Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Chronic rheumatic heart disease (RHD) is the persistence of valvar dysfunction following an episode of acute rheumatic fever (ARF) or ARF recurrence. Once the inflammatory markers normalize, any persistent valve dysfunction should be termed chronic RHD.
ARF, a delayed autoimmune reaction to group A streptococcal infection, is now rarely seen in high-income countries, where RHD is predominantly reported in the aging population as a consequence of ARF several decades earlier, usually occurring during childhood. However, in the world's poorest populations, RHD remains a leading noncommunicable disease of the young. In 2010, an estimated 34.2 million people worldwide had RHD, resulting in 345,110 deaths and 10.1 million disability-adjusted life-years lost per annum. These Global Burden of Disease figures could be an underestimate due to limited global data, underdiagnosis, and scarce formal reporting systems.
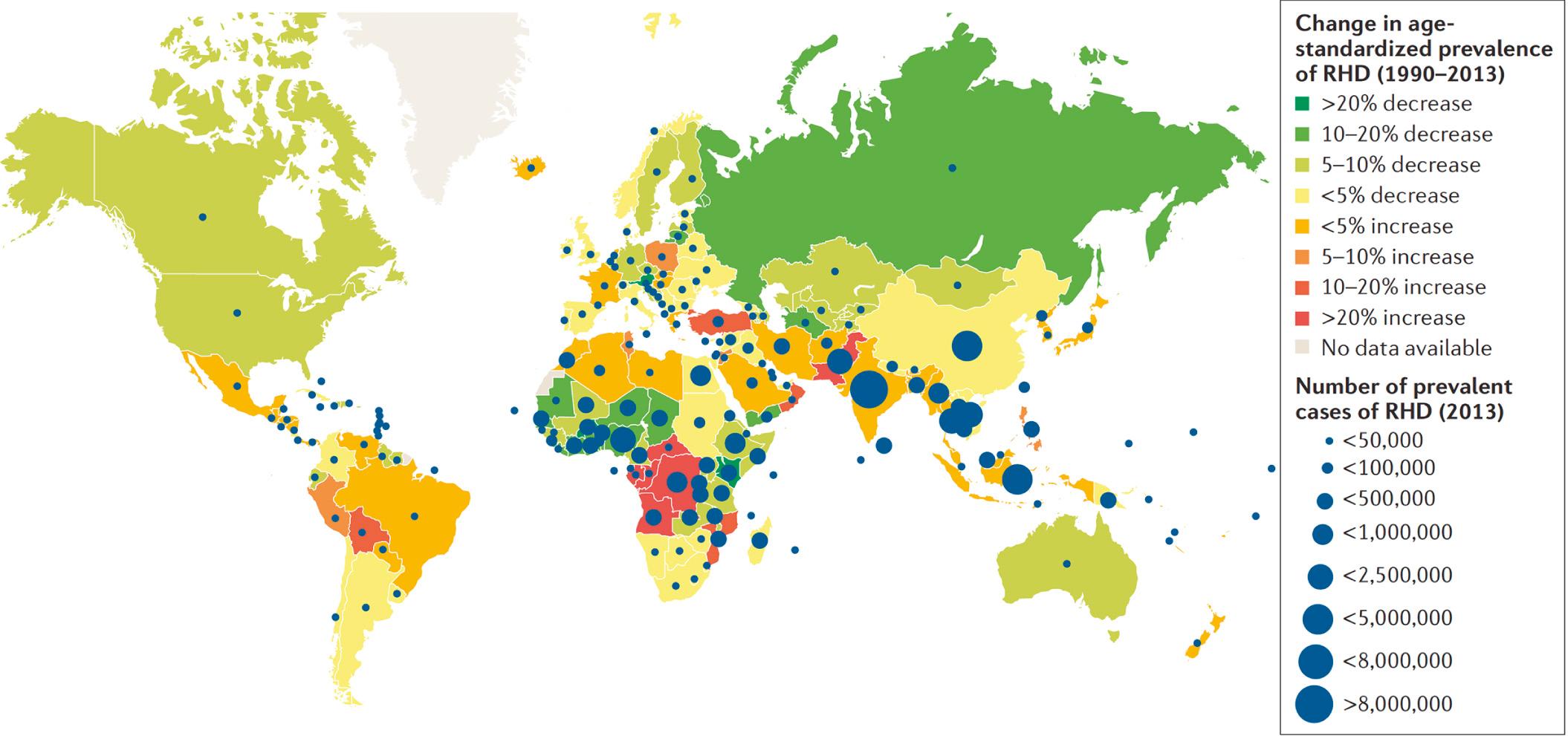
Regional heterogeneity exists regarding age of onset, mode of presentation, and specific valvar abnormality, which are influenced primarily by the socioeconomic and medical backgrounds of the populations involved. Global burden of disease is depicted in Fig. 55.1 . Children aged between 5 and 15 years are at greatest risk of a primary episode of ARF. In endemic populations, the peak prevalence of RHD is between ages 25 and 45 years, reflecting the cumulative effect of recurrent episodes of ARF ( Fig. 55.2 ).

