Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The bones of the pelvis are the rigid foundation to which all the pelvic structures are ultimately anchored. In the standing position, forces are dispersed to minimize pressures on the pelvic viscera and musculature and to transmit forces to bones that are better suited to the long-term, cumulative stress of daily life. In the upright position, the pubic rami are oriented in an almost vertical plane. Similar to the supports of an archway or bridge, the body weight is transmitted along these bony supports to the femurs. Where the pubic rami articulate in the midline, they are nearly horizontal. Much of the weight of the abdominal and pelvic viscera is inferiorly supported by the bony articulation.
The pelvic bones are the ilium, ischium, pubic rami, sacrum, and coccyx ( Fig. 1.1 A and B). The sacrum is composed of five sacral vertebrae that are fused together. The nerve foramina are positioned anterior and laterally. Overlying the middle of the sacrum is a rich neurovascular bed. The coccyx is inferiorly attached and is the posterior border of the pelvic outlet.
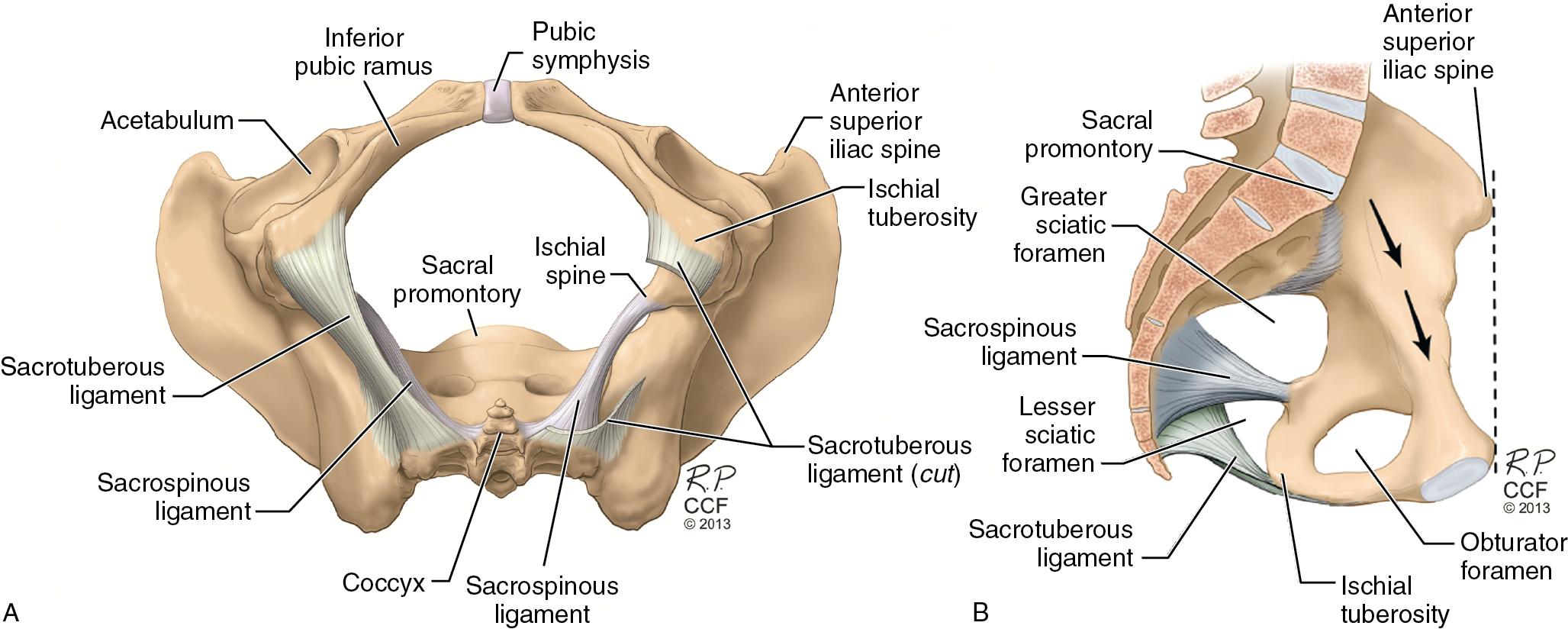
Several landmarks are important to the pelvic surgeon. The anterior superior iliac spine (ASIS) is easily identifiable and is anterior and laterally located on the superior ileum. The ischium is fused to the ilium. The medial surface of the ilium forms the lateral borders of the pelvic outlet. The superior greater sciatic notch and inferior lesser sciatic notch are medially separated by a projection, the ischial spine. The sacrospinous ligament, which is triangular in form, is laterally attached by its apex to the ischial spine; its broader base arises from the side of the lower sacral and coccygeal segments. This ligament converts the greater sciatic notch into the greater sciatic foramen (see Fig. 1.1 B). Through this foramen pass the piriformis muscle and all of the vessels and nerves that leave the pelvis for the gluteal region and back of the thigh. The sacrospinous ligament and the dorsal sacrotuberous ligament also convert the lesser sciatic notch to the lesser sciatic foramen. Through this foramen pass the tendon and nerve of the internal obturator muscle, the pudendal nerve, and the internal pudendal vessels.
