Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Q34.1 What is the difference between an ‘antiandrogen’ and ‘androgen inhibitor’? (Pg. 367)
Q34.2 For which skin disorders are antiandrogens and androgen inhibitors clinically useful from a mechanistic standpoint? (Pgs. 367, 368)
Q34.3 What are the key differences in type I versus type II isoenzymes of 5-α reductase, and how do these differences relate to the response to antiandrogen therapies? (Pgs. 368, 376, 378)
Q34.4 Concerning spironolactone (1) what are the primary biologic effects, and (2) what is the metabolite that contributes to the majority of the drug’s effects (Pgs. 369, 371)
Q34.5 What are several measures to reduce the incidence of menstrual irregularities in women treated with spironolactone? (Pg. 371)
Q34.6 What are the primary recommendations for women receiving spironolactone concerning the possibility of estrogen-dependent malignancies (including data for/against this risk)? (Pg. 372)
Q34.7 What are the most important drug interactions for spironolactone/drospirenone? (Pgs. 373, 375)
Q34.8 What are the progestins with antiandrogenic properties? (Pgs. 373x2, 380)
Q34.9 What are the FDA-approved antiandrogens or androgen inhibitors used to treat skin disorders? (Pgs. 376, 380)
Q34.10 What are the effects of finasteride on sexual function, if any? (Pg. 377)
Q34.11 What is the effect of finasteride on prostate-specific antigen (PSA) levels, and how should values for this test be ‘adjusted’ for men receiving finasteride? (Pg. 378)
Q34.12 What are the data that quantify the small risk of venous thromboembolism in women receiving hormonal contraceptives? (Pg. 380)
Q34.13 Which drugs truly alter hormonal levels of hormonal contraceptives through the cytochrome P-450 system, and can therefore definitively lead to contraceptive failure? (Pg. 380)
Q34.14 What role do herbal remedies play in treating androgen-related skin disorders? (Pg. 381)
Angiotensin-converting enzyme
Adverse effects
Androgenetic alopecia
Androgen receptor
Body mass index
Benign prostatic hypertrophy
Cutaneous disorders of hyperandrogenism
Congestive heart failure
Chronic kidney injury
Combined oral contraceptives
Cytochrome P450
Cyproterone acetate
Dehydroepiandrosterone
Dehydroepiandrosterone sulfate
Dihydrotestosterone
Deoxyribonucleic acid
Drosperinone
Ethinyl estradiol
US Food and Drug Administration
Female-patterned hair loss
Follicle-stimulating hormone
Glomerular filtration rate
Gonadotropin-releasing hormone
Hydroxysteroid dehydrogenase
Intrauterine device
Luteinizing hormone
Messenger ribonucleic acid
National Institutes of Health
Nonsteroidal anti-inflammatory drug
Oral contraceptive
Polycystic ovary syndrome
Persistent erectile dysfunction
Progestin-only pills
Progesterone receptor
Prostate-specific antigen
Randomized controlled trial
Sex hormone-binding globulin
Selective serotonin reuptake inhibitor
Venous thromboembolism
Circulating androgens can profoundly influence target cutaneous structures such as the pilosebaceous unit (hair follicle and sebaceous gland) and play a central role in the pathogenesis of cutaneous disorders of hyperandrogenism (CHA) which include androgenetic alopecia (AGA), acne vulgaris, and hirsutism ( Box 34.1 ). Androgens also appear to play a role in hidradenitis suppurativa.
