Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Rheumatic heart disease (RHD) remains the most common cause of multivalvular heart disease worldwide, and a major cause of cardiac morbidity and mortality in low- and middle-income countries.
The definitive management of patients with advanced rheumatic valvular disease includes replacement, repair, or mechanical opening of stenotic valves by either percutaneous (catheter-based) or surgical means. Appropriate management of sequelae such as atrial fibrillation and heart failure is also an essential component of the comprehensive care of such patients. Meticulous evaluation to establish an accurate pathological and hemodynamic diagnosis is needed to plan appropriate surgical or interventional therapy. As described in Chapter 5 , the diagnosis of RHD is based on the combination of clinical history and examination, review of the electrocardiogram (ECG) and chest X-ray, and transthoracic echocardiography. Both transesophageal echocardiography and catheter-based invasive investigation may aid assessment of severity of RHD.
Before the advent of modern echocardiography, cardiac catheterization was considered an essential step before valve surgery. Invasive evaluation was used: (1) to confirm the diagnosis and severity of valve disease; (2) to assess for the presence and severity of coexistent valve disease; (3) to document the presence and severity of pulmonary hypertension; (4) to estimate left ventricular function; and (5) for the evaluation of coexisting coronary artery disease (CAD). Currently, the role of catheterization is much more restricted given the ability of echocardiography to provide many of the answers to these clinical questions.
There is limited published data about the availability of catheter laboratories in RHD endemic regions of the world, nor of volume, outcome, and impact of procedures performed where they do exist. However, it is reasonable to assume that the consequences of limited access to the sometimes lifesaving and life-prolonging catheter-based approaches to the diagnosis and treatment of RHD likely mirror those of the limited capacity for cardiac surgery in the same regions of the world.
In this chapter, we provide an overview of the role of catheter-based investigation and treatment in patients with RHD. Specifically, we will review the indications for catheter-based evaluation, how to perform/technical aspects of the procedure, and discuss interpretation of the information obtained. We also discuss the indications for percutaneous mitral balloon commissurotomy (PMBC) and the role of aortic valvuloplasty and transcutaneous aortic valve implantation (TAVI) in patients with RHD.
Catheter-based measurements remain the gold standard for the evaluation of intracardiac chamber and vascular pressures, measuring pressure gradients across valves and between chambers, determining hemodynamic blood flow, stroke volume (SV), and cardiac output (CO), and providing direct accurate measures of oxygen content and saturation in all the chambers. Cardiac catheterization is therefore indicated: whenever there is a discrepancy between clinical information obtained from noninvasive evaluation (history, physical examination, ECG, chest X-ray and echocardiography); when there is doubt about the accuracy of the measured pulmonary artery pressure (PAP); when there is uncertainty regarding the severity of valve disease (common in cases of multivalvular involvement); and where echocardiography windows are poor and the quality of images do not allow for satisfactory analysis and interpretation.
Cardiac catheterization for full hemodynamic and valvular assessment in patients with RHD requires both arterial (for aortic and left ventricular pressure recording) and venous access (for right heart hemodynamics). Historically, femoral arterial and venous access were the most commonly used access routes. However, with growing evidence of improved safety and effectiveness of radial arterial access, it is likely that the use of radial/axillary vein or radial/femoral vein combinations will increase globally.
Before the procedure, the fluid-filled pressure lines should be attached properly to a pressure transducer at one end and to the side port of a manifold attached to the cardiac catheter at the other, with the height of the transducer fixed to correspond with that of the patient's heart (approximately the midaxillary line, phlebostatic axis). The pressure lines should be clear of air bubbles and kinks and any radiographic contrast medium or blood should be flushed out from the tubing and the catheters to ensure proper pressure measurement and minimization of errors.
An end-hole catheter such as the Swan-Ganz catheter (a balloon floatation end-hole catheter) is the catheter of choice for right heart catheterization due to the advantage of easy positioning and accurate measurement of pulmonary capillary wedge pressure (PCWP). Alternative catheters that are often used include stiffer end-hole catheters (e.g., Lehman, Cournand and Judkins right catheters). The use of end-hole catheters is particularly important when measurement of the PCWP is required (most right heart studies) as side-hole catheters such as NIH and Bermann catheters may introduce significant measurement error. Where severe tricuspid regurgitation is present, operators may experience difficulty with access to the right ventricle (RV) using balloon floatation catheters. Ventricle and stiffer nonballoon floatation catheters such as the Judkins right coronary catheter or the use of an over a wire technique may help.
By convention, the right heart study measurements (see Table 7.1 ) are obtained before the left heart catheterization. Measurement of ventricular and aortic pressures and gradients are obtained using a pigtail catheter due to its atraumatic tip. However, if coronary angiography is to be undertaken, it is reasonable to start with coronary angiography before entering the left ventricle (LV) to reduce the risk of embolic complications.
The catheter procedure should aim to acquire:
|
The atrial pressure waveform consists of three positive waves ( a, c, and v waves) and two negative waves (x and y descent) ( Fig. 7.1 ). Atrial contraction corresponds with the a wave and follows the P wave on the ECG. The a wave is followed by the x descent, which represents atrial relaxation and downward pulling of the tricuspid annulus as the RV contracts. The x descent is interrupted by a transient pressure increase, known as the c wave, which is caused by bulging of the closed tricuspid valve into the RA during right ventricular contraction. Both the a wave and x descent are absent in cases with atrial fibrillation. Passive atrial filling terminates the x descent which is followed by the v wave, which occurs near the end of (right) ventricular systole (the peak of atrial pressure). Opening of the tricuspid valve releases blood from the RA to the RV, resulting in a drop in atrial pressure and the final wave known as the y descent. The waveforms are similar for the left and the right atria, albeit that the mean pressures are slightly higher in the left atrium (LA), and the LA has a more prominent v wave.
