Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The term hemangioma has been used broadly in the past to describe any benign, nonreactive vascular process with an increase in normal or abnormal-appearing vessels or simply abnormally configured vessels. Hemangiomas have been further subclassified pathologically, based on the predominant type of vessel. This was a simple and convenient approach for the pathologist who was often not apprised of the clinical or radiographic findings in a given case but conveyed a limited amount of biologic information to the clinicians. Advances in understanding the pathogenesis of this diverse group of lesions have led to a multidisciplinary consensus that benign vascular lesions be divided into two biologic groups: tumors and malformations ( Tables 20.1 and 20.2 ). This dichotomy has important clinical implications.
| Tumors | Malformations | |||
|---|---|---|---|---|
| Simple | Combined | Of Major Named Vessels | Associated with Other Anomalies | |
| Benign | ||||
| Infantile hemangioma Congenital hemangioma: rapidly involuting (RICH), noninvoluting (NICH), partially involuting (PICH) Spindle cell hemangioma Epithelioid hemangioma Pyogenic granuloma (lobular capillary hemangioma) Others |
Capillary Cutis marmorata telangiectatica congenita Lymphatic Macrocystic Microcystic Gorham-Stout Primary lymphedema Venous Cutaneomucosal Cerebral cavernous Blue rubber bleb nevus Fibroadipose Verrucous Arteriovenous Capillary or arteriovenous malformation Hereditary hemorrhagic telangiectasia |
Capillary-venous Capillary-lymphatic Capillary-arteriovenous Lymphatic-venous Capillary-lymphatic-venous Capillary-venous-arteriovenous Capillary-lymphatic-venous-arteriovenous |
Aneurysm Atresia Ectasia Stenosis |
CLOVES syndrome Klippel-Trenaunay syndrome Megaloencephaly-capillary malformation Maffucci syndrome Sturge-Weber syndrome Proteus syndrome PTEN hamartoma |
| Intermediate | ||||
| Kaposiform hemangioendothelioma/tufted angioma Retiform hemangioendothelioma Dabska-type hemangioendothelioma Composite hemangioendothelioma Epithelioid sarcoma-like/pseudomyogenic hemangioendothelioma Kaposi sarcoma |
||||
| Malignant | ||||
|
||||
| Malformation | Locus | Mutated Gene |
|---|---|---|
| Hereditary capillary malformation (CM) | 5q13-15 | GNAQ |
| Cerebral cavernous (or capillary) malformation (CCM) | 7q11-22 | KRIT1 |
| 7p13-35 | ? | |
| 3q25.2-27 | ? | |
| Hyperkeratotic cutaneous capillary venous malformation (HCCVM) | 7q11-22 | KRIT1 |
| Arteriovenous malformation | 5q13-15? | ? |
| Hereditary hemorrhagic telangiectasia (HHT) | 9q33-34 | ENG |
| 12q11-14 | ALK1 | |
| Venous malformation (VM) | 9p21 | TIE2 (TEK) |
| Glomuvenous malformation | 1p21-22 | GLOMULIN |
| Primary congenital lymphedema (Milroy disease) | 5q34-35 | FLT4 (VEGFR3) |
The International Society for the Study of Vascular Anomalies, based on earlier work, has recommended that the term hemangioma be applied to lesions that arise as a result of cellular proliferation on the presumption that they are true neoplasms . Typically composed of capillary-sized vessels, they grow in a disproportionately rapid manner relative to the patient but, depending on the type, may involute. Vascular malformations, in contrast, are developmental abnormalities of the embryonic vasculature. They develop in utero, typically are evident at birth, in most cases grow proportionately with the patient, and display little or no proliferative activity. They are composed of abnormal arterial, venous, capillary, or lymphatic channels, often in combination. Some are associated with specific genetic defects ( Table 20.2 ).
Despite these defining features, the histologic distinction between hemangiomas and vascular malformations is not always possible without clinical and imaging information. In fact, the growing number of vascular lesions linked to specific genetic defects suggests that these also may ultimately be incorporated into a comprehensive classification scheme. Dividing lesions into hemangiomas and vascular malformations has been attempted to the extent possible. Lesions with an uncertain pathogenesis are discussed at the end of this chapter.
A hemangioma is one of the most common soft tissue tumors and is the most common tumor during infancy and childhood ( Table 20.3 ). Rather than a single entity, hemangiomas represent a group of distinct neoplasms, often with specific clinical and genetic features, and “hemangioma” should not be used as a stand-alone diagnosis without a qualifier (e.g., infantile hemangioma, epithelioid hemangioma).
| Lesion | Clinical Features | Pathologic Features |
|---|---|---|
| Infantile hemangioma | Skin and/or subcutaneous lesion developing in early postnatal period. Rapidly grows and slowly involutes over 1 to 2 years. | Lobules of poorly canalized capillaries with mitotically active endothelium and prominent pericytes. Late lesions with canalized vessels and multilayered basement membrane. Endothelium is GLUT1 positive. |
| Congenital nonprogressive hemangioma | Fully formed at birth with little or no postnatal growth. Pursues noninvoluting (NICH) or rapidly involuting (RICH) course. | Lobules of capillaries with prominent draining veins separated by fibrotic stroma. Endothelium is mitotically inactive and GLUT1 negative. |
| Kaposiform hemangioendothelioma | Congenital or acquired lesion of skin or deep tissues. Most common cause of Kasabach-Merritt phenomenon secondary to platelet trapping. Progressive growth and rare local metastasis. | Irregular cannonball nodules infiltrating tissues composed of slitlike vessels circumscribing glomeruloid vessels containing fibrin thrombi. Endothelium expresses lymphatic markers (LYVE 1, PROX1) but not GLUT1. |
| Vascular malformation | Developmental abnormality of embryonic vasculature presenting at birth. In deep locations, lesions can present later. Grows proportionately with patient. No regression. | Variable mixture of large arteries, veins, venules, and capillaries, some with arteriovenous shunting. Vessels are architecturally abnormal and mitotically inactive. Endothelium is mitotically inactive and GLUT1 negative. |
Most hemangiomas are superficial lesions with a predilection for the head and neck region, but they may also occur internally, such as in the liver. Hemangiomas are typically composed of capillary vessels arranged in lobules, which are subserved by a feeder vessel. This architectural organization has led to the term lobular hemangioma for some capillary hemangiomas. This term is descriptive and not useful for special forms of capillary hemangiomas occurring in the pediatric age group. Although some vascular tumors regress altogether (e.g., infantile hemangioma), most persist if untreated but have limited growth potential. Exceptionally rare examples of angiosarcoma arising in hemangiomas or vascular malformations have been reported, usually in elderly patients. The concept of “benign metastasizing hemangioma” is no longer accepted. Most prove to be angiosarcomas with well-differentiated areas.
