Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The neonatal and pediatric stages are periods of rapid physiologic changes, some of which affect the hemostatic system. The hemostatic system is a dynamic system that evolves gradually from birth into the mature adult form. Evaluation of bleeding and clotting disorders in children requires an understanding of the evolution of physiologic normal values for age, the congenital disorders that present in early life, and the common clinical settings that affect hemostasis and thrombosis risks in childhood. The rapid evolution of the blood coagulation system after birth leads to a dynamic group of age-dependent reference ranges for the levels of the various components that should be considered physiologically normal. Developmental hemostasis is the term applied to the evolution of the hemostatic and fibrinolytic systems through infancy and childhood into adult age.
The coagulation system in children provides innate protection from thrombosis without an increased risk for bleeding. The hemostatic system evolves throughout childhood and most rapidly during the neonatal period. Changes in the plasma concentrations of proteins involved in blood coagulation result in a dynamic group of reference ranges for preterm and term infants. Although different from adult values, these reference ranges are neither abnormal nor pathologic. The relative rarity of hemorrhagic or thrombotic complications in this population suggests that the neonatal coagulation system is physiologically replete.
The pioneering work of the late Dr. Maureen Andrew paved the way for research into developmental hemostasis. The concept of developmental hemostasis is now widely accepted, and her seminal papers describing the reference ranges for healthy premature and full-term neonates and children are still widely quoted. Laboratory evaluation of thrombosis or bleeding in neonates and children must take into account the age-related reference ranges, which differ significantly from adult levels. In addition, because coagulation assay results vary depending on the type of analyzer and reagents used, caution is needed when prior publications of defined reference ranges for neonates are used.
Although research has looked into age-specific differences in the quantitative levels of hemostatic proteins, functional assays that are reagent and analyzer-specific are still predominantly used for hemostatic diagnosis in the pediatric population. Changes in functional protein levels correspond with changes in global tests of coagulation. The prothrombin time (PT), expressed in seconds, in full-term and premature neonates is like that in children and adults, despite the fact that neonates have relative deficiencies of the vitamin K-dependent coagulation factors. The activated partial thromboplastin time (aPTT) is prolonged in newborns, which is attributed to relative deficiencies in the contact factors (see Chapter 126 ). Thromboelastography reaction time is significantly lower in neonates compared with children and adults. The thrombin time in neonates is like that in children and adults when measured in the presence of calcium, which compensates for the unique fetal form of fibrinogen that has increased sialic acid content.
The synthesis of fetal and neonatal coagulation proteins begins at approximately 10 weeks of gestation, and plasma concentrations of these proteins increase with gestational age. Maternal coagulation proteins cannot cross the placenta; however, maternal drugs, such as warfarin and phenytoin, can affect the synthesis of fetal vitamin K-dependent coagulation proteins.
In the healthy newborn, plasma levels of procoagulant factors, such as factor (F)VII, FIX, FX, and prothrombin (the vitamin K-dependent coagulation factors) and FXI, FXII, prekallikrein, and high-molecular-weight kininogen (HMWK) (the contact factors), are about 50% lower than adult values ( Table 148.1 ). The levels rise as the infant ages, and they reach about 80% of normal adult values by 6 months of age but remain decreased throughout childhood. The levels of fibrinogen, FV, FVIII, and FXIII in neonates are similar to those in adults and remain so throughout childhood. The level of von Willebrand factor (vWF) in newborns is about two-fold higher than that in adults and the level of vWF gradually decreases over the first 6 months of life. In contrast, the levels of antithrombin (AT) are lower than adult levels in the first 3 months of life and are comparable to the levels seen in patients with heterozygous AT deficiency (see Chapter 138 ). The physiologic ranges for coagulation factors in healthy newborns who have received intramuscular vitamin K after delivery are shown in Table 148.2 .