The exact pathogenesis of ARF is incompletely understood. RHD is thought to be the result of immune-mediated endothelial and connective tissue damage. Cardiac valves are especially prone to damage because of their thin structure, with a small core of connective tissue covered by two endothelial layers. The healing process of rheumatic valvulitis leads to varying degrees of neovascularization and fibrosis. This process disturbs the delicate architecture of the valvar apparatus, leading to valvar regurgitation, stenosis, or both. Clinical and echocardiographic regression and even resolution of mild to moderate disease is well documented. However, if the first episode of carditis results in more severe valvar dysfunction or if the valves are exposed to recurrent episodes of rheumatic fever, chronic deforming valvar damage and dysfunction develops.
The pericardial effusion seen during the acute phase of rheumatic fever usually resolves with no long-term sequelae. Myocardial impairment occurs only in the setting of severe valvar dysfunction, and recovery can be expected if timely surgical correction of the valvar dysfunction takes place.
The hallmark of RHD is mitral valve (MV) disease: mitral regurgitation (MR), mixed MV disease, and/or pure mitral stenosis (MS). Although postmortem studies show universal MV involvement, echocardiographic studies reveal that isolated aortic valve (AV) disease occurs in approximately 2% to 8% of patients with RHD ( Fig. 55.3 ). In advanced disease, the tricuspid valve and, very rarely, the pulmonary valve may also be affected, but seldom if ever without MV involvement.

Patients younger than 10 years predominantly have pure MR. By the second decade of life, RHD is characterized by mixed MV disease. In the third decade of life, up to 5% of RHD patients will develop pure MS. In some regions of Sub-Saharan Africa and India, pure MS is more common and often occurs earlier in life. Concomitant AV disease increases with age and is present in over 50% of patients by the second decade (see Fig. 55.3 ). Like MV disease, aortic disease in the young is characterized by regurgitation. By the second decade of life, mixed aortic disease develops in some; however, pure aortic stenosis is generally not seen until the fourth or fifth decade of life.
The majority of patients with RHD are diagnosed late, when individuals present with complications of RHD including heart failure, infective endocarditis, tachyarrhythmias, stroke, pregnancy-related complications, or sudden death. Patients with RHD often have a long latent phase of asymptomatic valvar heart disease, often without any preceding symptoms of ARF. The global registry of RHD, REMEDY, suggests that even in high-income populations, only 59% of patients with RHD had a preceding history of ARF, and this drops to 22% in low-income populations. The reason for this is likely multifactorial, and access to health care and public awareness are important factors. The current ARF guidelines may not be sufficiently sensitive to detect ARF in high-risk populations. Patients may not present to local health facilities with what might be seen as relatively minor symptoms or, alternatively, medical officers may not be equipped to make the diagnosis. In contrast to the arthritis of ARF, acute carditis may not cause symptoms. Consequently the early diagnosis of RHD remains challenging. This is especially so in resource-poor settings.