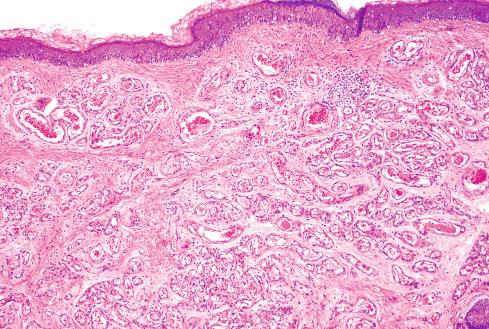
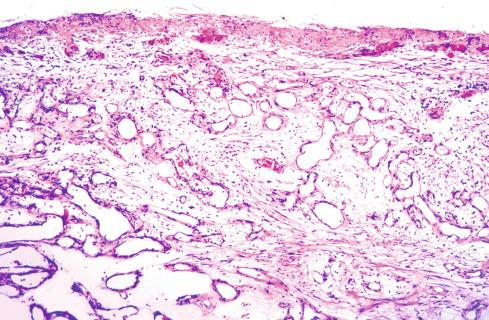
Cherry angioma is a common acquired vascular lesion of adult life. Lesions present as ruby-red papules with a pale halo, measure a few millimeters in diameter, and show a predilection for the trunk and extremity. These lesions may increase in number over time, with some noted to occur in crops in nursing homes, in association with infections and exposure to various chemicals. The lesions, located in the superficial dermis, consist of lobules of capillaries lined by prominent endothelium. With age, the capillaries dilate, resulting in elevation and mild atrophy of the skin ( Fig. 20.1 ). Some lesions have a collarette similar to a pyogenic granuloma.
Infantile hemangioma is a form of capillary hemangioma that affects about 5% of children. Females are affected more often than males by a ratio of 3 to 1. Although most cases are sporadic, some display familial segregation and have been linked to chromosome 5q31-33, suggesting that mutation at this locus predisposes to the tumor. Some sporadic cases may be the result of somatic mutations in VEGFR2 and VEGFR3 . A small subset of infantile hemangiomas has a segmental distribution and is associated with other abnormalities, including p osterior fossa brain malformation, h emangioma, a rterial cerebrovascular abnormalities, c ardiovascular anomalies, and e ye anomalies ( PHACE association). Large segmental infantile hemangiomas overlying the lumbosacral or perineal regions may be associated with a variety of structural abnormalities, including lipomyelomeningocele, tethered cord, and various urogenital malformations.
During the early stage, infantile hemangiomas resemble a common birthmark and are flat, red lesions that intensify in color when the infant strains or cries. With time, they acquire an elevated, protruding appearance that distinguishes them from birthmarks and has earned them the fanciful designation of strawberry nevus ( Fig. 20.2 ). Deeply situated lesions impart little color to the overlying skin and thus may be misdiagnosed preoperatively. These tumors may be in any location but are most common in the head and neck region, particularly the parotid gland, where they seemingly follow the distribution of cutaneous nerves and arteries. The “reticular” variant of infantile hemangioma often involves the hands, with a “biker glove” appearance, and may be associated with lipoatrophy and ulceration.

The evolution of these lesions is characteristic. They appear within a few weeks after birth and rapidly enlarge over several months, achieving the largest size in about 6 to 12 months; they regress over a few years. Regression is usually accompanied by fading of the lesion from scarlet to dull red-gray and by concomitant wrinkling of the once-taut skin. It has been estimated that by age 7 years, 75% to 90% have involuted, leaving a small pigmented scar and a fibrofatty residuum. In the lesions that have ulcerated, the cosmetic defect may be more significant. The clinical phases of infantile hemangioma have distinctive physiologic differences elegantly detailed by Takahashi et al., as described in the following section.
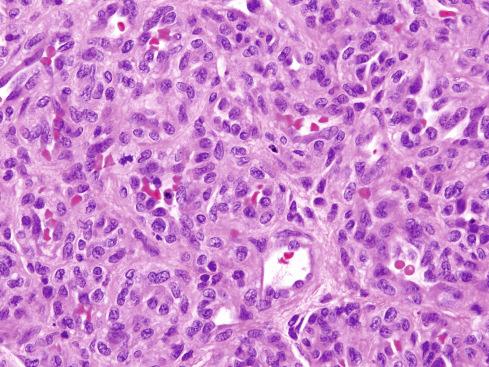
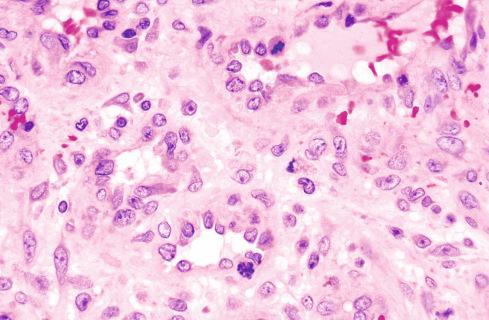
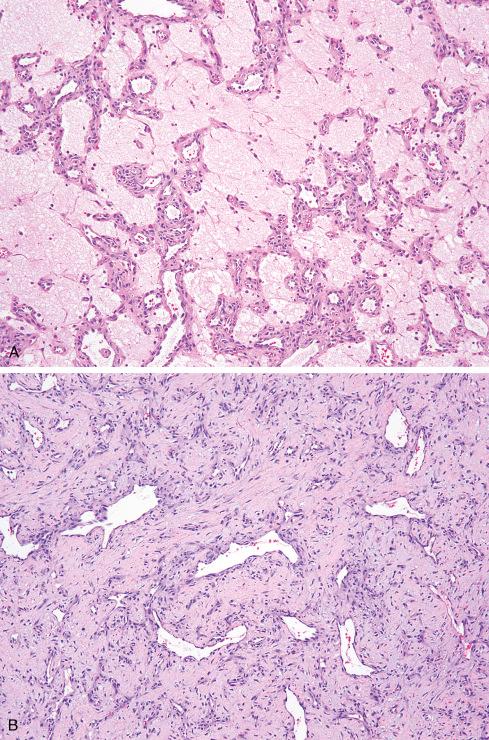
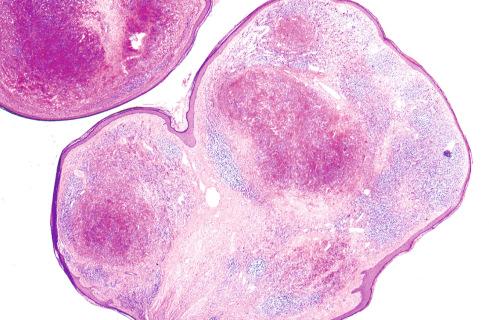
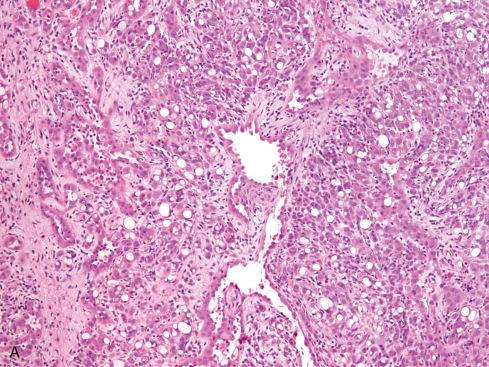
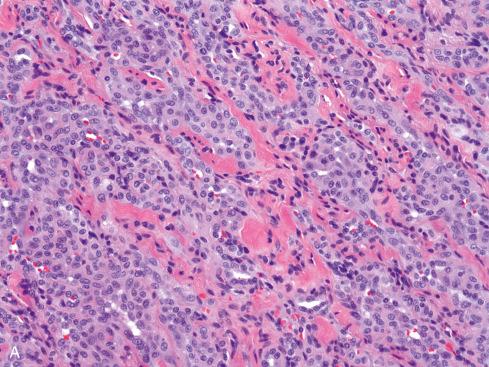
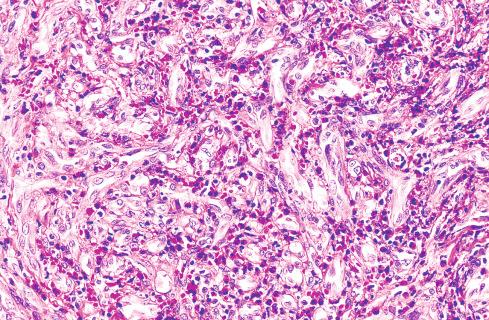
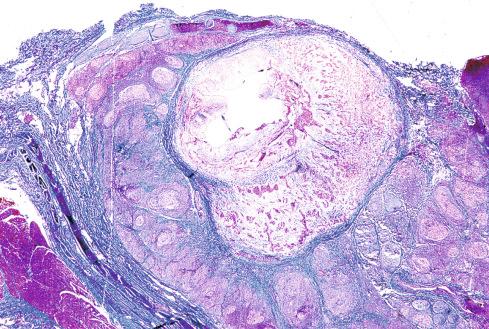
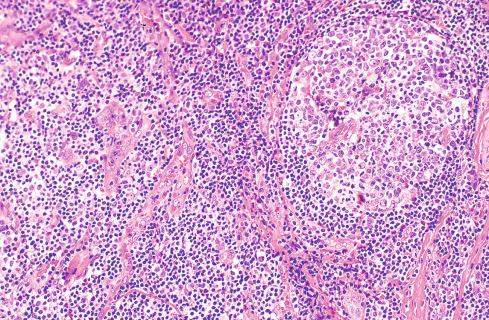
The tumors are multinodular masses fed by a single, normally occurring arteriole ( Fig. 20.3 ). Because they are high-flow lesions, draining vessels may be prominent. Histologically, the tumor varies with its age, although there is no sharp demarcation between proliferative and early involutional phase lesions. Early proliferative lesions are characterized by plump endothelial cells and pericytes with a clear cytoplasm, which form back-to-back small capillaries with inconspicuous lumens ( Fig. 20.4 ). The cellularity of the lesion may be so striking as to obscure the fundamental vascular pattern. Mitotic figures are present in moderate numbers, as are a few apoptotic cells. Mast cells and factor XIIIa–positive