The ischial spine can be palpated easily through a vaginal, rectal, or retropubic approach, and many supportive structures attach to it. The ischial spine is useful as a fixed point to describe the relative position of other anatomic structures and as a landmark in various reconstructive surgeries for pelvic organ prolapse. The superior and inferior pubic rami are anteriorly located and articulate in the midline at the pubic symphysis. The ridge along the superior, medial surface of the superior pubic rami is called the iliopectineal line, or Cooper’s ligament.
In the standing position, the ASIS and pubic symphysis are in the same vertical plane (see Fig. 1.1 B). This directs the pressure of the intraabdominal and pelvic contents toward the bones of the pelvis instead of the muscles and endopelvic fascia attachments of the pelvic floor. The posterior surface of the pubic symphysis is located in a plane approximately 2 to 3 cm inferior to the ischial spine. Therefore, a line drawn connecting the two structures would be almost horizontal in the standing position. This has important implications for the support of pelvic organs, and will be discussed later in the chapter.
The obturator internus and piriformis make up the pelvic sidewalls ( Fig. 1.2 ). The obturator membrane is a fibrous membrane that covers the obturator foramen. The obturator internus muscle lies on the superior (intrapelvic) side of the obturator membrane. The obturator internus origin is on the inferior margin of the superior pubic ramus and the pelvic surface of the obturator membrane. Its tendon passes through the lesser sciatic foramen to insert onto the greater trochanter of the femur to laterally rotate the thigh. The obturator internus receives its innervation from the obturator nerve originating from L5 to S2. The obturator vessels and nerve pass through the anterior and lateral border of the obturator membrane, in the obturator canal, to their destination in the adductor compartment of the leg.
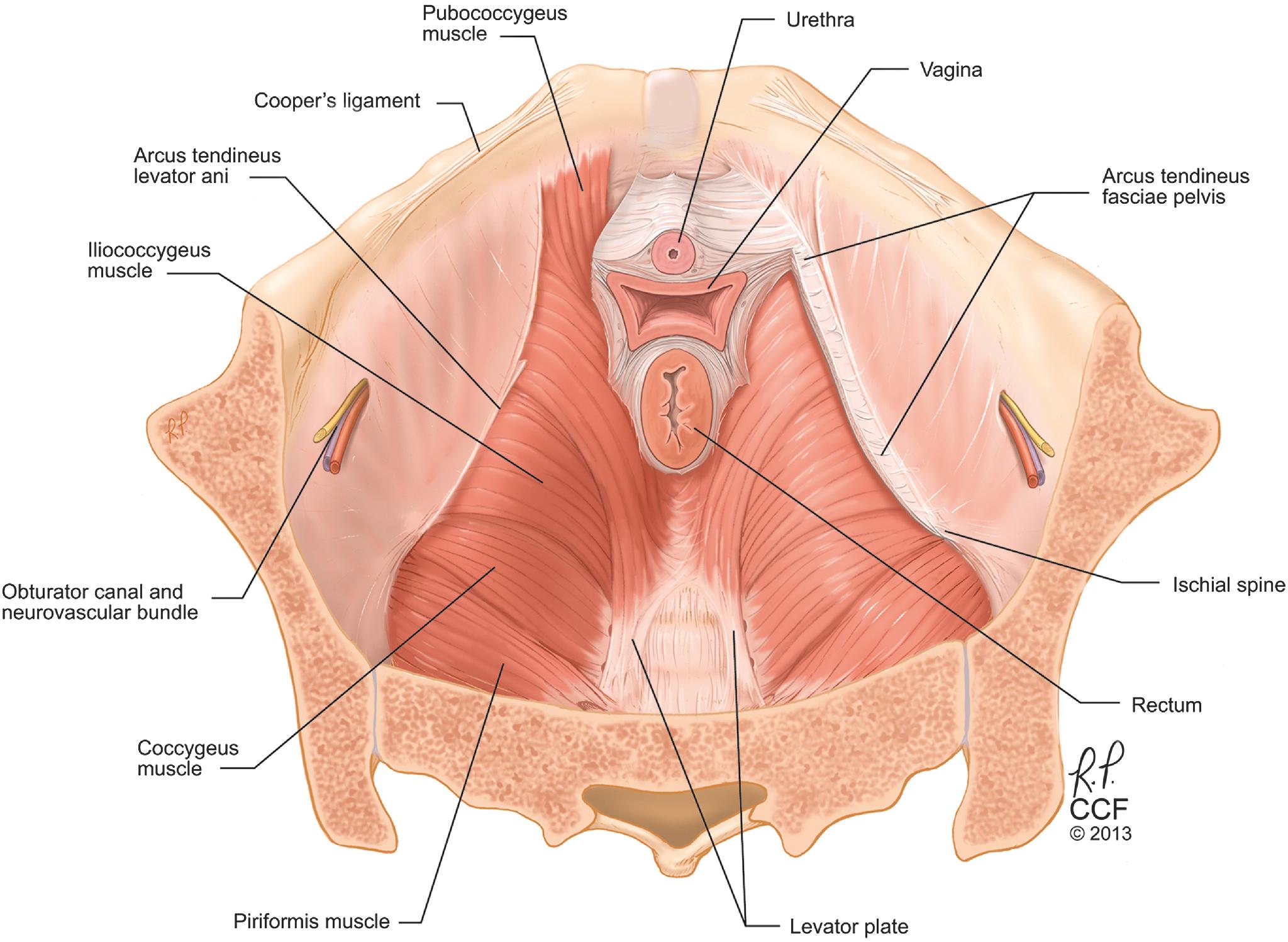
The piriformis is part of the pelvic sidewall and is located dorsal and lateral to the coccygeus. It extends from the anterolateral sacrum to pass through the greater sciatic foramen and insert onto the greater trochanter. Lying on top of the piriformis is a particularly large neurovascular plexus, the lumbosacral plexus.