| Component | Neonatal Versus Adult Level | |
|---|---|---|
| Primary hemostasis | ↔ | Platelet count |
| ↑ | vWF | |
| Coagulation factors | ↓ | FII, FVII, FIX, FX |
| ↓ | FXI, FXII | |
| ↓ to ↔ | FV, FXIII | |
| ↔ | Fibrinogen | |
| ↔ | FVIII | |
| Anticoagulant factors | ↓ | TFPI, AT, PC, PS |
| ↑ | α 2 M | |
| Fibrinolysis | ↓ | Plasminogen |
| ↔ to ↑ | PAI | |
| Day 1 | Day 3 (ref 3) vs. Day 5 (ref 2) | 1 month–1 year | Adult (measured) | |||||
|---|---|---|---|---|---|---|---|---|
| Ref 3 | Ref 2 | Ref 3 | Ref 2 | Ref 3 | Ref 2 | Rel 3 | Ref 2 | |
| Prothrombin time (s) | 15.6 | 13 | 14.9 | 12.4 | 13.1 | 12.3 | 13 | 12 |
| (14.4–16.4) | (11.6–14.4) | (13.5–16.4) | (10.5–13.9) | (11.5–15.3) | (10.7–13.9) | (11.5–14.5) | (11–14) | |
| PTT (s) | 38.7 | 42.9 | 36.3 | 42.6 | 39.3 | 35.5 | 33.2 | 33 |
| (34.3–44.8) | (31.3–54.5) | (29.5–42.2) | (25.4–59.8) | (35.1–46.3) | (28.1–42.9) | (28.6–38.2) | (27–40) | |
| Thrombin time (s) | N/A | 23.5 | N/A | 23.1 | 17.1 | 24.3 | 16.6 | N/A |
| (19–28.3) | (18–29.2) | (16.3–17.6) | (19.4–29.2) | (16.2–17.2) | ||||
| Fibrinogen (mg/dL) | 280 | 283 | 330 | 312 | 242 | 251 | 310 | 278 |
| (192–374) | (225–341) | (283–401) | (237–387) | (82–383) | (150–387) | (190–430) | (156–400) | |
| Prothrombin (%) | 54 | 48 | 62 | 63 | 90 | 88 | 110 | 108 |
| (41–69) | (37–59) | (50–73) | (48–78) | (62–103) | (60–116) | (78–138) | (70–146) | |
| Factor V (%) | 81 | 72 | 122 | 95 | 113 | 91 | 118 | 106 |
| (64–103) | (54–90) | (92–154) | (70–120) | (94–14) | (55–127) | (78–152) | (62–150) | |
| Factor VII (%) | 70 | 66 | 86 | 89 | 128 | 87 | 129 | 105 |
| (52–88) | (47 – 85) | (67–107) | (62–116) | (83–160) | (47–127) | (61–199) | (67–143) | |
| Factor VIII (%) | 182 | 1(X) | 159 | 88 | 94 | 73 | 160 | 99 |
| (105–329) | (61–139) | (83–274) | (55–121) | (54–145) | (53–109) | (52–290) | (50–149) | |
| Factor IX (%) | 48 | 53 | 72 | 53 | 71 | 86 | 130 | 109 |
| (35–56) | (34–72) | (44–97) | (34–72) | (43–121) | (36–139) | (59–254) | (55–163) | |
| Factor X (%) | 55 | 40 | 60 | 49 | 95 | 78 | 124 | 106 |
| (46–67) | (26–54) | (46–75) | (34–64) | (77–122) | (38–118) | (96–171) | (70–152) | |
| Factor XI (%) | 30 | 38 | 57 | 55 | 89 | 86 | 112 | 97 |
| (7–41) | (24–52) | (24–79) | (39–71) | (62–125) | (49–134) | (67–196) | (67–127) | |
| Factor XII (%) | 58 | 53 | 53 | 47 | 79 | 77 | 115 | 108 |
| (43–80) | (33–73) | (14–80) | (29–65) | (20–135) | (39–115) | (35–207) | (52–164) | |
| Antithrombin III (%) | 76 | 63 | 74 | 67 | 109 | 104 | 96 | 100 |
| (58–90) | (51–75) | (60–89) | (54–80) | (72–134) | (84–124) | (66–124) | (74–126) | |
| Protein C activity (%) | 36 | 35 | 44 | 42 | 71 | 59 | 104 | 96 |
| (24–44) | (26–44) | (28–54) | (31–53) | (31–112) | (37–81) | (74–164) | (64–128) | |
| Protein S activity (%) | 36 | 36 | 49 | 50 | 102 | 87 | 75 | 81 |
| (28–47) | (24–48) | (33–67) | (36–64) | (29–162) | (55–119) | (54–103) | (60–113) | |
| D-dirner (pg/mL) | 1.47 | N/A | 1.34 | N/A | 0.22 | N/A | 0.18 | N/A |
| (0.41–2.47) | (0.58–2.74) | (0.11–0.42) | (0.05–0.42) | |||||
Thrombin regulation in neonatal plasma is like that in plasma from adults who are receiving therapeutic doses of anticoagulants. The concentration of prothrombin is lower in neonates than that in adults. However, the extent of thrombin generation depends on the experimental system; thrombin generation in plasma from neonates has been reported to be comparable to that in adult plasma provided that thrombomodulin is added.
