant CMN ( Fig. 60.13 ). Most CMN are small to medium in size. The incidence of giant melanocytic nevi is approximately 1/20,000 live births. The majority of CMN have a variant in NRAS .

The malignant potential of CMN remains an area of great controversy. The risk for malignant transformation in the general population for small and medium congenital nevi is thought to be <1%, and there are no universal guidelines for their management. For comparison, the overall risk for melanoma in the general population in the United States is 2%. Removal of these nevi can wait until later childhood, when local anesthesia and outpatient surgery are feasible.
The risk for malignant transformation of giant CMN is another controversial issue. Interestingly, long-term prospective studies have shown melanoma of the central nervous system to be more common than melanoma of the skin. The incidence of melanoma is approximately 8% in those with CMN >60 cm with projected adult size. These large lesions warrant close observation and serial photography. Careful annual or semiannual examinations with palpation of the nevi are essential, as melanoma can arise from deep portions of the nevi with little or no apparent surface alterations. Removal of giant congenital nevi is also controversial from a future-melanoma-risk standpoint. Removal may require extensive grafting as well as soft tissue expansion procedures.
Neurocutaneous melanosis is defined as the presence of giant (>40 cm) and/or multiple CMN, in association with benign or malignant melanocytic infiltration of the leptomeninges. Clinically symptomatic neurocutaneous melanosis substantially worsens the prognosis of large or giant CMN and usually presents around or before 2 years of age, but some may not show symptoms until the second or third decade of life. Most symptomatic patients die within 3 years of the onset of initial neurologic symptoms, typically from central nervous system melanoma or mechanical obstruction. The most frequent clinical manifestations include hydrocephalus, seizures, papilledema, headaches, increase in head circumference, paresis, and developmental delay. Location overlying the axial skeleton and many satellite lesions are predictors of neurocutaneous melanosis.
Screening MRI of the central nervous system is currently the best predictor of all adverse outcomes. MRI with contrast of the head and spine within the first 6 months of life is suggested in newborns with giant CMN, particularly in the posterior axial distribution and especially if satellite nevi are present. An MRI is also recommended for any infant with two or more CMN, regardless of size. MRI abnormalities of the brain have been identified in asymptomatic patients with giant or multiple CMN. The most common imaging abnormalities in asymptomatic patients seen were T1 shortening in the cerebellum, temporal lobes, pons, and medulla. Radiologic findings can be very subtle and may be missed by radiologists unfamiliar with this entity. The risk of melanoma is higher in those with multiple CMN, particularly if neurologic abnormalities are noted on screening MRI.
Café-au-lait macules are well-circumscribed tan macules that usually measure <0.5 cm but may be as large as 15–20 cm in diameter. The lesions are found on any cutaneous site and may be present at birth or appear during early childhood. Although café-au-lait spots are seen in 10–20% of normal individuals, the presence of many macules should raise the clinical suspicion of NF or other genetic disorders (see Table 60.6 ). The presence of six or more café-au-lait spots (>0.5 cm in prepubertal children; >1.5 cm in postpubertal children) fulfills one of the diagnostic criteria for NF-1. Although the lesions are not pathognomonic, they are present in most patients with NF and tend to be larger and more numerous. Café-au-lait spots have also been associated with tuberous sclerosis, McCune-Albright syndrome, Turner syndrome, Bloom syndrome, ataxia-telangiectasia, Russell-Silver syndrome, Fanconi anemia, epidermal nevus syndrome, Gaucher disease, and Chédiak-Higashi syndrome.
Dermal melanocytosis (mongolian spots) are large, poorly demarcated, slate-gray to blue-black patches usually located over the buttocks or lumbosacral region of normal infants. The condition occurs in approximately 80–90% of Black infants, 75% of Asian infants, and 10% of White infants. Dermal melanocytosis may be single or multiple and frequently measure up to 10–20 cm in diameter. This benign disorder is present at birth, usually fades during early childhood, and necessitates no therapeutic intervention. In rare cases, the lesions may persist into adulthood and may benefit from therapy with lasers that treat dermal pigmentation. These lesions should not be confused with bruises. Dermal melanocytosis is also seen in Hurler, Hunter, GM1 gangliosidosis, Niemann-Pick, mucolipidosis, and mannosidosis syndromes.
The nevus of Ota and nevus of Ito are special variants of dermal melanocytosis commonly seen in Asian and Black individuals. In contrast to mongolian spots, these conditions tend to persist throughout adulthood. The nevus of Ota is a slate-gray to blue-black patch located in the distribution of the trigeminal nerve. The condition is usually unilateral and involves the forehead, temple, periorbital region, nose, and cheek. Pigmentation of the sclera, iris, and choroid occurs in about 50% of affected individuals. The disorder may be cosmetically disfiguring, and laser treatment may be promising in some cases. The nevus of Ito is a similar lesion occurring in the distribution of the lateral supraclavicular and brachial nerves. The condition is usually unilateral and involves the shoulder, neck, upper arm, scapular, and/or deltoid regions. It may be seen alone or in conjunction with the nevus of Ota.
