Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The elbow is one of the most congruous joints in the body. Joint stability is provided by a combination of the bony architecture and the collateral ligaments and muscles. The lateral collateral ligament (LCL) complex plays a key role in elbow stability, preventing the proximal ulna and radius from subluxation as the supinated forearm is axially loaded. Trauma, usually dislocation, is the most frequent cause of disruption of the LCL complex. , However, chronic varus load and steroid injections for epicondylitis have also been implicated as causes of LCL insufficiency. , After trauma has occurred, restoration of lateral soft tissue support can usually be accomplished by a direct repair of the lateral ligament and extensor tendon origins to the humeral epicondyle. In instances of recurrent dislocation or subluxation, temporally remote from the initial injury, a tendon graft may be needed.
Chronic Lateral Instability
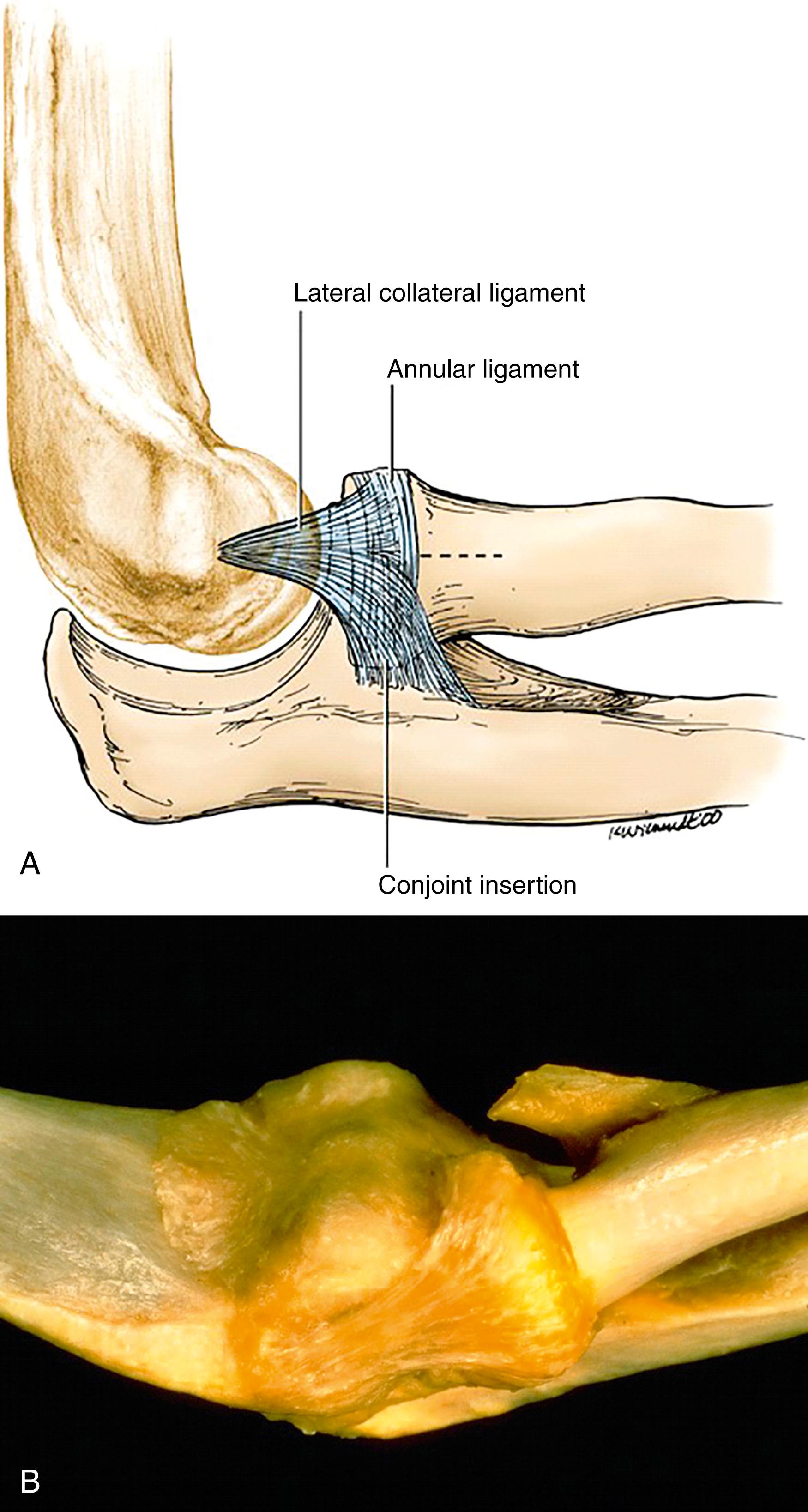
The LCL complex originates at the base of the lateral epicondyle and lateral aspect of the capitellum. The isometric origin of the LCL is located at the geometric center of the capitellum. In a perfect lateral radiograph of the elbow, the isometric origin can be localized at the intersection of a distal projection of the anterior cortex of the humerus and the longitudinal axis of the radius. Distally, the LCL blends with the annular ligament while its posterior fibers form a broad common insertion onto the proximal ulna ( Fig. 23.1 ). , The posterior fibers, which insert along the supinator crest, beginning at the proximal border of the radial head and extending 2 cm distally, are referred to as the lateral ulnar collateral ligament . The LCL complex is partly covered anteriorly by the supinator muscle, which originates off the lateral epicondyle, supinator crest, and annular ligament. Posteriorly, the anconeus muscle is in close proximity to the LCL complex as it originates off the lateral epicondyle and inserts onto the posterolateral aspect of the proximal ulna.
Both ligamentous and musculotendinous restraints provide stability to the elbow. The LCL complex, along with the anterior bundle of the medial collateral ligament (MCL), are the primary stabilizers of the elbow. Clinically, lateral elbow instability requires insufficiency of both ligamentous and musculotendinous stabilizers. The most common mechanism involves attenuation or avulsion of these structures from their humeral origins. , Occasionally, the ulnar insertion of the lateral ulnar collateral ligament may become compromised, either as an avulsion injury or as a fracture of the supinator crest. ,