interstitial cells are consistent features of these tumors. The former may be important in the production of angiogenic factors that regulate the growth of these tumors. As the lesions mature and blood flow through the lesion commences, the endothelium becomes flattened and the vessel lumens enlarge ( Fig. 20.5 ). Maturation usually begins at the periphery of the tumors but ultimately involves all zones. Involution of infantile hemangioma is accompanied by progressive disappearance of the capillaries, thickening of vascular basement membrane containing apoptotic dust, increased mast cells, and progressive interstitial fibrosis ( Fig. 20.6A ). Large arteries and veins, however, may remain. In unusual cases, infarction of the tumor occurs, presumably as a result of thrombosis.
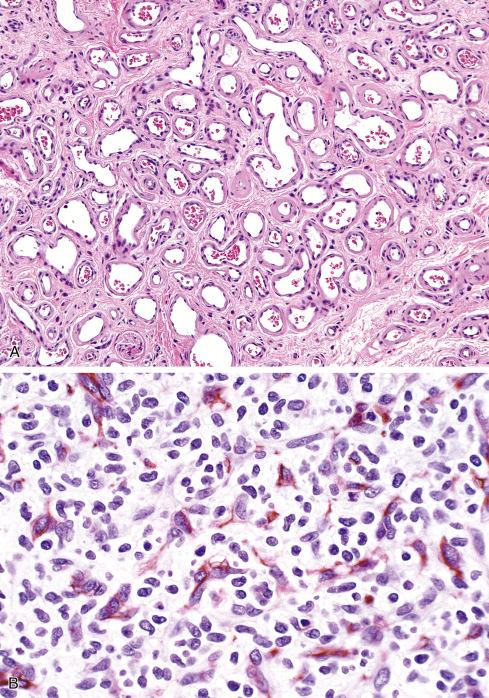
The clinical phases of infantile hemangiomas have been correlated with a distinctive immunophenotypic profile. The traditional vascular markers—CD31, von Willebrand factor (vWF), and smooth muscle actin (a pericyte marker)—are present during the proliferative and involutive phases ( Fig. 20.6B ). The endothelial cells of infantile hemangiomas consistently express GLUT1, a glucose transport receptor ( Fig. 20.6C ). The expression of this receptor is independent of proliferative activity and is not found in other vascular lesions except verrucous venous malformations and occasional angiosarcomas. This protein is also expressed by human placental endothelium and has led to the suggestion that these tumors arise from a vascular precursor cell in the placenta.
Treatment of these lesions must be individualized and depends on factors such as the location and rate of growth. Most tumors can be masterfully neglected and allowed to regress spontaneously. The treatment of infantile hemangiomas is complicated and depends on many clinical factors, and affected patients should be evaluated by a multidisciplinary team with significant experience in the management of pediatric vascular anomalies. The reader is referred to excellent recent review articles on the treatment of these lesions.
Congenital hemangiomas are recently recognized lesions once grouped with infantile hemangioma but that are clinically, morphologically, and genetically distinct. In contrast to infantile hemangioma, they present at birth as fully developed cutaneous lesions. They affect the sexes equally. Multiple lesions, some involving viscera, have been reported. Following birth, the lesions may remain static or rapidly involute. Static and involuting lesions are referred to as noninvoluting congenital hemangioma (NICH) and rapidly involuting congenital hemangioma (RICH), respectively, and represent the most common subtypes of congenital hemangioma. RICH typically regress at a much faster rate than infantile hemangiomas. Other rare, recently identified subtypes of congenital hemangioma are the partially involuting congenital hemangioma (PICH) and the rapidly involuting congenital hemangioma with fetal involution.
Despite the terms RICH and NICH, there is overlap between the two subtypes, indicating that they are part of a common spectrum. In fact, some use the term congenital hemangioma and modify it as appropriate when clinical history is available. Clinically, both RICH and NICH at birth display many similarities, both being dome shaped with cutaneous telangiectasias and a peripheral pallor, although RICH tends to have a higher dome shape than NICH, may have a shiny, red, and tense surface, and often develops a central depression or ulcer as it regresses ( Fig. 20.7A and B ). Both are composed of capillary lobules separated by dense fibrous tissue containing atrophic adnexal structures ( Fig. 20.7C ). RICH is generally characterized by small capillary lobules with modestly plump endothelial cells and pericytes, often a minimally prominent centrilobular draining channel, and foci where the lobules seem to have vanished, leaving a fibrous residuum and thin-walled draining vessels ( Fig. 20.7D ). Stromal arteries and veins are often prominent, and there may be calcareous deposits, cysts, and arteriovenous shunts. Draining and feeding vessels within these lesions can be quite prominent and suggest a vascular malformation if few lobules remain.