Thrombin is inhibited by AT, α 2 -macroglobulin, and heparin cofactor II. In neonates, the α 2 -macroglobulin concentration is two-fold higher than that in adults. The overall capacity of newborn plasma to inhibit thrombin is like that of adult plasma due in part to the increased binding of thrombin by α 2 -macroglobulin. Thrombin inhibition by heparin cofactor II is catalyzed by a dermatan sulfate-like proteoglycan, which is produced by the placenta and is found in both maternal and fetal plasma.
Regulation of thrombin generation is accomplished by upstream inhibition of the clotting proteins in the prothrombinase and tenase complexes (see Chapter 121, Chapter 125 ). Plasma concentrations of protein C are low at birth and gradually increase to adult levels by 6 months of age. Although the total concentration of protein S is low at birth, the functional activity of protein S is comparable to that in adults because low levels of C4b-binding protein result in more free protein S. The interaction of protein S with activated protein C in neonatal plasma may be limited by the elevated levels of α 2 -macroglobulin. Free tissue factor pathway inhibitor levels in neonates are lower than in adults, although total levels of tissue factor pathway inhibitor in neonatal plasma are like those in adult plasma.
Although the levels of some components of the fibrinolytic system in neonates and children are different from those in adults, the clinical relevance of this finding is probably minimal. The fibrinolytic system regulates fibrin deposition by generating plasmin, which solubilizes fibrin. At birth, the fibrinolytic system has all the key components, but there are important age-related differences in the quantity and quality of the fibrinolytic proteins and enzymes. Plasma concentrations of plasminogen, tissue plasminogen activator (tPA), and α 2 -antiplasmin (α 2 AP) are decreased, whereas plasma concentrations of plasminogen activator inhibitor 1 (PAI-1) are increased. Furthermore, plasmin generation and overall fibrinolytic activity are decreased. The capacity to generate plasmin in newborn plasma is generally reduced compared with adult plasma, which likely reflects the decreased plasminogen concentration. Despite lower levels of fibrinolytic components, the newborn fibrinolytic system is still effective.
The euglobulin clot lysis time is a global assay of fibrinolytic activity but reflects only part of the physiologic fibrinolytic potential. Maneuvers that induce the release of endogenous fibrinolytic components, such as venous occlusion, desmopressin infusion, or exercise, provide more sensitive measures of in vivo fibrinolytic activity.
Plasminogen levels are lower in neonates and children than in adults, and fetal plasminogen binds to cellular receptors with lower affinity because of its increased sialic acid and mannose content. Whereas healthy neonates have lower plasmin-generating potential than adults, baseline levels of tPA can increase up to eightfold with illness. Neonates with severe plasminogen deficiency have only a minimally increased risk for thrombosis, and most of their clinical findings are the result of impaired extravascular fibrinolysis. The major plasmin inhibitors circulate at near adult levels in the neonate. In children, plasminogen activator inhibitor (PAI-1) is elevated, which results in fibrinolytic suppression during childhood.