In individuals with a documented history of ARF, once acute inflammation subsides, the persistence of pathologic regurgitation of the mitral and/or AVs on echocardiography is sufficient to confirm chronic RHD. The echocardiographic criteria to diagnose pathologic mitral and aortic regurgitation (AR) are detailed in Box 55.1 . In circumstances where echocardiography is not available, the persistence of a mitral and/or aortic regurgitant murmur is sufficient, although auscultation has a low positive predictive value and hence low diagnostic utility in detecting mild regurgitation.
a Congenital anomalies must be excluded.
Pathologic MR and at least two morphologic features of RHD of the MV
MS mean gradient ≥4 mm Hg
Pathologic AR and at least two morphologic features of RHD of the AV
Borderline disease of both the AV and MV
At least two morphologic features of RHD of the MV without pathologic MR or MS
Pathologic MR
Pathologic AR
Seen in two views
In at least one view jet length is ≥2 cm b
b A regurgitant jet length should be measured from the vena contracta to the last pixel of regurgitant colour (blue or red) on nonmagnified (nonzoomed) images.
Peak velocity ≥3 m/s
Pansystolic jet in at least one envelope
Seen in two views
In at least one view jet length is ≥1 cm b
Peak velocity ≥3 m/s
Pandiastolic jet in at least one envelope
AMVL thickening ≥3 mm c
c AMVL thickness should be measured during diastole at full excursion. Measurement should be taken at the thickest portion of the leaflet and should be performed on a frame with maximal separation of chordae from the leaflet tissue.
Chordal thickening
Restricted leaflet motion
Excessive leaflet tip motion during systole
Irregular or focal thickening
Coaptation defect
Restricted leaflet motion
Prolapse
Borderline RHD category only applies to individuals younger than 21 years.
AR , Aortic regurgitation; AMVL, aortic mitral valve leaflet; AV , aortic valve; MR , mitral regurgitation; MS , mitral stenosis; MV , mitral valve; RHD , rheumatic heart disease.
The majority of patients with RHD worldwide fit into the category of having RHD with no prior history of ARF. The reason for cardiology referral or assessment may include evaluation of cardiac murmur, symptomatic status, complications of RHD, or abnormality detected on echocardiographic screening.
The 2012 World Heart Federation echocardiographic criteria were established to facilitate early diagnosis of RHD in individuals without a previous history of ARF. Box 55.1 details the minimum diagnostic criteria. In this setting, pathologic regurgitation is insufficient to diagnose RHD. Both morphologic features of RHD and pathologic regurgitation must be present or, alternatively, there must be multivalve disease of both the MVs and AVs.
If echocardiography is not available, then the diagnosis relies on auscultatory findings of valvar dysfunction. Naturally auscultation alone does not determine the etiology of disease. In this setting, the pretest probability of RHD will determine diagnostic and management strategies.
The outcome and progression of RHD relate to the severity at diagnosis, exposure to ARF recurrences, and access to tertiary medical care.
Those with mild RHD at diagnosis and good adherence to secondary prophylaxis have excellent long-term outcomes. Those with severe disease at diagnosis have a bleak prognosis and will likely require cardiosurgical intervention within 2 years of diagnosis or will succumb.
In the United States, before the introduction of secondary prophylaxis, 20-year mortality due to RHD was as high as 30% to 80%, with most affected individuals dying before the age of 30 years. Similar findings are still observed in many low- and middle-income countries, with annual mortality rates of 3.0% to 12.5%. In Nigeria and Ethiopia, the mean age at death is below 25 years. In New Zealand, a high-income country, the outcome of RHD is more favorable, with a median life expectancy of 56 years. The New Zealand data may reflect the tail of RHD in European adults who had milder forms of RHD from earlier decades, when ARF affected adults of European ethnicity, or it may reflect better access to medical care. Finally, there are limitations to using International Classification of Diseases (ICD) discharge data when nonspecified valvar disease is attributed a rheumatic etiology.