Acne vulgaris
Androgenetic alopecia (AGA)
Female pattern AGA
Male pattern AGA
Hirsutism
Hidradenitis suppurativa
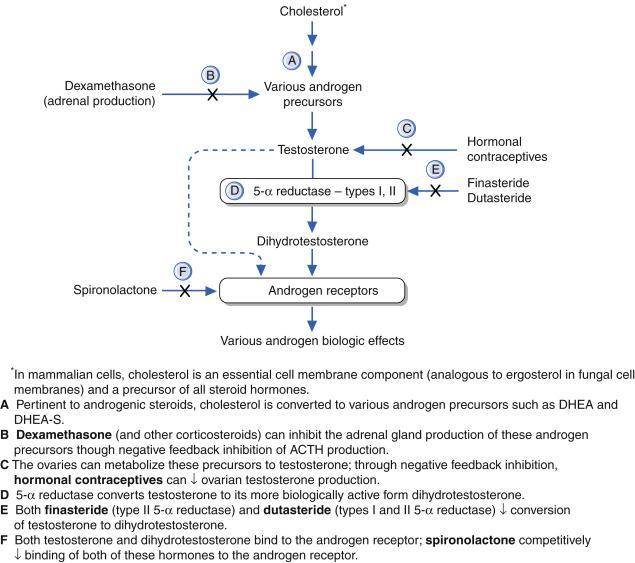
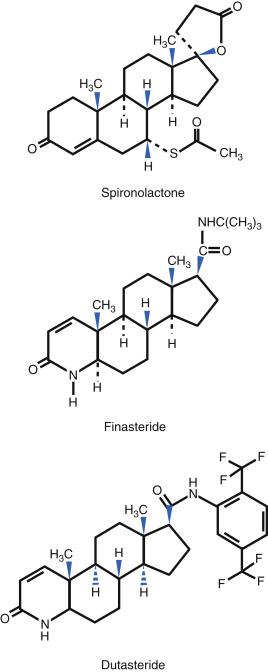
Therapeutically, two main categories of drugs affect androgens and their activity. Q34.1 The first are ‘antiandrogens’ which are agents that block the androgen receptor (AR) and include spironolactone, flutamide, and cyproterone acetate. The second are ‘androgen inhibitors,’ which block androgen synthesis, and include finasteride and dutasteride (these are specific 5-α reductase inhibitors, that inhibit formation of dihydrotestosterone [DHT]). This group also includes leuprolide and nafarelin, (which are gonadotropin-releasing hormone [GnRH] agonists, and work at the level of the ovary and pituitary). In this chapter ‘antiandrogens’ is the term used for specific AR blockers, and the term ‘androgen inhibitors’ will be used to distinguish those compounds that work by suppressing or inhibiting the formation of DHT. Other agents such as progestins and combined oral contraceptives (COC) are both antiandrogens and androgen inhibitors. The various drugs discussed in this chapter are categorized by their most important clinical mode of action ( Box 34.2 ).
Spironolactone
Progesterone
Cyproterone acetate
Cimetidine
Flutamide
Finasteride
Dutasteride
Ketoconazole
Combined oral contraceptives (see Table 34.5 )
Leuprolide
Nafareline
Herbal products (e.g. saw palmetto)
This chapter provides an overview of various antiandrogens (drugs that block the AR) and androgen inhibitors (enzyme inhibitors and other mechanisms). How these specific compounds work, and their approved and off-label indications, dosing, and AE, will be presented. Particular emphasis is given to spironolactone, finasteride, dutasteride, and oral contraceptives (OC).
Androgens affect biology at different stages of life. Virilization of the male urogenital tract occurs between 8 and 12 weeks of embryogenesis, and androgens are essential for the development of the male phenotype. Before puberty, testicular androgen secretion is minimal, and the adrenal cortex suppresses gonadotropin secretion. At puberty, gonadotropins become less sensitive to feedback inhibition. The testes enlarge and testicular Leydig cells produce testosterone. Thereafter, the penis and scrotum enlarge and pubic hair appears. The adrenal glands also produce small quantities of testosterone. Androgens have growth-promoting properties that cause an increase in height and the development of a masculine skeletal musculature. Androgens also modulate immune responses. Androgen and estrogen receptors are present on most immune competent cells and sex hormones are known to affect T-helper 1(Th1)/Th2 cell balance.
When androgen secretion increases at puberty, the skin becomes thicker and oilier (seborrhea). This occurs because of the interaction of androgens with AR on hair follicles and sebaceous glands. There may be enhanced follicular keratinization, proliferation of sebaceous glands and sebum secretion. Q34.2 Pilosebaceous units consequently can become prone to follicular plugging and bacterial colonization, which predisposes to acne vulgaris. Secondary sexual characteristics develop: growth of axillary, facial, and body hair, because of the conversion of vellus to terminal hairs, and voice changes occur because of growth of the larynx. Males who inherit the genes for AGA may show signs of frontal hairline recession and thinning over the vertex scalp later in puberty. The last growth spurt comes to an end in later puberty as the epiphyses of long bones close.