Imbalances in the fibrinolytic system, whether hereditary or acquired, can lead to thrombotic or bleeding complications. Hereditary disorders, although rare, include plasminogen deficiency, PAI-1 deficiency, and α 2 AP deficiency. The efficacy and safety of fibrinolytic therapy may be influenced by age-dependent differences in the fibrinolytic system. Data are lacking on the optimal doses of fibrinolytic agents for the pediatric population, especially for neonates. tPA is the agent of choice, with the most common dose and duration of treatment being 0.5 mg/kg/h infused over 6 hours.
Platelet production starts around the end of the first trimester of gestation and reaches adult levels in the middle of the third trimester. Therefore, platelet counts in term and premature newborns and children are not different from those in adults. Similarly, mean platelet volume and platelet ultrastructure in neonates and children closely resemble those in adults. Yet, all the main platelet functions are deficient at birth. Neonatal platelets exhibit reduced phospholipid metabolism, calcium mobilization, granule secretion, and aggregation in response to agonists compared with platelets from children or adults. Although thrombocytopenia is common in neonates, thrombocytosis is rare and is associated with prematurity.
There are two proposed theories behind the reduced platelet function at birth. One hypothesis suggests that platelet activation and degranulation at the time of labor and delivery leads to exhausted circulating platelets; the other suggests that intrinsic platelet peculiarities account for the reduced reactivity of neonatal platelets. Studies of platelets from neonates reveal reduced aggregation in response to agonists, such as ADP, epinephrine, collagen, thrombin, and thromboxane analogues. This is especially true when platelets from preterm infants are studied. Flow cytometry studies using labeled monoclonal antibodies against platelet activation markers also reveal that platelets from cord blood or from neonates on the first postnatal day are hyporeactive compared with adult platelets. This decreased responsiveness is transient, and the platelets usually regain normal reactivity 10 to 14 days after delivery.
Despite the reduced platelet reactivity at birth, platelet adhesion may be enhanced because of higher levels of functionally more potent high-molecular-weight vWF multimers in the plasma. Consistent with this concept, the bleeding time and the platelet function analyzer (PFA-100) closure time are shorter in neonates than in children and adults. In healthy neonates, enhanced platelet adhesion immediately after delivery may compensate for the reduced platelet activation in response to agonists. Nonetheless, sick neonates may be at increased risk for bleeding.
The PFA-100 closure time is preferred over the bleeding time as a means of assessing platelet-related hemostasis. Bleeding time is an in vivo screening test that reflects the interaction between platelets and the blood vessel wall, but the results are as variable in neonates as they are in children and adults (see Chapter 127 ). Although the PFA-100 will not detect mild defects in platelet function, such defects rarely cause serious bleeding in neonates.
Studies in vitro and in neonatal animals suggest that the endothelium in neonates has greater antithrombotic potential than that in adult vessels. In both rabbit venous and aortic models, neonatal endothelium expresses more heparan sulfate proteoglycans than adult endothelium, which results in greater AT-mediated anticoagulant activity in rabbit pups compared with adult rabbits. Circulating levels of endothelial cell adhesion markers vary with age, implying dynamic expression and/or secretion of these proteins as a function of age (see Chapter 122 ).
Significant bleeding in children should prompt clinical evaluation. In sick children, acquired factor deficiencies or thrombocytopenia are frequently to blame, but rare congenital factor deficiencies can also manifest with bleeding. Initial empirical therapy consists of platelet and/or factor supplementation, which is often administered while diagnostic studies are under way.