The contribution of the LCL complex and overlying extensor tendon origins to lateral elbow joint stability have been well described in ex vivo studies. , The LCL complex represents the primary lateral stabilizer of the elbow, maintaining the ulnohumeral and radiocapitellar joints in a reduced position when the elbow is axially loaded with the forearm in supination. The extensor muscles, along with their fascial bands and intermuscular septae, assume a role as secondary restraints. In supination, the extensor muscles provide a static and dynamic force to support the lateral elbow. The extensor carpi ulnaris originates on the lateral epicondyle and the posterior border of the ulna, and thus has the best mechanical advantage to support the proximal forearm. Its origin is reinforced with a fascial band on its undersurface, inserting onto the ulna approximately 5 cm distal to the radial head. This fascial band becomes taut in supination and, along with the extensor tendon origins and septae, provides secondary resistance to lateral rotatory instability.
Disruption of the LCL complex occurs in most instances during elbow dislocation. Although more than one pattern exists, dislocations frequently occur as the elbow is loaded with a combination of axial compressive, external rotatory, and valgus forces, in which the body internally rotates with respect to the affected extremity. , , In this setting, disruption of elbow stabilizers proceeds in a circular path from lateral to medial. A recent study of 62 video recordings of acute elbow dislocations suggests that most dislocations occur to the extended elbow when the forearm is planted in pronation and the shoulder is abducted and forward flexed. The most common dislocating forces were abduction, axial load, and supination. Less frequently, dislocation may result as a consequence of a varus-deforming force applied to the extended elbow.
Chronic LCL insufficiency varies in its presentation. A patient may report a painful clunking and/or snapping of the elbow. Others will describe apprehension or weakness when reaching for an object with an outstretched hand, in varus load. Some may have episodes of frank giving way or apprehension, especially when the elbow is axially loaded in extension and supination. This can occur, for example, when one is pushing up from a chair. In this setting, the supinated radius and proximal ulna rotate laterally off of the distal humerus in a pattern termed posterolateral rotatory instability (PLRI). Occasionally, unremitting lateral elbow pain is the patient’s chief complaint. LCL insufficiency should be considered in patients with nonremitting lateral epicondylitis, with or without a history of previous local steroid injections. Patients with chronic cubitus varus deformity, a prior history of failed surgery for lateral epicondylitis, or prior surgery of the radial head may have underlying iatrogenic lateral elbow instability. ,
Physical examination in patients with chronic PLRI is characteristically unremarkable. Grip strength and range of motion are usually unaffected, although some extension deficit may be present. In the setting of chronic instability, minor discomfort may be present on palpation of the lateral elbow. Occasionally, a synovial fistula can be observed as a fluid collection about the lateral elbow.
