Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Bundle branch reentry ventricular tachycardia (BBRVT), first elucidated by Guerot and colleagues in 1974, is a unique, usually fast (200–300 beats/min), monomorphic tachycardia associated with hemodynamic collapse, syncope, and/or cardiac arrest. It has also been described as a mechanism for nonsustained VT and coupled ventricular ectopy. , BBRVT is caused by a macroreentrant circuit involving the right and left bundle branches, an upper common pathway, and septal ventricular muscle. BBR occurs in patients who have dilated cardiomyopathy and in those with coronary artery disease, valvular heart disease, , muscular dystrophy, congenital heart disease, left ventricular noncompaction, endocardial fibrosis, arrhythmogenic right ventricular (RV) cardiomyopathy, Chagas disease, Brugada syndrome, or even no structural heart disease but with evident His-Purkinje system dysfunction. BBRVT after valvular surgery and transcatheter aortic valve replacement has been also reported. The incidence was reported to be 3.5% and 6% of VTs in separate series and 20% in a series of patients with nonischemic cardiomyopathy alone undergoing evaluation for ablation. Likely, BBRVT is underrecognized as a clinical problem. A high incidence of BBRVT has been reported in patients on ventricular assist device support. , ,
The QRS morphology of the tachycardia can have a typical left bundle branch block (LBBB) pattern ( Fig. 84.1A ) or right bundle branch block (RBBB) pattern (see Fig. 84.1B ). Some patients have both counterclockwise and clockwise BBR, causing an LBBB and RBBB morphology, respectively. , It is possible for LBBB morphology BBRVT to have more than one LBBB QRS configuration, presumably as the result of varying exits from an extensively diseased RBB in patients with dilated hearts. RBBB BBRVT can also have multiple monomorphic morphologies as anterograde conduction via the left anterior fascicle (LAF) or left posterior fascicle (LPF) can be present along with retrograde activation of the RBB. BBRVT with multiple morphologies has also been described in Ebstein anomaly. Further, a narrow QRS complex BBR has been postulated to occur via longitudinal dissociation in the His-RBB system allowing simultaneous retrograde and anterograde activation of the RBB.
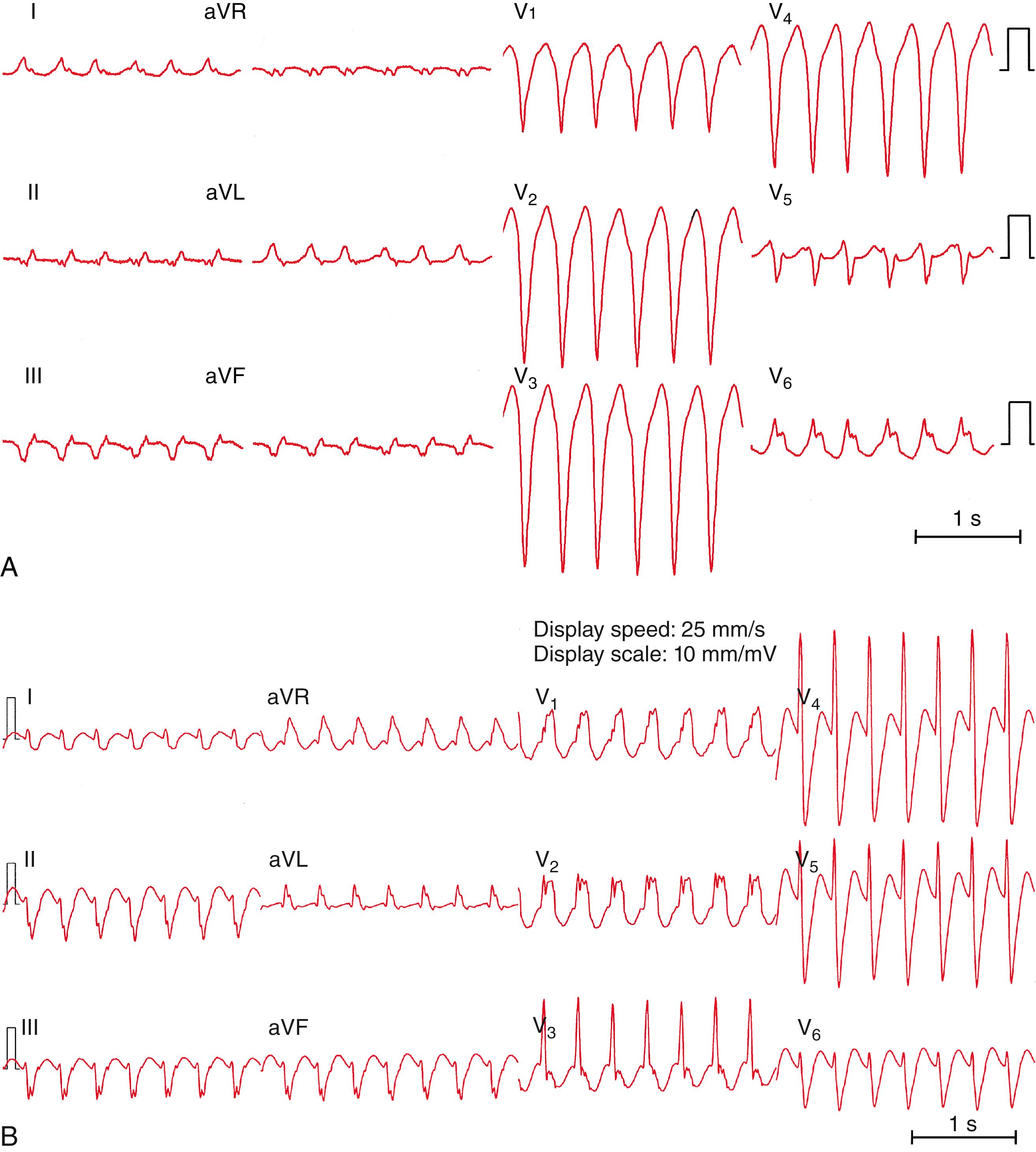
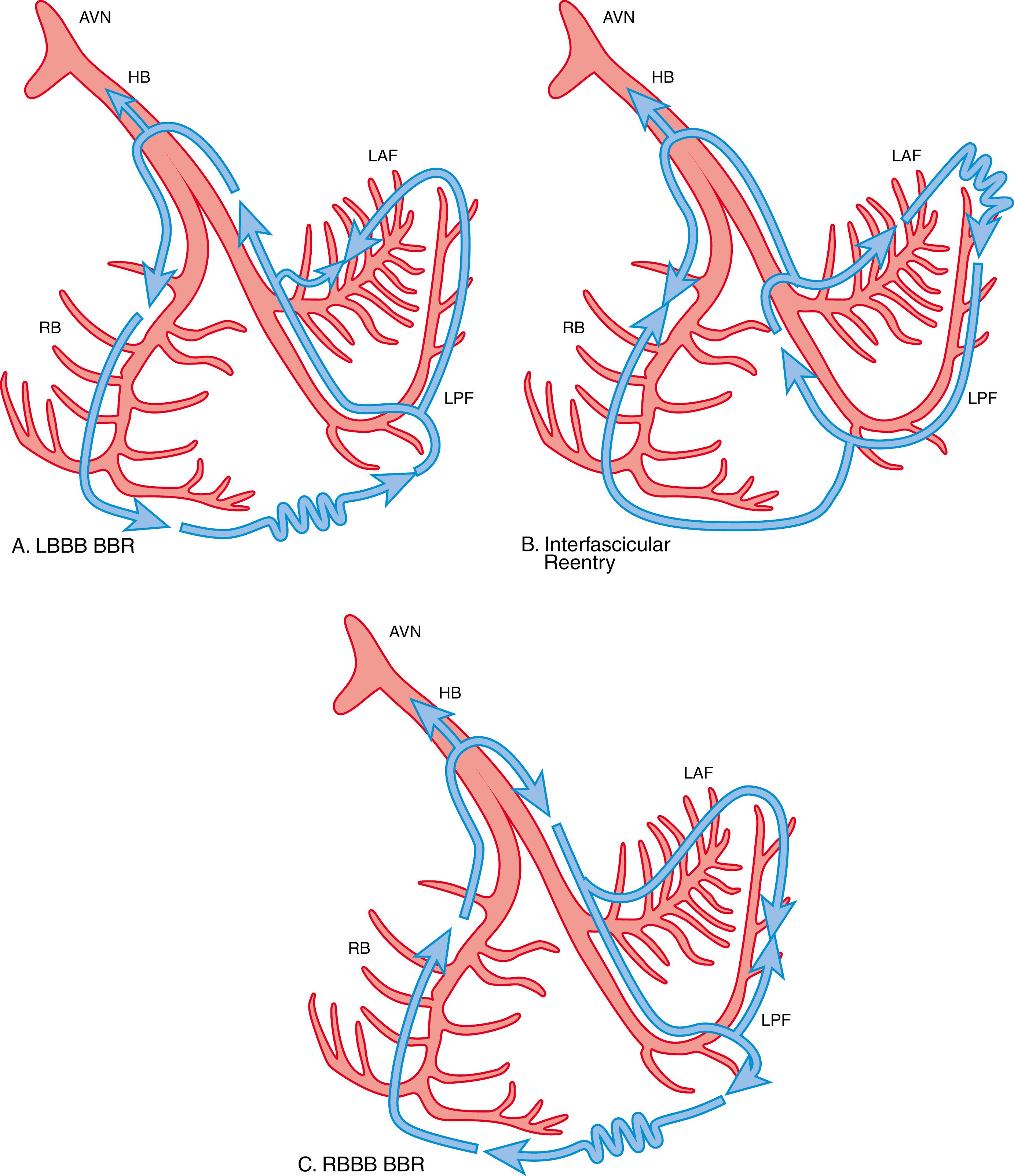