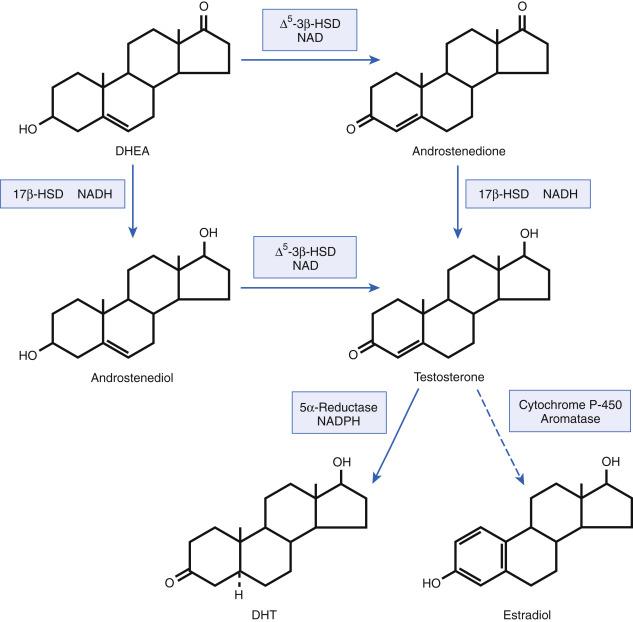
In women, androgens are derived from the ovaries, adrenal gland, and also from conversion of various steroids in the liver and peripheral tissues such as adipose tissue, skin and skin appendages. The circulating androgens include testosterone, dihydrotestosterone (DHT), androstenedione, dehydroepiandrosterone (DHEA) and its metabolite dehydroepiandrosterone sulfate (DHEA-S). Testosterone and androstenedione can both be metabolized to the more potent androgen DHT, by 5α-reduction in the liver and skin ( Fig. 34.1 ). The average daily rate of testosterone production in women is approximately 0.25 mg, with a quarter derived from the ovary, a quarter from the adrenal gland, and the remaining half from peripheral conversion of androstenedione. Androstenedione is produced equally from the ovary and the adrenal gland, while greater than 90% of DHEA/DHEA-S are secreted by the adrenal gland.
Fluctuations in plasma concentrations of testosterone and androstenedione occur during the menstrual cycle, and in women, testosterone levels range from 15 to 65 ng/dL (0.5–2.3 nM). Only about 1% to 2% of the total testosterone concentration is biologically active. It is only the free (unbound) steroid that is able to act on the AR. The remaining amount is bound to hepatic sex hormone-binding globulin (SHBG), and is unable to enter cells.
Testosterone has minimal biologic activity in many androgen-responsive tissues including the prostate and pilosebaceous unit until it is converted to the more potent androgen DHT by the enzyme 5-α reductase in local tissues. Q34.3 There are two isoenzyme forms of 5-α reductase: type I and type II. The biochemical characteristics and distributions of these two isoenzyme forms vary, as shown in Table 34.1 . Both enzymes are located in the pilosebaceous unit, but differ quantitatively depending on the location. Both testosterone and DHT exert their biological effects by binding to the intracellular AR, which is a member of the steroid and thyroid hormone receptor superfamily. This hormone–receptor complex subsequently binds to specific nuclear hormone regulatory elements in deoxyribonucleic acid (DNA) and acts to increase or reduce the synthesis of specific messenger ribonucleic acid (mRNA) and resultant proteins. AR are present on cells in many organ systems: striated muscle (leading to a muscular habitus), cardiovascular and endocrine systems, the liver and the skin. In the liver androgens can inhibit hepatic SHBG production and in skin, DHT can increase 5-α reductase levels and AR levels. The net result of androgen action in the liver and skin is a positive feedback loop with further augmentation of androgenic activity.
| Characteristic | Type I | Type II |
|---|---|---|
| Molecular weight | 29.5 kDa | 28.4 kDa |
| Number of amino acids | 259 | 254 |
| Optimum pH | Basic (8.0) | Acidic (6.0) |
| Michaelis–Menton constant | K m (μM) 24 | K m (μM) 0.3 |
| Chromosome location of gene | 5 | 2 |
| Sites most commonly present | Skin, liver, adrenal, kidney | Skin, prostate, epididymis, seminal vesicles, liver |
| Most common skin locations | Predominantly nongenital skin, including scalp. In the skin it is localized to sebaceous glands especially from face and scalp and in the dermal papilla. | Follicles on top of scalp, frontal to vertex. Absent from occipital scalp and axillary dermal papillae but is strongly present in beard dermal papilla. |
Q34.2 In women, dermatologic androgen excess disorders include acne, female-patterned hair loss (FPHL, also known as AGA), and hirsutism (see Box 34.1 ). Hidradenitis suppurativa is also described as an androgen-dependent condition, although the role of androgens is not fully delineated. These disorders may result from systemic hyperandrogenemia because of androgen overproduction in the ovary or adrenal gland, or from cutaneous hyperandrogenism. Cutaneous hyperandrogenism may be attributed to altered 5-α reductase levels, AR levels, aromatase levels or other local enzyme-level abnormalities at the pilosebaceous unit such as 3β-hydroxysteroid dehydrogenase (3β-HSD1) or 17β-hydroxysteroid dehydrogenase (17β-HSD3). Aromatase converts testosterone to estradiol and diverts androstenedione metabolism away from the production of testosterone to form estrone in the adipose tissue. 3β-HSD1, 17β-HSD3, and 5-α reductase are major steroidogenic enzymes present in the skin and its appendages, and are responsible for the formation of potent androgens locally in specific tissues (see Fig. 34.1 ). In women with CHA, underlying disorders must be considered, such as polycystic ovary syndrome (PCOS), other endocrine disorders, and tumors among other causes. Testing testosterone (total, free) and DHEA-S levels is of clinical value in select patients. Although measurable circulating hormone levels are normal in most women with acne and AGA, the etiology is likely the result of abnormalities in local androgen metabolism at the tissue level rather than the result of increased secretion of circulating androgens. Patients with hirsutism are more likely to have serum androgen level abnormalities. Further discussion of testing and the hyperandrogenemic disorders is beyond the scope of this chapter.