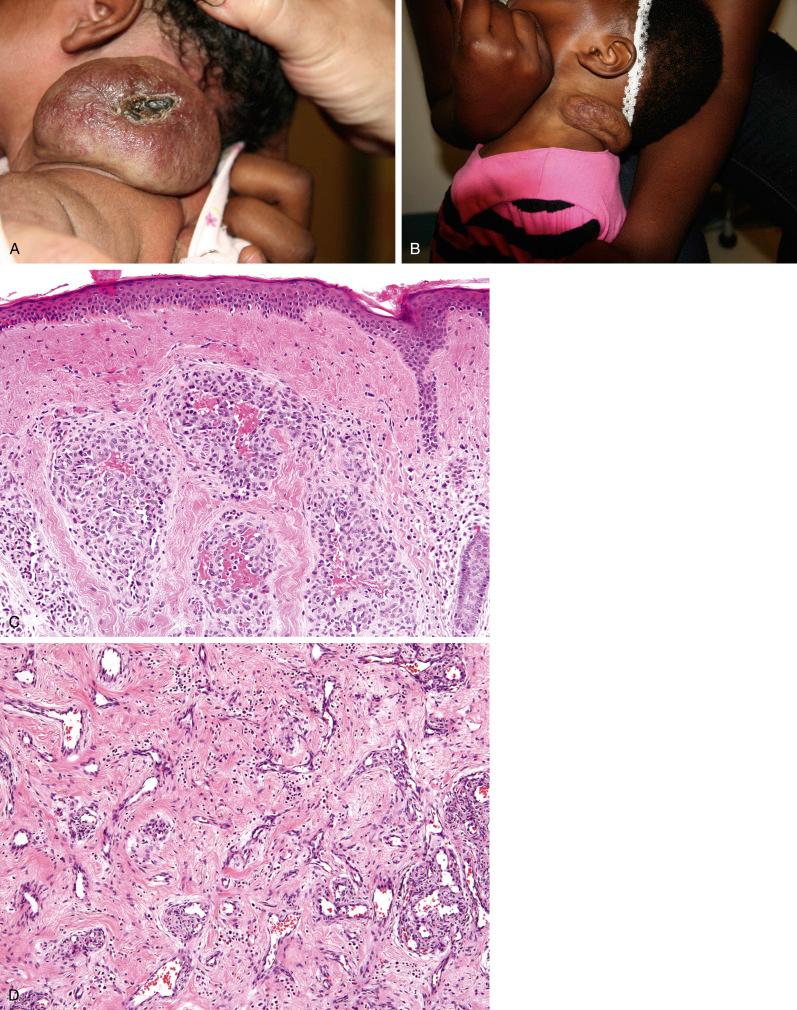
The initial histopathologic features of NICH are unknown, since they are removed after failure to involute. In most lesions the lobules vary in size, but some are large with peripheral small capillary channels, hobnailed endothelium, and large central veins ( Fig. 20.7E and F ). Eosinophilic globules may be present within the endothelial cells ( Fig. 20.7G and H ). The interlobular fibrous stroma has prominent arteries and veins, and small arteriovenous shunts occasionally are discernible. In some NICHs the lobular architecture is less distinct, with the lobules seemingly engulfed by the prominent intra- and interlobular vasculature. In some long-standing NICHs the high blood flow to the lesions may mimic an arteriovenous malformation.
The endothelial cells of both NICH and RICH are negative for GLUT1, a useful feature in the distinction of these lesions from infantile hemangioma. Mutations in the GNAQ and GNA11 genes have been identified in NICH and RICH.
The pyogenic granuloma is a polypoid lobular capillary lesion occurring on the skin and mucosal surfaces. Its pathogenesis is controversial, with some considering it a neoplasm and others a reactive hyperplasia. The lobular architecture has prompted some to use “lobular capillary hemangioma” for this lesion. Their appearance following trauma, during pregnancy (granuloma gravidarum), and during retinoid therapy suggests a reactive etiology for at least some cases of pyogenic granuloma. On the other hand, the presence of genetic mutations in subsets of pyogenic granulomas would seem to support the neoplastic nature of at least some.
Pyogenic granulomas bear a striking resemblance to granulation tissue, and in fact, most early pathologists considered them infectious. Poncet and Dor, credited with the first description, believed that these lesions were secondary to infection by Botryomyces organisms, whereas others implicated pyogenic bacteria, specifically Staphylococcus . Uncomplicated lesions, however, lack ulceration and inflammation and resemble other capillary hemangiomas.
These tumors occur on either the skin or the mucosal surfaces, although the latter accounts for about 60% of all cases. In the extensive review of 289 cases by Kerr, the gingiva, fingers, lips, face, and tongue accounted for more than 70% of cases. The genders are affected approximately equally, and the disease is evenly distributed over all decades. Approximately one-third develop following minor trauma, and in rare cases, pyogenic granuloma–like lesions develop in port-wine stains and other vascular anomalies. Multiple lesions may develop simultaneously, but this phenomenon almost always occurs in the cutaneous rather than the mucosal form of the disease. Disseminated (eruptive) forms of pyogenic granuloma have been reported, some after surgical removal of a solitary pyogenic granuloma. A rare form of congenital disseminated pyogenic granuloma has also been described. Disseminated pyogenic granulomas progress for a limited time and ultimately stabilize or regress. The mechanism for these initially alarming presentations is not clear, although some have suggested the release of angiogenic factors by the tumors. Usually the tumors develop rapidly and achieve their maximal size of several millimeters to a few centimeters within a few weeks or months. The well-established lesion is a polypoid, friable, purple-red mass that bleeds easily and frequently ulcerates. Sessile forms of this tumor also occur, but they tend to be recurrent lesions.