Tchou and colleagues described three categories of BBRVT ( Table 84.1 ; Fig. 84.2 ). Types A and C are the classic counterclockwise and clockwise BBRVT circuits, respectively. Type B is reentry within the LBB fascicles (interfascicular reentry). BBR can present with a similar, or identical, QRS complex morphology to that present in normal sinus rhythm. Although the QRS complex morphology in VT can be identical to that in sinus rhythm in all 12 electrocardiogram (ECG) leads, not all such VTs are BBR. An RBBB and left hemiblock pattern is more consistent with interfascicular reentry tachycardia (see Fig. 84.1C ).
| Type A | Type B (Interfascicular Tachycardia) | Type C | |
|---|---|---|---|
| ECG morphology | LBBB pattern | RBBB and left hemiblock pattern | RBBB pattern |
| Anterograde limb | RBB | LAF or LPF | LBB |
| Retrograde limb | LBB | Contra-left fascicle | RBB |
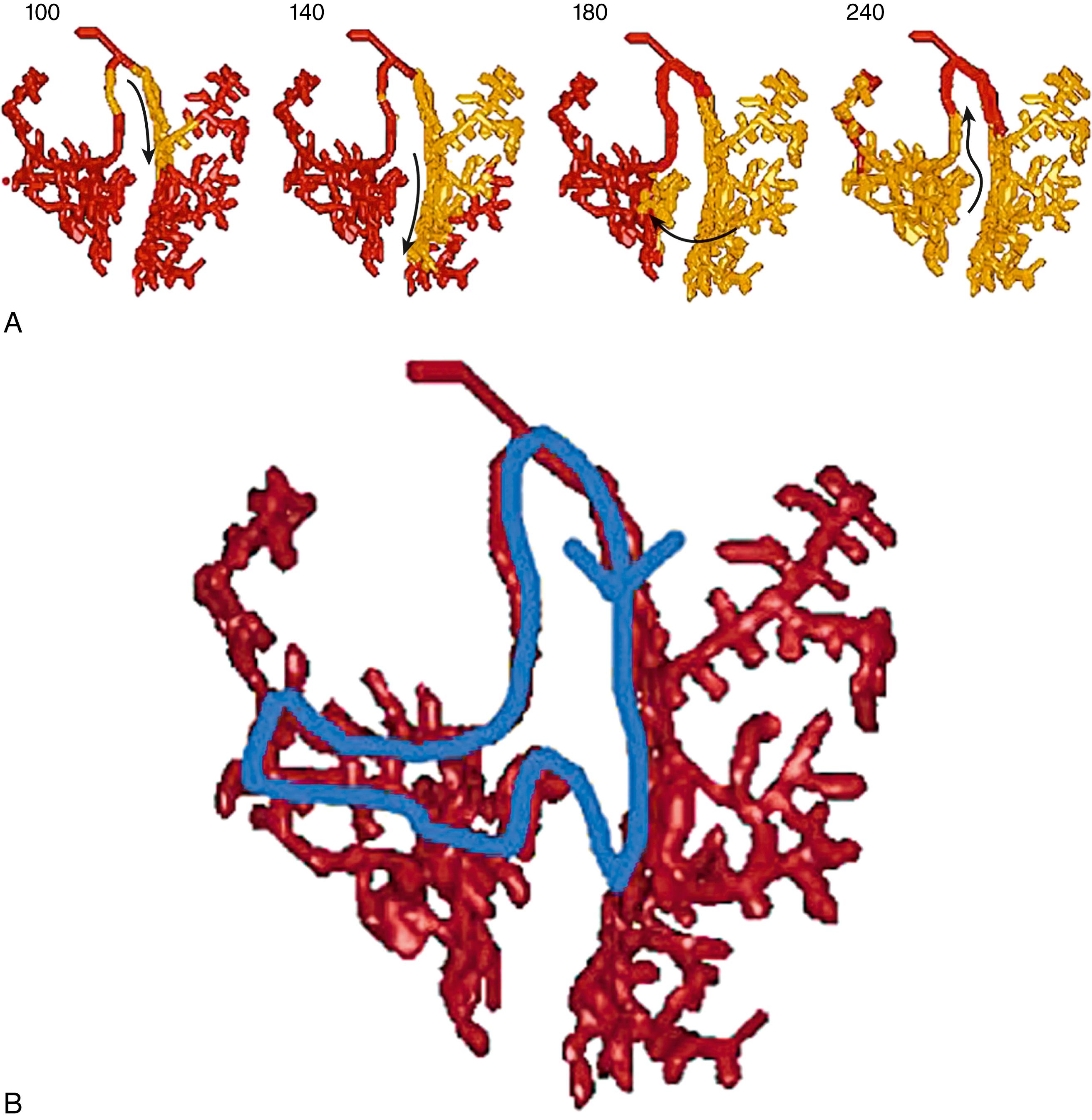
Attempts have been made to model the His-Purkinje system and to define the reentrant circuit(s) responsible for BBR. Under normal conditions, sustained reentry cannot occur, but under conditions of slowed conduction in the His-Purkinje system and ventricular muscle, the path length can be increased such that sustained anatomic reentry does occur using these structures and with an excitable gap ( eFig. 84.1 ).