Antiandrogens and androgen inhibitors can block or reverse the biologic effects of androgens at the cutaneous level ( Table 34.2 ). Table 34.3 lists key pharmacologic concepts for antiandrogens and androgen inhibitors, and Fig. 34.2 illustrates antiandrogen mechanisms of action.
| Generic Name | Trade Name | Generic Available | Manufacturer | Tablet/Capsule Sizes | Special Formulations | Standard Dosage Range |
|---|---|---|---|---|---|---|
| Antiandrogens | ||||||
| Spironolactone | AldactoneCarSpir | Yes | PfizerCMP Pharma | 25, 50, 100 mg | 25 mg/5 mL suspension a | 50–100 mg/day (BID dosing) |
| Medroxyprogesterone acetate | Many (see Table 34.5 ) | Yes | Various | 2.5, 5, 10 mg | Injectable, topical gels | Not established |
| Cimetidine | Tagamet | Yes/OTC | Prestige Health | 200, 300, 400, 800 mg | Oral solution | 400 mg BID–QID |
| Androgen Inhibitors | ||||||
| Finasteride | Propecia Proscar |
Yes | Merck | 1 mg 5 mg |
None | 1 mg QD (for AGA) |
| Dutasteride | Avodart | Yes | GlaxoSmithKline | 0.5 mg | None | 0.5 mg QD |
| Ketoconazole | Nizoral | Yes | Mylan, Taro | 200 mg | Yes | 200–400 mg/day |
| Drug Name | Absorption | Bioavailability | Elimination | |||
|---|---|---|---|---|---|---|
| Peak Levels | Half-Life | Percentage Bioavailable (%) | Protein Binding (%) | Metabolism | Excretion | |
| Antiandrogens | ||||||
| Spironolactone | 2–4 hours | 10–35 hours a | >90 | 98 a | Canrenone is the active metabolite | Urine and hepatobiliary routes |
| Medroxyprogesterone acetate | 1–2 hours | 8–9 hours | Varies | Varies | Prompt hepatic degradation | Especially renal, also hepatobiliary |
| Cimetidine | 0.75–1.5 hours | 2 hours | 60–70 | 13–25 | 30%–40% of drug metabolized by liver | Predominantly renal |
| Androgen Inhibitors | ||||||
| Finasteride | 1–2 hours | 5–6 hours | 64 | 90 | Extensive liver metabolism to inactive metabolites | 39% in urine, 57% in feces |
| Dutasteride | 2–3 hours | 5 weeks | 60 | 90 | Hepatic metabolism | Feces, urine |
| Ketoconazole | 1–2 hours | 8 hours | Uncertain b | 95–99 | Extensive liver metabolism to inactive metabolites | 85%–90% in feces, 10%–15% in urine |
a These values are for canrenone, the active metabolite of spironolactone.
b Bioavailability highly variable and is highly dependent on an acid pH in the gastrointestinal tract.
Q34.4 Spironolactone (see Table 34.2 ) is an aldosterone antagonist (antimineralocorticoid) and a relatively weak antiandrogen that blocks the AR, thereby competitively inhibiting DHT activity at the receptor level (see Fig. 34.2 ) It is not purely an antiandrogen and has been shown to inhibit androgen biosynthesis. For example, it may be converted to other active metabolites via progesterone 17-hydroxylase, and these metabolites reversibly inhibit adrenal and ovarian cytochrome P-450 (CYP) enzymes, resulting in a net decrease in testosterone and DHT production. Spironolactone has also been shown to have some inhibitory effect on 5-α reductase activity. Spironolactone has variable progestational activity. The drug influences the ratio of luteinizing hormone (LH) to follicle-stimulating hormone (FSH) by reducing the response of LH to GnRH.
Spironolactone is a steroid molecule containing the basic steroid nucleus of four rings ( Fig. 34.3 ). It resembles the mineralocorticoids, possessing an esterified lactone ring. Bioavailability from oral administration is at least 90%, but varies depending on the manufacturer. Q34.4 Spironolactone is 98% protein bound, and the primary metabolite, canrenone, is at least 90% protein bound. Canrenone is the active aldosterone antagonist and is the primary metabolite contributing to the diuretic and antiandrogen activities of spironolactone (see Table 34.3 ).
