Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The contributions to this chapter by Dr. Matthew P. Frosch, Department of Pathology, Massachusetts General Hospital, Harvard Medical School, Boston Massachusetts, and Dr. Robert Folberg in several previous editions of this book are gratefully acknowledged.
The principal focus of this chapter is on diseases of the central nervous system (CNS). At the end, we briefly describe some important disorders of the eye, which is linked anatomically and functionally to the CNS.
Disorders of the CNS are some of the most serious diseases of humankind. These diseases have many unique features that reflect the highly specialized structure and functions of the CNS. The principal functional unit of the CNS is the neuron (gray matter). Neurons of different types and in different locations have distinct properties, including functional roles, distribution of their connections, neurotransmitters used, metabolic requirements, and levels of electrical activity at a given moment. A population of neurons may show selective vulnerability to various insults because it shares one or more of these properties. Since different regions of the brain participate in different functions, the pattern of clinical signs and symptoms that follow injury depend both on the region of brain involved and the pathologic process. Mature neurons are incapable of cell division, so destruction of even a small number of neurons essential for a specific function may cause a neurologic deficit. In addition to neurons the CNS contains other cells, such as astrocytes and oligodendrocytes, which make up the glia (white matter). The components of the CNS are affected by a number of unique neurologic disorders and also respond to common insults (e.g., ischemia, infection) in a manner that is distinct from other tissues.
Before delving into specific disorders, we briefly review the characteristic morphologic changes that are often seen in the CNS in the setting of injury or infection.
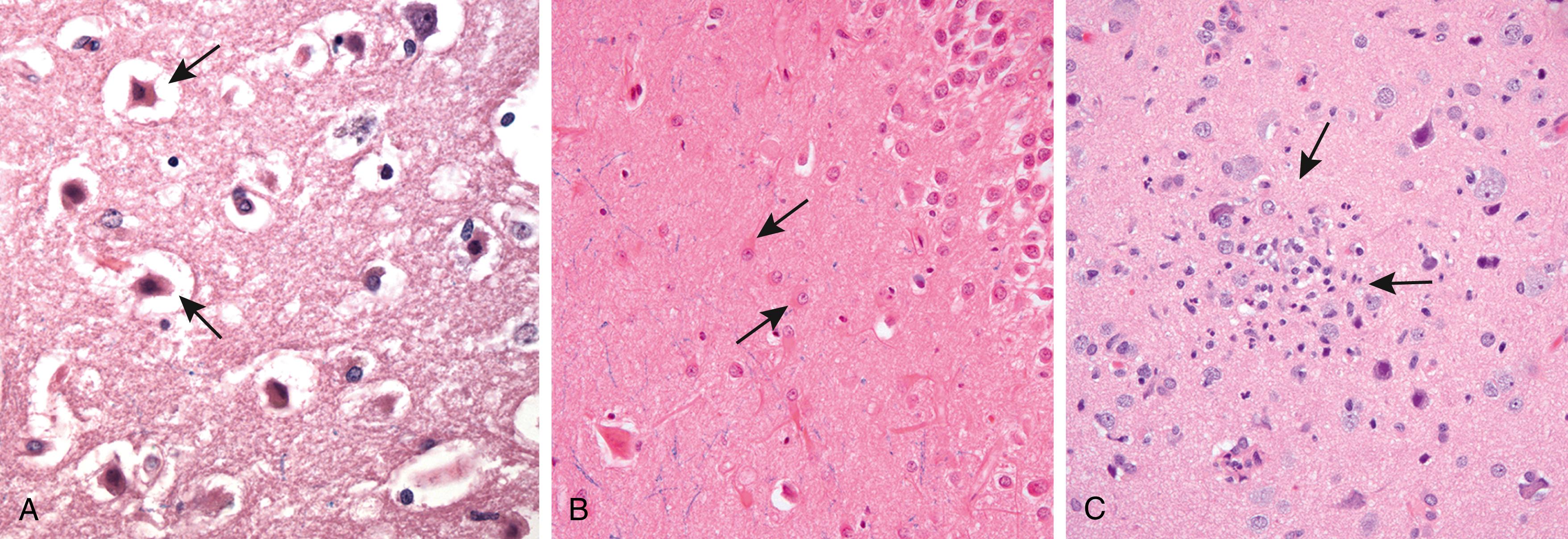
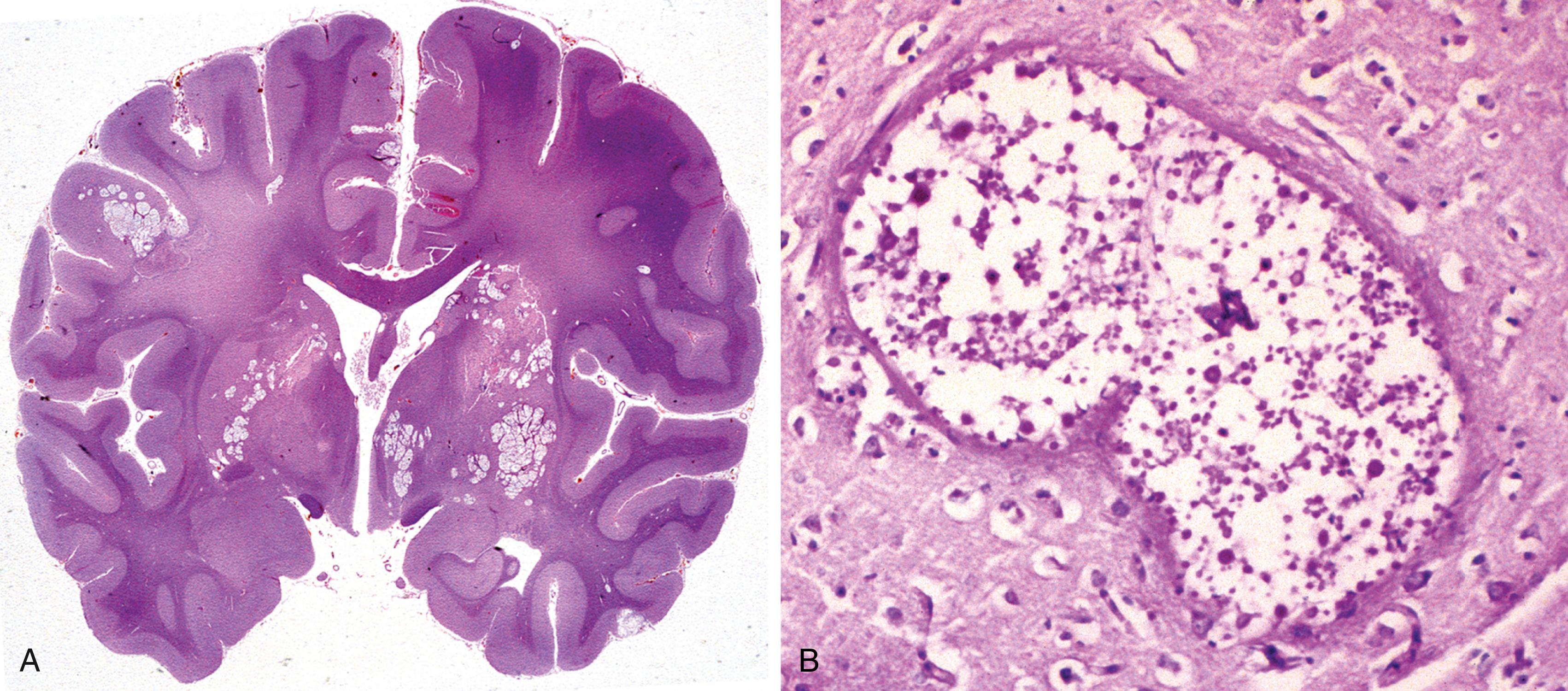
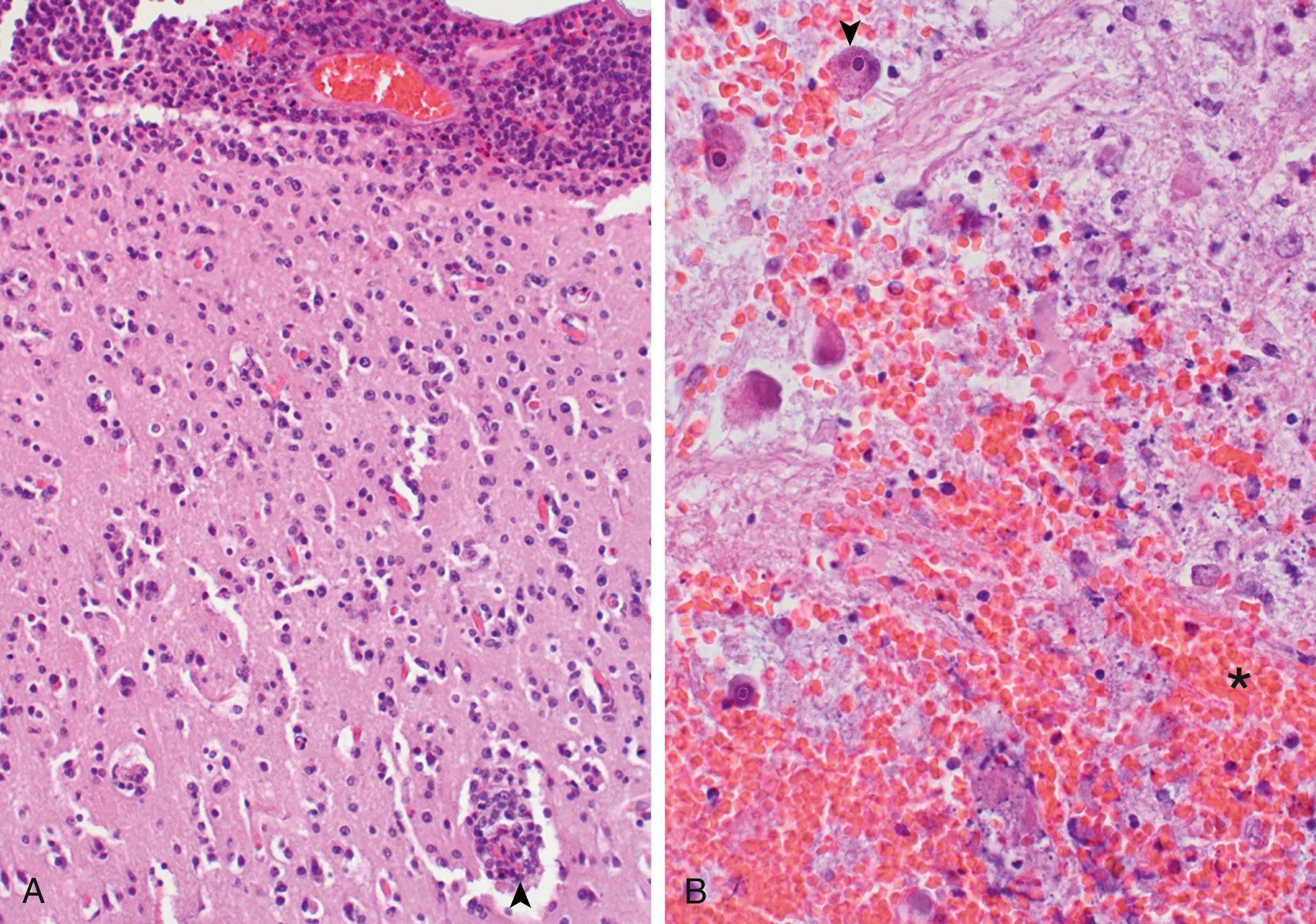
Features of Neuronal Injury. In response to injury, a number of changes occur in neurons and their processes (axons and dendrites). Within 12 hours of an irreversible hypoxic-ischemic insult, neuronal injury becomes evident on routine hematoxylin and eosin (H&E) staining ( Fig. 21.1 A ). There is shrinkage of the cell body, pyknosis of the nucleus, disappearance of the nucleolus, loss of cytoplasmic rough endoplasmic reticulum staining (referred to as Nissl substance in neurons), and intense eosinophilia of the cytoplasm (red neurons) . Axonal injury also leads to cell body enlargement and rounding, peripheral displacement of the nucleus, enlargement of the nucleolus, and peripheral dispersion of Nissl substance (central chromatolysis) . In addition, acute injuries typically result in breakdown of the blood-brain barrier and variable degrees of cerebral edema (discussed later).
Many neurodegenerative diseases are associated with accumulation of abnormal proteins (e.g., amyloid plaques in Alzheimer disease) or specific intracellular inclusions (e.g., Lewy bodies in Parkinson disease). Pathogenic viruses may form inclusions in infected neurons, just as in other cells, and such inclusions aid in the diagnosis. In some neurodegenerative diseases, neuronal processes become thickened and tortuous; these are termed dystrophic neurites.
Astrocyte Injury and Repair. Astrocytes are the principal cells responsible for repair and scar formation in the brain, a process termed gliosis. In response to injury, astrocytes undergo both hypertrophy and hyperplasia. The nucleus enlarges and becomes vesicular, and the nucleolus becomes prominent. The cytoplasm expands and takes on a bright pink hue, and the cell extends multiple stout, ramifying processes ( gemistocytic astrocyte; Fig. 21.1 B). In contrast to elsewhere in the body, fibroblasts do not contribute to healing after brain injury except in specific settings (e.g., penetrating brain trauma or around abscesses). In long-standing gliosis, the cytoplasm of reactive astrocytes shrinks in size, and the cellular processes become more tightly interwoven (fibrillary astrocytes). Rosenthal fibers are thick, elongated, brightly eosinophilic protein aggregates found in astrocytic processes in chronic gliosis and in some low-grade gliomas.
Oligodendrocytes, which produce myelin, exhibit a limited spectrum of specific morphologic changes in response to various injuries, such as the intranuclear viral inclusions seen in progressive multifocal leukoencephalopathy.
Microglial cells are long-lived cells derived from the embryonic yolk sac that function as the resident phagocytes of the CNS. When activated by tissue injury, infection, or trauma, they proliferate and become more prominent histologically. In areas of demyelination, organizing infarct, or hemorrhage, microglial cells resemble activated macrophages; in other settings such as infections, they develop elongated nuclei (rod cells) . Aggregates of elongated microglial cells at sites of tissue injury are termed microglial nodules ( Fig. 21.1 C). Similar collections can be found congregating around and phagocytosing injured neurons (neuronophagia).
Ependymal cells line the ventricular system and the central canal of the spinal cord. Certain pathogens, particularly cytomegalovirus (CMV), can produce extensive ependymal injury, with typical viral inclusions. Choroid plexus is in continuity with the ependyma, and its specialized epithelial covering is responsible for the secretion of cerebrospinal fluid (CSF).
Clinical evaluation of neurologic diseases often relies on localizing signs (e.g., contralateral weakness after occlusion of a cerebral artery), which indicate the site of the abnormality, and nonlocalizing signs (e.g., altered mental status), which indicate the presence of a neurologic disorder but not its site.
The brain and spinal cord are encased within the skull and spinal canal, with nerves and blood vessels passing through different foramina. Housing the delicate CNS within hard, rigid structures provides protection but leaves little room for expansion of the brain or its surrounding fluid in disease states. As a result, virtually any expansion of skull contents brings with it an increase in intracranial pressure. Substantial increases in intracranial pressure compromise the ability of the cardiovascular system to deliver blood to the brain, resulting in decreased brain perfusion, with serious or fatal consequences. Disorders that may cause dangerous increases in intracranial contents include generalized cerebral edema, hydrocephalus, hemorrhage, ischemia, and mass lesions such as tumors.
Cerebral edema is the accumulation of excess fluid within the brain parenchyma. There are two types, which often occur together, particularly after generalized injury.
Vasogenic edema occurs when the integrity of the blood-brain barrier is disrupted, allowing fluid to shift from the vascular compartment into the extracellular spaces of the brain. Vasogenic edema can be localized (e.g., the result of increased vascular permeability due to inflammation or a tumor) or generalized.
Cytotoxic edema is an increase in intracellular fluid secondary to neuronal and glial cell injury, as might follow a generalized hypoxic or ischemic insult or exposure to certain toxins.
