Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Persistent and nonresolving inflammation has been causally linked to many common disorders. Among these, inflammatory bowel disease (IBD), comprising Crohn’s disease and ulcerative colitis, and rheumatoid arthritis (RA) often affect young and middle-aged adults with severe and life impacting symptoms. IBD and RA affect about 1.4 ( ) and 1.5 ( ) million people in the United States, respectively, with total associated cost estimated between $33 and 70 billion ( ). Standard step-care treatments for both IBD and RA begin with glucocorticoids and immunosuppressive drugs (e.g., azathioprine in IBD and methotrexate in RA) and progress to newer, targeted biological or small molecule therapies such as tumor necrosis factor (TNF) and Janus kinase inhibitors ( ). While these biological therapies have improved disease control for many patients, not all respond (primary failure), and clinical responses are often lost over time (secondary failure) due to generation of antagonizing antibodies or other reasons ( ). In addition, these treatments are very expensive and are associated with severe side effects. Thus, there remains a significant need for alternative therapeutic approaches.
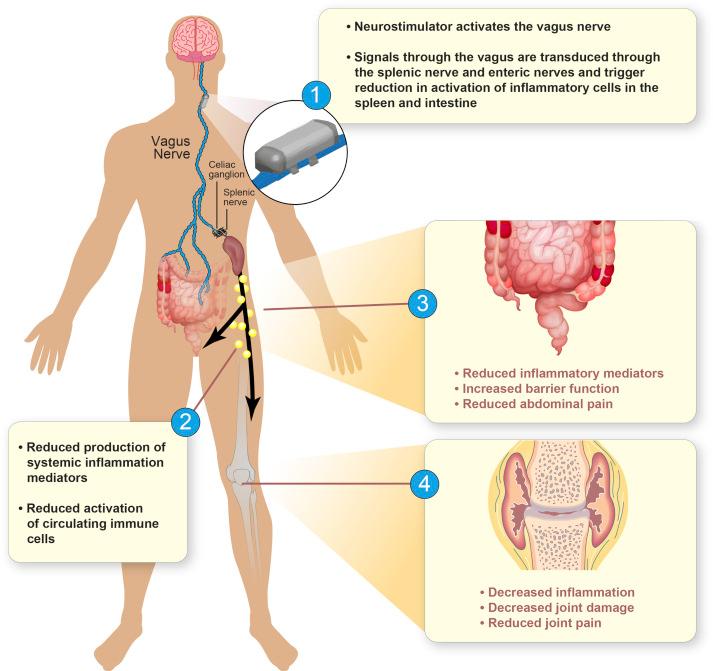
The recent discoveries of neural-immune reflexes have revolutionized our understanding of how the central nervous system (CNS) maintains immunologic homeostasis. One prototypical circuit, the “inflammatory reflex,” utilizes the vagus nerve as a bidirectional conduit, carrying sensory information about peripheral inflammation to the brain (afferent limb) and supplying antiinflammatory signals to immunoactive effector cells in the tissues (efferent limb) ( ). The protective effects of driving the inflammatory reflex, either with drugs targeting molecular components of the circuit or through electrical vagus nerve stimulation (VNS), have been demonstrated in numerous disease models ( ). In standard subacute rodent models of RA and IBD, VNS, using implanted electrodes, reduced the clinical and histological manifestations of disease in the joints or intestines, respectively, and reduced tissue and systemic mediators of inflammation ( ). These studies provided both the rationale and the framework for exploring VNS as a potential nonpharmacologic, bioelectronic treatment for RA and IBD ( ) ( Fig. 127.1 ).
In this chapter, we will discuss the proof-of-concept clinical studies in both RA and IBD. We will describe a novel, miniaturized VNS system that will soon enter studies in RA and IBD, and speculate on ways that this implanted device might be modified in the future to improve usability and function.
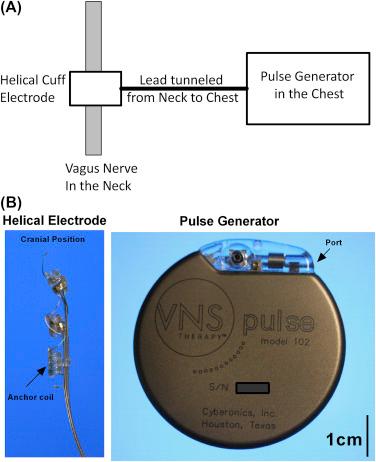
A clinical proof-of-concept study was completed that tested the feasibility of using VNS to treat the sequelae of RA. The investigational study devices used in this study were commercially purchased VNS systems, yet treated as investigational due to their off-label use in patients with RA ( Fig. 127.2 ). The study reported two distinct patient cohorts, an early-stage cohort of patients who have had an insufficient response to the standard first-line oral drug, methotrexate, and a second cohort, including patients who have had an insufficient response to at least two different biologic drugs (e.g., TNF inhibitors and IL-1β receptor antagonists), with at least two different modes of action. This study was designed as a single armed, open-label, proof-of-concept study with a treatment withdrawal period ( ).
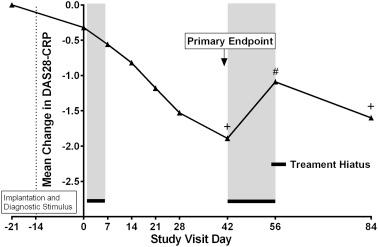
In brief, the devices were implanted, a single intraoperative stimulation was delivered, and the patients healed for approximately 2 weeks. On study day 0, the patients were given a single 60 s train of pulses, with the output current intensity titrated to the maximum tolerated dose. From day 7 to day 42, the patients self-stimulated once to four times daily by magnetically actuating the device. Stimulation trains were delivered at 10 Hz frequency, 0.25 ms pulse width, for 60 s. Following the primary endpoint of the study on the day 42 visit, there was a two-week treatment withdrawal period during which the device was switched off. The device was reactivated on day 56, and patients received stimulation with the same parameters as they had received at the day 42 visit, through the final study visit at day 84 ( ).
The primary study endpoint was the mean change in a standard composite RA study endpoint, the disease activity score 28 (DAS28), between baseline and day 42 visit. The DAS28 is a validated and scaled composite score composed of swollen joints and tender joints counts (maximum of 28), a patient defined, visual analog score (VAS), a global health assessment score, and serum C-reactive protein (CRP) levels ( ). The data showed a highly significant reduction in the mean DAS28 at day 42. The mean DAS28 worsened significantly during the withdrawal period between days 42 and 54 and was reduced once again at day 84 ( Fig. 127.3 ). American College of Rheumatology (ACR) rates of 20%, 50%, and 70% response, secondary clinical endpoints commonly used to measure effectiveness of a therapy in RA clinical trials ( ), were reported as 70.6%, 42.2%, and 11.8% respectively. A significant and DAS28-dependent decrease in IL-6 was reported, as well as significant decreases in whole blood LPS-induced TNF release. There were no serious adverse events (SAEs) or infections and the device was well-tolerated ( ). The study extends the evidence of chronic VNS reducing cytokine production and arthritic symptomatology from animals to humans and provides a clinical proof-of-concept for VNS devices in treating RA.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here