Overall, it can be said that the disease progression and mortality due to RHD is greatest in low-income countries, and within those countries it is the most disadvantaged groups that have the worst outcomes.
Mild to moderate chronic RHD is almost always asymptomatic in children and young adults. Even severe RHD may be associated with minimal or no symptoms in the young. Without surgical intervention for this latter group of patients, a rapid decompensatory phase often follows.
In the setting of MR, symptoms occur as increasing left atrial pressure causes pulmonary venous hypertension with symptoms of breathlessness. In the setting of chronic severe MV disease, symptoms may be very gradual and very subtle, such as being unable to complete a full game of football—thus shortness of breath during peak physical activity. This may progress to shortness of breath at rest, followed in time by clinical decompensation and death. More rapid progression of symptoms can also occur in the setting of acute-on-chronic MV disease.
The clinical signs of MR include a pansystolic murmur heard best at the apex with radiation to the axilla, as the direction of regurgitant jet is usually posterolateral. Less commonly the murmur radiates medially if the regurgitant jet is directed that way. Patients with moderate or more severe MR will have lateral displacement of the apex beat, and there may be an associated diastolic murmur related to increased transmitral flow.
If MR is severe, ECG and chest x-radiograph (CXR) will demonstrate left ventricular (LV) dilatation/hypertrophy as well as pulmonary congestion.
In the setting of MV stenosis, progressive obstruction to LV inflow develops, leading to a diastolic gradient between the left atrium and ventricle. This pressure gradient is increased in settings of increased flow and faster heart rates, for example during exercise, pregnancy, or in the presence of atrial fibrillation with rapid ventricular rates. Patients usually do not develop symptoms until the MV orifice decreases to less than 2 cm 2 . The initial symptom is exertional dyspnea with symptoms of orthopnea and paroxysmal dyspnea as the MV orifice decreases to less than 1.0 to 1.5 cm 2 . Symptoms of cough, hemoptysis, chest pain, palpitations, hoarse voice due to compression of the left recurrent laryngeal nerve and left atrial dilatation are signs of very advanced disease.
The characteristic clinical finding of mild to moderate MS is a low-pitched, diastolic rumble or heart murmur heard best at the apex with the patient in a left lateral position. The murmur is accentuated by increasing heart rate with mild exercise. As disease progresses in severity, the pulses become small in volume and a parasternal heave and loud P2 develop due to pulmonary hypertension. Unless the patient is in atrial fibrillation (AF), the duration of the murmur increases and a presystolic accentuation develops. Less commonly, patients may present with or have signs of systemic embolism from the left atrium, although this is likely related more to the development of AF rather than the severity of the MS in itself.
ECG is useful to confirm sinus rhythm or AF. Left atrial enlargement and right ventricular hypertrophy is a marker of severe disease. CXR may show left atrial enlargement and upper lobe diversion of blood flow. Calcification of the MV apparatus may be visible, as well as pulmonary congestion if in heart failure.
Patients with chronic stable moderate or severe regurgitation often remain asymptomatic for years. Eventually dyspnea on exertion, orthopnea, and even paroxysmal nocturnal dyspnea and edema develop. Angina can occur, even if the patient has normal coronary arteries, as the result of reduced coronary perfusion due to low diastolic blood pressure.
The clinical signs of mild AR are normal pulses and an early diastolic, blowing decrescendo diastolic murmur best heard at the lower left sternal edge at the end of expiration with the patient sitting upright and leaning forward. In general, more severe disease is associated with a shorter murmur. A widened pulse pressure indicates moderate to severe AR. Collapsing pulses indicate severe AR. In torrential AR, the murmur is heard with the patient lying flat and is associated with what is described as a “water-hammer pulse.” The Korotkoff sounds are heard almost down to the pressure of zero. The apical impulse is hyperdynamic and displaced due to LV enlargement. The presence of a systolic flow murmur across the AV reflects increased stroke volume.
If AR is severe, the ECG will show increased LV voltages and the CXR will demonstrate left ventricle enlargement.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here