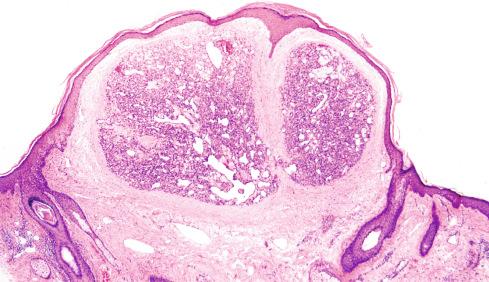
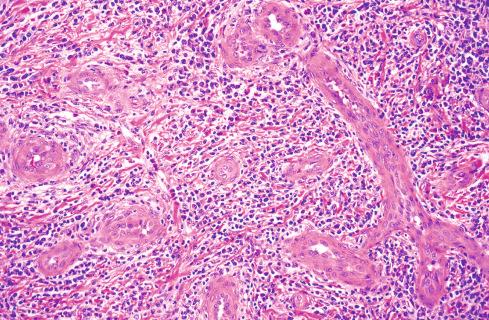
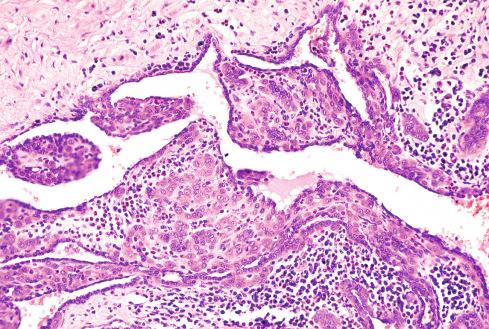
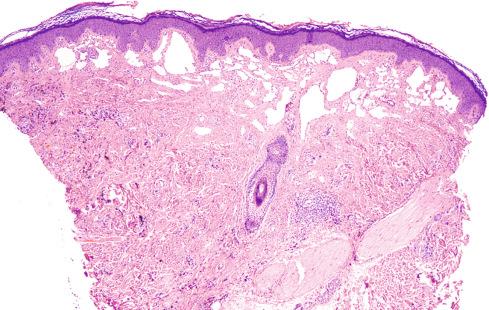
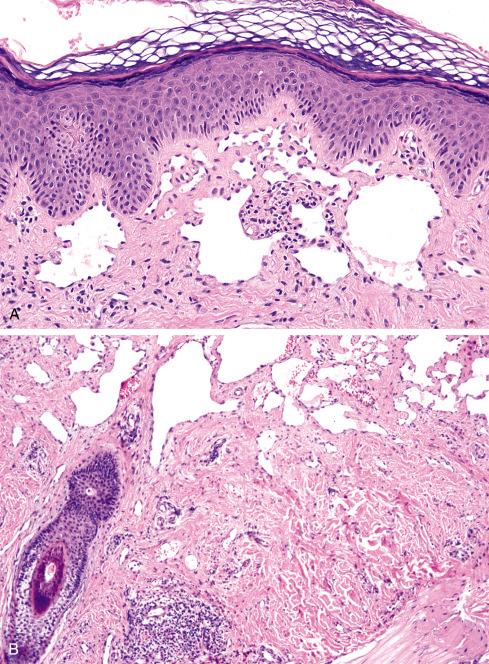
The appearance of these lesions at low magnification immediately suggests the diagnosis. They are a distinctly exophytic growth connected to the skin by a stalk of varying diameter and occasionally are surrounded by a heaped-up collar of normal tissue ( Figs. 20.8 to 20.12 ). The adjacent epithelium is hyperkeratotic or acanthotic, but the epithelium overlying the lesion itself is flattened, atrophic, or ulcerated. The basic lesion is a lobular (capillary) hemangioma set in a fibromyxoid matrix. Each lobule of the hemangioma is made up of a larger vessel, often with a muscular wall and surrounded by congeries of small capillaries. Most lesions, however, are altered by secondary inflammatory changes and thus have been likened to granulation tissue. Both acute and chronic inflammatory cells are scattered throughout the lesion but, not unexpectedly, are most numerous at the surface. Secondary invading microorganisms are occasionally present in the superficial reaches of ulcerated lesions. Stromal edema may separate the capillary lumens and obscure the lobular arrangement of the tumor ( Fig. 20.11 ). Mitotic activity may be brisk in the endothelium and stromal fibroblasts when secondary changes are present, such as edema and inflammation. In lesions that involute, a progressive stromal and perivascular fibrosis ensues. Rarely, pyogenic granulomas display epithelioid change of the endothelium (see later, Epithelioid Hemangioma). Pyogenic granulomas involving the nasal cavity often show striking stromal hyalinization and myxoid change, which may obscure the underlying lobular architecture, resulting in confusion with other highly vascular tumors of the nose, such as nasopharyngeal angiofibroma and sinonasal glomangiopericytoma ( Fig 20.13 ).

The clinical appearance of these lesions is quite characteristic and assists in the distinction between lesions such as well-differentiated angiosarcoma or an angiomatous form of Kaposi sarcoma. Pyogenic granuloma is a more or less circumscribed lesion, often with a lobular arrangement, in contrast to the rambling, poorly confined nature of malignant vascular neoplasms. The manner in which even well-differentiated angiosarcomas dissect through connective tissue and form irregular vascular spaces contrasts sharply with pyogenic granuloma. Kaposi sarcoma also is not well circumscribed and contains at least focal cellular zones of spindled cells, which form the classic slitlike vascular spaces. However, these diagnostic areas are typically located in the central or deep areas of the tumor, whereas the well-differentiated angiomatous component is seen peripherally or superficially. In difficult cases, immunohistochemistry for human herpesvirus 8 (HHV8) LANA protein may be of value in the distinction of angiomatous forms of Kaposi sarcoma from pyogenic granuloma. Therefore, in some instances, a superficial biopsy of a vascular neoplasm may not be adequate to exclude malignancy. Disseminated congenital pyogenic granulomas lack GLUT1 expression, distinguishing them from infantile hemangioma.
Although pyogenic granulomas are benign lesions, 16% were noted to recur in one large series of tumors treated conservatively. Mills et al. reported a significantly lower recurrence rate in 73 cases. Recurrent disease may present as a solitary nodule or as multiple small satellite nodules around the site of the original lesion. Analyzing the phenomenon of satellitosis in this disease, Warner and Wilson-Jones found that most of these lesions occurred on the trunk, particularly the scapular area, and most had been incompletely excised initially. In contrast to the original tumors, the satellites usually are not pedunculated but rather are sessile and have an intact surface epithelium. In these respects, they grossly resemble ordinary acquired adult hemangiomas. Although the rapid development of numerous satellite lesions often alarms the clinician, these lesions usually respond to reexcision and in some cases have even regressed spontaneously.
At the genetic level, subsets of pyogenic granulomas harbor mutations involving the KRAS , NRAS , HRAS, and BRAF genes. Those lesions that arise from capillary malformations often show GNAQ and BRAF mutations.
Granuloma gravidarum is a pyogenic granuloma that occurs on the gingival surface during pregnancy. Gingival changes occur in an estimated 50% of pregnant women, only about 1% of whom develop localized tumors. Typically, these lesions develop abruptly during the first trimester and arise from the interdental area of the gum. They are grossly and histologically indistinguishable from the ordinary form of pyogenic granuloma. They usually regress dramatically following parturition, although many persist as small mucosal nodules capable of renewed growth at the time of subsequent pregnancies. This unusual tumor has provided some of the most compelling evidence that the pyogenic granuloma lacks the degree of autonomous growth that characterizes most vascular tumors of adulthood. Hormone sensitivity manifested by granuloma gravidarum has led many to conclude that these are not neoplastic lesions.