Age, gender, presentation, birth and neonatal history, surgical history, family history, and medication use are each important in the evaluation of a child with hemorrhagic complications. Bleeding symptoms, such as epistaxis, occur in healthy children and do not always necessitate evaluation for an underlying bleeding disorder. It is important to consider frequency, duration, and severity of these symptoms to identify which children require testing. Table 148.3 highlights bleeding phenotypes in children that are concerning for an underlying bleeding disorder. Along with personal history, family history, such as bleeding tendencies, parental ethnicity, and history of consanguinity, may help to identify congenital bleeding disorders. A negative family history does not exclude an inherited bleeding disorder, especially X-linked and autosomal recessive disorders. In hemophilia, for example, up to one-third of patients have a negative family history. Pregnancy and delivery history, such as maternal infection, drug use, or immune thrombocytopenia (ITP), can provide important clues in cases of neonatal bleeding.
|
On physical examination, the location and characteristics of the bleeding (e.g., procedural, mucosal, cutaneous, intracranial, visceral), whether diffuse or localized, and the general appearance of the child as sick or well, may help to identify the underlying etiology of the hemorrhage. In ill-appearing children, disseminated intravascular coagulation (DIC) or liver disease may result in acquired factor deficiencies (see Chapter 137 ). These disorders tend to present with diffuse bleeding. Well-appearing children are more likely to have localized bleeding or ecchymoses because of thrombocytopenia, von Willebrand disease, platelet function defects, or a rare inherited factor deficiency.
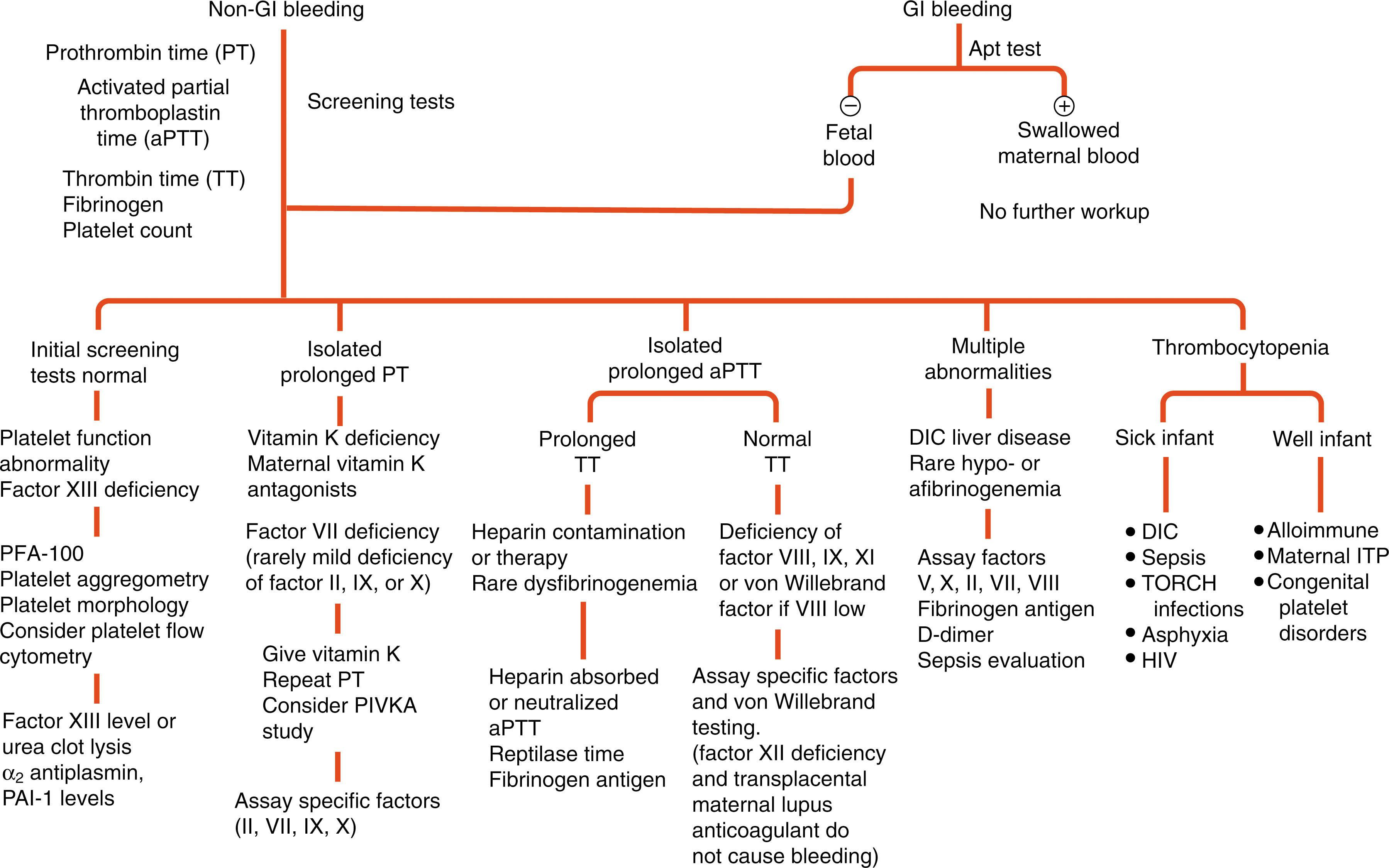
Laboratory evaluation of bleeding in children should include sepsis evaluation and determination of the platelet count, PT/international normalized ratio (INR), aPTT, thrombin time, and fibrinogen concentration ( Table 148.4 ). If the test results are normal, children with a history of bleeding should have levels of FXIII, α 2 AP, and PAI-1 activity determined because deficiencies of