Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]() Additional content is available online at Elsevier eBooks for Practicing Clinicians
Additional content is available online at Elsevier eBooks for Practicing Clinicians
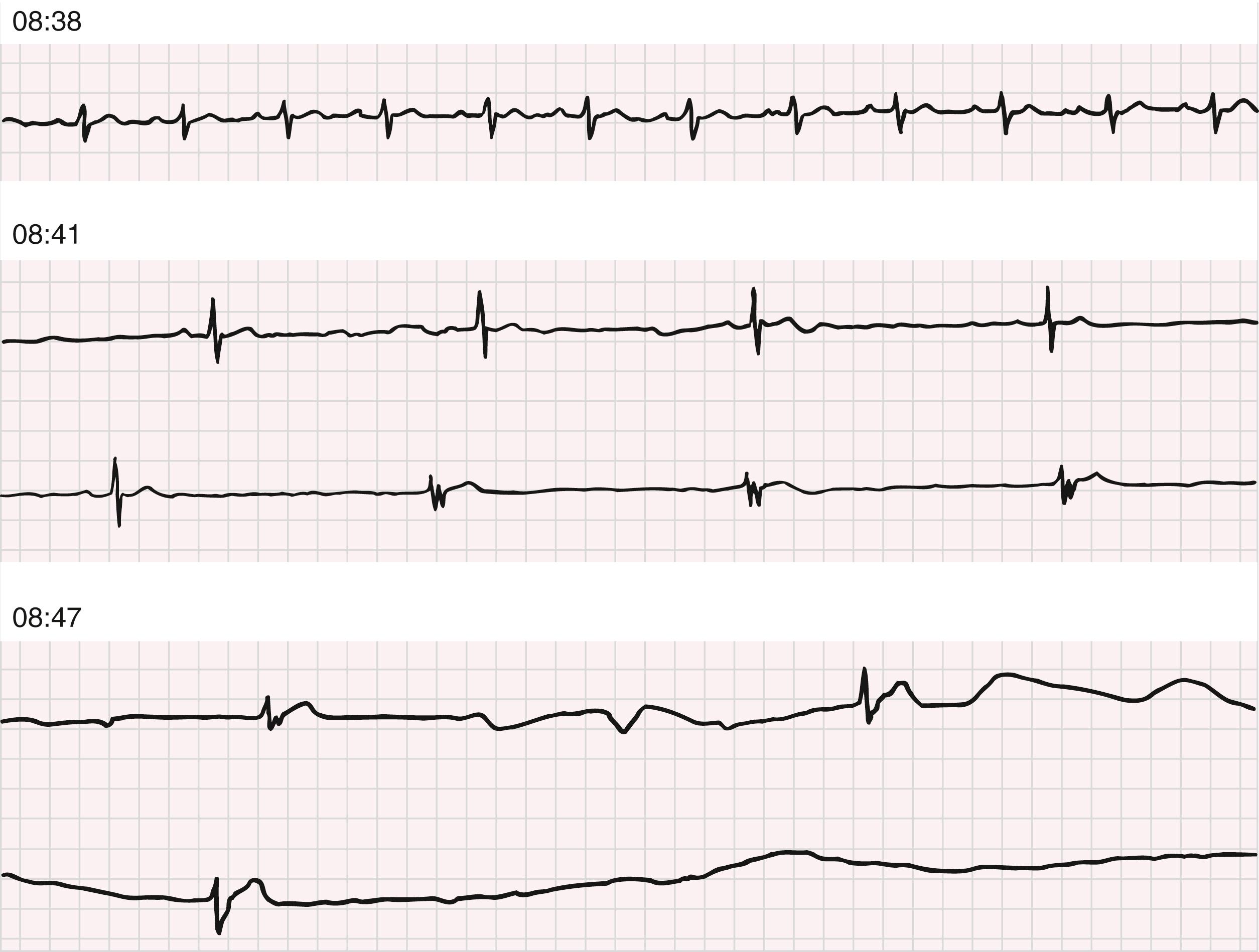
Based on large population studies of healthy individuals, the lower limit of normal resting heart rate is defined as 50 beats/min. , Frequently, bradyarrhythmias are physiologic, as in well-conditioned athletes with low resting heart rates or in type I atrioventricular (AV) block during sleep. In other cases, bradyarrhythmias can be pathologic. Similar to tachyarrhythmias, bradyarrhythmias can be categorized on the basis of the level of disturbance in the hierarchy of the normal impulse generation and conduction system (from sinus node to AV node to His-Purkinje system) (see Chapter 65 and Table 65.1).