Due to apprehension and guarding in an awake patient, it is often difficult to elicit frank posterolateral instability, especially in muscular individuals. Subluxation of the elbow can be appreciated, however, with the appropriate provocative maneuvers. The elbow should be examined with the patient sitting or lying supine on a table. In the sitting position, one hand stabilizes the adducted humerus, with the fingers placed along the lateral ulnohumeral joint line. While the elbow is flexed 40 to 45 degrees, the examiner’s contralateral hand loads the proximal forearm in supination with slight axial and valgus force applied. Instability is appreciated as gapping at the ulnohumeral articulation as the radius and ulna rotate posteriorly in relation to the humerus. This results in a posterolateral prominence as the radial head subluxates away from the capitellum. The ulnohumeral articulation can be reduced by pronation of the forearm and slight flexion of the joint. Reduction is occasionally accompanied by a palpable clunk.
Alternatively, the posterolateral rotatory apprehension (pivot shift) and drawer tests are performed with the patient in the supine position. The patient’s arm is brought overhead while the examiner stands at the head of the patient. By maximally flexing and externally rotating the shoulder, the humerus is “locked” into a fixed position. For the pivot shift test , the forearm is held in maximal supination while a valgus moment and axial compression is applied through the elbow at 40 to 70 degrees of flexion. In the relaxed patient with PLRI, this maneuver will lead to dimpling of the skin overlying the radiocapitellar joint, which occurs when the ulna and radius rotate off the distal humerus. The subluxated elbow is reduced with flexion, frequently causing a palpable and visible (and sometimes audible) clunk. The posterolateral rotatory drawer test is performed in the same position. A posteriorly directed force is applied onto the proximal radius while holding the forearm and elbow in the same position as for the apprehension test. Dimpling of the skin around the radiocapitellar joint at 40 to 70 degrees of flexion confirms PLRI. The amount of instability should decrease with greater elbow flexion.