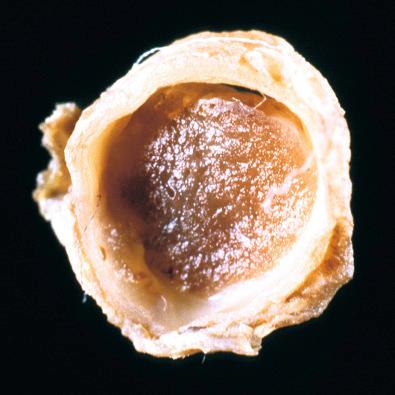
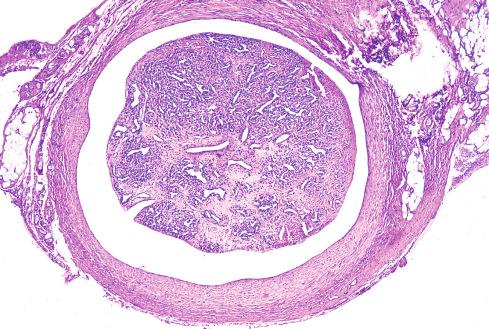
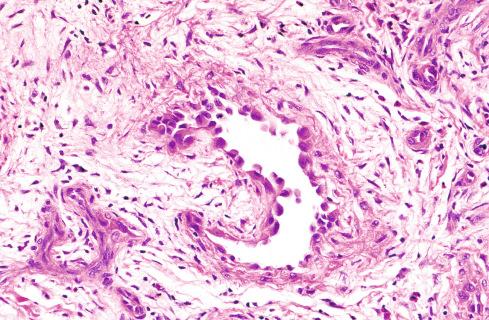
Cooper et al. recognized an intravenous counterpart of pyogenic granuloma that occurs most often on the neck and upper extremity and presents as a red-brown intravascular polyp that can be easily mistaken for an organizing thrombus ( Fig. 20.14 ). It arises from the venous wall and protrudes deeply into the lumen but remains anchored to the wall by means of a narrow stalk containing the feeder vessels. Intravenous pyogenic granuloma is covered by a lining of endothelium, and the stroma often contains smooth muscle fibers, presumably remnants of the wall of the vein. Histologically, it is identical to uncomplicated pyogenic granuloma in that it displays no inflammatory or ulcerative change ( Fig. 20.15 ). Occasionally, intravascular pyogenic granuloma–like foci may be seen within benign vascular malformations. As with other pyogenic granulomas, they are benign and display no tendency to spread in the bloodstream.
Intramuscular hemangiomas of capillary type most likely represent true neoplasms. Unlike cutaneous hemangioma, intramuscular hemangioma affects the genders about equally, and 80% to 90% make their appearance before age 30 years. Although any muscle can be affected, those of the lower extremity (particularly the thigh), trunk, and head and neck are most often involved.
Clinically, intramuscular lesions are more likely to pose diagnostic problems than superficial hemangiomas. Capillary-type intramuscular hemangiomas present as enlarging soft tissue masses with few signs or symptoms to reveal their vascular nature. In particular, there is rarely any overlying discoloration of the skin, visible pulsation, or audible bruit. Radiography and magnetic resonance arteriography (MRA) are much more helpful for suggesting the diagnosis. Plain films may reveal phleboliths in addition to a soft tissue mass, and MRA may demonstrate a highly vascular lesion with early venous runoff. Moreover, the vessels are oriented parallel to one another in a striated pattern. This pattern, created by the orderly entry and proliferation of vessels between fascicles of muscle, is considered a helpful feature in support of the benignancy of the lesion. Pain is a frequent but not invariable symptom and may be more common with tumors involving long, narrow muscles, where stretching of the muscle and nerve fibers by the tumor is more intense. Occasionally, function is impaired, or anatomic deformity occurs. Although a history of trauma is given in about one-fifth of cases, there is no evidence that the lesions are caused by trauma.
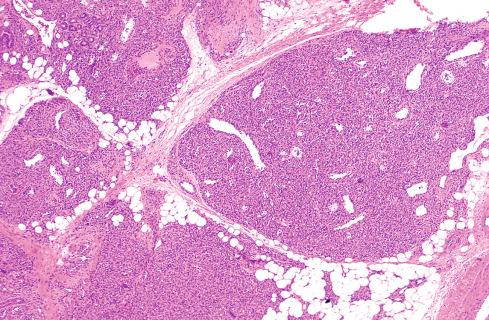
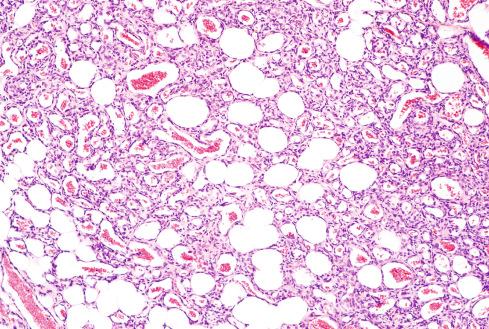
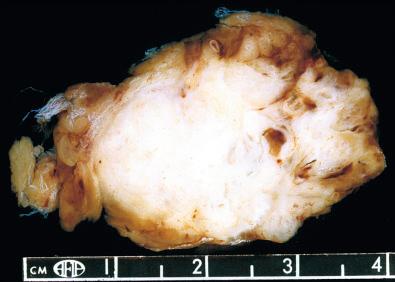
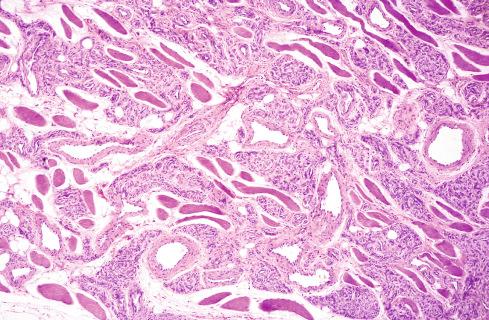
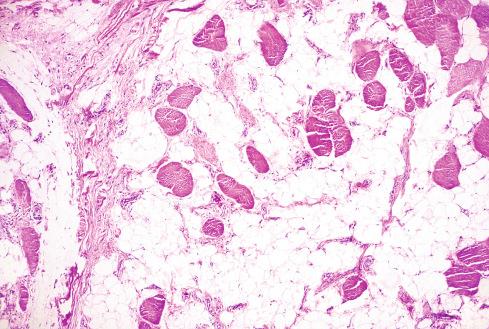
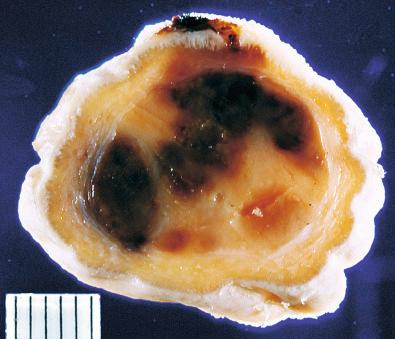
Intramuscular hemangiomas of the capillary type may be confused with a malignant tumor. Grossly, they do not always appear vascular because they vary from tan to yellow or red ( Fig. 20.16 ). They are composed of a myriad of small, capillary-sized vessels with plump nuclei that extend between individual muscle fibers ( Figs. 20.17 and 20.18 ). Well-developed lumen formation is apparent in most areas, although occasional tumors have a lobular or solidly cellular appearance similar to the early stage of infantile hemangioma. Occasional cases show mitotic activity, intraluminal papillary tufting, and a proliferation of capillary vessels in perineural sheaths. Although seemingly disturbing features, none of these features is indicative of malignancy. The presence of adipose tissue in these tumors is common, and at times it may be so conspicuous as to suggest a diagnosis of lipoma. Tumors described in the early literature as “infiltrating angiolipomas of muscle” or “benign mesenchymoma” are examples of intramuscular hemangiomas with striking fatty overgrowth ( Fig 20.19 ).