Food increases the absorption of spironolactone. The liver rapidly metabolizes spironolactone. The primary metabolite, canrenone, can be interconverted enzymatically to its hydrolytic product, canrenoate. The unmetabolized drug does not appear in the urine. Metabolites of spironolactone are excreted in urine and bile.
A linear relationship between a single dose of spironolactone and plasma levels of canrenone occurs within 96 hours when administered in a dose range of 25 to 200 mg. The half-life is approximately 19.2 hours for canrenone; for spironolactone it is 12.5 hours.
Box 34.3 lists indications for spironolactone.
Spironolactone is US Food and Drug Administration (FDA)-approved as a diuretic to treat a variety of medical conditions. It is used off-label to treat hirsutism, acne, and AGA. There are no FDA-approved dermatologic indications.
In hirsute women, spironolactone has demonstrable superiority over placebo and gradually reduces the growth rate and mean diameter of facial hair. It is not recommended as initial therapy for hirsutism unless combined with a combined oral contraceptive (COC), because of its teratogenic potential, unless the woman is not sexually active, has undergone permanent sterilization, or is on a long-acting reversible contraceptive. The effects of spironolactone on hirsutism are known to be dose-dependent, although rigorous dose–response trials are lacking.
Spironolactone has been used off-label for FPHL for roughly 40 years and available studies have shown that it can stabilize hair loss and induce scalp hair growth in some women. Optimal dose–response studies are lacking; however, a daily dose of 200 mg may be required.
Spironolactone has been used since the 1980s to treat acne in women and has endorsement for this by consensus and expert groups. However, the actual statistical evidence supporting its use comes from low quality randomized controlled trials (RCT) and case series.
Based on anecdotal evidence and limited studies, spironolactone may improve and control mild to moderate hidradenitis suppurativa.
Common dosing of spironolactone for dermatologic indications is between 50 and 200 mg daily, with 100 mg daily typically being better tolerated than higher dosages. Delivery may be divided into twice daily dosing. Doses start at 25 to 50 mg and are slowly titrated up as tolerated. At higher doses, and even at a 100 mg dose, menorrhagia or other menstrual dysfunction is common. Q34.5 These menstrual problems may resolve after 2 to 3 months of therapy. If menstrual abnormalities do not improve with time, the options include :
Reducing the spironolactone dose to 50 to 75 mg daily;
Adding an OC to reduce the menstrual dysfunction; or
‘Cycling’ the spironolactone (as done with OC), giving spironolactone for 21 consecutive days, followed by 7 days off the drug.
Patients are usually given an OC in conjunction with spironolactone because of the risk for teratogenicity, specifically the feminization of the developing male fetal genitalia during gestation.
Topical 5% spironolactone gel, lotion and cream have been used in Europe to treat grade II acne, but data for efficacy are limited. Compounded formulations have also been used anecdotally for FPHL and hirsutism. Allergic contact dermatitis has been reported to topical spironolactone. There has been no active research and development of this topical formulation in recent years.
Box 34.4 lists warnings, precautions, contraindications, and pregnancy prescribing status for spironolactone.
| Contraindications | |
|
|
| Boxed Warnings | |
|
|
| Warnings & Precautions a | |
Hyperkalemia and Related
|
Cardiovascular
Miscellaneous |
| Pregnancy Prescribing Status | |
|
|
a Under “Warnings & Precautions” these adverse effects can be considered relatively high risk or important clinical scenarios to avoid.
b See Chapter 65 Dermatologic Drugs During Pregnancy and Lactation, for detailed explanations of terms for “Newer rating” based on 2015 US Food and Drug Administration rulings.
This potentially serious adverse effect (AE) is most likely to occur when spironolactone is given to patients with severe renal insufficiency, or when the drug is taken in combination with other potassium-sparing medications (see Drug Interactions later). Spironolactone is contraindicated for patients with severe renal insufficiency, hyperkalemia, and those with aldosterone deficient conditions (e.g., Addison disease). Other important electrolyte abnormalities may occur in patients with CHF, renal insufficiency or liver cirrhosis ( Table 34.4 ).
| Drug Category | Drug Examples | Comments |
|---|---|---|
| Relatively High-Risk Drug Interactions ∗ | ||
| Inotropic agents | Digoxin | Spironolactone may ↑ digoxin levels and associated risks |
| Psychotropic agents | Lithium carbonate | Spironolactone may ↑ lithium levels and associated risks |
| Antihypertensives, other uses | ACE inhibitors | Concomitant use with spironolactone may augment the hyperkalemic potential of drug/drugs; conceptually higher/highest risk for ACE inhibitors and 6 categories below in older patients with CV and/or renal disease |
| Antihypertensives, other uses | Angiotensin II receptor blockers | same |
| Aldosterone antagonists | Eplerenone, amiloride | same |
| Anticoagulants | Heparin, low molecular weight heparin | same |
| Direct renin antagonist | Aliskiren | same |
| Hormonal contraceptives | Drospirenone (Yaz, others) | same |
| Calcineurin inhibitors | Cyclosporine, tacrolimus (oral) | same |
| Lower-Risk Drug Interactions | ||
| Nutritional | High potassium foods | Such as bananas, oranges, tomatoes, others in high amounts; less risk than above drugs |
| Supplements | Potassium salts | Increase hyperkalemic potential of spironolactone |
∗ Overall highest-risk drug interactions designated as bold italics font.