Patients with BBR generally have a prolonged PR interval, QRS duration, and H-V interval. For BBR to occur, there must be a delay or complete anterograde block in at least one bundle branch. An LBBB (most commonly) or an RBBB present on the surface 12-lead ECG is more indicative of conduction slowing than of complete block in LBB or the RBB, respectively. If complete anterograde block is present in one bundle branch, there must be conduction (likely slow) retrograde in that bundle branch for BBRVT to occur.
During type A BBRVT, activation proceeds anterograde via the RBB and then through the septum. After this, retrograde conduction via the LBB activates the septal summit/His bundle and sequentially reactivates the RBB (“counterclockwise” reentry). The ECG morphology of counterclockwise BBRVT (type A) is a typical LBBB with an R wave transition between leads V 4 and V 5 . Type A BBRVT with an LBBB morphology is the cause of 98% of BBRVT episodes. The LBB may be the preferred retrograde route of activation.
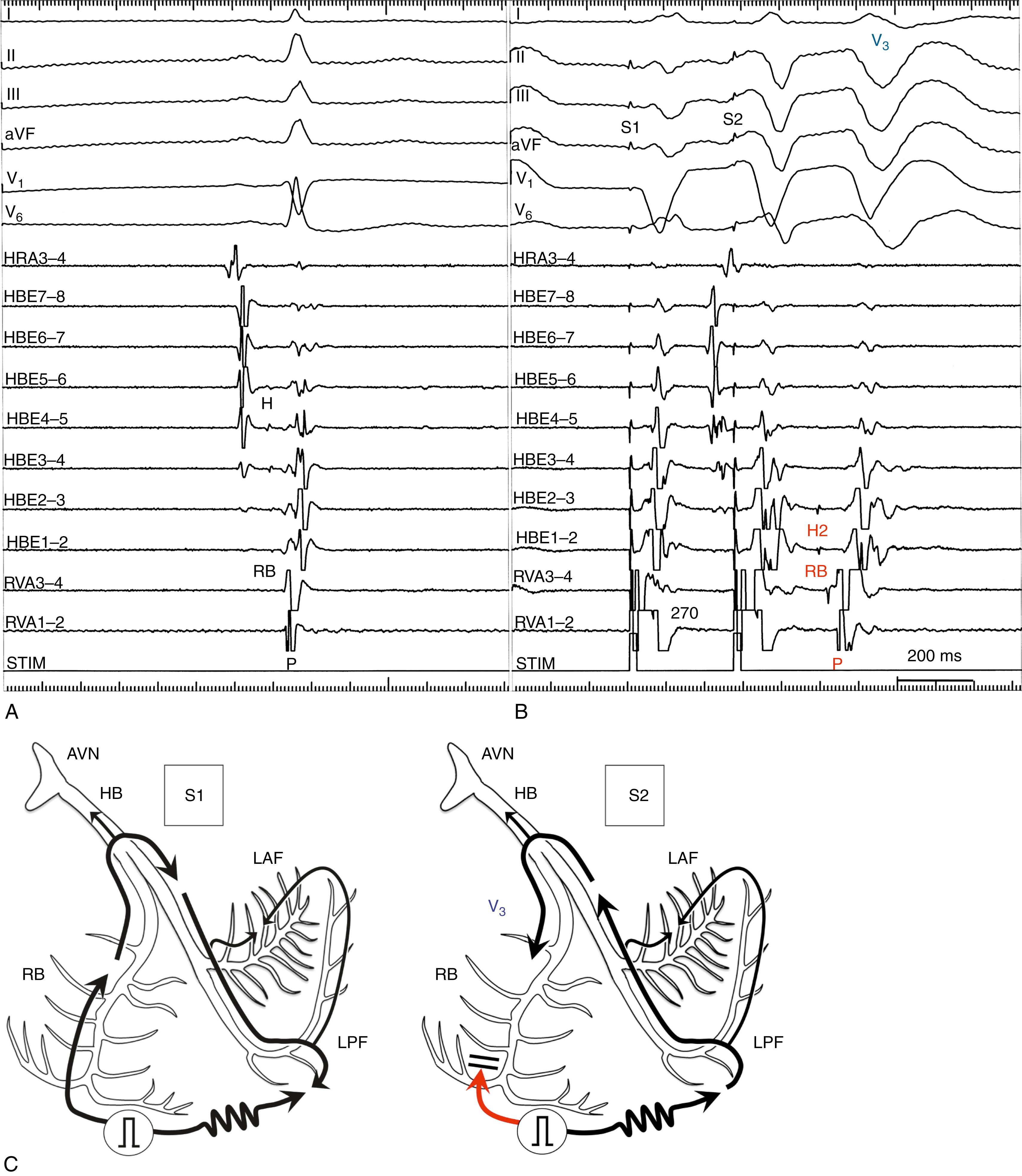
Alternatively, anterograde activation can proceed via the LBB and then through the septum. Retrograde activation can then proceed via the RBB, creating an RBBB morphology (“clockwise” reentry, type C). , Anterograde activation via the RBB and retrograde via the LPF or the LAF alone is another possibility. eFig. 84.2 demonstrates the spontaneous change from interfascicular reentrant VT (type B BBRVT) to type A BBRVT.
Although the His bundle potential can be recorded during BBRVT, the His bundle itself is not a necessary contributor to the BBRT circuit. During counterclockwise BBRVT (type A), conduction travels down the RBB, transits through the septal myocardium, and travels retrograde through the LBB. The turnaround point from the LBB to the RBB is inferior to, and does not include, the His bundle.
Conduction delay, critical for initiation and perpetuation of BBR, may be present in the connections between the bundles. Anisotropic conduction in the infra-Hisian conduction system, potentially critical for initiation and maintenance of BBR, may explain the greater degree of H-V delay often noted during tachycardia than in sinus rhythm. Alternatively, the observed H-V prolongation during tachycardia could be caused by progressive distal Purkinje system conduction delay in diseased bundles, which is more apparent at rapid rates (phase 3 block).
