Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Increased gassiness is a complaint frequently encountered by physicians. Although 10% to 30% of the general adult population report symptoms related to excessive gastrointestinal gas, its prevalence in children remains unknown. , The investigation of gas-related complaints is challenging because of the difficulty of measuring the volume or composition of gastrointestinal gas and verifying its relation to symptoms. In addition, it has been suggested that the perception of gassiness and bloating in some patients with abdominal pain is more likely a manifestation of the visceral hypersensitivity implicated in irritable bowel syndrome (IBS) than true excessive gastrointestinal gas.
Patients with complaints of excessive gastrointestinal gas are at risk of being subjected to expensive and unnecessary diagnostic tests in an effort to “cure” a nonexistent problem, and it is important to appreciate the physiology of gastrointestinal gas to understand its relationship to disease. Most unscientific notions and home remedies available for gassiness further challenge effective management of such patients. In this chapter, the physiology of gastrointestinal gas is reviewed, the clinical manifestations of excessive gastrointestinal gas are discussed, and infantile colic is reviewed.
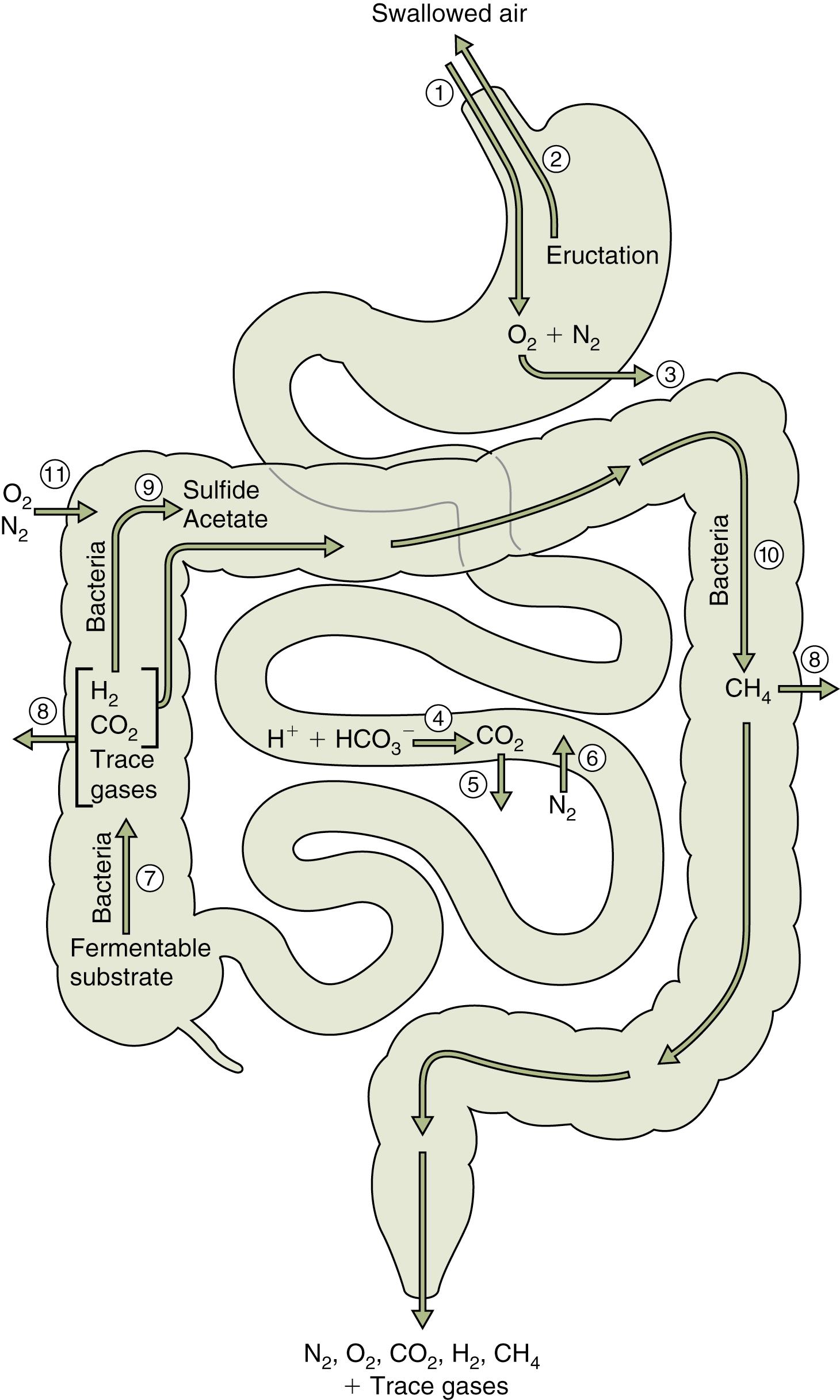
Gastrointestinal gas may originate from three sources: (1) swallowed air; (2) intraluminal production, that is, bacterial production and reaction of acid and bicarbonate; and (3) diffusion from the blood ( Fig. 10.1 ). Gas may be lost from the gastrointestinal tract through eructation or belching, passage of flatus, bacterial consumption, and diffusion into the bloodstream. Although there are no published data on the gas content of the gastrointestinal tract in an infant or a child, studies in healthy adults indicate that the normal gastrointestinal tract contains less than 200 mL of gas.
More than 99% of gastrointestinal gas is made up of five gases, namely carbon dioxide (CO 2 ), hydrogen (H 2 ), methane (CH 4 ), nitrogen (N 2 ), and oxygen (O 2 ), in varying percentages ( Box 10.1 ). Two of these, H 2 and CH 4 , are combustible and can be explosive in a proper mixture with O 2 . All of these gases are odorless. Odoriferous gases are present in trace amounts, that is, less than 1% of flatus, and are sulfur based. Most of the symptoms from excessive gastrointestinal gas are attributable to the five odorless gases, although socially, the odoriferous gases are the most unacceptable.