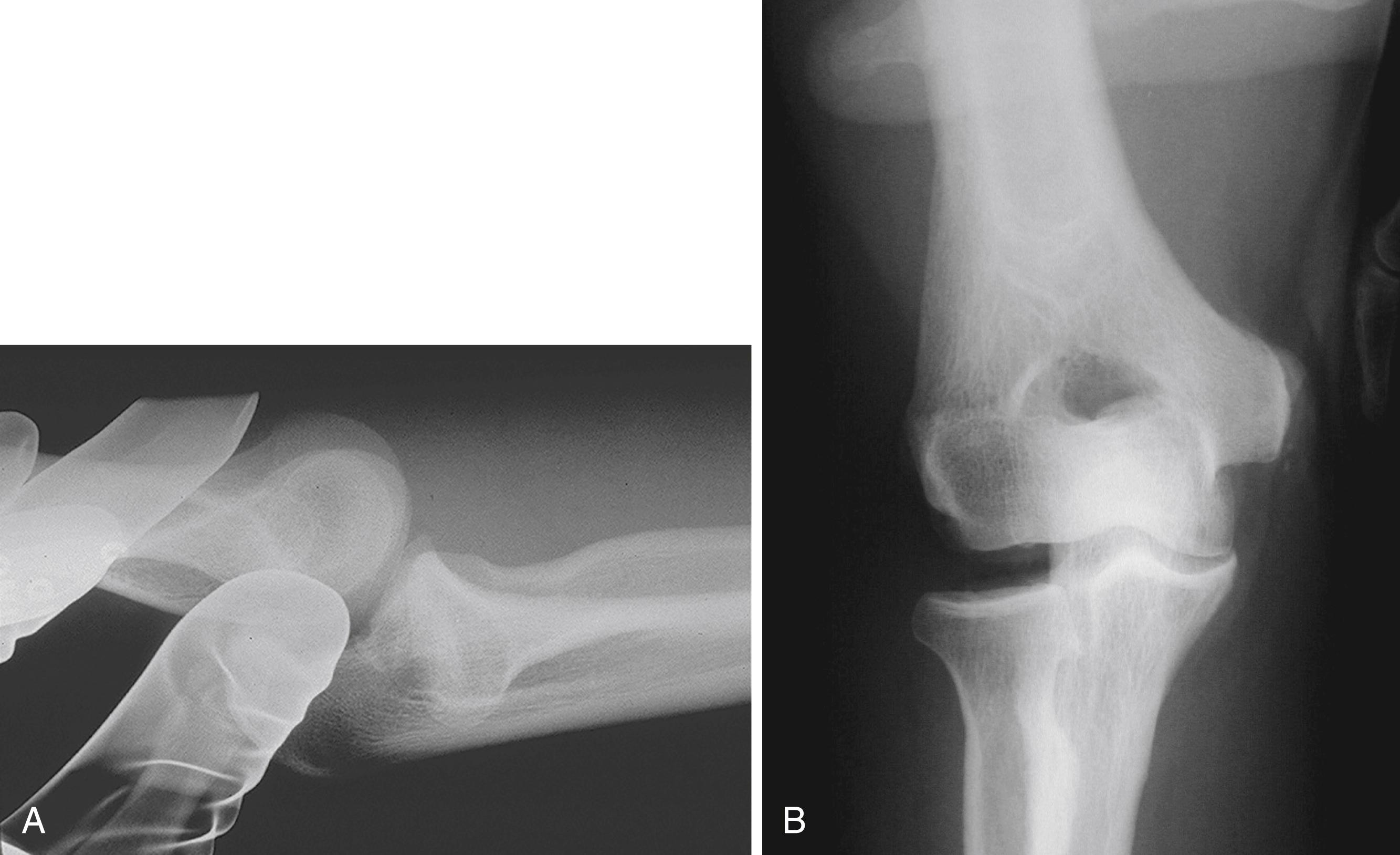
In addition, we routinely examine patients with suspected PLRI under image intensification. The clinical suspicion can in many cases be confirmed radiographically, aiding in establishing an appropriate treatment plan. In addition to the aforementioned rotatory tests, the extended elbow can be simply loaded in varus. Pathologic gapping at the radiocapitellar joint confirms lateral instability. This should be compared with the contralateral, unaffected side ( Fig. 23.2B ).
Patients with PLRI characteristically actively resist provocative maneuvers that stress the joint, which in and of itself can be interpreted as a “positive apprehension sign.” However, in the cooperative patient, a successful examination can be performed with careful manipulation. As one would expect, the most reliable examination is performed under anesthesia. The recommendation is to always perform these maneuvers as the first step in evaluation of a patient for surgical reconstruction. It is also advisable to include these examination maneuvers prior to elective surgery for lateral epicondylitis, especially after multiple injections have been administered. ,
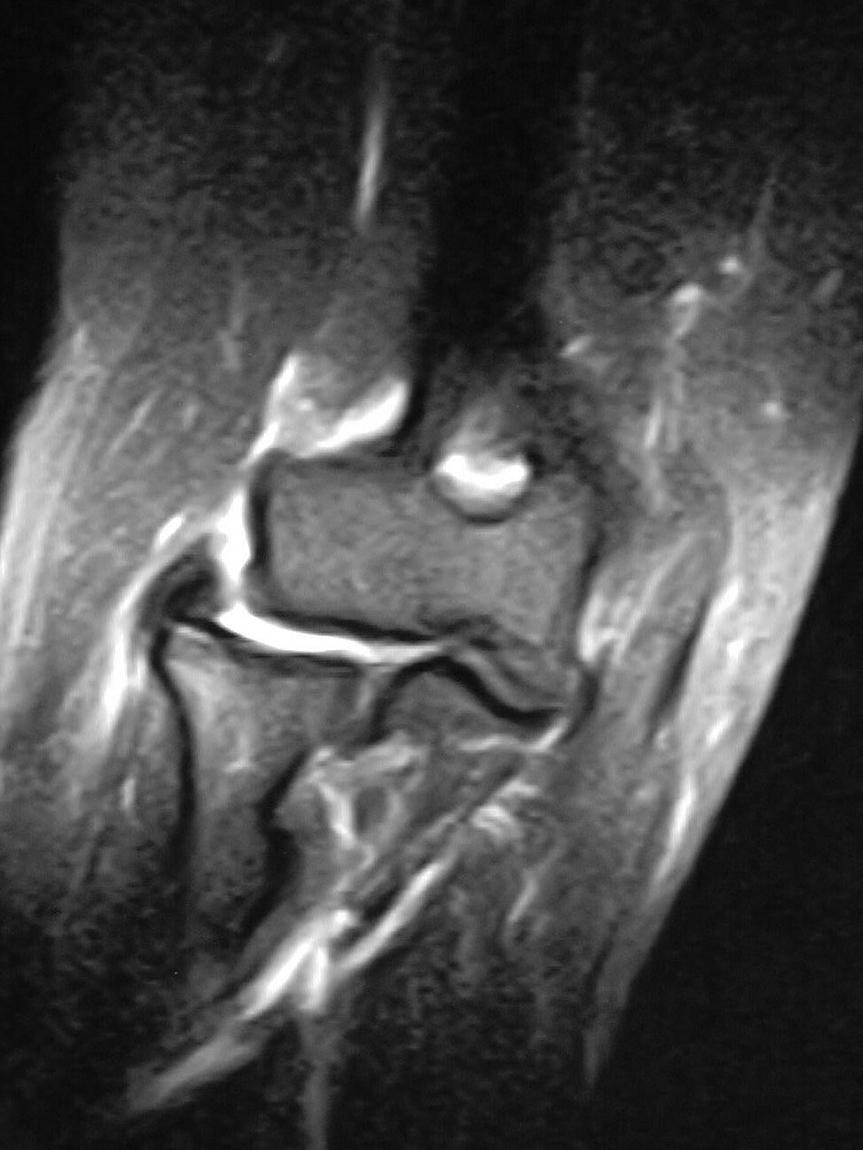
Plain radiographs of the elbow are frequently negative in patients with PLRI. However, small avulsion fragments or ossification at the humeral origin of the LCL can sometimes be visualized. If PLRI is suspected, posterolateral and varus stress examinations are obtained in the office using image intensification. The elbow is maximally supinated and axially loaded during valgus stress. Instability is confirmed by widening of the ulnohumeral joint and posterior subluxation of the radial head in the lateral projection ( Fig. 23.2A ). Anteroposterior radiographs or fluoroscopy under varus load can often reveal pathologic gapping of the radiocapitellar joint (see Fig. 23.2B ). Imaging of the contralateral elbow is recommended to help confirm asymmetric gapping or displacement. Magnetic resonance imaging (MRI) can aid in confirming the diagnosis by demonstrating signal changes at the epicondyle and disruption of the LCL and extensor tendinous origins from the lateral epicondyle ( Fig. 23.3 ).