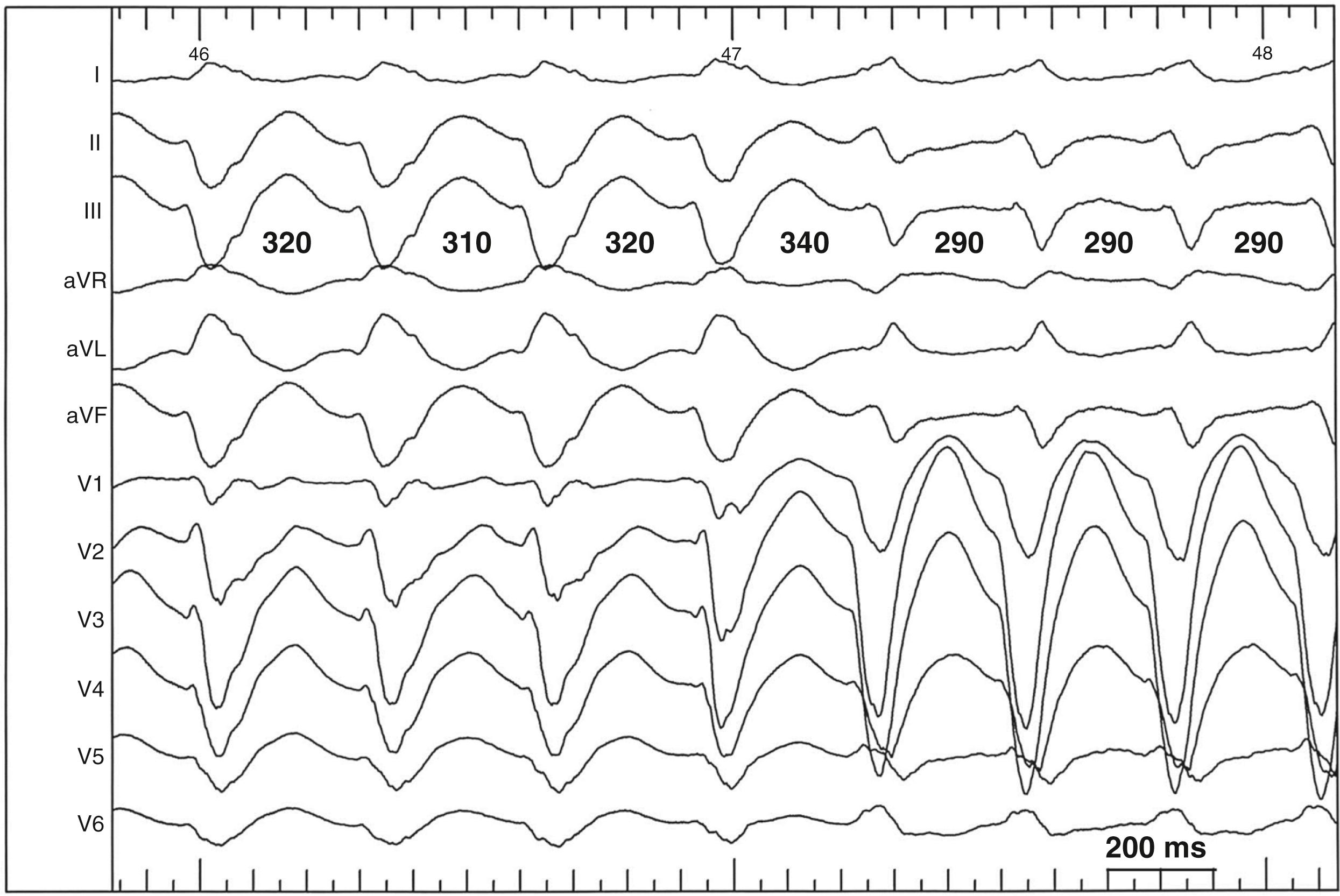
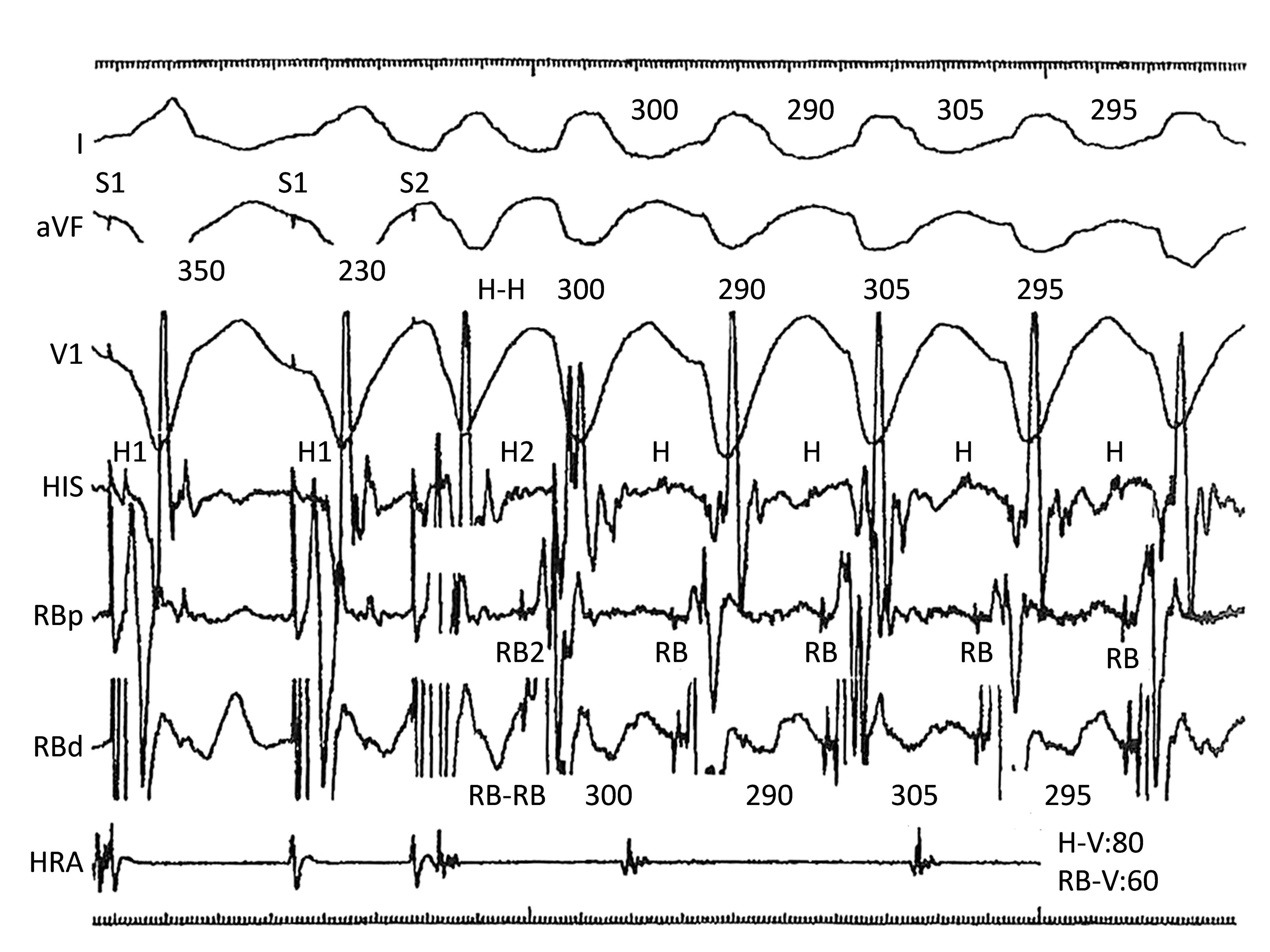
BBRVT can occur in patients who have apparently normal His-Purkinje conduction during sinus rhythm but who have functional conduction impairment at faster rates. Li and colleagues reported a series of 178 patients with VT, of whom 13 had BBRVT. Of those 13, 6 had an H-V interval 55 ms or less during sinus rhythm (i.e., normal). In those BBRVT patients with a normal H-V interval at baseline, the H-V interval was prolonged during BBRVT. Functional His-Purkinje delay was present with rapid atrial pacing or premature extrastimuli in patients of this group but not in those with prolonged H-V intervals in sinus rhythm who had BBRVT. Functional block initiating BBR may be perpetuated by persistent “linking.” A successive impulse entering a BBR circuit preferentially propagates along one limb because of functional block in the contralateral limb, resulting from the effects of the prior impulse. Fig. 84.3 shows the induction of type A BBRVT by RV extrastimulus with retrograde slow conduction via the left Purkinje system. H1 was retrograde over RBB during S1 pacing and H2 was recorded by retrograde decremental conduction over the LBB after S2 extrastimulus. Furthermore, the BBRVT was sustained by anterograde conduction over the RBB and retrograde conduction over the LBB.
Even in otherwise normal individuals, occasional spontaneous BBR beats are common. This is seen as a normal response to premature ventricular extrastimuli in patients undergoing programmed electrical stimulation who do not have BBRVT or even known His-Purkinje disease ( eFig. 84.3 ). This finding is known as the V 3 phenomenon. , A premature stimulus (S2) produces an impulse that blocks retrogradely in the RBB system but propagates through the septum to the left ventricle, where it conducts retrogradely via the LBB system, causing a prolongation of the S-H2 interval that is followed by V 3 from anterograde conduction down the RBB. Spontaneous repetitive ventricular premature beats caused by BBR have been reported. ,
BBR has been described as the mechanism responsible for up to 40% of sustained VT episodes in patients with idiopathic dilated cardiomyopathies. Moreover, BBR can occur in patients who have no intrinsic heart disease but who have associated His-Purkinje system conduction disease. , , , , However, BBRVT, in patients without structural heart disease, is rare. Recently Chen and colleagues reported nine young patients with structurally normal hearts and BBRVT in whom extensive conduction disturbances within His-Purkinje system was observed. With 3D mapping of the left ventricle, slow anterograde or retrograde conduction over the left His-Purkinje system, with normal myocardial voltage, was identified. Initiation of BBRVT during programmed RV extrastimulus testing demonstrated decremental retrograde conduction over the LBB. Anterograde slow conduction over the RBB was also identified between the distal RBB and the ventricle and at the junction of the RBB and the ventricle. In addition, other Purkinje-related VTs were induced in five of nine patients. Induction of multiple Purkinje network–related VTs suggested the presence of diffuse His-Purkinje disease.