The most important consideration in the differential diagnosis of these lesions is the distinction from an angiosarcoma of skeletal muscle. Angiosarcomas of deep soft tissue, specifically skeletal muscle, are rare (see Chapter 22 ); therefore, a vascular lesion of skeletal muscle is much more likely to be benign than malignant. Moreover, capillary-type intramuscular hemangiomas do not develop the freely anastomosing sinusoidal pattern, except in areas where organization of thrombus material occurs. Their recurrence rate varies from 18% to 50%, depending on adequacy of excision. Treatment should be directed toward complete excision without resorting to radical surgery. Prior embolization of the tumor has been used as a means to facilitate surgical excision.
Epithelioid hemangioma is an unusual but distinctive vascular tumor that was first described as angiolymphoid hyperplasia with eosinophilia and subsequently as inflammatory angiomatous nodule, atypical or pseudopyogenic granuloma, and histiocytoid hemangioma. However, the lesions reported in the Japanese literature as Kimura disease represent a different entity.
Epithelioid hemangiomas typically occur during early to middle adulthood (ages 20-40) and affect women more often than men. Most are situated superficially in the head and neck, particularly the region around the ear. As a result, they can be detected relatively early as small, dull-red, pruritic plaques. Crusting, excoriation, bleeding, and coalescence of lesions are common secondary features. About half the patients develop multiple lesions, generally in the same area. Affected patients appear relatively well, although occasionally significant regional lymph node enlargement and eosinophilia of the peripheral blood accompany the lesions.
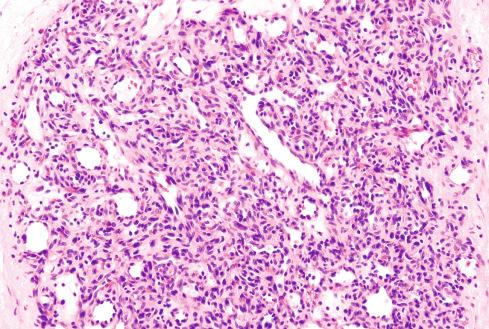
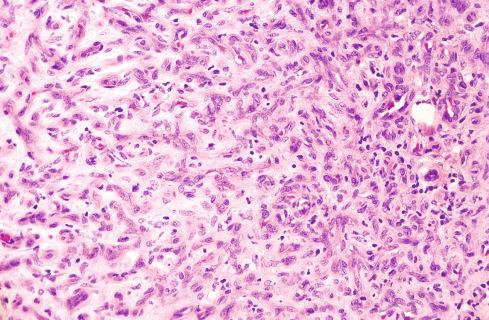
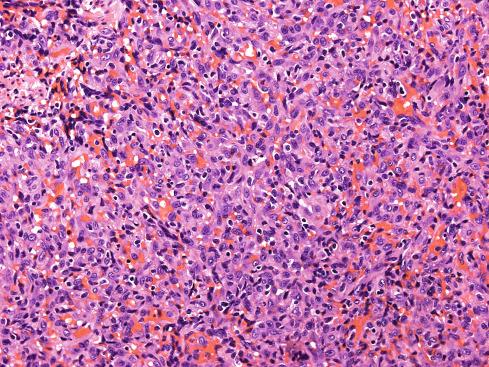
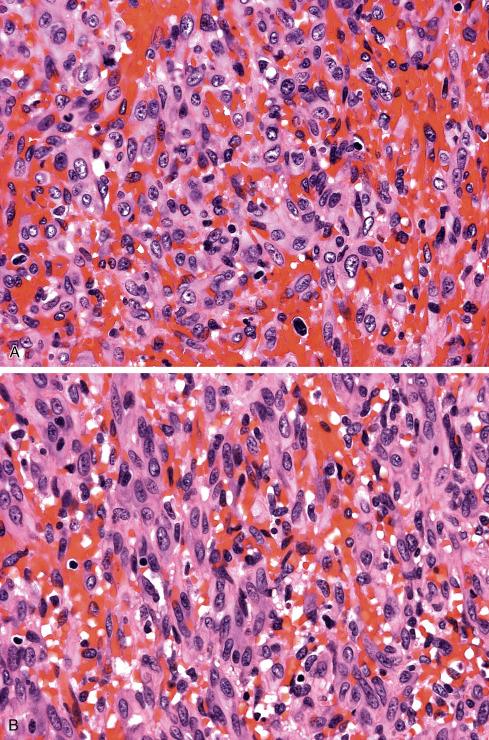
These tumors are circumscribed lesions of the subcutis or dermis ( Figs. 20.20 and 20.21 ), but occasionally involve deep soft tissue, vessels, or parenchymal organs. As with other capillary hemangiomas, epithelioid hemangiomas consist of lobules of small, capillary-sized vessels centered around a larger central vessel ( Fig. 20.22 ). In most cases, the capillary vessels are well-formed, multicellular channels with perceptible lumina. However, in epithelioid hemangiomas that are large and deep, the canalization of the vessels may be poor and suggest the lesion consists of solid sheets of epithelioid to slightly spindled cells ( Figs. 20.23 and 20.24 ). Solid forms of epithelioid hemangioma are problematic for pathologists and occasionally are misdiagnosed as epithelioid sarcoma or epithelioid angiosarcoma (see later text).
The hallmark of these lesions is the epithelioid endothelial cells that line most, but not necessarily all, of the vessels and protrude deeply into the lumen like tombstones ( Figs. 20.25 to 20.29 ). The epithelioid endothelial cells have rounded or lobated nuclei and abundant acidophilic cytoplasm containing occasional vacuoles that represent primitive vascular lumen formation. Although they have many of the ultrastructural features of normal endothelium, including micropinocytotic vesicles, antiluminal basal lamina, and Weibel-Palade bodies, there are also differences. Adjacent cells are often separated by rather large gaps and interdigitate only along their lateral basal borders by means of tight junctions. Organelles are more abundant in these cells and include increased numbers of mitochondria, smooth and rough endoplasmic reticulum, free ribosomes, and thin cytofilaments.
Epithelioid hemangiomas are typically associated with a prominent inflammatory component. Eosinophils are particularly characteristic of these tumors, but lymphocytes, mast cells, and plasma cells are also present. Lymphoid aggregates replete with germinal centers are occasionally present but may be a feature of long-standing lesions or a peculiar host response.
Although about one-third of these lesions recur, virtually none has produced metastasis. One case reported by Reed and Terazakis evidently gave rise to microscopic metastases in a regional lymph node, but this appears to be a unique event. Rare lesions have been noted to regress spontaneously, but usually surgical excision is required. About 80% of reported patients have responded at least partially to superficial radiotherapy, but cryotherapy and injection of intralesional steroids have not met with success.