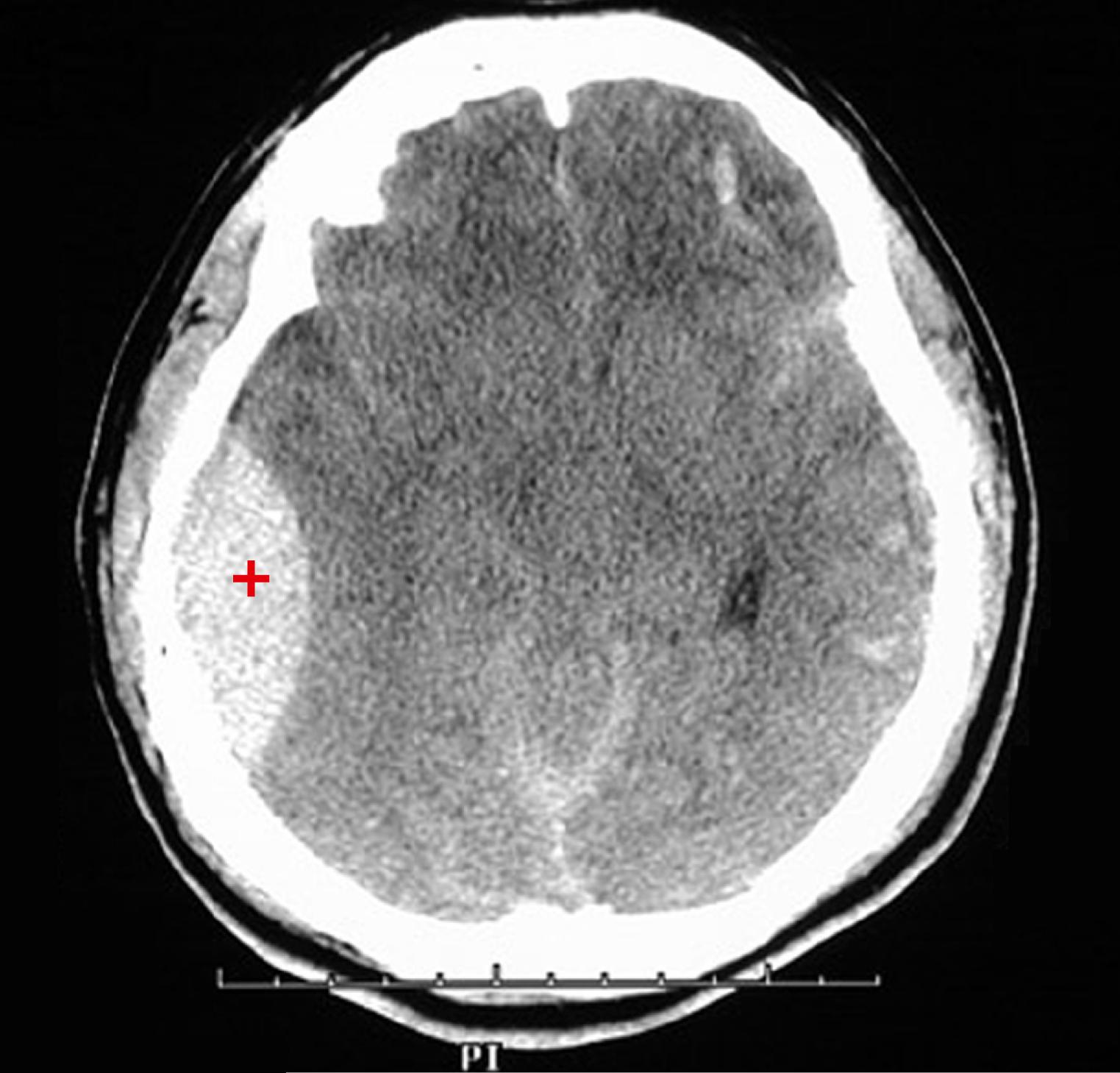
The edematous brain is softer than normal and often appears to fill the cranial vault. In generalized edema, the gyri are flattened, the intervening sulci are narrowed, and the ventricular cavities are compressed ( Fig. 21.2 ).

CSF is produced by the choroid plexus within the ventricles, then circulates through the ventricular system and flows through the foramina of Luschka and Magendie into the subarachnoid space, where it is absorbed by arachnoid granulations. The balance between rates of generation and resorption regulates CSF volume.
Hydrocephalus is increase in the volume of the CSF within the ventricular system. Most often, this disorder is a consequence of impaired flow or decreased resorption of CSF. If there is a localized obstacle to CSF flow within the ventricular system, then a portion of the ventricles enlarge while the remainder do not. This pattern is referred to as noncommunicating hydrocephalus and is most commonly caused by masses (e.g., tumor, hemorrhage, or infection) obstructing the foramen of Monro or compressing the cerebral aqueduct. In communicating hydrocephalus, the entire ventricular system is enlarged, usually secondary to reduced CSF resorption, for unknown reasons.
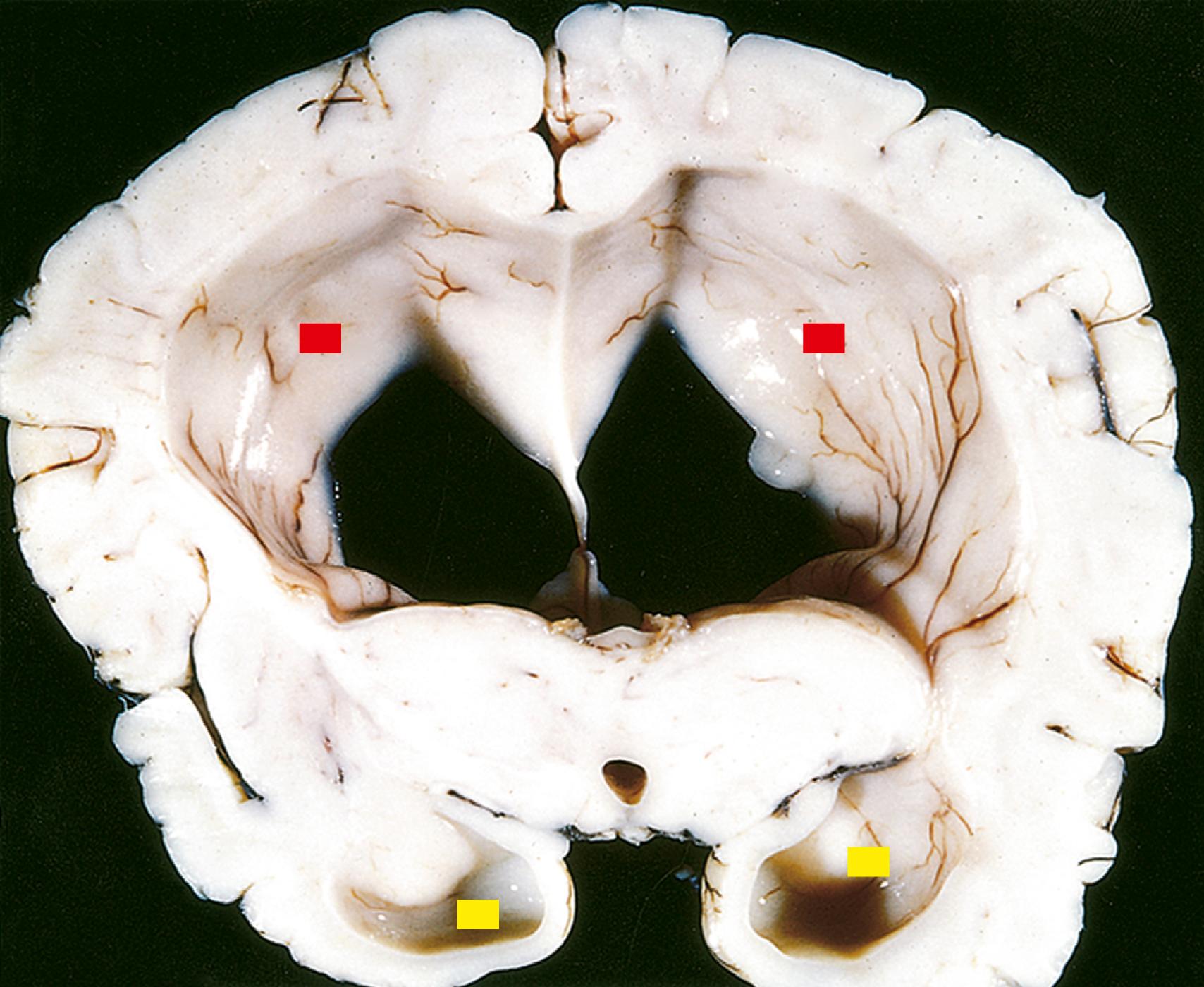
When hydrocephalus develops in infancy before closure of the cranial sutures, the head enlarges. Once the sutures fuse, hydrocephalus causes ventricular expansion and increased intracranial pressure, but no change in head circumference ( Fig. 21.3 ). In contrast to these disorders, in which increased CSF volume is the primary process, a compensatory increase in CSF volume (hydrocephalus ex vacuo) may occur secondary to a loss of brain volume from any underlying cause (e.g., infarction, neurodegenerative disease).
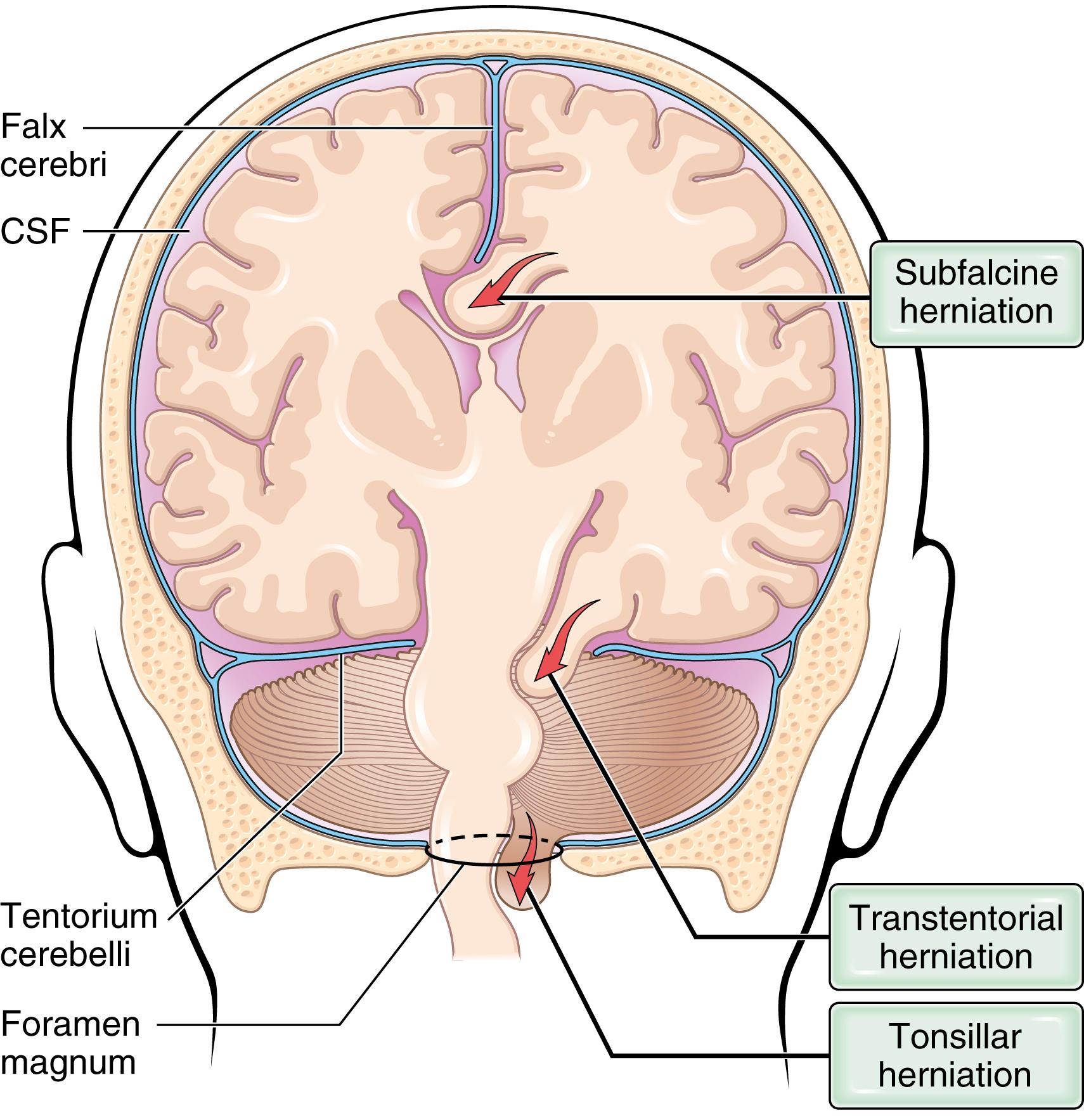
Herniation is the displacement of brain tissue past rigid dural folds (the falx and tentorium) or through openings in the skull because of increased intracranial pressure. The brain herniates when its limited capacity to accommodate the increased pressure is exceeded. Brain herniation is most often caused by mass effects, either diffuse (generalized brain edema) or focal (tumors, abscesses, or hemorrhages). Elevated intracranial pressure may also compress the vasculature and reduce perfusion of the brain, causing ischemic injury and further exacerbating cerebral edema.
The brain may herniate through different openings, and if the expansion is sufficiently severe, herniation may occur simultaneously in several locations ( Fig. 21.4 ):
Subfalcine (cingulate) herniation occurs when unilateral or asymmetric expansion of a cerebral hemisphere displaces the cingulate gyrus under the edge of the falx. This may compress the anterior cerebral artery resulting in contralateral leg weakness, or aphasia if the herniation affects the dominant hemisphere.
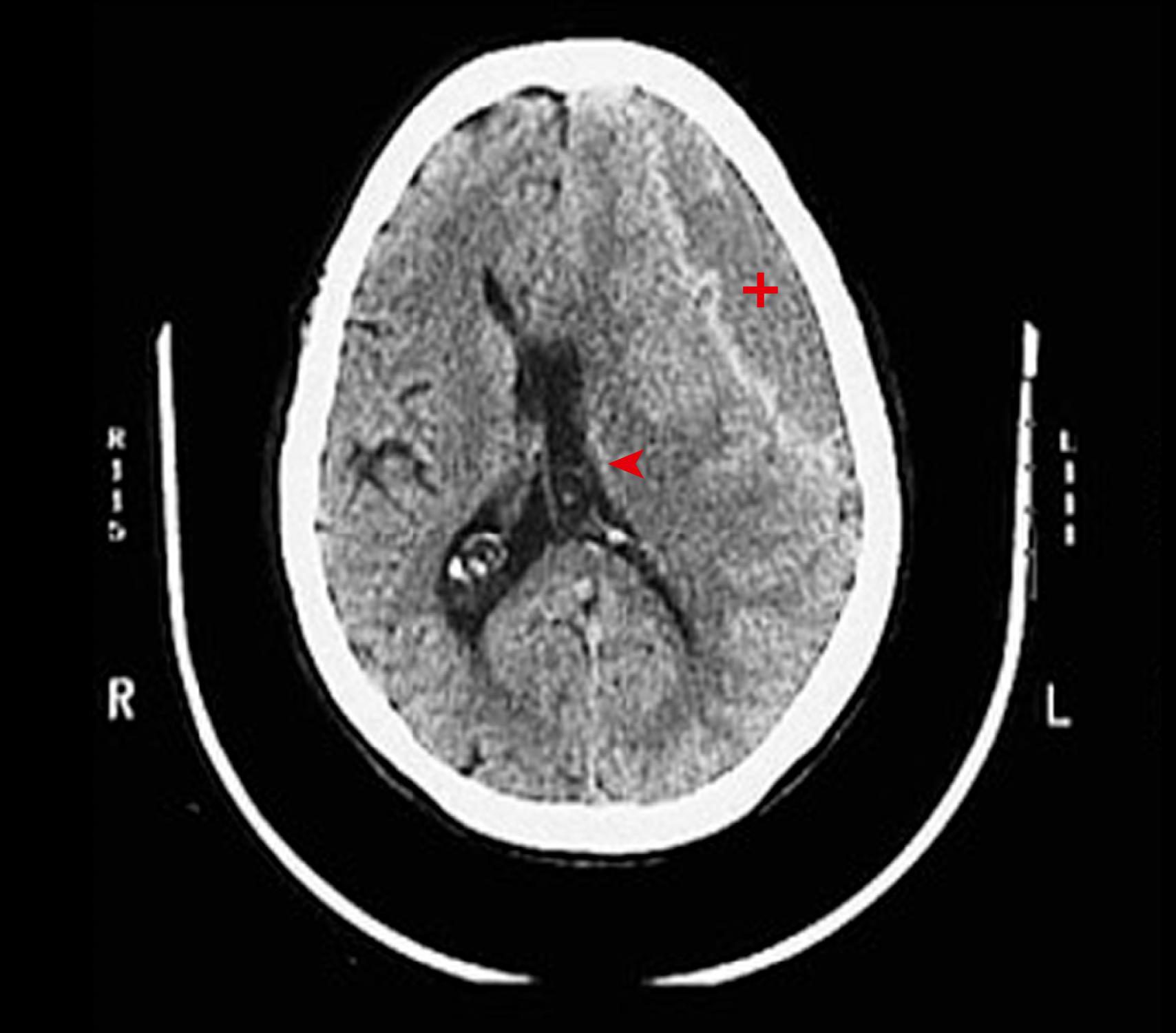
Transtentorial (uncinate) herniation occurs when the medial aspect of the temporal lobe is compressed against the free margin of the tentorium. As the temporal lobe is displaced, the third cranial nerve is compromised, resulting in pupillary dilation and impaired ocular movements on the side of the lesion (“blown pupil”). The posterior cerebral artery may also be compressed, resulting in ischemic injury to tissue supplied by that vessel, including the primary visual cortex. With further displacement of the temporal lobe, pressure on the midbrain may compress the contralateral cerebral peduncle against the tentorium, resulting in hemiparesis ipsilateral to the side of the herniation. The compression of the peduncle creates a deformation known as Kernohan’s notch. Compression of the midbrain and the ascending reticular activating system with transtentorial herniation leads to depressed consciousness. Progression of transtentorial herniation is often accompanied by linear or flame-shaped hemorrhages in the midbrain and pons, termed Duret hemorrhages ( Fig. 21.5 ). These lesions usually occur in the midline and paramedian regions and are believed to be the result of tearing of penetrating veins and arteries supplying the upper brain stem.
Tonsillar herniation refers to displacement of the cerebellar tonsils through the foramen magnum. This type of herniation causes brain stem compression and compromises vital respiratory and cardiac centers in the medulla and is often rapidly fatal.
The incidence of CNS malformations, giving rise to mental disability, cerebral palsy, or neural tube defects, is estimated at 1% to 2% of pregnancies. Malformations of the brain are more common in the setting of multiple anomalies. Mutations affecting genes that regulate the differentiation, maturation, or intercellular communication of neurons or glial cells can cause CNS malformation or dysfunction. Prenatal or perinatal insults, including various chemicals and infectious agents, may interfere with normal CNS development or cause tissue damage. During gestation, the timing of an injury determines the pattern of malformation, with earlier events typically leading to more severe phenotypes.