Roberts and colleagues reported six cases of idiopathic BBRVT in patients with normal biventricular size and function. All patients were noted to have His-Purkinje system conduction abnormalities with prolonged H-V at baseline (mean, 69.2 ms); all had successful ablation targeting the RBB. Three of six patients had gene mutations identified, two in the SCN5A and one in the LMNA gene.
BBRVT has been reported in patients with myotonic dystrophy but no apparent structural heart disease (see Chapter 112 ). Myotonic dystrophy in adulthood (prevalence: 1:8000) predominantly shows neurologic involvement and cataracts. Myocardial conduction disturbances, also frequent, are secondary to extensive and selective damage to the cardiac conduction system, which is classically not associated with structural cardiomyopathy. Thus neurologic and ophthalmologic evaluations are recommended in patients with wide QRS tachycardia, conduction disturbance, and no structural heart disease.
BBRVT has several modes of spontaneous initiation. Ventricular premature beats are often the trigger. Occasionally, premature atrial beats or atrial fibrillation can initiate BBR. Bradycardia-dependent LBBB initiation of BBR, without obvious intramyocardial conduction delay, is possible spontaneously during sinus bradycardia. BBR has also been described in a patient with cycles of atrioventricular (AV) block and in association with bradycardia-dependent (phase 4) bundle branch block. BBRVT storm has been related to ventricular pacing when pacing initiates retrograde activation through the His-Purkinje system.
In the electrophysiology laboratory, ventricular extrastimuli delivered with short-long-short coupling intervals (pacing train of 400 ms with a delay of 600 ms or 800 ms before a short-coupled premature extrastimulus) tend to cause unidirectional block or sufficient conduction delay in a bundle branch to initiate BBRVT. Long-short coupling intervals are specific for initiation of BBRVT.
Atrial pacing and/or isoproterenol may be required. In one report, incremental atrial pacing during isoproterenol infusion initiated BBR with an RBBB pattern in four of six patients with inducible BBRVT. Class IA or IC antiarrhythmic drugs may sufficiently slow conduction in one of the bundles to allow BBRVT to occur (and thus may be proarrhythmic for this condition). Rarely are such drugs used to initiate BBRVT in the electrophysiology laboratory.
Initiation of interfascicular reentry occurs when an atrial or ventricular premature depolarization conducts over the healthy fascicle, giving rise to a QRS identical to that in sinus rhythm, and then reenters the blocked fascicle in the retrograde direction to induce and sustain reentrant interfascicular VT.
Several criteria help diagnose BBRVT ( Box 84.1 ). The 12-lead ECG morphology during tachycardia tends to be a typical LBBB or RBBB morphology. However, an atypical surface ECG differing from a typical LBBB pattern can manifest during BBRVT in patients with severe biventricular cardiomyopathy ( Fig. 84.4 ). Criteria of a typical LBBB QRS morphology are therefore not a requisite criterion in those with suspected BBRVT. Misleading BBRVT cases with an ECG morphology exhibiting negative concordance in the precordial leads have been reported. These may mimic myocardial VT originating from the anterior or apical RV.
VT morphology is a typical LBBB or RBBB
Induction is dependent on H-P conduction delay
His potential precedes each QRS complex
H-V during VT usually ≥ HV during sinus rhythm
Terminates with block in H-P system
His, RBB, and LBB activation sequences during an LBBB morphology tachycardia or His, LBB, and RBB activation sequences during an RBBB morphology tachycardia
Variations in the V-V interval are preceded by similar changes in the H-H interval
PPI-TCL <30 ms with entrainment from RV apex
QRS morphology during atrial entrainment is similar to that during VT
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here