Q34.6 The potential for spironolactone to induce estrogen-dependent malignancies has been long debated. Many authors suggest caution in prescribing spironolactone for women with a personal or family history of breast cancer and other estrogen-dependent malignancies; however, proof of causality in such malignancies is lacking. The FDA package insert warns that tumors were found in chronic toxicity studies of rats, in which 25 to 250 times the usual human dose (on a body weight basis) was administered. These doses resulted in benign adenomas of the thyroid and testes, malignant mammary tumors, and proliferative changes in the liver. Because of these and other changes reported in the rat, it has been recommended to withhold giving spironolactone to women with a genetic predisposition for breast cancer.
This rare but serious AE is of greater concern in patients of advanced age and with hepatic or renal impairment. Drug dosage and duration of use as well as concurrent medications are additional risk factors that may predispose patients taking spironolactone to agranulocytosis.
Other important AE include hypotension and worsening renal function, gynecomastia (usually, but not always reversible), and minor gastrointestinal symptoms. Rarely gastric ulceration and bleeding, and mixed cholestatic/hepatocellular toxicity have been reported. Previous data reported that spironolactone does not alter serum uric acid levels; however, a recent report showed that in patients with chronic kidney disease, low dose spironolactone can cause hyperuricemia and gout.
Spironolactone and its metabolites can cross the placental barrier. Studies in rats demonstrate feminization of the male rat fetus during gestation. Limited reports in humans have not shown adverse pregnancy outcomes. Although FDA labeled as a pregnancy category C drug, because of the potential risk based on animal studies and the antiandrogenic properties of spironolactone, it should be avoided in pregnant women and women should be advised of the potential risk to a male fetus. (see Box 34.4 ) The spironolactone metabolite canrenone has been detected in breast milk of nursing women.
Q34.7 Drugs that increase the risk of hyperkalemia and/or other electrolyte abnormalities, such as angiotensin-converting enzyme (ACE) inhibitors, aliskiren (a direct renin inhibitor), angiotensin-II receptor blockers, and other aldosterone inhibitors (eplerenone), as well as heparin and low molecular weight heparin, trimethoprim, nonsteroidal anti-inflammatory drugs (NSAID) such as indomethacin, and selective serotonin reuptake inhibitors (SSRI) should be avoided. Drospirenone containing OC should be avoided because of additive antimineralocorticoid activity. Patients should be cautioned about excessive dietary intake of potassium-rich foods. Spironolactone may increase levels of lithium and digoxin leading to toxicity.
If abnormal at baseline, laboratory monitoring of circulating androgens (testosterone or DHEA-S) every 3 to 4 months is recommended to verify androgen suppression. Complete suppression usually takes 4 to 12 months of therapy and plateaus after 1 year. It may be necessary to add either an adjunctive antiandrogen or an androgen inhibitor. Assessment of a metabolic panel with renal function, sodium and potassium level is reasonable in select patients (see later).
It has long been thought necessary to monitor serum potassium levels periodically, especially at baseline and after the first month of therapy, or with any dose increase. However, a recent multicenter study in 974 women found mild hyperkalemia at a rate of 0.72% in women taking 50 to 200 mg of spironolactone daily versus baseline rate of 0.76% derived from all available serum potassium measurements for females of the same age (no difference in frequency of hyperkalemia among users vs. nonusers). This study along with a recent systematic review, concluded that routine monitoring of serum potassium in healthy women taking spironolactone for acne is unnecessary. Hyperkalemia from spironolactone is uncommon in the absence of the aforementioned risk factors for this complication. Testing may be justified on an individual basis (1) when risk factors are present, (2) in patients vomiting excessively, or (3) in individuals with unusual diets. Patients should be advised to report new onset of muscle cramps or weakness, muscle fatigue, lethargy, drowsiness, paresthesia, or cardiac irregularities, which may clinically indicate fluid or electrolyte imbalance. Blood pressure and weight should also be monitored periodically.