Neural tube defects are midline malformations that involve some combination of neural tissue, meninges, and overlying bone or soft tissue; collectively, they are the most common CNS malformations. Two distinct pathogenic mechanisms are contributory: (1) failure of neural tube closure, in which secondary mesenchymal tissue defects stem from aberrant skeletal modeling around the malformed tube (e.g., anencephaly and myelomeningocele), and (2) primary bony defects that are caused by abnormal axial mesoderm development and lead to secondary CNS abnormalities (e.g., encephalocele, meningocele, and spina bifida). Folate deficiency during the first trimester increases risk through uncertain mechanisms and represents an important opportunity for prevention, as folate supplements in women of child-bearing age reduce the incidence of neural tube defects by up to 70%. Serum α-fetoprotein (AFP) is elevated in the setting of neural tube defects; maternal screening for AFP combined with imaging studies has increased the early detection of neural tube defects.
The most common defects involve the posterior end of the neural tube, from which the spinal cord forms. These can range from asymptomatic bony defects (spina bifida occulta) to spina bifida , a severe malformation consisting of a flat, disorganized segment of spinal cord associated with an overlying meningeal outpouching.
Myelomeningocele is an extension of CNS tissue through a defect in the vertebral column that occurs most commonly in the lumbosacral region ( Fig. 21.6 ). Patients have motor and sensory deficits in the lower extremities and problems with bowel and bladder control. The clinical problems derive from the abnormal spinal cord segment and often are compounded by infections due to defects in the thin overlying skin, which is prone to ulceration.

Anencephaly is a malformation of the anterior end of the neural tube that leads to the absence of the forebrain and the top of the skull. Varying amounts of posterior fossa structures may be present.
An encephalocele is a diverticulum of malformed CNS tissue extending through a defect in the cranium. It most often involves the occipital region or the posterior fossa. When it occurs anteriorly, brain tissue may extend into the sinuses.
Microencephaly describes the group of malformations in which the volume of brain is abnormally small; usually it is associated with a small head as well (microcephaly). There are a wide range of associations, including chromosome abnormalities, fetal alcohol syndrome, and in utero infection by human immunodeficiency virus (HIV) and Zika virus. The underlying mechanism is decreased generation of neurons destined for the cerebral cortex. During the early stages of brain development, as progenitor cells proliferate in the subependymal ventricular zone, the balance between cells leaving the progenitor population to form the cortex and those remaining in the proliferating pool affects the overall number of neurons and glial cells generated. If too many cells leave the progenitor pool prematurely, there is inadequate generation of mature neurons, leading to a small brain. Disruption of neuronal migration and differentiation during development can lead to abnormalities of gyration and neocortical architecture, with neurons often ending up in the wrong location. Mutations in various genes that control migration result in a variety of malformations. A representative example is holoprosencephaly, characterized by disruption of normal midline patterning. Mild forms show absence of the olfactory bulbs and related structures (arrhinencephaly). In severe forms, the brain is not divided into hemispheres or lobes, and there may be facial midline defects such as cyclopia. The best known genetic causes involve inherited loss-of-function mutations in components of the Hedgehog signaling pathway.
Other examples include loss of gyri, which may be complete (lissencephaly) or partial, and increased number of irregularly formed gyri (polymicrogyria).
The most common malformations in this region of the brain result in misplacement or absence of portions of the cerebellum.
Arnold-Chiari malformation (Chiari type II malformation) combines a small posterior fossa with a misshapen midline cerebellum and downward extension of the vermis through the foramen magnum; hydrocephalus and a lumbar myelomeningocele typically are also present.
The far milder Chiari type I malformation has low-lying cerebellar tonsils that extend through the foramen magnum. Excess tissue in the foramen magnum results in partial obstruction of CSF flow and compression of the medulla, with symptoms of headache or cranial nerve deficits often manifesting only in adult life. Surgical intervention can alleviate the symptoms.
Dandy-Walker malformation is characterized by an enlarged posterior fossa, absence of the cerebellar vermis, and a large midline cyst.
Several genetic diseases disrupt metabolic processes in neurons and glia, resulting in progressive disorders that present early in life. These diseases can be grouped based on the cells or compartment (e.g., neurons or white matter), organelles (e.g., lysosome, peroxisome, or mitochondrion), or metabolites (e.g., sphingolipidoses, very long–chain fatty acids) that are affected. The mutations underlying these diseases typically disrupt synthetic or degradation pathways that are specific to the nervous system.
Neuronal storage diseases are characterized by the accumulation of storage material within neurons, typically resulting in neuronal death. Cortical neuronal involvement leads to loss of cognitive function and also may cause seizures. Most commonly, they are autosomal recessive disorders caused by the deficiency of a specific enzyme involved in the catabolism of sphingolipids (including the gangliosides), mucopolysaccharides, or mucolipids; others appear to be caused by defects in protein or lipid trafficking within neurons. Several examples of these diseases, such as Tay-Sachs and Niemann-Pick disease and mucopolysaccharidoses (all lysosomal storage disorders) are discussed in Chapter 4 .
Mitochondrial encephalomyopathies are disorders of oxidative phosphorylation, often affecting multiple tissues including skeletal muscle ( Chapter 20 ). When they involve the brain, gray matter is more severely affected than white matter due to the greater metabolic requirements of neurons. These disorders may be caused by mutations in mitochondrial or nuclear genes. They present with muscle weakness, seizures, and visual defects, alone or in combination.
Cerebrovascular diseases are brain disorders caused by pathologic processes involving blood vessels. They are a major cause of death and morbidity in high resource parts of the world. The three main pathogenic mechanisms are (1) thrombotic occlusion, (2) embolic occlusion, and (3) vascular rupture. Stroke is the clinical designation applied to all these conditions when symptoms begin acutely. Thrombosis and embolism have similar consequences for the brain: loss of oxygen and metabolic substrates, resulting in infarction or ischemic injury of regions supplied by the affected vessel. Similar injury occurs globally when there is complete loss of perfusion, severe hypoxemia (e.g., hypovolemic shock), or profound hypoglycemia. Hemorrhage accompanies rupture of vessels and leads to direct tissue damage as well as secondary ischemic injury. Traumatic vascular injury is discussed separately in the context of trauma.
The brain is a highly oxygen-dependent tissue that requires a continuous supply of glucose and oxygen from the blood. Although it constitutes no more than 2% of body weight, the brain receives 15% of the resting cardiac output and is responsible for 20% of total body oxygen consumption. Cerebral blood flow normally remains stable over a wide range of blood pressure and intracranial pressure because of autoregulation of vascular resistance. The brain may be deprived of oxygen by two general mechanisms:
Functional hypoxia, caused by a low partial pressure of oxygen (e.g., high altitude), impaired oxygen-carrying capacity (e.g., severe anemia, carbon monoxide poisoning), or toxins that interfere with oxygen use (e.g., cyanide poisoning)
Ischemia, either transient or permanent, due to tissue hypoperfusion, which can be caused by hypotension, vascular obstruction, or both
Global cerebral hypoxia or ischemia occurs when there is a generalized reduction of cerebral perfusion (as in cardiac arrest, shock, and severe hypotension) or decreased oxygen-carrying capacity of the blood (e.g., in carbon monoxide poisoning). The clinical outcome varies with the severity and duration of the insult. When the insult is mild, there may be only transient confusion followed by complete recovery. Neurons are more susceptible to hypoxic injury than are glial cells, and the most susceptible neurons are the pyramidal cells of the hippocampus and neocortex and Purkinje cells of the cerebellum. In some cases, even mild or transient global ischemic insults may cause damage to these vulnerable areas. In severe global cerebral ischemia, widespread neuronal death occurs irrespective of regional vulnerability. Patients who survive often remain severely impaired neurologically, sometimes in a persistent vegetative state. Other patients meet the clinical criteria for so-called “brain death,” in which all voluntary and reflex brain and brain stem function is absent, including respiratory drive. When patients with this form of irreversible injury are maintained on mechanical ventilation, the brain may gradually undergo autolysis.
In the setting of global ischemia, the brain is swollen, with wide gyri and narrowed sulci. The cut surface shows poor demarcation between gray matter and white matter. The histopathologic changes that accompany irreversible ischemic injury (infarction) are grouped into three categories. Early changes, occurring 12 to 24 hours after the insult, include acute neuronal cell change (red neurons) (see Fig. 21.1 A) characterized initially by microvacuolation, followed by cytoplasmic eosinophilia, and later nuclear pyknosis and karyorrhexis. Similar changes occur somewhat later in astrocytes and oligodendroglia. After this, the reaction to tissue damage begins with infiltration of neutrophils. Subacute changes, occurring at 24 hours to 2 weeks, include necrosis of tissue, influx of macrophages, vascular proliferation, and reactive gliosis. Repair, seen after 2 weeks, is characterized by removal of necrotic tissue and gliosis.
Cerebral arterial occlusion leads first to ischemia and then to infarction in the distribution of the compromised vessel. The size, location, and shape of the infarct and the extent of tissue damage that results may be modified by collateral blood flow. Specifically, collateral flow through the circle of Willis or cortical-leptomeningeal anastomoses can limit damage in some regions. By contrast, there is little if any collateral blood flow to structures such as the thalamus, basal ganglia, and deep white matter, which are supplied by deep penetrating vessels.
Infarctions caused by emboli are more common than infarctions due to thrombosis. Cardiac mural thrombi are a frequent source of emboli; myocardial dysfunction, valvular disease, and atrial fibrillation are important predisposing factors. Thromboemboli also arise in arteries, most often from atheromatous plaques in the carotid arteries or aortic arch. Emboli of venous origin may cross over to the arterial circulation through a patent foramen ovale and lodge in the brain (paradoxical embolism; see Chapter 9 ); these include thromboemboli from deep leg veins and fat emboli, usually following bone trauma. The territory of the middle cerebral artery, a direct extension of the internal carotid artery, is most frequently affected by embolic occlusion. Emboli tend to lodge where vessels branch or in areas of stenosis, usually caused by atherosclerosis.
Thrombotic occlusions causing cerebral infarctions are usually superimposed on atherosclerotic plaques; common sites are the carotid bifurcation, the origin of the middle cerebral artery, and either end of the basilar artery. These occlusions may be accompanied by anterograde extension, as well as thrombus fragmentation and distal embolization. Thrombotic occlusions causing small infarcts of only a few millimeters in diameter, so-called lacunar infarcts, occur when small penetrating arteries get occluded due to chronic damage, usually from long-standing hypertension (discussed later).
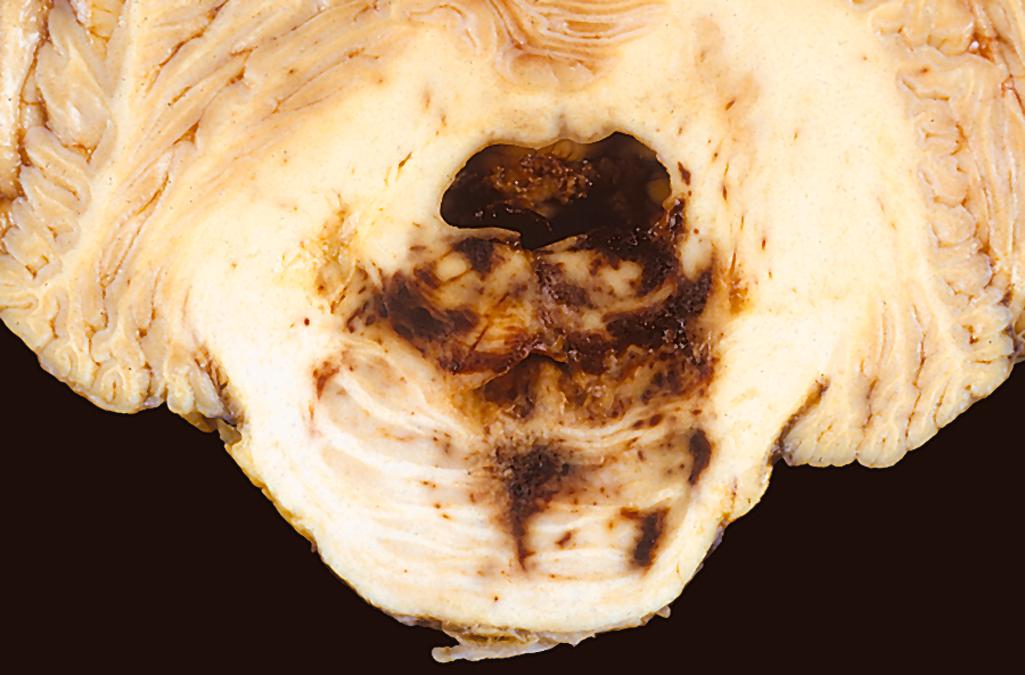
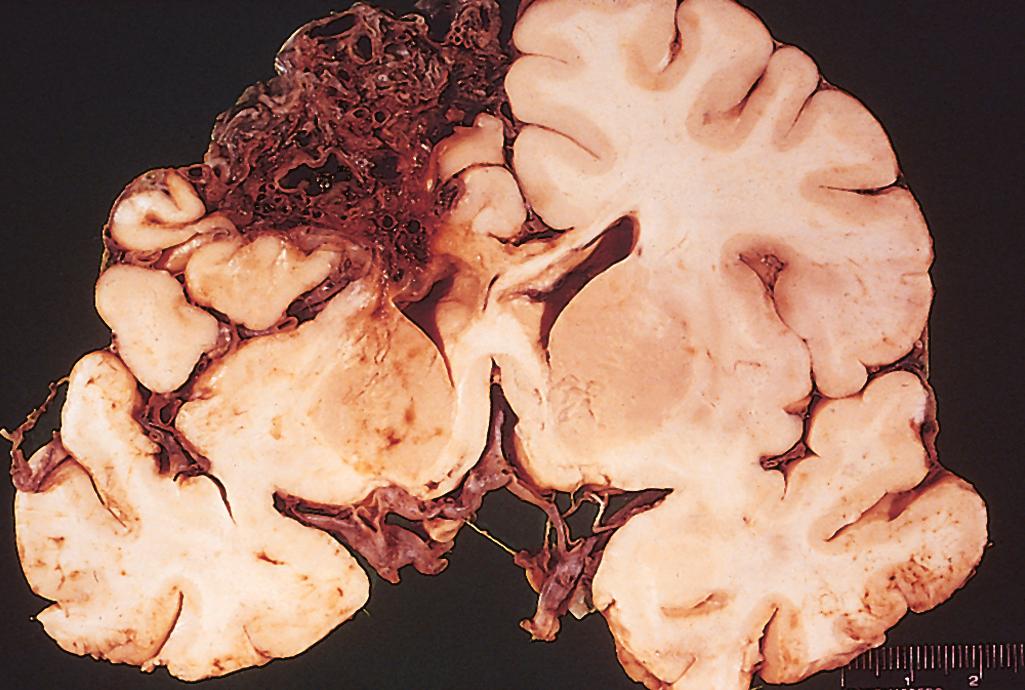
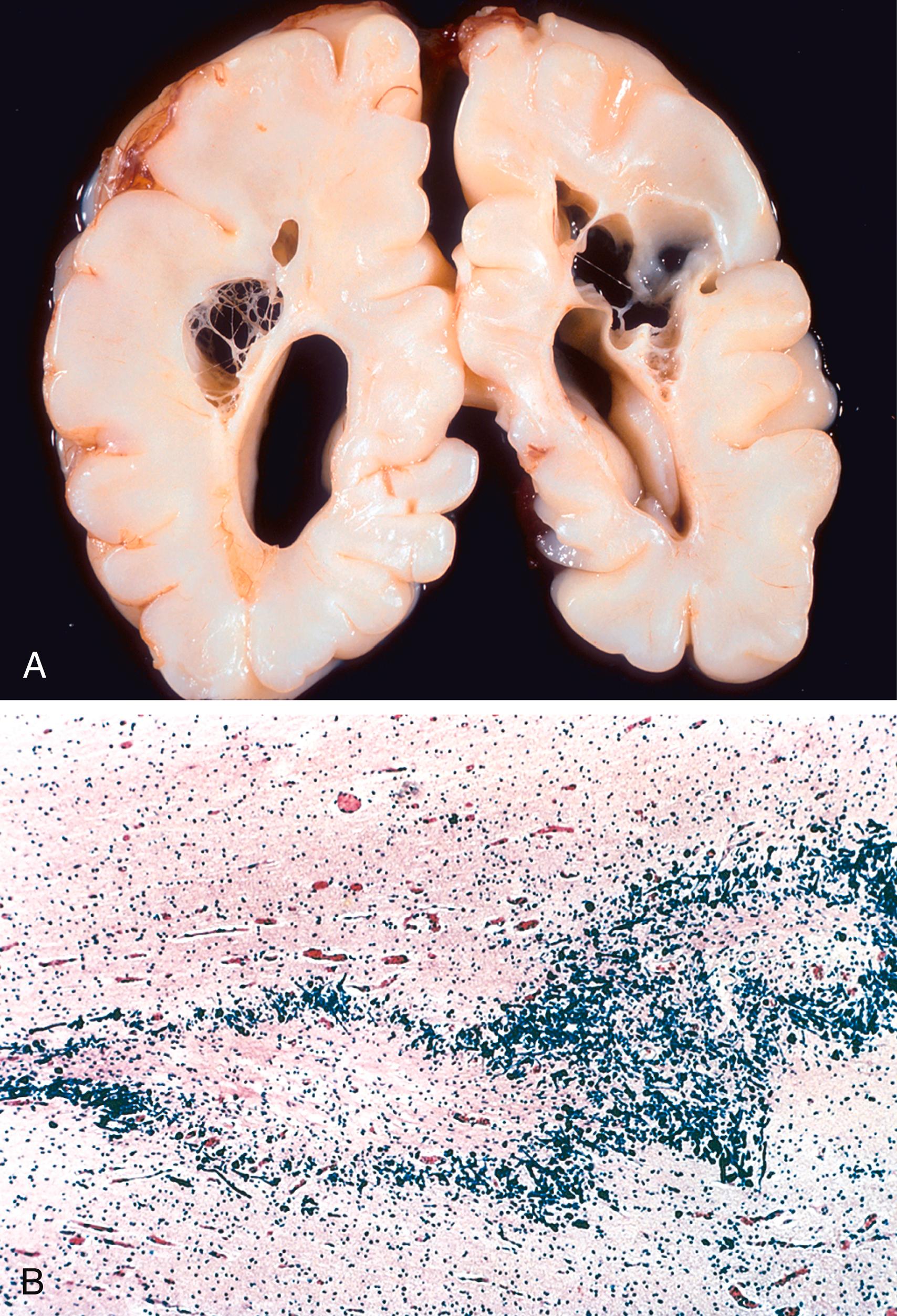
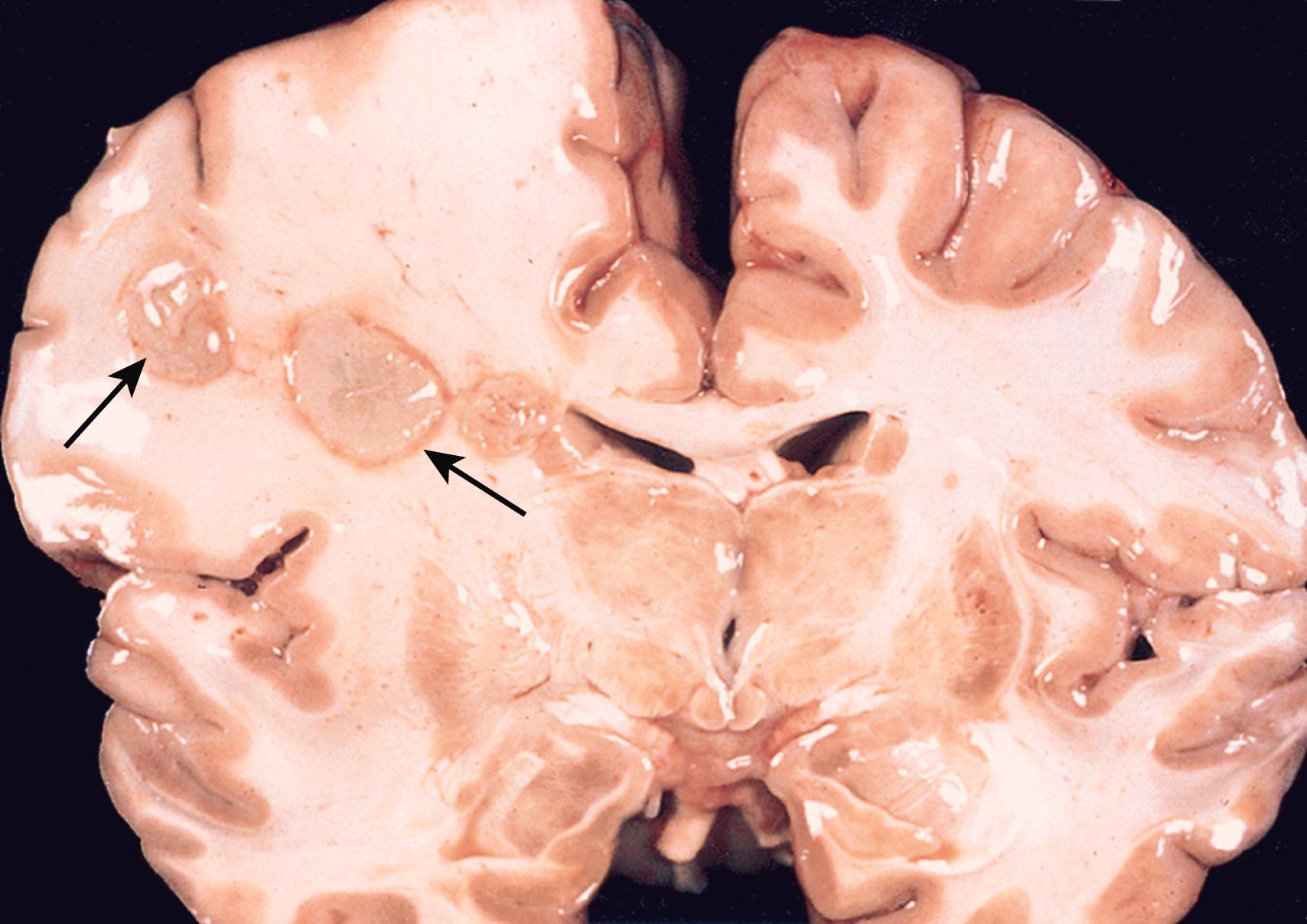
Infarcts can be divided into two broad groups. Nonhemorrhagic infarcts result from acute vascular occlusions and may evolve into hemorrhagic infarcts when there is reperfusion of ischemic tissue, either through collaterals or after dissolution of emboli. Hemorrhagic infarcts usually manifest as multiple, sometimes confluent, petechial hemorrhages ( Fig. 21.7 A, B ). The microscopic picture and evolution of hemorrhagic infarction are similar to those of nonhemorrhagic infarction, with the addition of blood extravasation and resorption. In individuals with coagulopathies, hemorrhagic infarcts may be associated with large intracerebral hematomas.