these proteins are not detected with routine screening. The approach to laboratory screening in neonates is summarized in Fig. 148.1 , which has been modified from Blanchette and Rand. Platelet function should be evaluated when primary hemostatic defects are suspected. In children with a family history of hemophilia or when hemophilia is suspected, the levels of FVIII and FIX should be determined regardless of the extent of aPTT prolongation.
| Prolonged PT/INR, Normal APTT | Normal PT/INR, Prolonged APTT | Prolonged PT/INR and APTT | Normal PT/INR and APTT |
|---|---|---|---|
|
|
|
|
The following factors are important to consider when evaluating children with thrombocytopenia: congenital or acquired, sick or well, maternal antibody or drug (in case of neonates), and platelet size. Thrombocytopenia is defined as a platelet count less than 150 × 10 9 /L. Causes of thrombocytopenia in children include decreased platelet production, increased platelet consumption, and/or hypersplenism ( Table 148.5 ). Other contributing factors include infection, placental insufficiency, genetic disorders, medications, DIC, or immune deficiency. Rare causes of decreased platelet production in children include primary congenital platelet or marrow disorders and infiltrative disorders.
| Decreased Production | Increased Destruction/Consumption | |||
|---|---|---|---|---|
| Congenital | Acquired | Immune | Non-immune | Sequestration/Consumption |
|
|
|
|
|
Platelet counts in the range of 100 to 150 × 10 9 /L are common in healthy neonates; these mostly reflect transient thrombocytopenia and require no further investigation unless there is an ongoing decrease in the count. More severe thrombocytopenia (platelet count <50 × 10 9 /L) in neonates rarely manifests with bleeding, particularly in the absence of maternal antiplatelet antibodies (see Chapter 129 ). The estimated prevalence of thrombocytopenia is in the range of 1% to 5% of all newborns. The prevalence of thrombocytopenia increases to 22% to 35% in neonates admitted to the neonatal intensive care unit (NICU), with the rates increasing with decreasing gestational age. With severe thrombocytopenia, platelet transfusion may be necessary to treat or decrease the risk of bleeding.