These conditions are often cosmetically disfiguring and persistent. They can be markers of serious systemic diseases. Pigmentary disorders may be localized or generalized; congenital or acquired; and transient, stable, or progressive ( Table 60.7 ).
| Disorder | Congenital or Acquired | Clinical Features |
|---|---|---|
| Piebaldism | Congenital | Autosomal dominant inheritance Leukoderma of frontal scalp White forelock Usually involves face, neck, trunk, flank, and extremities Waardenburg syndrome is a variant, with sensorineural deafness, limb defects, and Hirschsprung disease |
| Nevus depigmentosus | Congenital | Well-circumscribed hypopigmented patch (not typically depigmented) May be isolated or segmental Usually present at birth or infancy Wood lamp may aid in diagnosis Often found on trunk or extremities |
| Hypomelanosis of Ito | Congenital | Whorls or streaks of hypopigmentation that follow lines of Blaschko Usually present at birth, but may present in first few years of life Can be associated with central nervous system, eye, or musculoskeletal abnormalities |
| Nevus anemicus | Congenital | Rubbing or temperature change causes erythema of surrounding skin Often unilateral and on trunk Not accentuated by Wood lamp Asymptomatic |
| Ash leaf spot | Congenital | Hypopigmented macules/patches often present at birth Wood lamp may aid in diagnosis Solitary lesion often of no significance Multiple lesions are associated with tuberous sclerosis |
| Vitiligo | Acquired | Complete loss of pigment in involved areas May be segmental in distribution Hyperpigmentation can be seen at the edges of lesions Infrequently seen with autoimmune disorders, such as hypothyroidism |
| Albinism | Congenital | Complete depigmentation or hypopigmentation in skin Affects eyes and hair Increased risk for skin cancer |
Nevus depigmentosus is a benign, solitary, hypopigmented macule or patch that is noted at birth. It is not depigmented as the name suggests. It typically remains stable in size and may grow in proportion to the patient as they grow. It should be differentiated from vitiligo.
Ash leaf spots are hypopigmented macules, sometimes present at birth or within the first few months or years of life, that allow early identification of individuals with tuberous sclerosis ( Fig. 60.14 ). Although occasionally observed in normal infants, the characteristic lesions are present in up to 90% of patients with tuberous sclerosis. They are usually 2–3 cm in size and are located on the trunk and extremities. The macules may be lancet shaped or may have a confetti-like or irregularly shaped appearance. Wood lamp examination may facilitate identification . Although tuberous sclerosis is an autosomal dominant disorder, spontaneous gene variants are responsible for up to 50% of new cases. Other cutaneous findings include facial angiofibromas (adenoma sebaceum), periungual or subungual fibromas, gingival fibromas, shagreen patches (connective tissue hamartomas), and fibrous plaques (typically on the forehead). Systemic manifestations include seizures, intellectual disability, cardiac rhabdomyomas, renal angiomyolipomas and cysts, retinal nodular hamartomas, and pulmonary cysts. Imaging studies of the brain may demonstrate cortical tubers or subependymal nodules, which are pathognomonic for tuberous sclerosis.
Piebaldism is characterized by circumscribed areas of depigmentation in the newborn. The leukoderma is usually located on the frontal scalp and is associated with a white forelock; however, the depigmented patches characteristically involve the trunk, upper arms, and legs. Hyperpigmented or normally pigmented macules or patches may occur within the depigmented patches. This rare condition is transmitted in an autosomal dominant pattern. The disorder is usually present at birth but may not be recognized until later because of the light color of neonatal skin. A Wood lamp may enhance the contrast between depigmented and normal skin.
Piebaldism is a stable condition throughout life, and most affected individuals are otherwise normal. Sun protection and cosmetic camouflage of the depigmented skin are the mainstays of therapy.
Waardenburg syndrome is a rare genetic disorder characterized by a white forelock, areas of leukoderma, congenital sensorineural deafness, heterochromia of the irides, and lateral displacement of the medial canthi. Other features may include a flattened nasal bridge, confluent eyebrows, hypoplasia of the nasal alae, speech impairment that may or may not be related to presence of a cleft lip or palate, and various skeletal abnormalities. It is most commonly inherited in an autosomal dominant fashion, though autosomal recessive inheritance patterns are sometimes seen.
Albinism is manifested by diffuse congenital hypopigmentation or depigmentation of the skin, hair, and eyes. This heterogeneous group of disorders is composed of approximately 10 types of oculocutaneous albinism and 5 forms of ocular albinism. Most types of oculocutaneous albinism are inherited in an autosomal recessive pattern. The variants of ocular albinism are transmitted in an X-linked or autosomal recessive mode of inheritance.
The various forms of albinism can usually be diagnosed by findings on physical examination. These features include absent or reduced pigmentation of skin and hair and ophthalmologic findings such as foveal hypoplasia, nystagmus, photophobia, transillumination of the irides, fundal depigmentation, and decreased visual acuity. Patients should be monitored closely by ophthalmologists and evaluated for hearing loss. In White persons, the skin is usually milk white and the hair is white, blond, or light brown. The pupils are usually pink, and the irides are blue or gray. In African-Americans, the skin may appear tan or white and is frequently freckled. The hair is usually blond or red, and the eyes are blue or hazel.
Treatment of albinism includes photoprotection and sun avoidance. Individuals are predisposed to severe actinic damage and should be monitored closely for the development of actinic keratoses, basal cell carcinomas, squamous cell carcinomas, and melanomas.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here