Primary repair of the LCL is required in the setting of fracture-dislocations of the elbow. The so-called terrible triad of the elbow indicates a fracture of the coronoid process and radial head, with elbow dislocation. In this setting, the LCL is usually disrupted, and repair is an integral part of the treatment algorithm. In chronic PLRI of the elbow, some authors have shown favorable outcomes with simple repair of the LCL complex, but reconstruction is typically required to restore lateral joint stability.
LCL repair or reconstruction requires an intact buttress at the radiocapitellar joint. In cases of radial head insufficiency, operative reduction and fixation of the radial head or prosthetic replacement should accompany the reconstruction. Patient compliance with postoperative rehabilitation plays a key role in achieving adequate outcomes. Patients who are unable or unwilling to follow rehabilitation guidelines should not undergo reconstruction, especially as an elective procedure.
Almost universally, the surgical techniques described for the management of PLRI involve a free tendon graft as originally reported by Nestor et al. Their technique utilizes a free graft passed through a lateral ulnar tunnel, positioned over the tubercle of the supinator crest. Once the tendon is passed through the ulna, the graft ends are threaded through the humerus. The humeral tunnel begins slightly proximal and posterior to the point of isometry. The graft arms are then passed out divergent proximal exit holes on the anterior and posterior aspects of the lateral humeral column and tied to one another. Most recently, Daluiski and colleagues compared outcomes of two cohorts of patients treated with primary repair of the LCL complex: one within 30 days of injury and the other 30 or more days after dislocation; the results were similar. Their technique involves placing a large, nonabsorbable suture in a running locking fashion through the tendon and ligament origins. The entire soft tissue sleeve is then advanced to the humerus using a modified docking technique, with a drill hole, a suture anchor, or a combination of both. These authors recommend that the tissue origin be attached just anterior to the isometric point to improve elbow stability.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here