See Tables 34.2 and 34.3 for general information and key pharmacologic concepts of progestins. Progestogens, include both endogenous progesterone secreted by the ovary, and synthetic steroids (progestins). Progestins suppress ovulation through their antigonadotrophic activity and further exert contraceptive function by altering the quality of cervical mucus, inducing endometrial changes and altering Fallopian tube motility. Progestins are biologically active through their interaction with the progesterone receptor (PR). All progestins bind to the PR, with varying affinity. Depending upon their chemical structure, progestins also interact with other steroid hormone receptors, including the androgen, estrogen, mineralocorticoid, and glucocorticoid (corticosteroid) receptors and may act as agonists or antagonists. Knowledge of these interactions is important to understanding the biological activity and AE of the various progestins.
Progesterone and testosterone share basic structural similarity possessing the same steroid A, B, C, D rings. Because of this structural similarity, progestins can bind to the AR and either block it or activate it. The different progestins vary in activity from androgenic to antiandrogenic to mildly antiandrogenic or neutral. Synthetic progestins are classified according to three tetracyclic structures: estranes and gonanes (both testosterone derivatives), and pregnanes or 19-norpregnanes (derived from progesterone). Drosperinone (DRSP), unlike the other progestins, is a 17α-spironolactone derivative ( Table 34.5 ). The estranes correspond to first-generation progestogens and include norethisterone, norethindrone, and ethynodiol diacetate. Also, included here is dienogest, which shares the 19-nortestosterone structure but lacks the ethynyl structure shared by this group and is cyanomethylated. Gonanes correspond to both second-generation levonorgestrel and norgestrel and third-generation desogestrel, gestodene (not available in the United States) and norgestimate. In general, the testosterone-derived progestins are androgenic (with the exception of dienogest) and later generations are generally less androgenic than earlier generations, although biological activity is difficult to predict from chemical structure alone. The progesterone-derived pregnanes (medroxyprogesterone acetate, cyproterone acetate [CypA], chlormadinone acetate) and 19-norpregnanes (a newer group that includes nomegestrol acetate, trimegestone, and segesterone acetate [Nestorone]) have no androgenic activity with the exception of medroxyprogesterone acetate, which is mildly androgenic. The newer 19-norpregnane derivatives have greater PR specificity and negligible androgenic, estrogenic, glucocorticoid, and mineralocorticoid activity, thereby more closely mimicking endogenous progesterone.
| Moderate to High Androgenicity | Norethindrone | Norethindrone Acetate | Ethynodiol Diacetate | Levonorgestrel | Norgestrel |
|---|---|---|---|---|---|
| Brevicon (Jolivette) Necon (Nora BE) Norinyl (Nor-QD) Ovcon Tri-Norinyl |
Activelle Aygestin Combipath (2) Estrostep (7) Femhrt Loestrin Microgestin |
Demulen Zovia |
Alesse-28 Climara Pro (2) Levlen Levora Mirena (3) Next Choice (4) Plan B (4) Preven EC (4) Seasonale (5) Tri-Levlen Triphasil Trivora |
Lo Ovral Low-Orgestrel Ogestrel Ovral Ovrette |
|
| Low Androgenicity | Norgestimate | Norelgestromin a | Desogestrel | Etonogestrel a | Gestodene b |
| Mono Nessa Ortho-Cyclen Ortho Tri-Cyclen (7) Ortho-Cyclen Tri Nessa |
Ortho-Evra (2) | Cyclessa Desogen Kariva Mircette Ortho-Cept Velivet |
Impalon (8) Nuvaring (1) |
||
| Mildly Androgenic | Medroxyprogesterone Acetate | ||||
| Depo-Provera (6) Premphase Prempro |
|||||
| Non-Androgenic/Neutral and Mildly Antiandrogenic | Progesterone | Trimegestone c | Nestorone g | Nomogestrol Acetate d | |
| Crinone gelPrometrium suppository | Annovera (9) | ||||
| Antiandrogenic Progestins | Drosperinone | Dienogest | Cyproterone Acetate e | Chlormadinone Acetate | |
| Beyaz (7) Gianvi Ocella Slynd [10] Yasmin Yaz (7) Zarah (Slynd)10 |
Natazia f Qlaira f |
Vaginal ring
Transdermal products
Intrauterine device
Postcoital emergency contraception
Contraceptive with four menstrual cycles per year
Injections
US Food and Drug Administration-approved for treatment of acne vulgaris
Implantable device
Long-acting vaginal system; continuous daily 0.15 mg/day Nestorone + 0.013 mg ethinyl estradiol
New progesterone-only pill containing DRSP 4 mg daily
a Etonogestrel is a metabolite of desogestrel (3-keto-desogestrel); norelgestromin is a metabolite of norgestimate.
b Gestodene is used for contraception in other countries. Not approved for use in the US.
c Trimegestone is not available for contraception. Sold under brand name Ondeva in Latin America and Europe for non-contraceptive uses.
d Available in Europe: Zoely 2.5 mg/1.5 mg nomegestrol acetate/estradiol.
e Available in Canada as Diane or Diane-35.
f Combined oral contraceptive containing estradiol valerate.
g Nestorone also known as segesterone acetate; recently approved for contraception in US; also in clinical trials for male contraception.