Neonatal alloimmune thrombocytopenia is the platelet equivalent of hemolytic disease of the newborn. It affects approximately 1 in 2000 pregnancies. When fetal platelets express paternal antigens (HPA) that the mother lacks, transplacental passage of maternal immunoglobulin G directed against fetal platelets can occur and usually results in severe neonatal thrombocytopenia (platelet count <30 × 10 9 /L). This may result in major bleeding, particularly ICH, which can occur in 10% to 20% of untreated pregnancies. Incompatibilities for HPA-1a account for the majority of cases of neonatal alloimmune thrombocytopenia in populations of European ancestry. About half of the cases of neonatal alloimmune thrombocytopenia occur in the first pregnancy because fetal platelets pass into the maternal circulation early in the pregnancy. Treatment options include transfusion of antigen-negative platelets if available (HPA-1a ± 5b). Although large, randomized studies are lacking, the threshold count for platelet transfusion in most studies is 30 × 10 9 /L. High-dose intravenous immunoglobulin and/or a trial of random donor platelets can be given if compatible platelets are unavailable. The recommended total dose of intravenous immunoglobulin is 1 to 2 g/kg administered either at a dose of 0.4 g/kg daily for 3 to 5 days or at a dose of 1 g/kg daily for 1 or 2 days.
ITP is a common cause of symptomatic thrombocytopenia in children with an annual incidence of 1 to 6.4 per 100,000. Although ITP can occur at any age, its incidence peaks in children 2 to 5 years of age (see Chapter 129 ). ITP is classified as newly diagnosed (<3 months), persistent (3 to 12 months), or chronic (>12 months) based on the duration of symptoms and the thrombocytopenia. ITP generally presents in an otherwise healthy child, who may have a history of preceding viral illness with a sudden onset of petechial rash, bruising, and/or bleeding. While bleeding symptoms are variable, the majority of children have mucosal bleeding (40%), and only 3% have serious bleeding requiring blood transfusion and/or hospitalization. Intracranial hemorrhage (ICH) is rare and occurs in less than 1% of children with ITP. The diagnosis of ITP is based on typical presentation, isolated thrombocytopenia (platelets <100,000 × 10 9 /L), and an absence of features suggestive of an alternate diagnosis (e.g., signs and symptoms of malignancy or autoimmune conditions, abnormal white count or hemoglobin on CBC, and abnormal peripheral blood smear among others). The management of newly diagnosed ITP patients is based on severity of bleeding symptoms, degree of thrombocytopenia, and medical and social history. Options include observation alone or one of glucocorticoids, IVIG, or anti-D immune globulin. All patients should be advised to restrict high-risk activities and to avoid antiplatelet and anticoagulant medications. Most children with ITP recover within 3 to 6 months, while 10% to 20% go on to have chronic ITP. Risk factors for chronic ITP include older age, lack of preceding infection, and less severe thrombocytopenia. Options for managing chronic ITP include rituximab, thrombopoietin receptor agonists (romiplostim, eltrombopag), splenectomy, and other immunosuppressive medications (see Chapter 129 ).
Qualitative platelet disorders are rarely associated with overt bleeding in young age. Patients presenting with bleeding who have normal coagulation test results and platelet counts require further investigation. Bleeding may be from mucocutaneous sites, sites of blood sampling and procedures, or may present as cephalohematoma and umbilical stump bleeding in neonates. Platelet function disorders range from defects in several structures and signaling pathway as outlined in Table 148.6 . Only the most severe genetic disorders of platelet function present in the neonatal period. These include Glanzmann thrombasthenia and Bernard-Soulier syndrome (see Chapter 124 ).
| Defects in Receptors for Adhesive Proteins |
| Defects in Soluble Agonist Receptors |
|
| Defects in Platelet Granules |
|
| Defects in Signal-Transduction Pathways |
|
| Abnormalities of Cytoskeleton |
|
| Abnormalities of Membrane Phospholipids |
|
Platelet function is affected by commonly used medications, such as aspirin and non-steroidal anti-inflammatory drugs (e.g., ibuprofen, naproxen). Herbal medicines, such as ginkgo biloba, are also known to alter platelet function and can cause bleeding symptoms. In neonates, common medications, such as nitric oxide, prostaglandin E 2 , and indomethacin, can affect platelet function (see Chapter 128 ).