Sinus bradycardia is diagnosed in an adult when the sinus node discharges at a rate less than 50 beats/min ( Fig. 68.1A ). P waves have a normal contour, and are usually upright in leads I, II, and aVF, and occur before each QRS complex, usually with a constant PR interval longer than 120 msec. Sinus arrhythmia often coexists.

Sinus bradycardia can result from excessive vagal or decreased sympathetic tone, as an effect of medications, or from anatomic changes in the sinus node. In most cases, symptomatic sinus bradycardia is caused or worsened by the effects of medication. Asymptomatic sinus bradycardia frequently occurs in healthy young adults, particularly well-trained athletes, and decreases in prevalence with advancing age. During sleep, the normal heart rate can fall to 35 to 40 beats/min, especially in adolescents and young adults, with marked sinus arrhythmia sometimes producing pauses of 2 seconds or longer. Eye surgery, coronary arteriography, meningitis, intracranial tumors, increased intracranial pressure, cervical and mediastinal tumors, and certain disease states (e.g., severe hypoxia, myxedema, hypothermia, fibrodegenerative changes, convalescence from some infections, gram-negative sepsis, mental depression) can produce sinus bradycardia. Sinus bradycardia also occurs during vomiting or vasovagal syncope , (see Chapter 71 ) and can be produced by carotid sinus stimulation or by the administration of parasympathomimetic drugs, lithium, amiodarone, beta adrenoceptor–blocking drugs, clonidine, propafenone, ivabradine (a specific I f pacemaker current blocker; see Chapter 62 ), or calcium antagonists. Conjunctival instillation of beta blockers for glaucoma can produce sinus or AV nodal abnormalities, especially in elderly patients.
In most cases, sinus bradycardia is a benign arrhythmia that can actually be beneficial by producing a longer period of diastole and increasing ventricular filling time, especially in heart failure patients. Conversely, it can be associated with syncope caused by an abnormal autonomic reflex (cardioinhibitory; see Chapter 71 ). Sinus bradycardia occurs in 10% to 15% of patients with acute myocardial infarction (MI) and may be even more prevalent when patients are seen in the early hours of infarction. Unless it is accompanied by hemodynamic decompensation or arrhythmias, sinus bradycardia is generally associated with a more favorable outcome after MI than sinus tachycardia. It is usually transient and occurs more commonly during inferior than during anterior MI; sinus bradycardia has also been noted during reperfusion with thrombolytic agents (see Chapter 38 ). Bradycardia that follows resuscitation from cardiac arrest is associated with a poor prognosis.
Treatment of sinus bradycardia is not usually necessary unless cardiac output is inadequate or arrhythmias result from the slow rate. Atropine (0.5 mg intravenously as an initial dose, repeated if necessary) is generally acutely effective; lower doses, particularly given subcutaneously or intramuscularly, can exert an initial parasympathomimetic effect, possibly by a central action. For recurrent symptomatic episodes, temporary or permanent pacing may be needed (see Chapter 64, Chapter 69 ). Although theophylline and terbutaline can be used to increase the sinus rate, as a general rule, no drugs are available that increase the heart rate reliably and safely during long periods without undesirable side effects.
Sinus arrhythmia is characterized by a phasic variation in sinus cycle length during which the maximum sinus cycle length minus the minimum sinus cycle length exceeds 120 msec or the maximum sinus cycle length minus the minimum sinus cycle length divided by the minimum sinus cycle length exceeds 10% ( Fig. 68.1B ). It is the most frequent form of arrhythmia and is physiologically normal. P wave morphology does not usually vary, and the PR interval exceeds 120 msec and remains unchanged because the focus of discharge remains relatively fixed within the sinus node. On occasion, the pacemaker focus can wander within the sinus node, or its exit to the atrium may change and produce P waves of a slightly different contour (although not retrograde) and a slightly changing PR interval that exceeds 120 msec.