The main source of N 2 is swallowed air. An adult ingests more than half an ounce (15 mL) of air with each swallow, the main components of which are N 2 and O 2 , and as such, these are the main components of gastric luminal gas. CO 2 , H 2 , and CH 4 are produced mainly within the gastrointestinal lumen. CO 2 is generated through the interaction of H 2 ion and bicarbonate and found in large volumes in the duodenum following the chemical reaction between gastric hydrochloric acid and alkaline intestinal fluid. The distal small intestine gas composition is not well defined. In patients with pathologic conditions such as small bowel bacterial overgrowth, significant amounts of H 2 are generated in the small intestine.
Both H 2 and CH 4 are generated in the colonic lumen. H 2 is mainly a product of bacterial fermentation; germ-free rats and newborn infants do not produce H 2 . Carbohydrates, for example, lactose, and proteins to a much lesser degree are substrates for bacterial production of H 2 . Colonic microbiota, mainly Methanobrevibacter smithii , generate CH 4 using H 2 and CO 2 . About one-third of adults carry sufficient numbers of methanogenic bacteria to produce appreciable CH 4 . The tendency to produce CH 4 appears to be familial and determined by early environmental factors rather than genetic causes. CH 4 tends to be trapped within stool, and large CH 4 producers have stools that float in water.
Generation of H 2 and CH 4 is also enhanced by carbohydrate overload, as in excessive intake of fruit juices; ingestion of sugar alcohols (sorbitol and xylitol); ingestion of poorly absorbed carbohydrates such as cauliflower, cabbage, broccoli, Brussels sprouts, and beans; or disaccharidase deficiency. Disaccharidase deficiency may be primary, as noted in primary lactase deficiency or hereditary fructose intolerance, or secondary, as in a variety of disorders that injure the small intestine including celiac disease, allergic enteropathy, inflammatory bowel disease, giardiasis, and viral gastroenteritis.