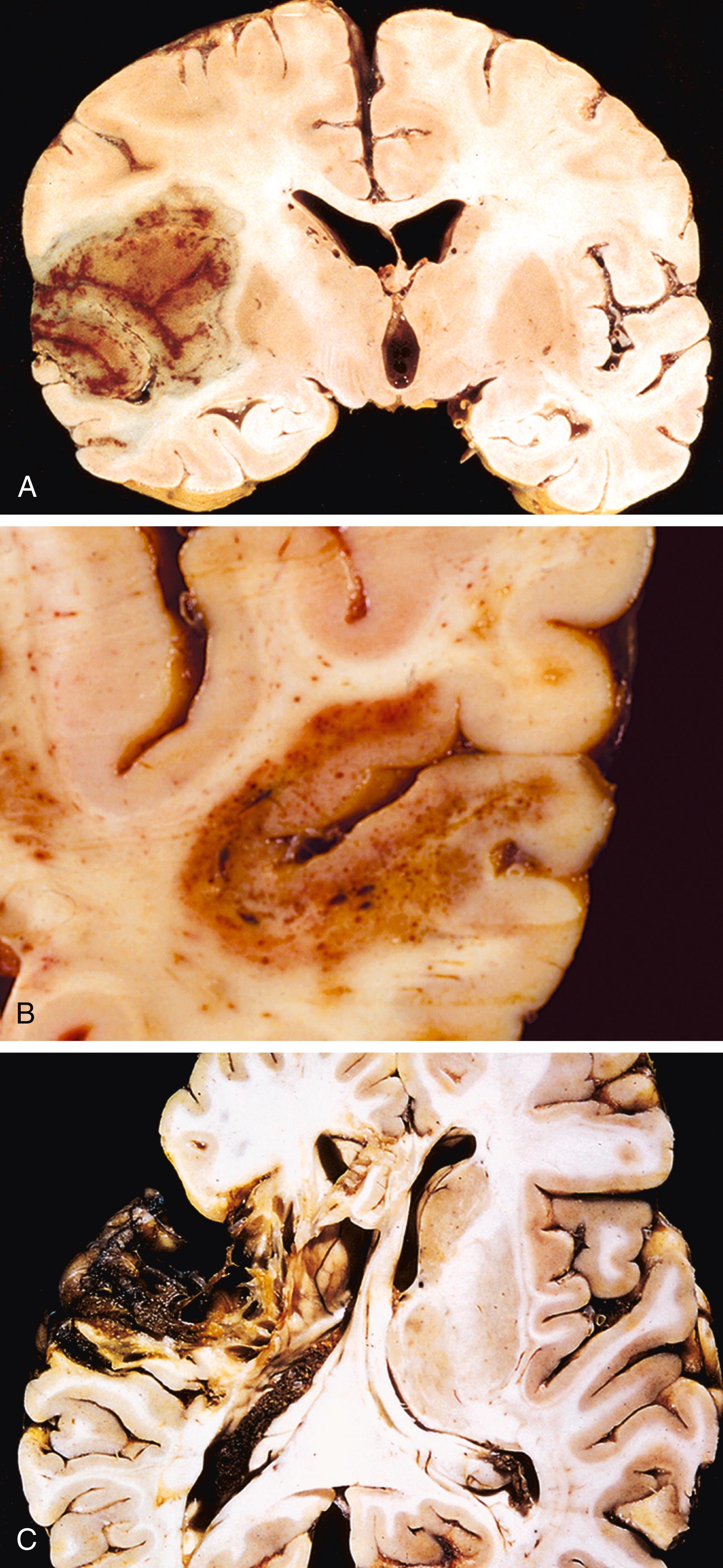
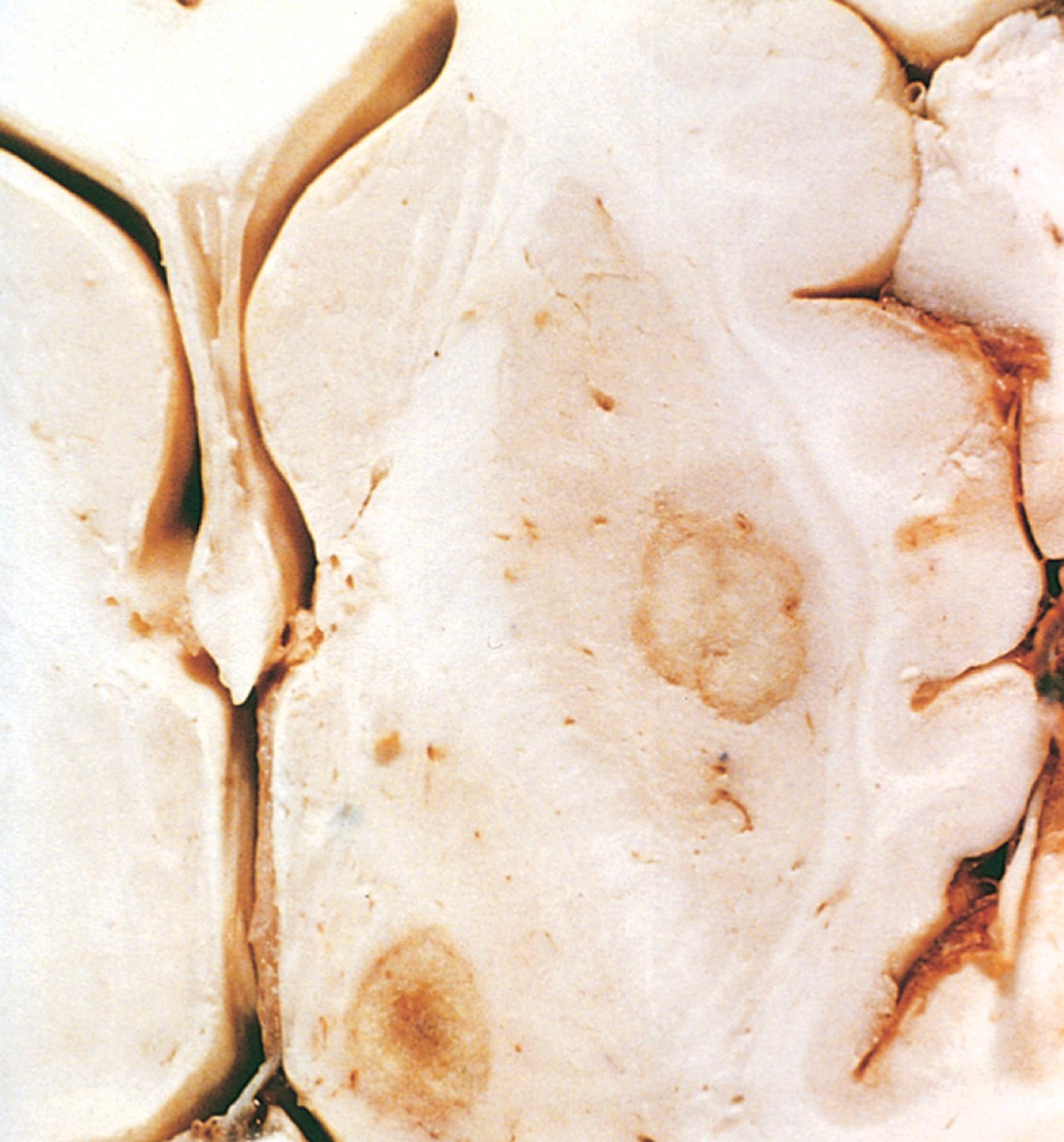
The macroscopic appearance of a nonhemorrhagic infarct evolves over time. During the first 6 hours, the tissue is unchanged in appearance, but by 48 hours, the tissue becomes pale, soft, and swollen. From days 2 to 10, the injured brain turns gelatinous and friable, and the boundary between normal and abnormal tissue becomes more distinct as edema resolves in the adjacent viable tissue. From day 10 to week 3, the tissue liquefies, eventually leaving a fluid-filled cavity, which gradually appears larger as dead tissue is resorbed ( Fig. 21.7 C).
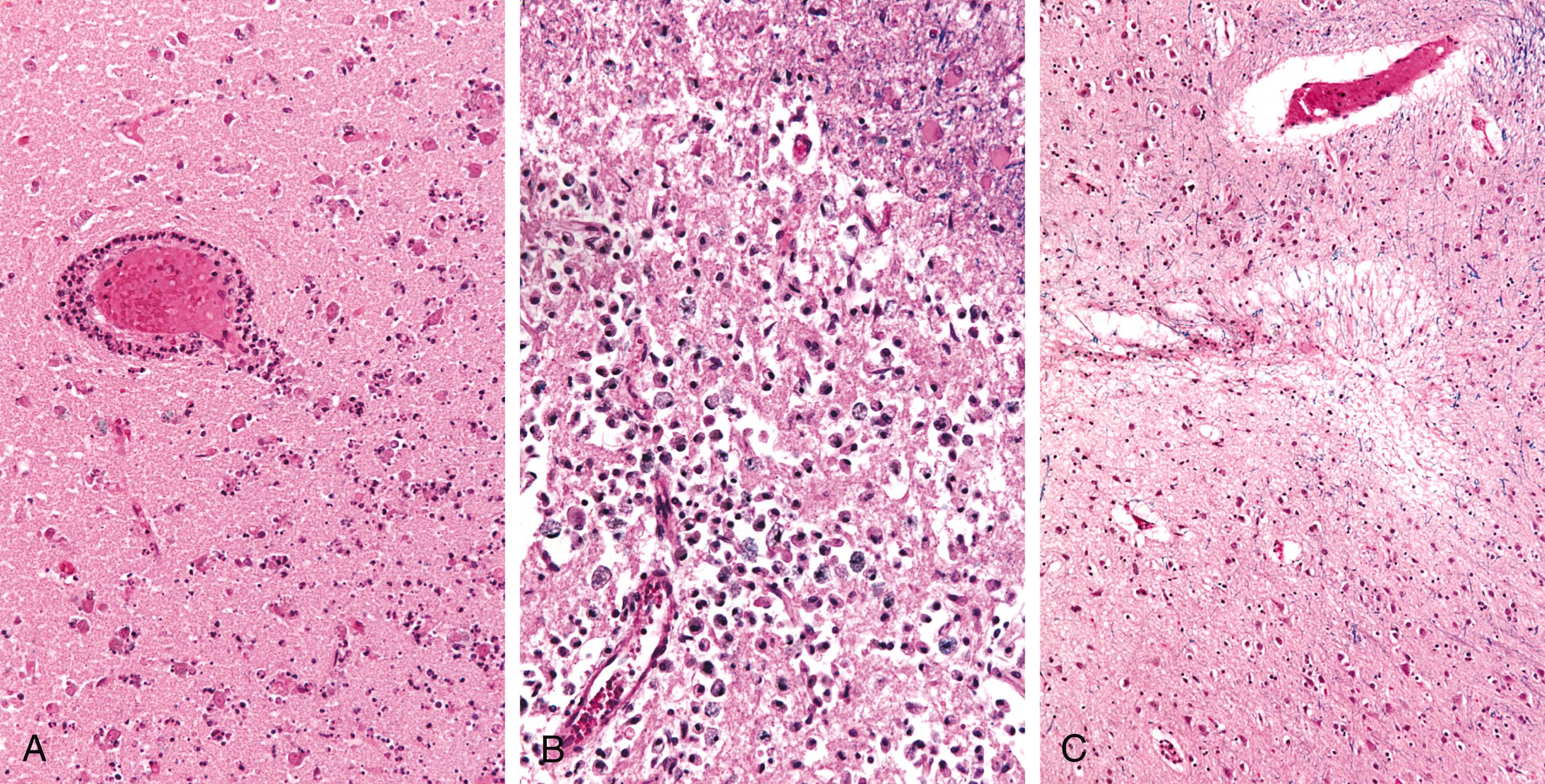
Microscopically, the tissue reaction follows a characteristic sequence. After the first 12 hours, ischemic neuronal change (red neurons) (see Fig. 21.1 A) and cytotoxic and vasogenic edema appear. Endothelial and glial cells, mainly astrocytes, swell, and myelinated fibers begin to disintegrate. During the first several days neutrophils infiltrate the area of injury ( Fig. 21.8 A ), but these are replaced over the next 2 to 3 weeks by macrophages. Macrophages containing myelin or red cell breakdown products may persist in the lesion for months to years. As the process of phagocytosis and liquefaction proceeds, astrocytes at the edges of the lesion progressively enlarge, divide, and develop a prominent network of cytoplasmic extensions (gemistocytic change) ( Fig. 21.8 B). After several months, the striking astrocytic nuclear and cytoplasmic enlargement regresses. In the wall of the cavity, astrocyte processes form a dense feltwork of glial fibers admixed with new capillaries and a few perivascular connective tissue fibers ( Fig. 21.8 C).
Border zone (“watershed”) infarcts occur in regions of the brain and spinal cord that lie at the most distal portions of arterial territories. They are usually seen after episodes of hypotension. In the cerebral hemispheres, the border zone between the anterior and the middle cerebral artery distributions is at greatest risk. Damage to this region produces a wedge-shaped band of necrosis over the cerebral convexity a few centimeters lateral to the interhemispheric fissure.