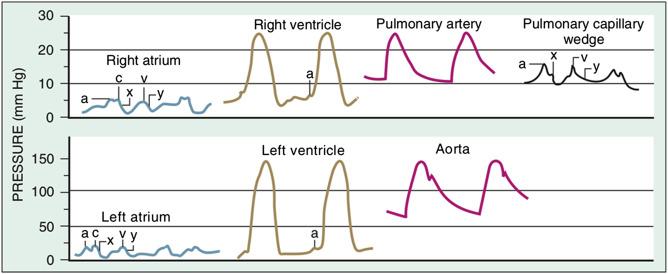
The ventricular pressure waveform ( Fig. 7.1 ) consists of a systolic and a diastolic phase. The systolic ejection phase begins with a steep rapid rise after the opening of the semilunar valve. The systolic ejection peak pressure occurs when the ventricular pressure equals the peak pressure of the connected great vessel. Both pressures then fall; the great vessel pressure falls to its nadir as diastole begins. The dicrotic notch is observed on the ventricular waveform that corresponds to the closure of the semilunar valves. The ventricular pressure then descends to close to zero, assuming no abnormalities of ventricular relaxation and compliance. Ventricular diastolic pressure typically consists of three independent phases: an energy-dependent early rapid filling phase; a period of passive ventricular filling called diastasis; and the final filling phase that corresponds to atrial systole and active emptying of the atria into the ventricle before AV valve closure.
An important aim of a well-performed hemodynamic study is to obtain and record all pressures within a short time span to avoid significant changes in hemodynamics that may occur over time. It is highly recommended to record simultaneous pressures for calculation of gradients across the mitral valve. Gradients across the tricuspid, pulmonary, and aortic valves are usually obtained as “pullback” measurements across the valve. Artifactual pressure waveform recordings can cause false readings. Common artifacts include damping artifacts when catheters have not been flushed correctly; errors in zeroing and calibration; and peripheral systolic pressure amplification due to summation of the reflected wave.
Blood samples should be taken from all appropriate cardiac chambers and blood vessels for oxygen saturation as they are required for the hemodynamic calculations. At a minimum, samples should include blood from the pulmonary artery (PA) (where venous blood from the superior vena cava, inferior vena cava, and coronary sinus are all mixed) and aorta. The samples should be collected in 2 mL heparinized syringes for the purpose of measurement of CO by Fick's method and should be analyzed promptly to reduce error. Care should be taken to avoid any air bubbles in the sample. The spectrophotometric method may produce inaccurate results in the presence of abnormal hemoglobin. Reflectance oximetry is commonly used and is accurate if the oxygen saturation range is from 45% to 98%. However, reliability decreases below 40% saturation, which is seen in mixed venous samples in low CO states and cyanotic congenital heart disease.
The PCWP, which is a surrogate of the left atrial pressure (LAP), is best measured with an end-hole catheter (often a Swan-Ganz catheter). This is placed in a distal branch of the PA with the inflated balloon completely occluding the antegrade flow, thus forming a continuum of blood between the distal PA, the pulmonary capillaries, and the pulmonary venous system draining into the LA. Although the PCWP waveform is similar to that from the atria ( Fig. 7.1 ), it is delayed by as much as 50–150 ms due to the transmission through the pulmonary capillary bed and often appears more damped. These important differences need to be kept in mind when PCWP is used as a surrogate for LAP while valve gradient calculations are determined in mitral stenosis.
The ideal PCWP trace should have well defined a and v waves, a mean pressure that is equal to or less than the PA diastolic pressure, and an oxygen saturation of ≥95% (in the absence of pulmonary parenchymal diseases that distort normal gas exchange). Accurate measurement of the PCWP may be difficult to obtain as both over inflation and under inflation of the catheter balloon remain common source of errors. Over inflation leads to dampening of the pressure waveforms and underinflation leads to transmittance of the PAP and the overestimation of PCWP.
The two most frequently used methods for estimating the CO are the Fick and thermodilution method. Using the Fick principle, the CO is calculated by dividing oxygen consumption (VO 2 ) by the arteriovenous oxygen difference, where the latter is assumed based on age, sex, and body surface area. Although discrepancies may exist between the measured and estimated VO 2 , direct measurement of VO 2 is rarely performed as it is technically demanding, time consuming, and expensive. Blood samples from the aorta and the PA (mixed venous sample) are used to calculate the arteriovenous oxygen difference ( Box 7.1 ). The Fick method looses accuracy in patients with significant mitral regurgitation or AR and should not be used in these conditions. It remains accurate however in low CO and tricuspid regurgitation.
The thermodilution technique uses specific catheters (such as the Swan-Ganz), which allow for the downstream placement of a thermistor in the PA to measure the temperature change (increase) of a fixed volume of cold saline injected into a proximal port. Automated complex calculations give the value of CO depending upon the temperature change noted at the distal thermistor. The major advantage of this technique is that it has significantly less measurement variability and better reliability compared to Fick's method. However, the thermodilution method becomes unreliable in the presence of intracardiac shunts, low flow states, in those with atrial fibrillation or severe tricuspid regurgitation.
In patients with RHD, the catheter study allows determination of the nature and severity of the valve abnormality (stenosis, regurgitation, or both). The severity of stenotic valves is judged by the valve area and pressure gradients across the valves and the hemodynamic sequelae of the valve abnormality (ventricular and LAPs, etc.). The interpretation of any hemodynamic changes may include changes in the atrial and ventricular waveform exerted by the effect of isolated or multiple valvular lesions. As a rule, the hemodynamic abnormalities are dominated by the effect of the more proximal lesion and the lesion greater in severity.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here