Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A bone scan (i.e., bone scintigraphy) requires the intravenous injection of a small amount of a radioactive tracer (e.g., technetium-99m [ 99m Tc] methylene diphosphonate [MDP]) that is adsorbed into the hydroxyapatite structure of bone. Areas of increased radiotracer uptake relate to bone that is actively being remodeled such as with infection or tumor. The radiotracer carries a relatively low dose of radioactivity and is extremely unlikely to result in any allergic or adverse reactions. The patient can eat and take medications regularly and is able to continue all daily activities before and after the scan. The scan itself occurs approximately 2 hours after injection of the radiotracer, and the scan time is approximately 30-45 minutes for a whole body scan. Single photon emission computed tomography (SPECT) of specific structures may also be performed to better delineate those structures, especially if the SPECT images are coregistered with computed tomography (CT) images. Three-phase bone scans require initial scanning for approximately 20 minutes at the time of the injection as well as delayed images obtained approximately 2 hours after injection.
An 18 F-NaF PET scan requires the intravenous injection of a small amount of a radioactive sodium fluoride, which is absorbed into bone. Areas of increased radiotracer uptake relate to bone that is actively being remodeled such as with infection or tumor. As with a conventional bone scan, the patient can eat and take medications regularly and is able to continue all daily activities before and after the scan. The scan itself occurs approximately 30-60 minutes after injection of the radiotracer, and the scan time is approximately 30 minutes for a whole body tomographic scan. The major advantage of 18 F-NaF PET is improved spatial resolution and contrast compared to a conventional bone scan. Coregistered CT is also routinely obtained.
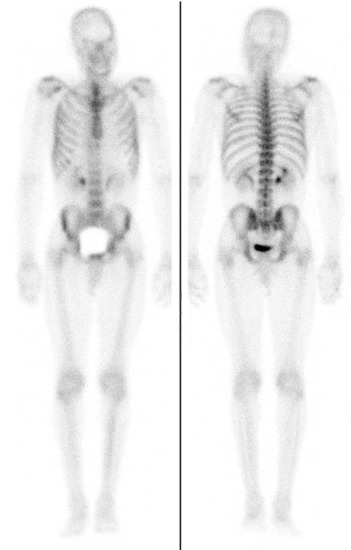
Normally, all of the bones should be visible on a bone scan, including individual vertebrae and ribs ( Figure 78-1 ). The kidneys and bladder are also seen in most patients due to radiotracer excretion. Normal soft tissue uptake can occur in the breasts and sometimes in vascular structures such as the uterus. Calcified cartilage is also commonly seen in the costochondral and thyroid cartilages.
Common nonmalignant findings in asymptomatic patients include degenerative disease of the spine or peripheral joints, dental or sinus disease, calcification associated with atherosclerotic disease, and prior fractures.
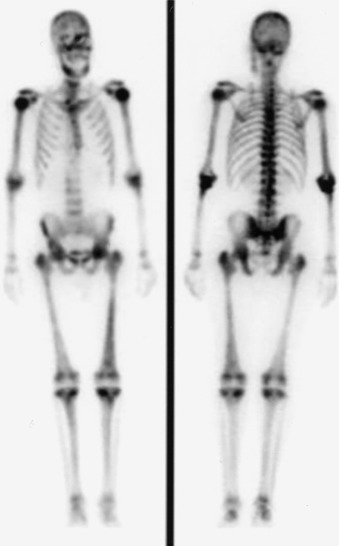
On 18 F-NaF PET imaging, a similar pattern of radiotracer uptake and excretion is observed, with uniform uptake seen throughout the skeleton. The tomographic images provided by PET provide high contrast resolution assessment of the skeletal structures.
A “superscan” implies that so much of the radiotracer is taken up by the bones that there is no significant excretion in the kidneys and bladder or uptake in the soft tissues. The scan appears almost “too good” with high contrast between the bones and other tissues. The most common causes of a “superscan” are widespread metastatic disease, metabolic bone disease such as by primary or secondary hyperparathyroidism, and widespread Paget's disease. In a patient with cancer, a “superscan” implies widespread osseous metastases that cannot be individually distinguished, but rather occupy almost the entire skeleton.
Patients with bone pain from osteoblastic metastases can be treated primarily with four modalities: cancer-specific chemotherapy, radiation therapy, narcotic pain management, or radiopharmaceutical agents that target bone. The last option is often the best when multiple sites are involved that cannot be easily targeted by radiation therapy or would result in excessive radiation to uninvolved tissues or the whole body. Radiopharmaceutical agents, such as strontium-89 ( 89 Sr) chloride (Metastron) or samarium-153 ( 153 Sm) ethylenediaminetetramethylene phosphonic acid (EDTMP) (Quadramet), which are beta-emitters, can be injected intravenously in patients with osteoblastic metastases for relief of pain. Studies suggest that 80% of patients experience some pain relief, and almost 50% have complete relief. Pain relief lasts a mean of 6-8 months, and patients can be retreated with similar pain relief. Although these treatments are not considered curative, they can substantially improve a patient's quality of life and decrease reliance on narcotic medications.
Patients with such symptoms after a traumatic event typically have either osseous or soft tissue uptake characteristic of focal injury. In these patients, a three-phase bone scan helps make that determination. The first two phases—the blood flow, or vascular, phase and the blood pool, or tissue, phase—help to show whether there is soft tissue edema. If there is also focal uptake on the delayed bone scan images, an osseous injury is suspected, which may be superimposed on soft tissue injury. The scan in Figure 78-3 shows diffusely increased uptake on all three phases, however, which is suggestive of reflex sympathetic dystrophy (RSD). RSD is a response to a traumatic event and results from autonomic dysfunction in the extremity, causing altered regulation of blood flow. On a bone scan, the typical finding is increased flow and radiotracer uptake on all three phases, with a predominantly periarticular distribution seen on delayed bone scan images. Other patterns have also been described. Regardless, the findings are almost always diffuse because they affect the entire extremity, including all of the fingers and distal upper extremity.

Usually, a suboptimal bone scan is related to technical factors, such as not waiting at least 2 hours between radiotracer injection and scan acquisition, poor preparation of the MDP, a significantly infiltrated radiotracer dose during injection, patient motion, or the camera being set to the incorrect energy window (e.g., for 123 I rather than for 99m Tc). Physiologic reasons for suboptimal scans include large patient size, resulting in significant photon attenuation, or poor circulation states, such as congestive heart failure in which the radiotracer is not adequately delivered to the bones. Finally, patients with osteoporosis simply do not have enough bone for good visualization of osseous structures, and patients with iron overload may also have inhibited uptake of the radiotracer.
Bone scans generally are not sensitive for lytic bone lesions, and patients who show findings of multiple myeloma or other lytic osseous abnormalities on CT or radiography should not be referred for a bone scan. Instead, evaluation with either a bone survey using multiple radiographs, a magnetic resonance imaging (MRI) scan, or an 18 F-fluorodeoxyglucose (FDG) PET/CT scan is performed. Patients with certain cancers that lead to mixed lytic and blastic osseous metastases may still benefit from a bone scan. Also, patients with multiple myeloma with lytic disease in weight-bearing bones that are susceptible to pathologic fracture may still benefit from a bone scan, as a fracture would show up as a focus of increased radiotracer uptake. If a nuclear medicine scan is needed to better detect or characterize the osseous lesions, FDG PET/CT is the most appropriate choice as this directly reveals sites of cancer in the bone marrow whether or not there is associated bone lysis or sclerosis rather than the indirect effects of cancer upon the surrounding bones.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here