Sinus arrhythmia usually occurs in the young, especially those with slower heart rates or with enhanced vagal tone, for example, following the administration of digitalis or morphine, or due to athletic training. The prevalence of sinus arrhythmia decreases with age or with autonomic dysfunction, such as in diabetic neuropathy. Sinus arrhythmia appears in two basic forms. In the respiratory form, the P-P interval cyclically shortens during inspiration, primarily as a result of reflex inhibition of vagal tone, and slows during expiration; breath-holding eliminates the variation in cycle length (see Chapter 61 ). Nonrespiratory sinus arrhythmia is characterized by a phasic variation in the P-P interval unrelated to the respiratory cycle and can be the result of digitalis intoxication. Loss of sinus rhythm variability is a risk factor for sudden cardiac death (see Chapter 70 ).
Symptoms produced by sinus arrhythmia are uncommon, but on occasion, if the pauses are excessively long, palpitations or dizziness can result. Marked sinus arrhythmia can produce a sinus pause sufficiently long to cause syncope if it is not accompanied by an escape rhythm. Treatment is usually unnecessary. Increasing the heart rate by exercise or drugs generally abolishes sinus arrhythmia. Symptomatic individuals may experience relief from palpitations with sedatives, tranquilizers, atropine, ephedrine, or isoproterenol administration, as for the treatment of sinus bradycardia.
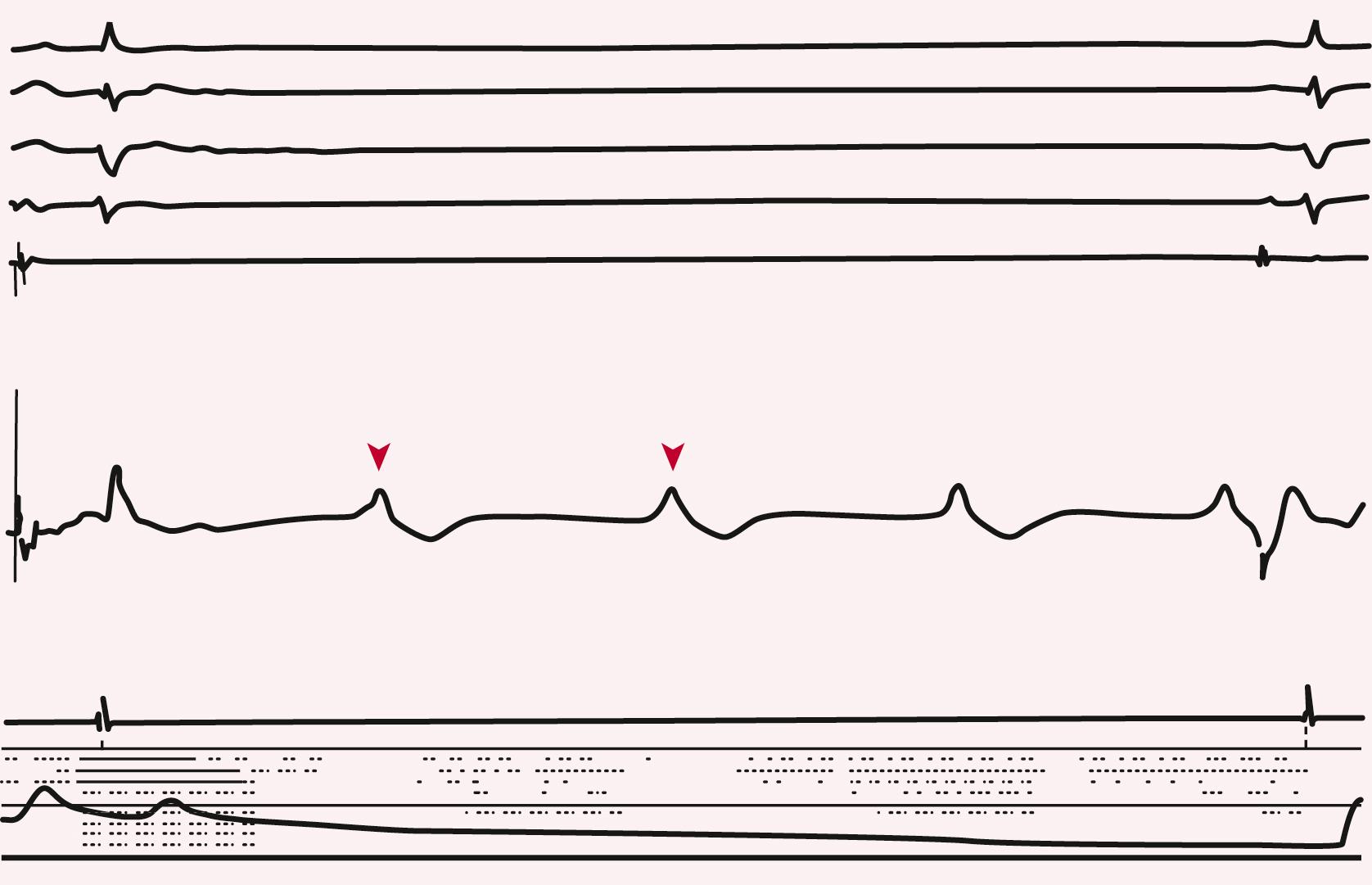
The most common example of ventriculophasic sinus arrhythmia occurs during complete AV block and a slow ventricular rate, when P-P cycles that contain a QRS complex are shorter than P-P cycles without a QRS complex. Similar lengthening can be present in the P-P cycle that follows a premature ventricular complex (PVC) with a compensatory pause. Alterations in the P-P interval are probably caused by the influence of the autonomic nervous system responding to changes in ventricular stroke volume.
Sinus pause or sinus arrest is recognized by a pause in the sinus rhythm ( eFig. 68.1 ). The P-P interval delimiting the pause does not equal a multiple of the basic P-P interval. Differentiation of sinus arrest, which is thought to be caused by slowing or cessation of spontaneous sinus node automaticity, and therefore is a disorder of impulse formation, from sinoatrial (SA) exit block in patients with sinus arrhythmia can be difficult without direct recordings of sinus node discharge. Failure of sinus nodal discharge results in the absence of atrial depolarization and can also