It is challenging to diagnose platelet function disorders in neonates and young children because of the technical limitations of platelet function assays and the need for large volumes of blood for testing (see Chapter 127 ). Initial screening for suspected platelet function disorders can be performed using the PFA-100 analyzer, followed by evaluation of platelet morphology and platelet aggregation responses using light transmission aggregometry. Flow cytometry can be used to evaluate specific surface glycoproteins and electron microscopy studies can be used to assess platelet granule morphology (see Chapter 124 ). Absent platelet aggregation in response to all agonists and deficiency of αIIbβ3 on flow cytometry are diagnostic for Glanzmann thrombasthenia (see Chapter 124 ). Flow cytometry also provides definitive diagnostic information about Bernard-Soulier syndrome, dense granule deficiency, and Scott syndrome.
Platelet transfusions are often given if the patient is bleeding. However, the potential risk of HLA allosensitization if normal platelets are given to patients with congenital deficiency of platelet surface antigens must be weighed against the severity of bleeding when functional defects are suspected. It is recommended that platelet transfusion be restricted to patients with Glanzmann thrombasthenia. Recombinant activated FVII (rFVIIa) has been used to manage serious bleeding and avoid the need for platelet transfusion. Other adjunctive local measures include topical thrombin, fibrin sealants, and antifibrinolytic medications, such as tranexamic acid.
Isolated prolonged PT/INR can be secondary to factor VII deficiency or vitamin K antagonists (e.g., warfarin). Inherited FVII deficiency is a rare, autosomal recessive condition with a strong gene dosage effect (see Chapter 135 ). Neonatal bleeding can occur in severe cases (i.e., homozygosity or compound heterozygosity for two mutations in the FVII gene). FVII deficiency can be associated with microcephaly or midline defects because disruption of chromosome 13q can lead to loss of adjacent genes. As a vitamin K-dependent protein, FVII deficiency can occur in association with deficiencies of the other vitamin K-dependent clotting proteins with abnormalities of the vitamin K pathways. Low doses of rFVIIa can be used for treatment of isolated FVII deficiency; FFP and/or vitamin K can be used for management of combined deficiencies.
Isolated prolonged aPTT can be secondary to deficiencies of factors VIII, IX, XI, XII, HMWK, or prekallikrein and specific or non-specific antibodies (e.g., lupus anticoagulant) affecting these factors (see Chapter 127, Chapter 139 ). Evaluation for FVIII, FIX, and FXI deficiencies should be undertaken immediately in any child with bleeding symptoms and isolated prolongation of the aPTT or a positive family history. Deficiencies of FXII, HMWK, and prekallikrein are associated with prolonged aPTT but do not contribute to bleeding symptoms (see Chapter 135 ). Neonates have a physiologically prolonged aPTT compared with older children and adults; hence, age-appropriate reference ranges must be utilized (see Table 159.2 ).
The association of bleeding with prolongation of both the PT/INR and the aPTT in otherwise healthy children may indicate vitamin K deficiency or congenital deficiencies of prothrombin, FV or FX, as well as rare combined deficiencies (see Chapter 127, Chapter 135 ). Routine prophylactic administration of vitamin K to newborns can complicate the diagnosis of neonatal bleeding related to vitamin K deficiency. More commonly, combined PT and aPTT prolongation occurs in sick children with DIC or severe hepatic disease. Combined factor deficiencies are rare but must be considered when the laboratory findings or clinical course is confusing. Autosomal recessive mutations in LMAN1 (ERGIC-53) or MCFD2 can lead to combined FV and FVIII deficiency because of defective intracellular processing of the factors (see Chapter 135 ). Mutations in γ-glutamyl carboxylase are associated with inherited combined deficiencies of all the vitamin K-dependent proteins. FVII deficiency has rarely been reported in combination with FV, FVIII, FIX, FX, FXI, and protein C defects, as reviewed by Girolami et al.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here