Excessive gastrointestinal gas may contribute to a number of symptoms including eructation, aerophagia, gas-bloat syndrome, abdominal bloating and distention, and flatulence.
Belching is the audible escape of air from the esophagus into the pharynx, and its medical term is eructation . Physiologically, there are two types of belches— gastric belch and supragastric belch. Gastric belching is the escape of swallowed intragastric air that enters the esophagus during a transient lower esophageal sphincter relaxation (TLESR) that is triggered by distention of the proximal stomach and allows venting of air from the stomach. Once in the esophagus, esophageal distention initiates reflex relaxation of the upper esophageal sphincter (UES). Gastric belches occur 25 to 30 times per day and are physiological. In supragastric belches, the air is ingested immediately before it is expelled again. Supragastric belches are behavioral termed as eructosa nervosa and if excessive can be treated by speech therapy or behavior therapy. Recent progress in both high-resolution manometry and impedance monitoring system enables the objective differentiation of supragastric belching from gastric belching.
In a large U.S. population study, aerophagia was found in 4.2% of children. It is particularly common in patients with neurocognitive disabilities. According to the Rome IV criteria, the diagnosis of aerophagia includes all of the following :(1) Excessive air swallowing, (2) abdominal distention due to intraluminal air, which increases as the day progresses, (3) repetitive belching and/or increased flatus, and (4) symptoms inexplicable by another medical condition following appropriate evaluation. These symptoms should be present for at least 2 months before diagnosis. It is important to differentiate aerophagia from gastrointestinal motility disorders such as gastroparesis, megacolon, and intestinal pseudo-obstruction. Aerophagia can also result from excessive gum chewing, use of a straw, clenching on a pencil, or oral breathing as in adenotonsillar hypertrophy or unrecognized H-type tracheoesophageal fistula. Patients should be counseled on chewing their food slowly and not gulping. Excessive upper gastrointestinal gas can be associated with consumption of large amounts of carbonated beverages, and appropriate lifestyle modifications might be needed.
Gas-bloat syndrome, seen in children following gastric surgery such as Nissen fundoplication, results from an inability of the patient to belch effectively. The newly made wrap around the lower esophageal sphincter (LES) prevents expulsion both by reducing the number of TLESRs and by increasing sphincter pressure during TLESRs. The resultant air accumulation in the stomach and intestines manifests as bloating, abdominal discomfort (sensation of intestinal gas), and difficulty to burp. While the symptoms can be intractable, leading at times to reversal of the wrap or conversion of a 360 degrees wrap to a 180 degrees wrap, other interventions include simethicone, prokinetics, and venting of the gastrostomy tube if present. ,
Bloating refers to a sensation of abdominal fullness, whereas distention connotes visible or measurable increase in abdominal girth. Patients often attribute the feeling of abdominal bloating to excessive gas burden, although the relationship between the amount of intestinal gas and symptoms is not linear. Studies of adult patients with complaints of excessive gas revealed that the quantity of intestinal gas is usually not different between “gassy” and “nongassy” subjects. , One study reported that patients with a history of abdominal bloating had significantly delayed transit of small intestinal gas compared with a healthy control population.
Bloating is part of the symptom constellation of IBS. The discomfort associated with bloating in patients with IBS is likely due to dysmotility and heightened perception. No appreciable differences were found in the volume of gastrointestinal gas in adults with complaints of bloating versus controls, although there was an increased symptomatic response to gas infusion in patients with bloating.
Abdominal distention may result from excessive aerophagia or increased gastrointestinal gas production as in malabsorption syndromes. Children with aerophagia often have a nondistended abdomen upon rising, which progressively distends over the day and may be accompanied by cramps and abdominal pain. The physical examination may be impressive for abdominal distention and tympany. Plain abdominal films reveal gaseous distention of the bowel. Symptoms and signs may be so intense as to mimic intestinal obstruction or celiac disease. Fatal tension pneumoperitoneum has been reported secondary to aerophagia.