Infarcts present with combinations of localizing and nonlocalizing signs, which are usually more rapid in onset with embolic occlusions than with thromboses. Motor and/or sensory deficits (e.g., in the legs) dominate with anterior cerebral artery occlusions; aphasia, motor and/or sensory defects and hemiplegia if the middle cerebral artery in the dominant hemisphere is occluded; and visual defects with occlusion of the posterior cerebral artery.
Hemorrhages within the brain are caused by (1) hypertension and other diseases leading to vascular wall injury; (2) structural lesions such as arteriovenous and cavernous malformations; (3) trauma; and (4) tumors. Hemorrhages may occur at any site within the cranium—outside the brain or within it (intraparenchymal) ( Table 21.1 ). Hemorrhages in the epidural or subdural space are typically associated with trauma and are discussed later; by contrast, hemorrhages within the brain parenchyma and in the subarachnoid space are more commonly a manifestation of underlying cerebrovascular disease and are discussed here.
| Location | Etiology | Additional Features |
|---|---|---|
| Intraparenchymal | Trauma (contusions) | Selective involvement of the crests of gyri, where the brain is in contact with the inner surface of the skull (frontal and temporal tips, orbitofrontal surface) |
| Ischemia (hemorrhagic conversion of an ischemic infarct) | Petechial hemorrhages in an area of previously ischemic brain (reperfusion injury), usually following the cortical ribbon | |
| Cerebral amyloid angiopathy | “Lobar” hemorrhage, involving subcortical white matter and often extending into the subarachnoid space | |
| Hypertension | Centered in the deep white matter, thalamus, basal ganglia, or brain stem; may extend into the ventricular system | |
| Tumors (primary or metastatic) | Associated with high-grade gliomas or certain types of metastatic tumors (melanoma, choriocarcinoma, renal cell carcinoma) | |
| Subarachnoid space | Trauma | Typically associated with underlying parenchymal injury |
| Vascular abnormality (arteriovenous malformation or aneurysm) | Sudden onset of severe headache, often with rapid neurologic deterioration; secondary injury may emerge and is associated with vasospasm | |
| Epidural space | Trauma | Usually associated with skull fracture (in adults); rapidly evolving neurologic symptoms (often after a short lucid period) that require intervention |
| Subdural space | Trauma | May follow minor trauma; slowly evolving neurologic symptoms, often with a delay from the time of injury |
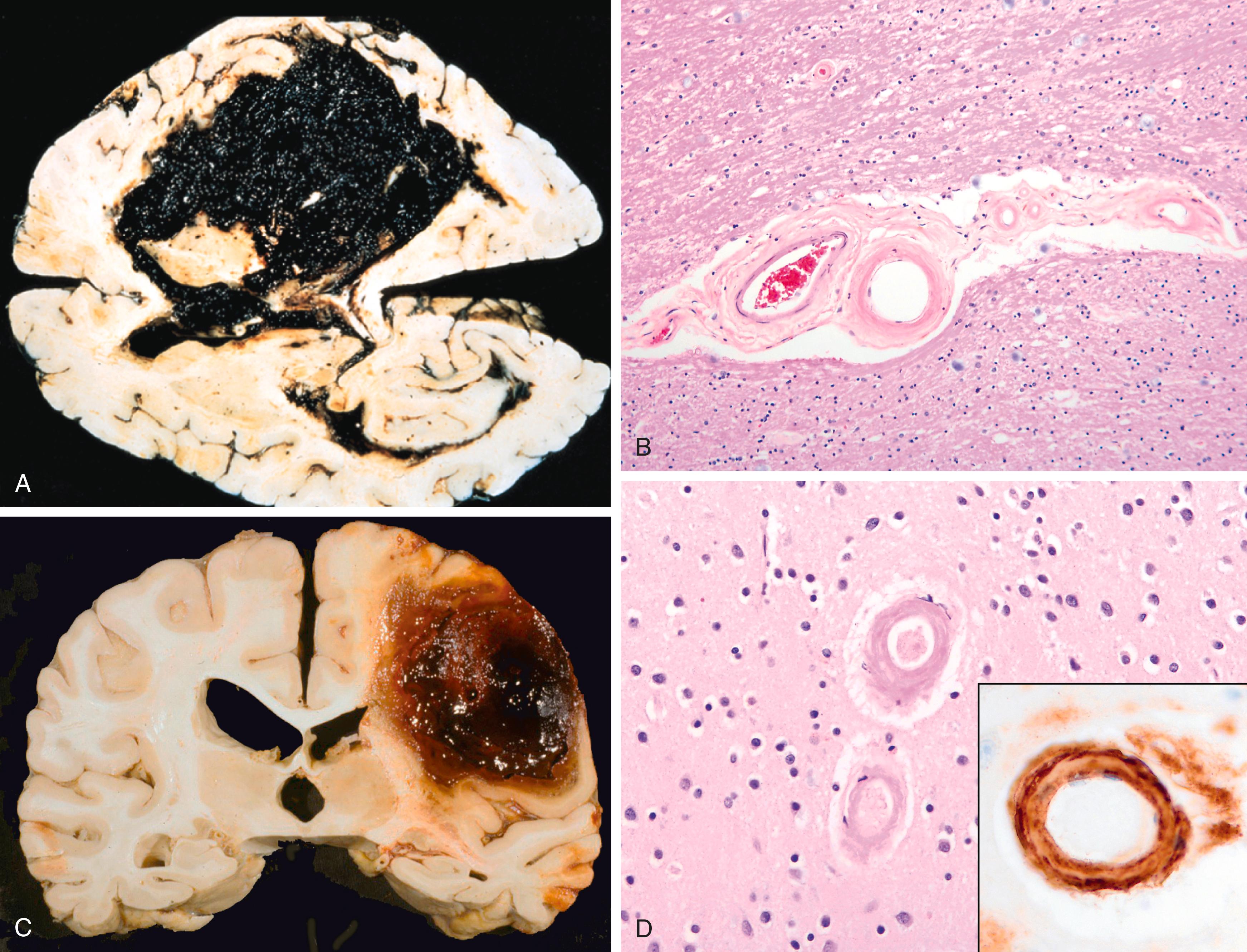
Hypertension is the most common risk factor for deep brain parenchymal hemorrhages, accounting for more than 50% of clinically significant hemorrhages and for roughly 15% of deaths among individuals with chronic hypertension. Spontaneous (nontraumatic) intraparenchymal hemorrhages are most common in mid to late adult life, with a peak incidence at about 60 years of age. Most are due to the rupture of a small intraparenchymal vessel. Intracerebral hemorrhage can be devastating when it affects large portions of the brain or extends into the ventricular system, or it can be clinically silent if it affects small regions. Hypertensive intraparenchymal hemorrhages typically occur in the basal ganglia, thalamus, pons, and cerebellum, with the location and the size of the bleed determining its clinical manifestations. If the individual survives the acute event, gradual resolution of the hematoma ensues, sometimes with considerable clinical improvement.
In acute intracerebral hemorrhage, extravasated blood compresses the adjacent parenchyma ( Fig. 21.9 A ). With time, hemorrhages are converted to a cavity with a brown, discolored rim. On microscopic examination, early lesions consist of clotted blood surrounded by edematous brain tissue containing neurons and glia displaying morphologic changes typical of anoxic injury. Eventually the edema resolves, pigment- and lipid-laden macrophages appear, and a reactive astrocyte proliferation becomes visible at the periphery of the lesion. The cellular events then follow the same time course observed after cerebral infarction. Arteries may show arteriosclerosis ( Fig. 21.9 B).
As in infarcts, the signs and symptoms of parenchymal hemorrhage are determined largely by its location. The symptoms often develop rapidly over several minutes and may continue to evolve over hours, often followed by gradual improvement. They include hemiplegia, acute-onset confusion and memory loss, and visual deficits.
Cerebral amyloid angiopathy (CAA) is a disease in which amyloidogenic peptides, similar to those found in Alzheimer disease (discussed later), deposit in the walls of medium- and small-caliber meningeal and cortical vessels. Amyloid deposition makes vessel walls rigid and fragile, increasing the risk for hemorrhages, which differ in distribution from those associated with hypertension. CAA-associated hemorrhages often occur in the lobes of the cerebral cortex (lobar hemorrhages) ( Fig. 21.9 C, D). In addition to these symptomatic hemorrhages, CAA can also result in small (<1 mm), silent cortical hemorrhages (microhemorrhages).
The most frequent cause of clinically significant nontraumatic subarachnoid hemorrhage is rupture of a saccular (berry) aneurysm. Hemorrhage into the subarachnoid space may also result from vascular malformation, trauma, rupture of an intracerebral hemorrhage into the ventricular system, coagulopathies, and tumors. Epidural and subdural hemorrhages are typically secondary to trauma and are discussed later.
In about one-third of cases, rupture of a saccular aneurysm occurs because of an acute increase in intracranial pressure, such as occurs with straining at stool or sexual orgasm. Blood under arterial pressure is forced into the subarachnoid space, and the patient experiences a sudden, excruciating headache (known as a thunderclap headache, often described as “the worst headache I’ve ever had”) and rapidly loses consciousness. Between 25% and 50% of affected individuals die from the first bleed, and recurrent bleeds are common in survivors. The prognosis worsens with each bleeding episode.
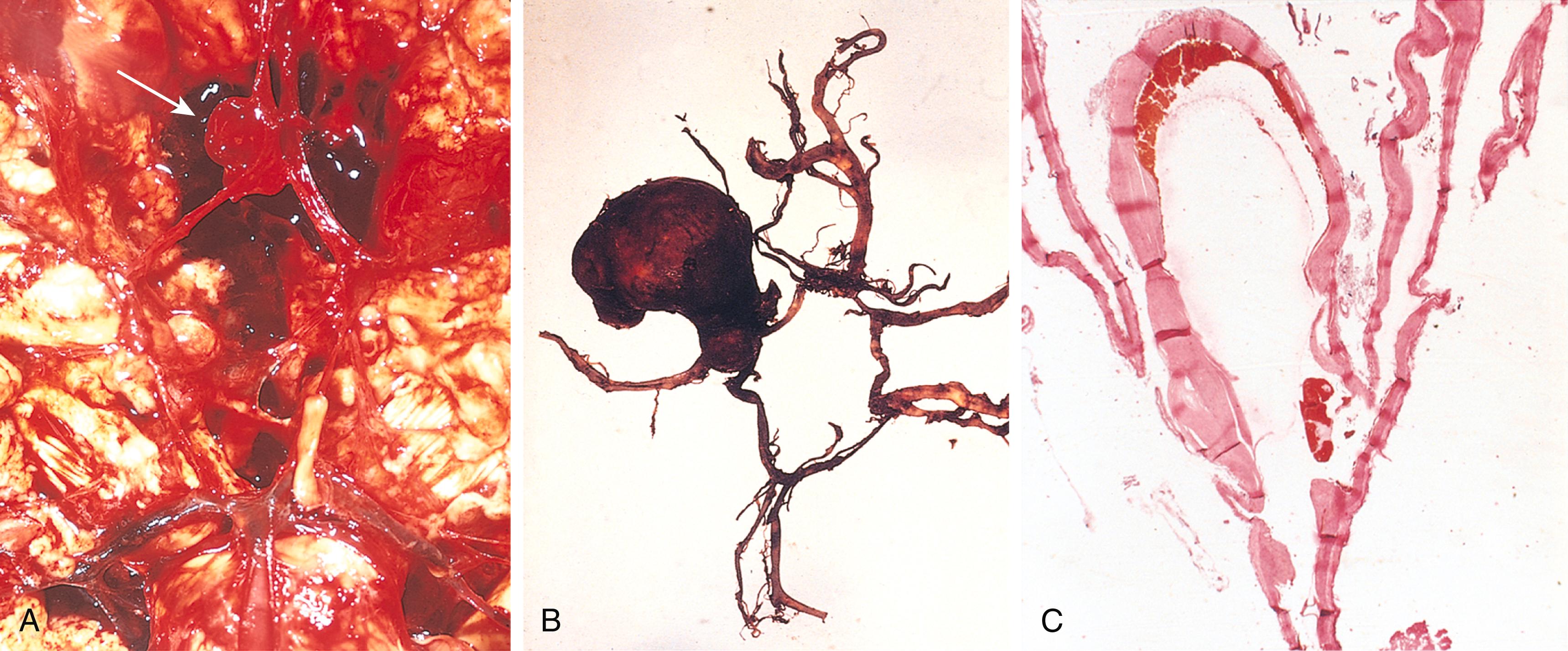
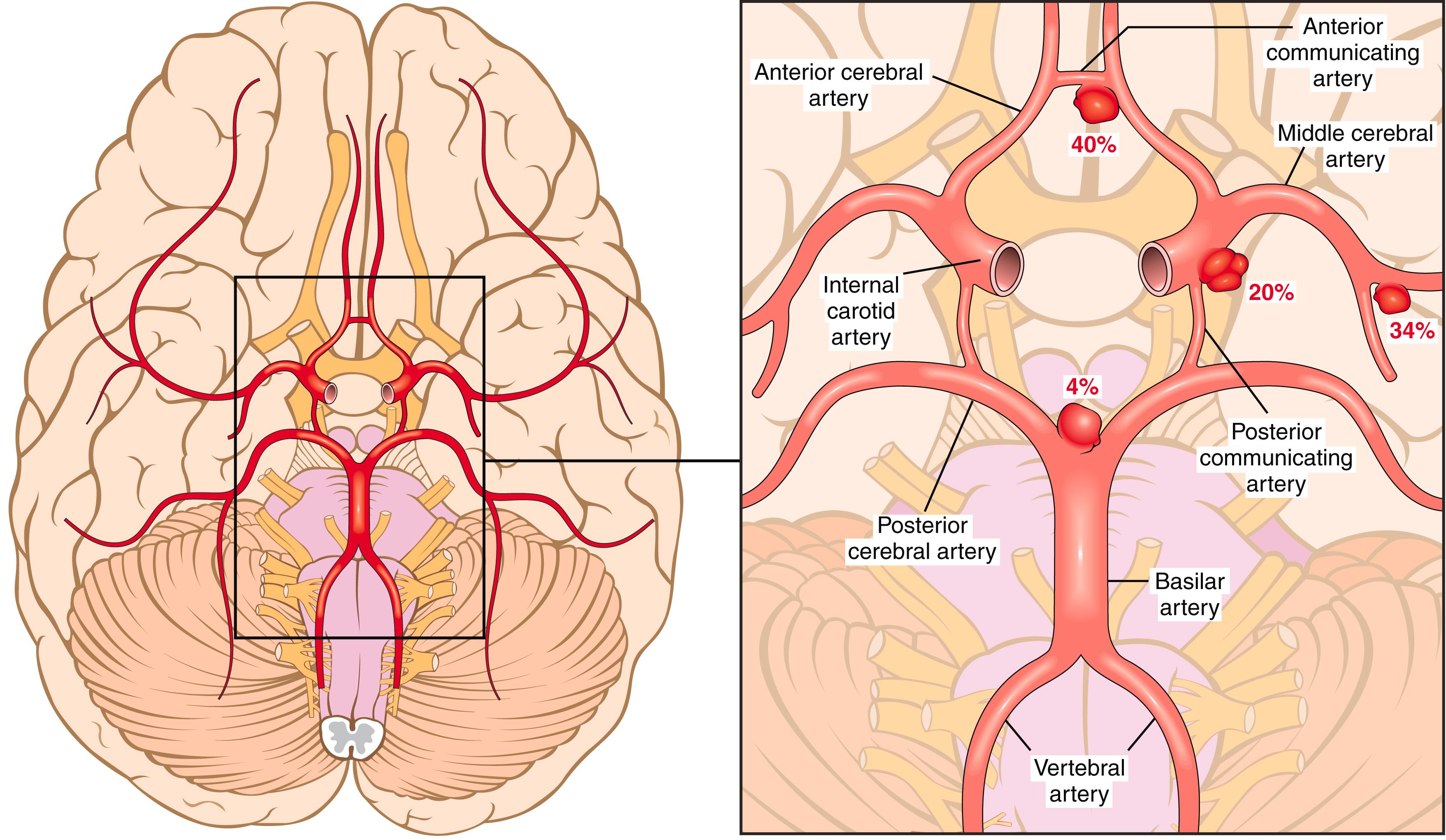
About 90% of saccular aneurysms occur in the anterior circulation near major arterial branch points ( Fig. 21.10 ); multiple aneurysms exist in 20% to 30% of cases. The aneurysms are not present at birth but develop over time because of underlying defects in the vessel media. There is an increased risk for aneurysms in patients with autosomal dominant polycystic kidney disease ( Chapter 12 ) and genetic disorders of extracellular matrix proteins (e.g., Ehler-Danlos syndrome). Overall, roughly 1.3% of aneurysms bleed per year, with the probability of rupture increasing with size. For example, aneurysms larger than 1 cm in diameter have a roughly 50% risk for bleeding per year. In the early period after a subarachnoid hemorrhage, there is an additional risk for ischemic injury from vasospasm of other vessels. Healing and the attendant meningeal fibrosis and scarring sometimes obstruct CSF flow or disrupt CSF resorption, leading to hydrocephalus.
A saccular aneurysm is a thin-walled outpouching of an artery ( Fig. 21.11 ). Beyond the neck of the aneurysm, the muscular wall and intimal elastic lamina are absent, such that the aneurysm sac is lined only by thickened hyalinized intima. The adventitia covering the sac is continuous with that of the parent artery. Rupture usually occurs at the apex of the sac, releasing blood into the subarachnoid space, the substance of the brain, or both.
Nonsaccular intracranial aneurysms may be atherosclerotic, mycotic, traumatic, and dissecting ( Chapter 8 ). The last three types (like saccular aneurysms) are most often found in the anterior circulation, whereas atherosclerotic aneurysms are frequently fusiform and most commonly involve the basilar artery. Nonsaccular aneurysms usually manifest as cerebral infarction due to vascular occlusion instead of subarachnoid hemorrhage.