Q34.8 CypA is the progestin with the most potent antiandrogen properties. The drug has long been used in Europe and Canada as the progestin in a COC named Diane or Dianette. This progestin is not available in the United States. Potent antiandrogenic effects are exerted by competition of cyproterone with DHT for the AR-binding site. The drug also has strong progestational activity thereby suppressing gonadotropin secretion and testosterone production. When given to pregnant animals, CypA blocks the actions of androgens in the male fetus and induces a form of pseudohermaphroditism. In Canada, Diane (2 mg CypA/0.035 mg ethinyl estradiol [EE]) is approved by Health Canada for the treatment of androgen-sensitive skin conditions. Off-label uses include AGA, hirsutism, and virilizing syndromes. Although it provides effective birth control, it does not have official approval for this indication.
Q34.8 Dienogest (a 19-nortestosterone derivative) and drosperinone (a spironolactone derivative), both possess antiandrogenic activity equivalent to roughly 30% to 40% of the potency of cyproterone acetate. Drosperinone also has antimineralocorticoid activity (3-mg dose of DRSP is comparable with a 25-mg dose of spironolactone). Chlormadinone acetate (available in Europe) also has moderate antiandrogenic activity. The newer 19-norprogesterone derivatives nomogestrol acetate and trimegestone show mild antiandrogenic activity similar to that of endogenous progesterone.
Progesterone is readily absorbed intramuscularly and orally, but at a rate that may be too rapid for optimal therapeutic efficacy. Biotransformation takes place largely in the liver. Many progestins are conjugated by glucuronidation or sulfonation to more hydrophilic metabolites for excretion in the urine. A small amount can be stored in body fat. Multiple analogs of progesterone are less susceptible to hepatic metabolism, and therefore may have a more sustained therapeutic effect compared with progesterone. Approximately 50% to 60% of administered radioactive progesterone appears in the urine and 10% in feces.
Oral systems include progestin-only pills (POP or mini-pills) and COC – progestin in combination with an estrogen (see Table 34.5 ). Norethindrone acetate, norethindrone, and norgestrel are available as POP. A new drosperinone-only pill (4 mg of DRSP daily for 24 days followed by a placebo for 4 days) was approved June 2019 by the FDA. Several controlled-release drug delivery formulations also exist including long-acting reversible contraceptives like subdermal contraceptive implants and intrauterine devices (IUD), which use levonorgestrel or etonogestrel released in small quantities. These last for several years but can be removed at any time. A common oral formulation used clinically is medroxyprogesterone acetate (Provera). It can also be given as an intramuscular injection once every 3 months for long-acting contraception (Depo-Provera) (see Tables 34.2 and 34.3 ).
Common therapeutic indications for progesterone are for ovarian disorders, post-menopausal disorders, and contraception. Current POP are ineffective for disorders of androgen excess such as hirsutism with the possible exception of the newly approved DRSP-only pill. Because most current progestin-only contraceptives do not contain antiandrogenic progestins, they may in fact play a role in the development of acne, although a causal relationship has been difficult to establish. Acne has been cited as an AE leading to termination of levonorgestrel-releasing IUD. However, levonorgestrel in a COC has been shown to reduce acne counts, and this is largely attributed to the estrogen component of the pill. (See section on Oral Contraceptives.) Compounded topical progesterone at 2% to 5% concentrations has been used off-label for treating FPHL, with variable effectiveness.
Because most progestins recommended by dermatologists are used in conjunction with an estrogen in a COC, further indications and AE are discussed in the section on Oral Contraceptives ( Box 34.5 ). Q34.7 Note that COC and POP containing drospirenone share similar contraindications to spironolactone. Specifically, the drug should not be used in patients with conditions that predispose to hyperkalemia (i.e., renal insufficiency, hepatic dysfunction, and adrenal insufficiency), or in women who are receiving chronic treatment with medications that may increase serum potassium levels. In addition, all patients receiving COC must be appropriately selected and counseled regarding risk for venous thromboembolism (VTE). This is further discussed in the section Oral Contraceptives.
| Contraindications | |
|
|
| Boxed Warnings | |
|
|
| Warnings & Precautions a | |
Malignancies
Gastrointestinal Cardiovascular
Psychiatric
|
Thromboembolic Disease
Metabolic
Miscellaneous
|
| Pregnancy Prescribing Status | |
|
|
a Under “Warnings & Precautions” these adverse effects can be considered relatively high risk or important clinical scenarios to avoid.
b See Chapter 65 Dermatologic Drugs During Pregnancy and Lactation, for detailed explanations of terms for “Newer rating” based on 2015 US Food and Drug Administration rulings.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here