Despite their benign behavior, controversy exists as to whether the lesions are reactive or neoplastic. The fact that 10% occur following trauma, are symmetrically arranged around a vessel with mural damage ( Fig. 20.30 ), and are associated with a prominent inflammatory response has led some to conclude they are reactive ( Fig. 20.31 ). On the other hand, epithelioid hemangiomas can occur on a multifocal basis and are associated with local recurrences and, in extraordinary cases, with regional lymph node deposits. The most plausible reconciliation for these divergent observations is that the entity is heterogeneous, and that the various lesions included under this umbrella are linked by epithelioid change of the endothelium. The prevailing view is that epithelioid change is an altered functional state of endothelium that may be encountered in benign and malignant vascular tumors as well as in reactive vascular lesions.
Recent genetic evidence supports the neoplastic nature of at least some epithelioid hemangiomas. FOSB alterations have been identified in a subset of epithelioid hemangiomas, in particular those of penile origin or those having atypical morphologic features, such as necrosis. Fluorescence in situ hybridization (FISH) subsequently confirmed these findings, most often in highly cellular lesions, but not in cases with angiolymphoid hyperplasia–like features. In contrast, FOSB protein expression has been identified in about half of epithelioid hemangiomas, including those with angiolymphoid hyperplasia–like features. Interestingly, cases classified as “epithelioid angiomatous nodule,” a lesion whose relationship to epithelioid hemangioma is controversial, are FOSB-negative.
The differential diagnosis of epithelioid hemangioma includes the full spectrum of epithelioid vascular lesions, most often epithelioid hemangioendothelioma and occasionally other epithelioid tumors. In contrast to epithelioid hemangiomas, epithelioid hemangioendotheliomas are angiocentric tumors with a distinctive myxohyaline or chondroid background. The cells are arranged in short cords or chains rather than in multicellular vascular channels and rarely have a prominent inflammatory component. Epithelioid hemangiomas with solid or medullary zones may be mistaken for epithelioid angiosarcomas. The most important observation in this regard is the nuclear grade of the cells. Epithelioid angiosarcomas are invariably high-grade lesions composed of large cells with prominent nuclei and nucleoli that sharply contrast with the nuclei of epithelioid hemangioma.
It is unclear whether epithelioid angiomatous nodule is a variant of epithelioid hemangioma with a predominantly solid growth pattern, or a separate lesion. As with epithelioid hemangioma, it presents as dermal nodules, occasionally displays multicellular vascular channel formation and inflammation, and pursues a benign course. Unlike epithelioid hemangioma, epithelioid angiomatous nodule is FOSB negative.
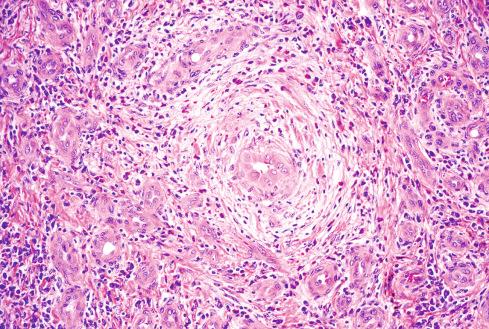
The lesion first described by Kim in the Chinese literature and later by Kimura et al. in the Japanese literature as Kimura disease is a chronic inflammatory condition that appears to be endemic in the Asian population and occurs only infrequently in Western populations. Although formerly thought to be identical to epithelioid hemangioma (angiolymphoid hyperplasia), many data indicate they are unrelated lesions with only a few superficial histologic similarities. Kimura disease is often confused with angiolymphoid hyperplasia (epithelioid hemangioma) largely because the term was inappropriately applied to classic examples of angiolymphoid hyperplasia. In fact, the two lesions are clinically and histologically quite different. Kimura disease presents as lymphadenopathy with or without an associated soft tissue mass. Peripheral eosinophilia is almost always present. Increased serum immunoglobulin E (IgE), proteinuria, and nephrotic syndrome may also occur as part of the disease. Lesions are most common in the subcutis of the head and neck area, although lesions have been noted in the groin, extremities, and chest wall. There is a striking male predilection in Kimura disease. The lesions are characterized by dense, lymphoid aggregates containing prominent germinal centers ( Fig. 20.32 ). Within the germinal centers, one occasionally identifies nuclear debris, polykaryocytes, and a delicate eosinophilic matrix. Immunohistochemical procedures reveal that IgE-bearing cells, corresponding to the distribution of dendritic reticulum cells, populate the germinal center. Thin-walled vessels, with the characteristics of postcapillary venules, reside adjacent to the germinal centers, occasionally dipping into the centers. Dense infiltrates of eosinophils adjacent to the lymphoid aggregates occasionally form eosinophilic abscesses. During the late stages of the disease, a dense hyaline fibrosis supervenes. The adherence of the mass to the surrounding structures often triggers alarm in the surgeon regarding the possibility of malignancy. Affected lymph nodes show exuberant follicular hyperplasia with preservation of the architecture. The changes in the germinal center are as described previously for soft tissue lesions.
The etiology of this condition is unknown, although the peripheral eosinophilia and elevated serum IgE suggest an immunologic reaction to an unknown stimulus. The lesions are benign, but recurrence may develop after surgical excision. There are no instances of malignancy supervening on these peculiar lymphoid proliferations.
Although Kimura disease and angiolymphoid hyperplasia both have a lymphoid infiltrate with eosinophils, there are rather striking differences. The vascular proliferation in Kimura disease is relatively minor and is eclipsed by the inflammatory component. Moreover, the vessels in Kimura disease are not lined by epithelioid endothelium but by more attenuated endothelial cells.
Hobnail hemangioma, described by Guillou et al., develops on the skin of the extremities in young adults as an angiomatous/pigmented or exophytic mass and has a distinctive biphasic appearance ( Figs. 20.33 and 20.34 ). The superficial portion of the lesion consists of dilated vessels lined by hobnail endothelial cells containing occasional intraluminal papillary tufts similar to the Dabska tumor (see Chapter 21 ). The deep portion consists of attenuated, slitlike capillaries that ramify in the dermis. Although the pattern suggests an angiosarcoma, the vessels have an innocuous appearance. Hemorrhage, hemosiderin deposits, lymphocytes, and dermal sclerosis can accompany the lesions. The endothelial cells in hobnail hemangiomas are CD31, VEGFR3, and D2-40 positive and CD34 negative, indicating a lymphatic phenotype similar to retiform hemangioendothelioma. The lesional vessels lack a pericytic cuff as would be expected for small lymphatic vessels. Microshunts between small blood and lymphatic vessels may explain the frequent microaneurysms, hemorrhage, inflammatory changes, and scarring that are typical of these lesions. The cases reported (>50) have had a benign clinical course.
Hobnail hemangiomas correspond to some lesions originally termed targetoid hemosiderotic hemangioma . However, this is a clinical term referring to the presence of an ecchymotic halo surrounding a violaceous papule, and it is unclear whether these clinically defined lesions have a common pathologic appearance. The term hobnail hemangioma has therefore proved to be more useful to pathologists.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here