Vascular malformations of the brain are classified into four principal types based on the nature of the abnormal vessels: arteriovenous malformations (AVMs), cavernous malformations, capillary telangiectasias, and venous angiomas. AVMs, the most common of these, affect males twice as frequently as females and most commonly manifest between 10 and 30 years of age with seizures, an intracerebral hemorrhage, or a subarachnoid hemorrhage. In the newborn period, large AVMs may lead to high-output congestive heart failure because of blood shunting from arteries to veins. The risk for bleeding makes AVM the most dangerous type of vascular malformation. Multiple AVMs can be seen in the setting of hereditary hemorrhagic telangiectasia, an autosomal dominant condition often associated with mutations affecting the TGF-β pathway.
AVMs may involve subarachnoid vessels extending into brain parenchyma or occur exclusively within the brain. On gross inspection, they resemble a tangled network of wormlike vascular channels ( Fig. 21.12 ). Microscopic examination shows enlarged blood vessels separated by gliotic tissue, often with evidence of previous hemorrhage.
Cavernous malformations consist of distended, loosely organized vascular channels with thin collagenized walls without intervening nervous tissue. They occur most often in the cerebellum, pons, and subcortical regions and have a low blood flow without significant arteriovenous shunting. Foci of old hemorrhage, infarction, and calcification frequently surround the abnormal vessels.
Capillary telangiectasias are microscopic foci of dilated thin-walled vascular channels separated by relatively normal brain parenchyma and occur most frequently in the pons. Venous angiomas (varices) consist of aggregates of ectatic venous channels. These two types of vascular malformation are unlikely to bleed or to cause symptoms, and most are incidental findings.
Hypertension causes hyaline arteriolar sclerosis ( Chapter 8 ) of the deep penetrating small arteries and arterioles that supply the basal ganglia, the hemispheric white matter, and the brain stem. Affected arteriolar walls are weakened and are vulnerable to rupture. In some instances, minute aneurysms form in vessels less than 300 μm in diameter. In addition to massive intracerebral hemorrhage (discussed earlier), several other pathologic outcomes are related to hypertension.
Lacunes or lacunar infarcts are small cavitary infarcts, just a few millimeters in size, that are found most commonly in the deep gray matter (basal ganglia and thalamus), the internal capsule, the deep white matter, and the pons. They are caused by occlusion of a single penetrating branch of a large cerebral artery. Depending on their location, lacunes can be silent clinically or cause significant neurologic impairment.
Rupture of the small-caliber penetrating vessels may occur, leading to the development of small hemorrhages. In time, these hemorrhages resorb, leaving behind a slitlike cavity (slit hemorrhage) surrounded by brownish discoloration.
Acute hypertensive encephalopathy is most often associated with sudden sustained increases in diastolic blood pressure to greater than 130 mm Hg (so called severe, or malignant, hypertension, see Chapters 8 and 12 ). It is characterized by increased intracranial pressure and global cerebral dysfunction, manifesting as headaches, confusion, vomiting, convulsions, and sometimes coma. Rapid therapeutic intervention to reduce the blood pressure is essential. Postmortem examination may show brain edema, with or without transtentorial or tonsillar herniation. Petechiae and fibrinoid necrosis of arterioles in the gray matter and white matter may be seen microscopically, as in other tissues ( Chapters 8 and 12 ).
Vasculitis in the CNS is most often the result of infections or systemic autoimmune diseases. It may impair blood flow and cause cerebral dysfunction or infarction. Infection-associated arteritis of small and large vessels was previously seen mainly in association with syphilis and tuberculosis but is now more often caused by opportunistic infections (e.g., aspergillosis, herpes zoster, or CMV) in the setting of immunocompromise. Some systemic forms of vasculitis, such as polyarteritis nodosa, may involve cerebral vessels and cause single or multiple infarcts.
Individuals who cumulatively suffer over the course of years multiple, bilateral, gray matter (cortex, thalamus, basal ganglia) and white matter infarcts may develop a distinctive clinical syndrome characterized by dementia, gait abnormalities, and pseudobulbar signs (emotional instability), often with superimposed focal neurologic deficits. The syndrome, generally referred to as vascular dementia, is caused by multifocal vascular disease of several types, including (1) cerebral atherosclerosis; (2) vessel thrombosis or embolization from carotid vessels or from the heart; and (3) cerebral arteriolosclerosis from chronic hypertension. Many individuals with neurodegenerative diseases resulting in cognitive impairment or dementia also have evidence of cerebrovascular disease.
The physical forces associated with head injury may result in skull fractures, parenchymal injury, and vascular injury; all three can coexist. The anatomic location of the lesion and the limited capacity of the brain for functional repair are major determinants of the consequences of CNS trauma. The magnitude and distribution of a traumatic brain lesion also depend on the shape of the object causing the trauma, the force of impact, and whether the head is in motion at the time of injury. A blow to the head may be penetrating or blunt; it may cause either an open or a closed injury. Injury of several cubic centimeters of brain parenchyma may be clinically silent (if in the frontal lobe), severely disabling (e.g., in the spinal cord), or fatal (e.g., in the brain stem).
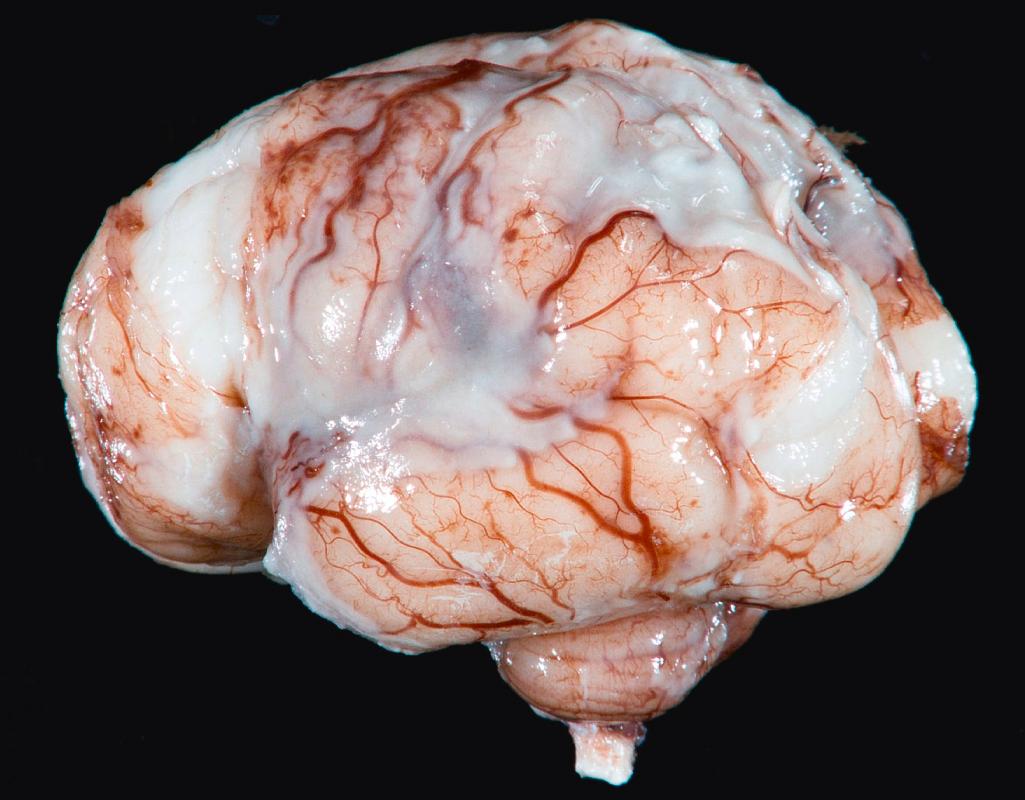
When the head strikes a fixed object, brain injury may occur at the site of impact—a coup injury —or opposite the site of impact on the other side of the brain as the brain rebounds from the initial impact—a contrecoup injury. Both coup and contrecoup lesions are contusions, with comparable gross and microscopic appearances. A contusion is caused by rapid tissue displacement, disruption of vascular channels, and subsequent hemorrhage, tissue injury, and edema. Since they are closest to the skull, the crests of the gyri are the parts of the brain that are most susceptible to traumatic injury. Contusions are common in regions of the brain overlying rough and irregular inner skull surfaces, such as the orbitofrontal regions and the temporal lobe tips. Penetration of the brain by a projectile such as a bullet or a skull fragment from a fracture causes a laceration, with tissue tearing, vascular disruption, and hemorrhage.
Contusions are wedge shaped, with the widest aspect closest to the point of impact ( Fig. 21.13 A ). Within a few hours of injury, blood extravasates throughout the involved tissue, across the width of the cerebral cortex, and into the white matter and subarachnoid spaces. Although functional effects are seen earlier, morphologic evidence of neuronal injury (i.e., nuclear pyknosis, cytoplasmic eosinophilia, cellular disintegration) takes about 24 hours to appear. The inflammatory response to the injured tissue follows its usual course, with neutrophils preceding the appearance of macrophages. In contrast with ischemic lesions, in which the superficial layer of cortex may be preserved, trauma affects the superficial layers most severely.
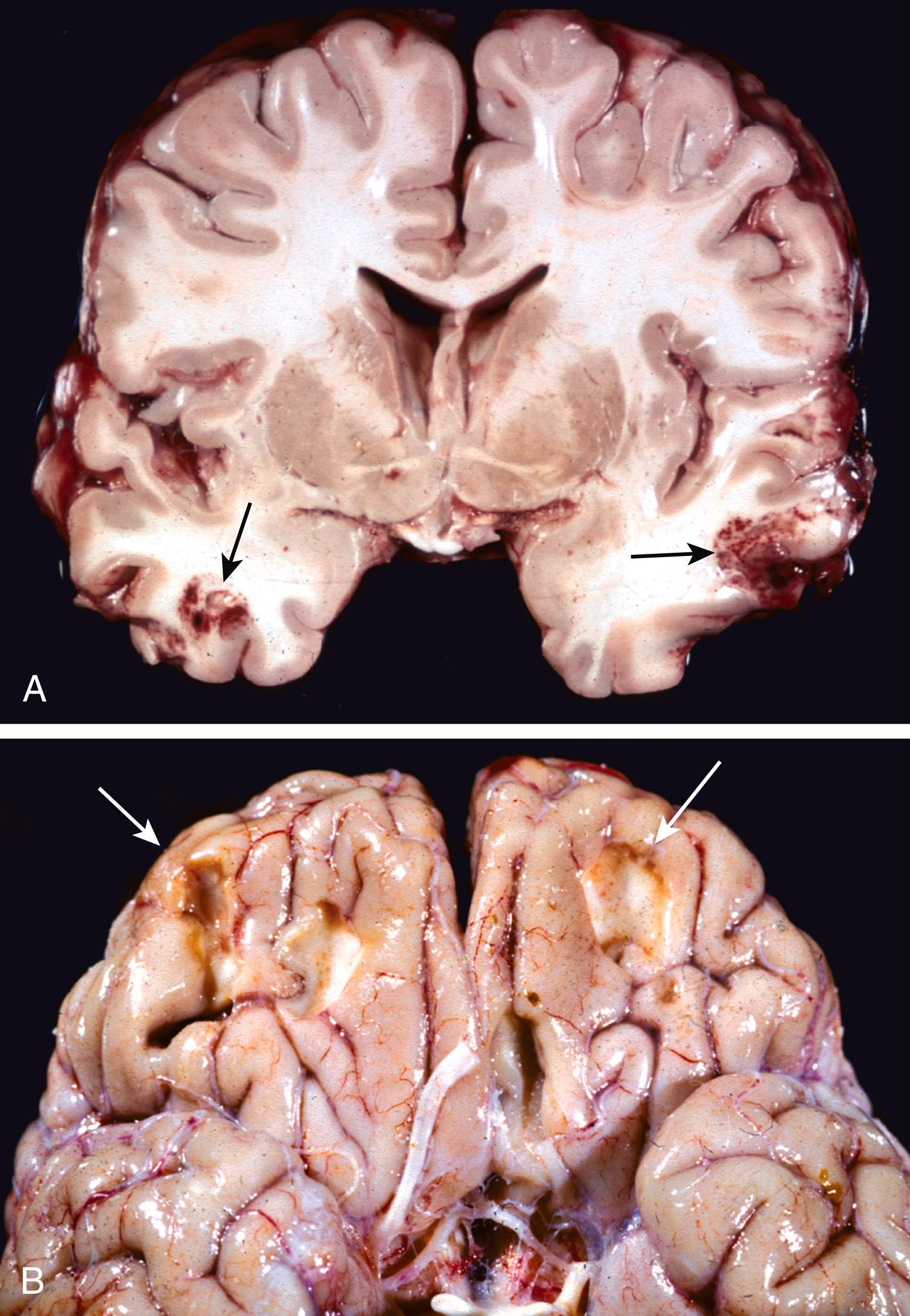
Old traumatic lesions characteristically appear as depressed, retracted, yellowish brown patches (plaques jaunes) involving the crests of gyri ( Fig. 21.13 B). These lesions show gliosis and residual hemosiderin-laden macrophages.
Trauma may also cause more subtle but widespread injury to axons within the brain (diffuse axonal injury), sometimes with devastating consequences. The movement of one region of brain relative to another is thought to disrupt axonal integrity and function. Angular acceleration, even in the absence of impact, may cause axonal injury as well as hemorrhage. As many as 50% of patients who develop coma shortly after trauma are believed to have white matter damage and diffuse axonal injury, which can be seen as axonal swellings that appear within hours of the injury.
Concussion describes reversibly altered brain function, with or without loss of consciousness, as a result of head injury. The characteristic transient neurologic dysfunction includes loss of consciousness, temporary respiratory arrest, and loss of reflexes. Neurologic recovery is the norm, although amnesia for the event may persist. The pathogenesis of the sudden disruption of nervous activity is unknown.
Chronic traumatic encephalopathy (CTE, previously referred to as dementia pugilistica ) is a dementing illness that develops after repeated head trauma as may occur in football players and boxers. Affected brains are atrophic, with enlarged ventricles, and show accumulation of tau-containing neurofibrillary tangles (which are also seen in some neurodegenerative diseases, discussed later) in a characteristic pattern involving gyral depths and perivascular regions in the frontal and temporal lobe cortices. Repeated concussions predispose to the development of CTE; however, it remains uncertain what factors (e.g., the number, frequency, and/or severity of individual traumatic events, or some combination of these) determine whether encephalopathy ultimately develops.
Vascular injury is a frequent component of CNS trauma; it results from disruption of the vessel wall and leads to hemorrhage in different anatomic sites (see Table 21.1 ). Depending on the affected vessel, the hemorrhage may be epidural, subdural, subarachnoid, or intraparenchymal ( Fig. 21.14 A ), occurring alone or in combination. Subarachnoid and intraparenchymal hemorrhages were discussed earlier in the context of aneurysms and hypertension, respectively; when traumatic, they most often occur at sites of contusions and lacerations.
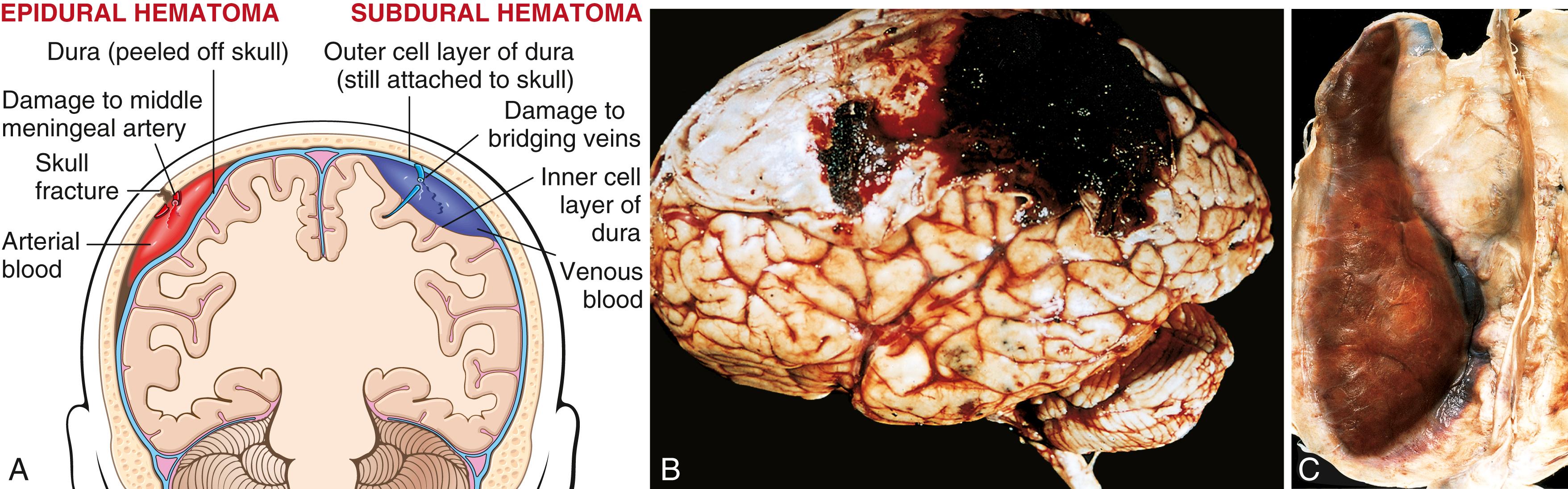
Dural vessels—especially the middle meningeal artery—are vulnerable to traumatic injury. In children and adults, tears involving dural vessels almost always stem from skull fractures. In infants, by contrast, traumatic displacement of the easily deformable skull may tear a vessel, even in the absence of a skull fracture. Once a vessel tears, blood accumulates under arterial pressure and separates the tightly applied dura away from the inner skull surface, producing a hematoma that compresses the brain surface ( Fig. 21.14 B; eFig. 21.1 ). Clinically, patients can be lucid for several hours after the traumatic event before neurologic signs appear. An epidural hematoma may expand rapidly and constitutes a neurosurgical emergency necessitating prompt drainage and repair to prevent death.