result in ventricular asystole if escape beats initiated by latent pacemakers do not occur (see eFig. 68.1 ). Involvement of the sinus node by acute MI, degenerative fibrotic changes, digitalis toxicity, stroke, or excessive vagal tone can produce sinus arrest. Transient sinus arrest (especially while sleeping) may have no clinical significance by itself if latent pacemakers promptly escape to prevent ventricular asystole or the genesis of other arrhythmias precipitated by slow rates. Sinus arrest and AV block have been demonstrated in many patients with sleep apnea (see Chapter 89 ).
Treatment is as outlined earlier for sinus bradycardia. In patients who have a chronic form of sinus node disease characterized by marked sinus bradycardia or sinus arrest, permanent pacing is often necessary. However, as a general rule, chronic pacing for sinus bradycardia is indicated only in symptomatic patients.
SA exit block is an arrhythmia that is recognized electrocardiographically by a pause resulting from absence of the normally expected P wave ( eFig. 68.2 ). The duration of the pause is a multiple of the basic P-P interval. SA exit block is caused by a conduction disturbance during which an impulse formed within the sinus node fails to depolarize the atria or does so with delay ( eFig. 68.3 ). An interval without P waves that equals approximately two, three, or four times the normal P-P cycle characterizes type II second-degree SA exit block. During type I (Wenckebach) second-degree SA exit block, the P-P interval progressively shortens before the pause, and the duration of the pause is less than two P-P cycles. (See Chapter 14 for further discussion of Wenckebach intervals.) First-degree SA exit block cannot be recognized on the electrocardiogram (ECG) because SA nodal discharge is not recorded. Third-degree SA exit block can be manifested as a complete absence of P waves and is difficult to diagnose with certainty without sinus node electrograms.

Excessive vagal stimulation, acute myocarditis, MI, or fibrosis involving the atrium, as well as drugs such as quinidine, procainamide, flecainide, and digitalis, can produce SA exit block. SA exit block is usually transient. It may be of no clinical importance except to prompt a search for the underlying cause. On occasion, syncope can result if the SA block is prolonged and unaccompanied by an escape rhythm. SA exit block can occur in well-trained athletes. Therapy for patients who have symptomatic SA exit block is as outlined earlier for sinus bradycardia.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here