An average adult passes flatus about 10 to 12 times per day, with an upper limit of 20 times a day. The frequency of flatus does not correlate with age or gender, although data on children are lacking. Although flatulence can be a social embarrassment, comfort should be derived from the fact that over 99% of the flatus consists of odorless gases. Increased gastrointestinal gas production, rather than aerophagia, is usually responsible for flatulence in adults, although it is not known if the same can be extrapolated to children. The source of the flatus may be assessed by gas chromatographic analysis of flatus collected via a rectal tube. Aerophagia should be considered the main contributor if N 2 is the leading component; predominance of H 2 , CO 2 , and CH 4 would suggest increased intraluminal production, for example, secondary to bacterial fermentation of malabsorbed carbohydrates.
An extensive radiologic and endoscopic evaluation of a patient with excessive flatulence alone is generally fruitless and should be avoided. Efforts should instead be directed at eliciting a detailed history ( Table 10.1 ). Appropriate investigation should be considered if the flatulence is accompanied by other symptoms such as diarrhea, hematochezia/melena, abdominal pain, or weight loss. Otherwise, dietary modifications directed toward limiting intake of fruit juices and poorly absorbed carbohydrates, such as cabbage and legumes, may need to be enforced. Excessive consumption of high-carbohydrate–containing beverages (e.g., high-fructose corn syrup) is more apt than high intake of cruciferous vegetables such as cabbage to be a culprit in children. A detailed inquiry into intake of liquid medications and “sugar-free” drinks should be undertaken because these products contain sorbitol, an artificial sweetener that is poorly absorbed and readily fermented by colonic bacteria.
| Symptom or Sign | Air Swallowing | Bacterial Fermentation |
|---|---|---|
| Increased eructation | Yes | No |
| Increased salivation | Yes | No |
| Gas is stress related | Yes | No |
| Gas is meal related | No | Yes |
| Abdominal bloating | Yes | No |
| Malodorous gas | No | Yes |
| Nocturnal gas | No | Yes |
If the patient is bothered by odoriferous flatus, there are now several commercially available charcoal-lined seat cushions and undergarments to help in social situations by effectively absorbing odiferous sulfur gases.
Although traditionally viewed as an inert bystander, CH 4 has recently been linked to and even implicated in the pathogenesis of constipation. Recent studies in both children and adults have revealed strong associations between CH 4 production (as detected on breath testing) and constipation. In a study that examined if CH 4 production was associated with diarrhea or constipation in adults with IBS or inflammatory bowel disease, the researchers noted that CH 4 production on lactulose breath testing was present in all patients with constipation-predominant IBS (C-IBS). Similar studies in children have linked severity of constipation to CH 4 production. Soares and colleagues reported higher rates of CH 4 production in children with constipation and soiling compared with those with constipation but no soiling. These studies highlight associations but leave questions as to whether CH 4 production is a cause or effect of constipation. However, there is accumulating evidence that CH 4 has direct effects on gut motility. Among patients with constipation, CH 4 production was higher in adults with slow-transit constipation than those with normal-transit constipation. Animal studies may provide an explanation for this; Pimentel and colleagues infused CH 4 in vivo into canine small intestine and demonstrated delayed transit compared with infusion of room air. In a second phase of the study, they showed that although CH 4 augmented contractility of guinea pig ileum, it had an overall slowing effect by promoting segmental, nonpropagating contractions in the small bowel. The effects of CH 4 on the small intestine are important to elucidate further, as patients with IBS may have altered gut flora and small intestinal bacterial overgrowth, as evident on breath testing. These recent advances, at least in adults, suggest that patients with C-IBS may benefit from treatment with neomycin or other similar antibiotics that eradicate methanogenic flora.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here