Rapid movement of the brain during trauma can tear the bridging veins that extend from the cerebral hemispheres through the subarachnoid and subdural space to the dural sinuses. Their disruption produces bleeding into the subdural space. Because the inner cell layer of the dura is quite thin and in very close proximity to the arachnoid layer, the blood appears to be between the dura and arachnoid, but it is actually between the two layers of the dura. In patients with brain atrophy (e.g., due to age-related changes), the bridging veins are stretched and there is additional space within which the brain can move, accounting for the higher rate of subdural hematomas in older adults, even with minor trauma. Infants are also susceptible to subdural hematomas because their bridging veins are thin walled.
Subdural hematomas typically become manifest within the first 48 hours after injury. They are most common over the lateral aspects of the cerebral hemispheres and are bilateral in about 10% of cases. Neurologic signs are attributable to the pressure exerted on the adjacent brain. Symptoms are most often nonlocalizing, taking the form of headache, confusion, and slowly progressive neurologic deterioration.
Acute subdural hematoma appears as a collection of freshly clotted blood apposed to the contour of the brain surface, without extension into the depths of sulci ( Fig. 21.14 C, eFig. 21.2 ). The underlying brain is flattened, and the subarachnoid space is often clear. Subdural hematomas organize by lysis of the clot (about 1 week), growth of granulation tissue from the dural surface into the hematoma (2 weeks), and fibrosis (1–3 months). Subdural hematomas commonly rebleed, presumably from the thin-walled vessels of the granulation tissue, leading to microscopic findings consistent with hemorrhages of varying ages.
Symptomatic subdural hematomas are treated by surgical removal of the blood and associated reactive tissue.
Cerebral palsy is a term for nonprogressive neurologic motor deficits characterized by spasticity, dystonia, ataxia or athetosis, and paresis attributable to injury occurring during the prenatal and perinatal periods. There may be no associated intellectual disability. Signs and symptoms may not be apparent at birth and only declare themselves later, well after the causal event.
The two major types of injury that occur in the perinatal period are hemorrhages and infarcts. These differ from the otherwise similar lesions in adults in terms of their locations and the tissue reactions they engender. In premature infants, there is an increased risk for intraparenchymal hemorrhage within the germinal matrix, most often adjacent to the anterior horn of the lateral ventricle. Hemorrhages may extend into the ventricular system and from there to the subarachnoid space, sometimes causing hydrocephalus. Ischemic infarcts may occur in the supratentorial periventricular white matter (periventricular leukomalacia), especially in premature infants ( Fig. 21.15 ). The residua of these infarcts are chalky yellow plaques consisting of discrete regions of white matter necrosis and dystrophic calcification. When sufficiently widespread to involve both gray matter and white matter, large cystic lesions can develop throughout the hemispheres, a condition termed multicystic encephalopathy.
Infections may damage the nervous system directly through injury of neurons or glia by the infectious agent, or indirectly through microbial toxins or the destructive effects of the inflammatory response. There are four principal routes by which microbes enter the nervous system:
Hematogenous spread is the most common; microbes ordinarily gain access through the arterial circulation, but retrograde venous spread can occur via anastomoses between the veins of the face and the venous sinuses of the skull.
Direct implantation of microorganisms is almost invariably due to open or penetrating trauma but sometimes can be associated with congenital malformations (e.g., meningomyelocele) that provide ready access for microbes.
Transplacental spread. Certain perinatal infections may be acquired transplacentally or during birth and have a propensity to cause destructive brain lesions. Agents in this group include Toxoplasma and CMV, both of which can result in parenchymal calcifications along with tissue injury; these are discussed later.
Local extension can originate from infected adjacent structures, such as air sinuses, teeth, skull, or vertebrae.
Viruses may also be transported along the peripheral nervous system, as occurs with rabies and herpes zoster viruses.
In the following sections we discuss infections that are specific to the central nervous system ( Table 21.2 ).
| Type of Infection | Clinical Syndrome | Common Causative Organisms |
|---|---|---|
| Bacterial Infections | ||
| Meningitis | Acute pyogenic meningitis | Escherichia coli or group B streptococci (infants) |
| Neisseria meningitidis (young adults) | ||
| Streptococcus pneumoniae or Listeria monocytogenes (older adults) | ||
| Chronic meningitis | Mycobacterium tuberculosis | |
| Localized infections | Abscess | Streptococci and staphylococci |
| Empyema | Polymicrobial (staphylococci, anaerobic gram-negative) | |
| Viral Infections | ||
| Meningitis | Acute aseptic meningitis | Enteroviruses |
| Measles (subacute sclerosing panencephalitis) | ||
| Human immunodeficiency virus (HIV) | ||
| Influenza species | ||
| Lymphocytic choriomeningitis virus | ||
| Encephalitis | Encephalitic syndromes | Herpes simplex (HSV-1, HSV-2) |
| Cytomegalovirus | ||
| Human immunodeficiency virus | ||
| JC polyomavirus (progressive multifocal leukoencephalopathy) | ||
| Arthropod-borne encephalitis | West Nile virus, other arboviruses | |
| Brain stem and spinal cord syndromes | Rhombencephalitis | Rabies |
| Spinal poliomyelitis | Polio | |
| Encephalitis, meningitis | West Nile virus | |
| Rickettsia, Spirochetes, and Fungi | ||
| Meningitic syndromes | Rocky Mountain spotted fever | Rickettsia rickettsii |
| Neurosyphilis | Treponema pallidum | |
| Lyme disease (neuroborreliosis) | Borrelia burgdorferi | |
| Fungal meningitis | Cryptococcus neoformans | |
| Candida albicans | ||
| Protozoa and Metazoa | ||
| Meningitic syndromes | Cerebral malaria | Plasmodium falciparum |
| Amebic encephalitis | Naegleria species | |
| Localized infections | Toxoplasmosis | Toxoplasma gondii |
| Cysticercosis | Taenia solium | |
Meningitis is an inflammatory process typically induced by an infection involving the leptomeninges within the subarachnoid space; if the infection spreads into the underlying brain, it is termed meningoencephalitis. The term is also used in noninfectious settings such as chemical meningitis, a response to an irritant such as debris from a ruptured epidermoid cyst, and carcinomatous meningitis, inflammation caused by metastatic cancer cells that have spread to the subarachnoid space.
Infectious meningitis can be divided into acute pyogenic (usually bacterial), aseptic (usually viral), and chronic (usually tuberculous, spirochetal, or fungal) subtypes. Examination of the CSF is often useful in identifying the cause of the meningitis.
The most likely causes of bacterial meningitis vary with patient age. In neonates, common organisms are Escherichia coli and group B streptococci. In adolescents and young adults, Neisseria meningitidis is the most common pathogen; in older adults, Streptococcus pneumoniae and Listeria monocytogenes are more common. Across all ages, patients typically show systemic signs of infection along with meningeal irritation and neurologic impairment, including headache, photophobia, irritability, clouding of consciousness, and neck stiffness. Lumbar puncture reveals an increased pressure; examination of the CSF shows abundant neutrophils, elevated protein, and reduced glucose. Untreated pyogenic meningitis is often fatal, but with prompt diagnosis and administration of antibiotics, most patients can be cured.
In acute meningitis, an exudate is evident within the leptomeninges on the surface of the brain ( Fig. 21.16 ). The meningeal vessels are engorged and prominent, and tracts of pus may extend along blood vessels. On microscopic examination, neutrophils may fill the entire subarachnoid space or, in less severe cases, may be confined to regions adjacent to leptomeningeal blood vessels. Particularly in untreated meningitis, gram stain reveals varying numbers of the causative organism, particularly in untreated meningitis. In fulminant meningitis, the inflammatory cells infiltrate the walls of the leptomeningeal veins and may extend focally into the substance of the brain (cerebritis); secondary vasculitis and venous thrombosis may lead to hemorrhagic cerebral infarction. Leptomeningeal fibrosis may follow pyogenic meningitis and cause hydrocephalus; it is more common as a complication of tuberculous meningitis (discussed later).
Aseptic meningitis is a clinical term used for manifestations of meningitis, such as meningeal irritation, fever, and alterations of consciousness of relatively acute onset, in the absence of organisms detectable by bacterial culture. The disease is generally of viral etiology but may be rickettsial or autoimmune in origin (see Table 21.2 ). The clinical course is less fulminant than that of pyogenic meningitis, and the CSF findings also differ: in aseptic meningitis, there is a lymphocytic pleocytosis, the protein elevation is only moderate, and the glucose content is nearly always normal. The viral aseptic meningitides are usually self-limited and are treated symptomatically. The etiologic agent is identified in only a minority of cases; however, this may change through use of more sensitive and specific detection techniques (such as DNA sequencing). When pathogens are identified, enteroviruses are the most common etiology, accounting for 80% of cases.
Several pathogens, including mycobacteria, some spirochetes, and fungi, cause a chronic meningitis; infections with these organisms also may involve the brain parenchyma.
Tuberculous meningitis usually manifests with generalized signs and symptoms of headache, malaise, mental confusion, and vomiting. There is only a moderate increase in CSF cellularity, with mononuclear cells or a mixture of polymorphonuclear and mononuclear cells; the protein level is elevated, often strikingly so, and the glucose content typically is moderately reduced or normal. Infection with Mycobacterium tuberculosis may also result in a well-circumscribed intraparenchymal mass (tuberculoma), which may be associated with meningitis. Chronic tuberculous meningitis leads to arachnoid fibrosis, particularly at the base of the brain, and hydrocephalus from interference with CSF resorption.
Neurosyphilis, a tertiary stage of syphilis, occurs in about 10% of individuals with untreated Treponema pallidum infection. Coinfection with HIV increases the risk for developing neurosyphilis, and the disease is often more aggressive in this setting. There are several patterns of CNS involvement by syphilis, which may be present alone or in combination.
Meningovascular neurosyphilis is a chronic meningitis, usually involving the base of the brain, often with an obliterative endarteritis rich in plasma cells and lymphocytes.
Paretic neurosyphilis stems from parenchymal involvement by spirochetes and is associated with neuronal loss and marked proliferation of microglial cells. Clinically, this form of the disease causes an insidious progressive loss of mental and physical functions, mood alterations (including delusions of grandeur), and eventually severe dementia.
Tabes dorsalis results from damage to the sensory nerves in the dorsal roots. Consequences include impaired joint position sense and ataxia; loss of pain sensation, leading to skin and joint damage (Charcot joints) ; other sensory disturbances, particularly characteristic sudden, brief, severe stabs of pain (“lightning pains”); and the absence of deep tendon reflexes.
Neuroborreliosis refers to involvement of the nervous system by the spirochete Borrelia burgdorferi, the causative agent of Lyme disease. Neurologic signs and symptoms are highly variable and include aseptic meningitis, facial nerve palsies, mild encephalopathy, and polyneuropathies.
Fungal infection of the nervous system can give rise to chronic meningitis and, as with other pathogens, can be associated with parenchymal infection. Immunocompromise increases the risk for these diseases. Several fungal pathogens cause CNS disease:
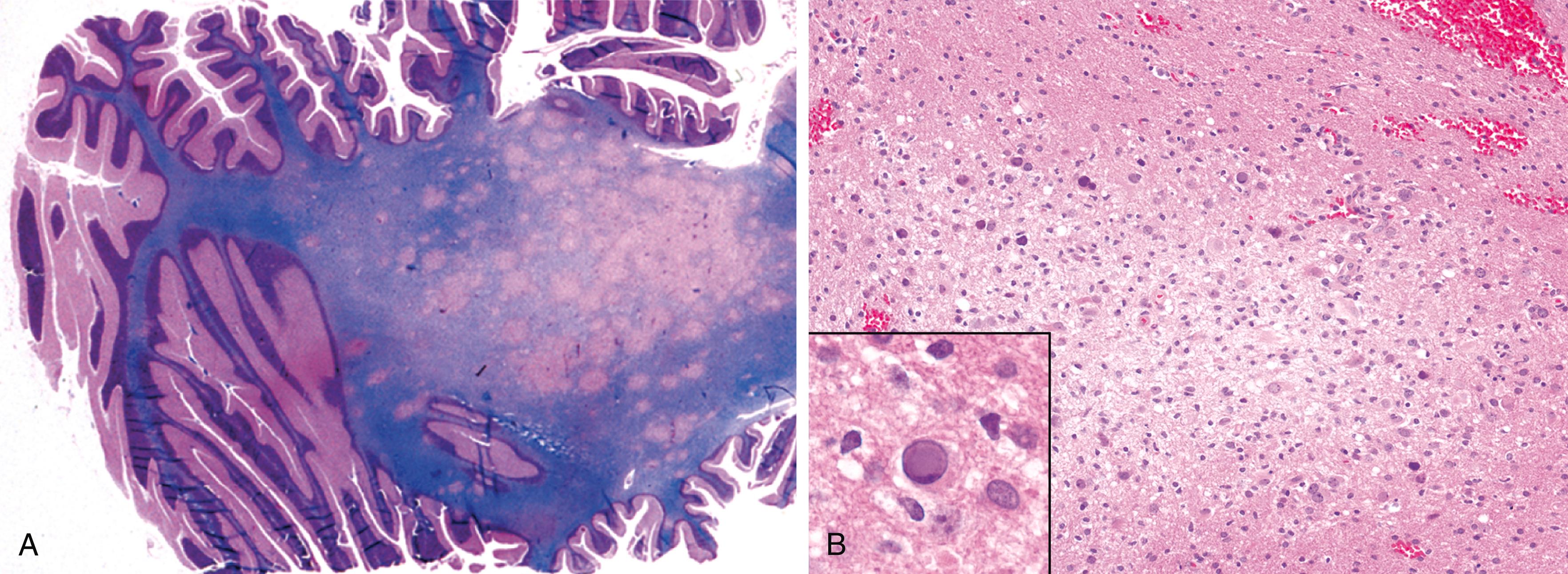
Cryptococcus neoformans and Cryptococcus gattii both may cause meningitis and meningoencephalitis. C. neoformans mainly produces disease in the setting of immunocompromise, whereas C. gattii often causes disease in immmunocompetent individuals, usually accompanied by pulmonary involvement ( Chapter 11 ). CNS involvement by both organisms may be fulminant and fatal in as little as 2 weeks or may be indolent, evolving over months or years. The CSF may have few cells but elevated protein. The mucoid encapsulated yeasts can be visualized on India ink preparations or detected using cryptococcal antigen tests. Extension into the brain follows vessels in the Virchow-Robin spaces. As organisms proliferate, these spaces expand, giving rise to a “soap bubble”–like appearance ( eFig. 21.3 ).
Histoplasma capsulatum commonly involves the nervous system in the setting of disseminated infection. There is an increased risk for disease in the setting of HIV infection. Histoplasmosis (like tuberculosis) typically causes a basilar meningitis, with elevated CSF protein, mildly decreased glucose, and mild lymphocytic pleocytosis. Parenchymal lesions can occur, mostly from tracking of organisms along Virchow-Robin spaces.
Coccidioides immitis, a fungus endemic to desert regions of the American Southwest, most commonly causes meningitis in the setting of disseminated infection. Diagnosis can be made by examining the CSF for specific antibodies or by antigen detection. Without treatment, coccidioidal meningitis has a high fatality rate.
The entire spectrum of infectious pathogens (viruses to parasites) can infect the brain, often producing characteristic lesions. In general, viral infections are diffuse, bacterial infections (when not associated with meningitis) are more localized, and other organisms produce mixed patterns. In immunocompromised individuals, widespread involvement with any agent is typical.
A brain abscess is a localized focus of necrotic brain tissue with accompanying inflammation, usually caused by a bacterial infection. Abscesses can arise by direct implantation of organisms, local extension from adjacent foci (e.g., mastoiditis, paranasal sinusitis), or hematogenous spread (usually from a primary site in the heart, lungs, or distal bones). Predisposing conditions include acute bacterial endocarditis, from which septic emboli are released that may produce multiple abscesses; cyanotic congenital heart disease, associated with a right-to-left shunt and loss of pulmonary filtration of organisms; and chronic pulmonary infections, as in bronchiectasis, which provide a source of microbes that spread hematogenously.
Abscesses are discrete destructive lesions with central liquefactive necrosis surrounded by edema ( Fig. 21.17 ). At the outer margin of the necrotic lesion, there is exuberant granulation tissue with neovascularization. The newly formed vessels are abnormally permeable, accounting for marked edema in the adjacent brain tissue. Patients often present with progressive focal neurologic deficits; signs and symptoms related to increased intracranial pressure may also develop. Typically, the CSF has a high white cell count and an increased protein concentration, but the glucose content is normal. The source of infection may be apparent or may be traced to a small (extracranial) focus that is not symptomatic. Increased intracranial pressure can lead to fatal herniation; other complications include abscess rupture with ventriculitis or meningitis, and venous sinus thrombosis. With surgery and antibiotic treatment, the otherwise high mortality rate can be reduced to less than 10%.
Viral encephalitis is a parenchymal infection of the brain that is almost invariably associated with meningeal inflammation (meningoencephalitis). While different viruses show varying patterns of injury, the most characteristic histologic features are perivascular and parenchymal mononuclear cell infiltrates ( Fig. 21.18 A ), microglial nodules ( Fig. 21.18 B), and neuronophagia. Certain viruses also form characteristic inclusion bodies. CSF examination helps to distinguish viral from bacterial infections of the CNS. The CSF usually shows a slightly elevated pressure and an early neutrophilic pleocytosis that rapidly converts to a lymphocytosis; the protein concentration is elevated, but glucose is normal.
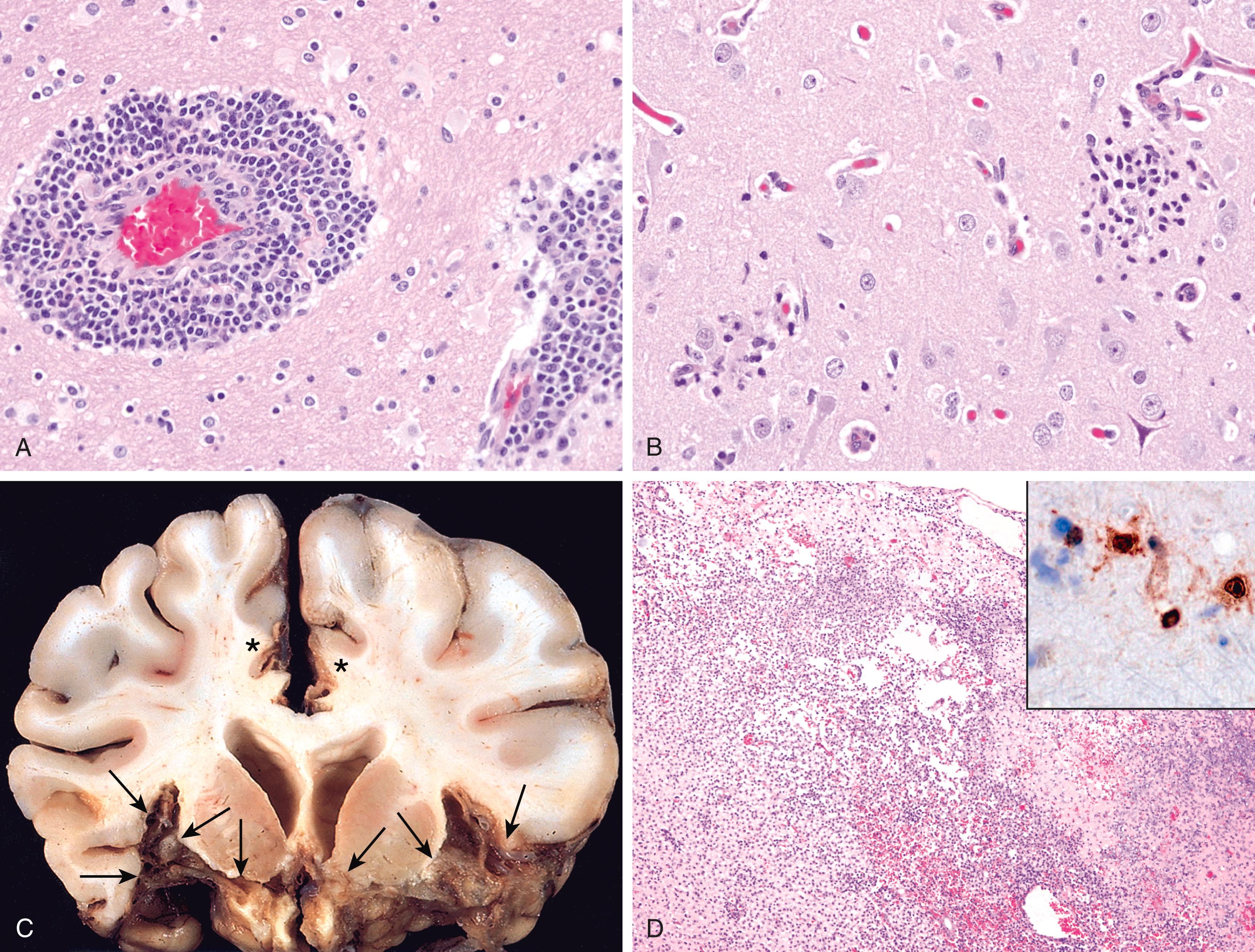
The nervous system is particularly susceptible to certain viruses such as rabies virus and poliovirus. Some viruses infect specific CNS cell types, while others preferentially involve particular brain regions (e.g., medial temporal lobes, limbic system) that lie along the viral route of entry. Intrauterine viral infection following transplacental spread of rubella and CMV may cause destructive lesions, and Zika virus causes developmental abnormalities of the brain. In addition to direct infection of the nervous system, the CNS can also be injured by immune mechanisms after systemic viral infections.
Arboviruses (arthropod-borne viruses) are an important cause of epidemic encephalitis, especially in tropical regions of the world, and are capable of causing serious morbidity and high mortality. Among the more commonly encountered types are Eastern and Western equine encephalitis and West Nile virus infection. Patients develop generalized neurologic symptoms, such as seizures, confusion, delirium, and stupor or coma, as well as focal signs, such as reflex asymmetry and ocular palsies.
Arbovirus encephalitides produce a similar histopathologic picture. Characteristically, there is a perivascular lymphocytic meningoencephalitis (sometimes with neutrophils). Multifocal gray matter and white matter necrosis is seen, often associated with neuronophagia ( eFig. 21.4 ), the phagocytosis of neuronal debris, as well as microglial nodules (see Fig. 21.1 C). In severe cases, there may be a necrotizing vasculitis with associated focal hemorrhages. FLOAT NOT FOUND
HSV-1 encephalitis may occur in any age group but is most common in children and young adults. It typically manifests with alterations in mood, memory, and behavior, reflecting involvement of the frontal and temporal lobes. Recurrent HSV-1 encephalitis is sometimes associated with inherited mutations that interfere with Toll-like receptor signaling (specifically that of TLR-3), which has an important role in antiviral defense.
Herpes encephalitis starts in and most severely affects the inferior and medial regions of the temporal lobes and the orbital gyri of the frontal lobes ( Fig. 21.18 C). The infection is necrotizing and often hemorrhagic in severely affected regions. Perivascular inflammatory infiltrates are usually present ( Fig. 21.18 D), and large eosinophilic intranuclear viral inclusions (Cowdry type A bodies) can be found in both neurons and glial cells.
HSV-2 also affects the nervous system. This usually takes the form of meningitis in adults, whereas disseminated severe encephalitis may occur in neonates born by vaginal delivery to women with active primary HSV genital infections.
Varicella-zoster virus (VZV) causes chickenpox during primary infection, usually without any evidence of neurologic involvement. The virus establishes latent infection in neurons of dorsal root ganglia. Reactivation in adults results in inflammation and neuronal damage in sensory ganglia. It manifests as neuropathic pain and a painful, vesicular skin eruption in the distribution of one or a few dermatomes (shingles). This is usually a self-limited process, but there may be a persistent pain syndrome in the affected region (postherpetic neuralgia). VZV also may cause a granulomatous arteritis that can lead to tissue infarcts. In patients who are immunocompromised, acute herpes zoster encephalitis can occur. Inclusion bodies can be found in glial cells and neurons.
CMV infects the nervous system of fetuses and individuals who are immunocompromised. All cells within the CNS (neurons, glial cells, ependyma, and endothelium) are susceptible to infection. Intrauterine infection causes periventricular necrosis, followed later by microcephaly with periventricular calcification. When adults are infected, CMV produces a subacute encephalitis, which is also often most severe in the periventricular region. Lesions can be hemorrhagic and contain cells with typical viral inclusions ( eFig. 21.5 ).
Poliovirus is an enterovirus that most often causes a subclinical or mild gastroenteritis; in a small fraction of cases, it secondarily invades the nervous system and damages motor neurons in the spinal cord and brain stem (paralytic poliomyelitis) . The loss of motor neurons results in a flaccid paralysis with muscle wasting and hyporeflexia in the corresponding region of the body. In the acute disease, death can occur from paralysis of respiratory muscles. Long after the infection has resolved, typically 25 to 35 years after the initial illness, a poorly understood postpolio syndrome of progressive weakness associated with decreased muscle bulk and pain may appear. The re-emergent weakness has the same distribution as the prior polio infection. With worldwide vaccination, polio has been nearly eliminated but still persists in underresourced parts of Pakistan and Afghanistan. Additionally, in parts of the world in which endemic polio has been eliminated, such as Africa, back-mutation of the attenuated virus in oral vaccines has produced small numbers of cases of paralytic polio acquired through contaminated drinking water.
Rabies is a severe encephalitis usually transmitted to humans by the saliva of a rabid animal, including dogs, bats, or various wild mammals that are natural reservoirs. According to the WHO, about 60,000 people die of canine rabies worldwide each year. The virus enters the CNS by ascending along the peripheral nerves from the wound site, so the incubation period (usually 1 to 3 months) depends on the distance between the wound and the brain. The disease manifests initially with nonspecific symptoms of malaise, headache, and fever. As the infection advances, the patient shows extraordinary CNS excitability; the slightest touch is painful, with violent motor responses progressing to convulsions. Contracture of the pharyngeal musculature may create an aversion to swallowing even water (hydrophobia). Periods of mania and stupor progress to coma and eventually death in virtually all cases, typically from respiratory failure.
Before the availability of effective antiretroviral therapy, neuropathologic changes were demonstrated at postmortem examination in as many as 80% to 90% of AIDS cases. These changes stem from direct effects of the virus on the nervous system, opportunistic infections, and primary CNS lymphoma, most commonly an EBV-positive B-cell tumor. There has been a decrease in the frequency of these secondary effects of HIV infection due to the efficacy of multidrug antiretroviral therapy. HIV-associated neurocognitive disorder (HAND), a cognitive dysfunction ranging from mild to full-blown dementia, continues to be a source of morbidity, however. This syndrome is believed to stem from HIV infection of microglial cells in the brain and activation of innate immune responses. Neuronal injury likely stems from a combination of cytokine-induced inflammation and toxic effects of HIV-derived proteins.
Aseptic meningitis occurs within 1 to 2 weeks of onset of primary HIV infection in about 10% of patients; antibodies to HIV can be demonstrated, and the virus can be isolated from the CSF. The few neuropathologic studies of the early, acute phases of symptomatic or asymptomatic HIV invasion of the nervous system have shown mild lymphocytic meningitis, perivascular inflammation, and some myelin loss in the hemispheres.
When effective anti-HIV therapy is begun in the setting of established infection, there is a risk for a neurologic disorder called immune reconstitution inflammatory syndrome (IRIS). Neurologic manifestations include rapidly developing cognitive impairment and cerebral edema. The pathogenesis of IRIS is unclear, but it is thought to be due to the activation of a previously suppressed inflammatory response brought about by effective treatment of HIV infection. IRIS is often associated with the presence of a mycobacterial, fungal, or viral opportunistic CNS infection, although it can also occur in the absence of any other inciting disease.
HIV encephalitis is a chronic inflammatory process with widely distributed microglial nodules, sometimes with associated foci of tissue necrosis and reactive gliosis. The microglial nodules are also found in the vicinity of small blood vessels, which show abnormally prominent endothelial cells and perivascular foamy or pigment-laden macrophages. These changes are especially prominent in the subcortical white matter, diencephalon, and brain stem. An important component of microglial nodules is macrophage-derived multinucleate cells. In some cases, there is also a disorder of white matter characterized by multifocal or diffuse areas of myelin loss, axonal swellings, and gliosis. HIV is present in CD4+ mononuclear and multinucleate macrophages and microglia.
Unlike HIV encephalitis, the brain lesions of IRIS may be associated with a CD8+ T-cell infiltrate, both around blood vessels and diffusely in the parenchyma, in the absence of significant HIV burden or multinucleated cells.
Progressive multifocal leukoencephalopathy (PML) is caused by JC virus, a polyomavirus, which preferentially infects oligodendrocytes, resulting in demyelination as the injured cells die. Most people show serologic evidence of exposure to JC virus during childhood, and it is believed that PML results from virus reactivation, as the disease is restricted to individuals who are immunocompromised. Patients develop relentlessly progressive neurologic signs and symptoms, and imaging studies show extensive, often multifocal lesions in the hemispheric or cerebellar white matter. There is no specific treatment and the disease is usually fatal in less than a year.
The lesions are patchy, irregular, ill-defined areas of white matter destruction that enlarge as the disease progresses ( Fig. 21.19 ). Each lesion is an area of demyelination, in the center of which are scattered lipid-laden macrophages and a reduced number of axons. At the edges of the lesion are greatly enlarged oligodendrocyte nuclei whose chromatin is replaced by glassy amphophilic viral inclusions. The virus also infects astrocytes, leading to bizarre giant forms with irregular, hyperchromatic, sometimes multiple nuclei that can be mistaken for a tumor.
Fungal infections usually produce parenchymal granulomas or abscesses, often associated with meningitis. The most common fungal infections have the following distinctive patterns:
Candida albicans usually produces multiple microabscesses, with or without granuloma formation.
Mucormycosis, caused by several fungi belonging to the order Mucorales, typically presents as an infection of the nasal cavity or sinuses in a patient who has diabetes and ketoacidosis. It may spread to the brain through vascular invasion or by direct extension through the cribriform plate. The proclivity of Mucor to invade the brain directly sets it apart from other fungi, which reach the brain by hematogenous dissemination from distant sites.
Aspergillus fumigatus tends to cause a distinctive pattern of widespread septic hemorrhagic infarctions because of its marked predilection for blood vessel wall invasion with subsequent thrombosis.
While a wide range of other organisms can infect the nervous system and its covering, only three of the most common entities are considered here.
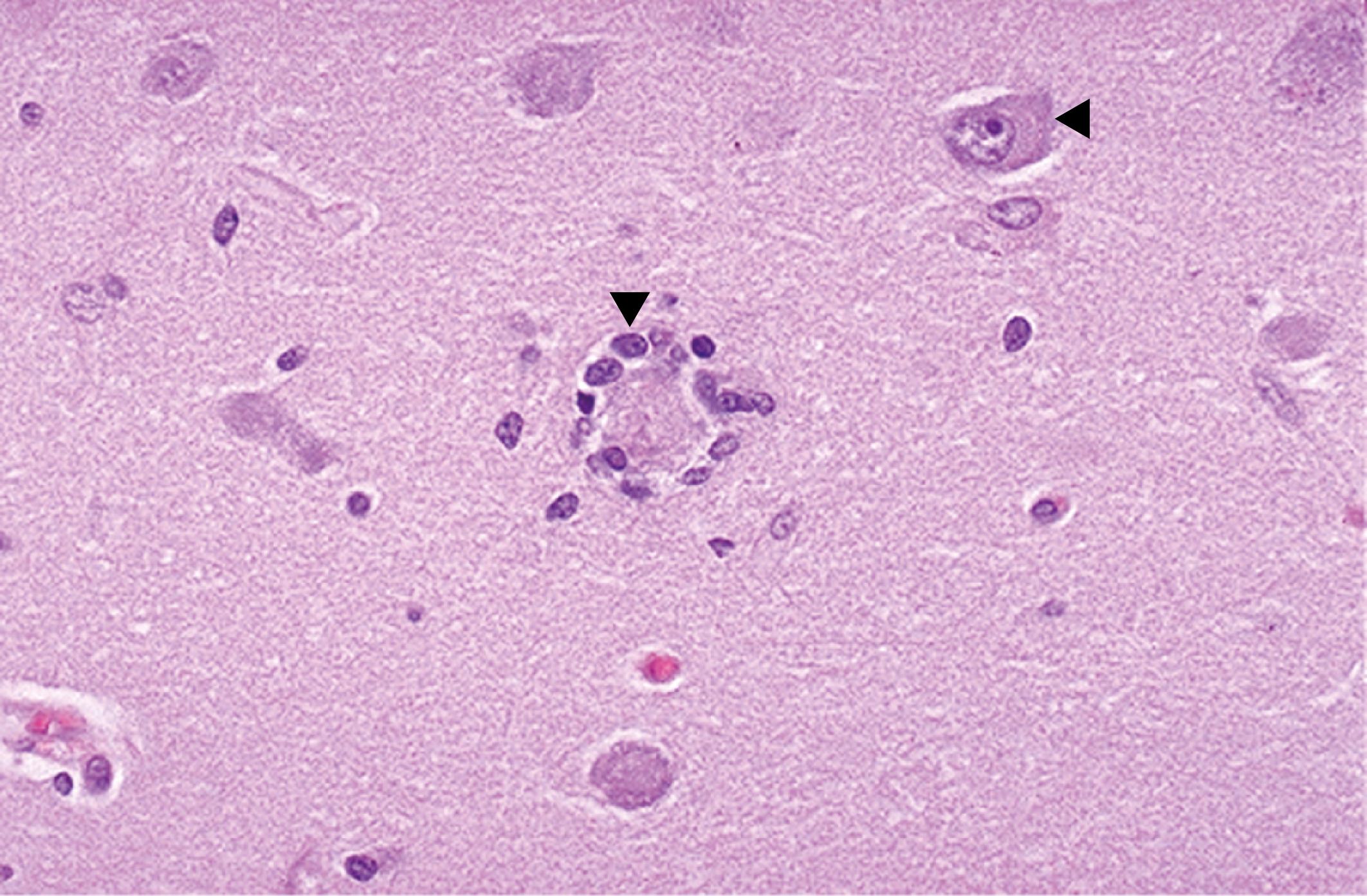
Cerebral infection with the protozoan Toxoplasma gondii can occur in adults who are immunocompromised or in newborns who acquire the organism transplacentally from a mother with an active infection. The consequences include the triad of chorioretinitis, hydrocephalus, and intracranial calcifications . In adults, the clinical symptoms are subacute, evolving over weeks, and may be both localizing and diffuse. Due to inflammation and breakdown of the blood-brain barrier at sites of infection, imaging studies often show edema associated with ring-enhancing lesions.
When the infection is acquired in adults who are immunocompromised, the brain shows abscesses, frequently multiple, most often involving the cerebral cortex (near the gray-white junction) and deep gray nuclei. Acute lesions consist of central foci of necrosis surrounded by acute and chronic inflammation, macrophage infiltration, and vascular proliferation. Both free tachyzoites and encysted bradyzoites may be found at the periphery of the necrotic foci ( eFig. 21.6 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here