There is a linear thickening of the fascial covering of the obturator internus muscle called the arcus tendineus levator ani. This thickened fascia forms an identifiable line from the ischial spine to the posterior surface of the ipsilateral superior pubic ramus. The muscles of the levator ani originate from this musculofascial attachment.
The pelvic diaphragm is defined as the levator ani muscles and the coccygeus muscle. It is stretched hammock-like between the pubis in front and the coccyx behind, and is attached along the lateral pelvic walls to the arcus tendineus levator ani. The puborectalis, pubococcygeus, and iliococcygeus are the three components of the levator ani muscle recognized by Terminologia Anatomica (see Fig. 1.2 ). The more medial puborectalis arises from the posterior inferior pubic rami and passes posteriorly, forming a sling around the vagina, rectum, and perineal body to form the anorectal angle and contribute to fecal continence. The pubococcygeus has a similar origin, but it inserts in the midline onto the anococcygeal raphe and the anterolateral borders of the coccyx. The pubococcygeous muscle further subdivides into fibers that blend with the muscularis of the vagina ( pubovaginalis m. ), perineal body ( puboperineal m. ), and anal sphincter muscle ( puboanalis m. ). Because of the significant attachments of the pubococcygeus to the walls of the pelvic viscera, the term “pubovisceral muscle” is frequently used to describe it, although this term is not officially recognized by Terminologia Anatomica . The iliococcygeus extends along the arcus tendineus levator ani from the pubis to the ischial spine to insert in the midline onto the anococcygeal raphe and coccyx.
The coccygeus, although not part of the levator ani, does make up the posterior part of the pelvic floor, and it plays a role in support. Its origin is on the ischial spine and sacrospinous ligament. It inserts on the lateral lower sacrum and coccyx, and it overlies the sacrospinous ligament. The muscle becomes thin and fibrous with age. The coccygeus often blends with the sacrospinous ligament, and it can be difficult to distinguish the two because they have the same origin and insertion.
The space between the levator ani musculature through which the urethra, vagina, and rectum pass is called the levator hiatus. The fusion of the levator ani where they meet in the midline creates the levator plate. The levator plate forms the basis for pelvic support. The levator ani may be very thin and attenuated, especially in elderly patients and those with pelvic organ prolapse.
With the change from plantigrade to erect posture, the human pelvis and vertebral column underwent various evolutionary changes that restored the balance between intraabdominal pressure and visceral support. The lumbosacral curve, a specific human characteristic, directs abdominal pressure forward onto the abdominal wall and the nearly horizontal, flattened pubic bones. Downward pressure is directed backward onto the sacrum and the rearranged pelvic muscles, which now fill in the pelvic cavity to form the pelvic floor and sidewalls.
The pelvic floor and sidewalls are made up of muscular and fascial structures that enclose the abdominopelvic cavity, the external vaginal opening (for intercourse and parturition), and the urethra and rectum (for elimination). The fascial components consist of two types of fascia: parietal and visceral (endopelvic). Parietal fascia covers the pelvic skeletal muscles and provides attachment of muscles to the bony pelvis; it is characterized histologically by regular arrangements of collagen. Visceral endopelvic fascia is less discrete and exists throughout the pelvis as a meshwork of loosely arranged collagen, elastin, and adipose tissue through which the blood vessels, lymphatics, and nerves travel to reach the pelvic organs, similar to the mesentery of the intestines. By surgical convention, condensations of the visceral endopelvic fascia of the pelvis have been described as discrete “ligaments,” such as the cardinal or uterosacral ligaments. The role of the endopelvic fascia in pelvic organ support will be discussed in detail later in this chapter.
The pelvic floor muscles have constant tone except during voiding and defecation, and they can be voluntarily contracted. This activity serves to close the urethral and anal sphincters, narrow the urogenital hiatus, and provide a constant support for the pelvic viscera. The levator muscles and the skeletal components of the urethral and anal sphincters all have the ability to contract quickly at the time of an acute stress, such as a cough or sneeze, to maintain continence. The muscles contain type I (slow-twitch) fibers to maintain constant tone and type II (fast-twitch) fibers to provide reflex and voluntary contractions.
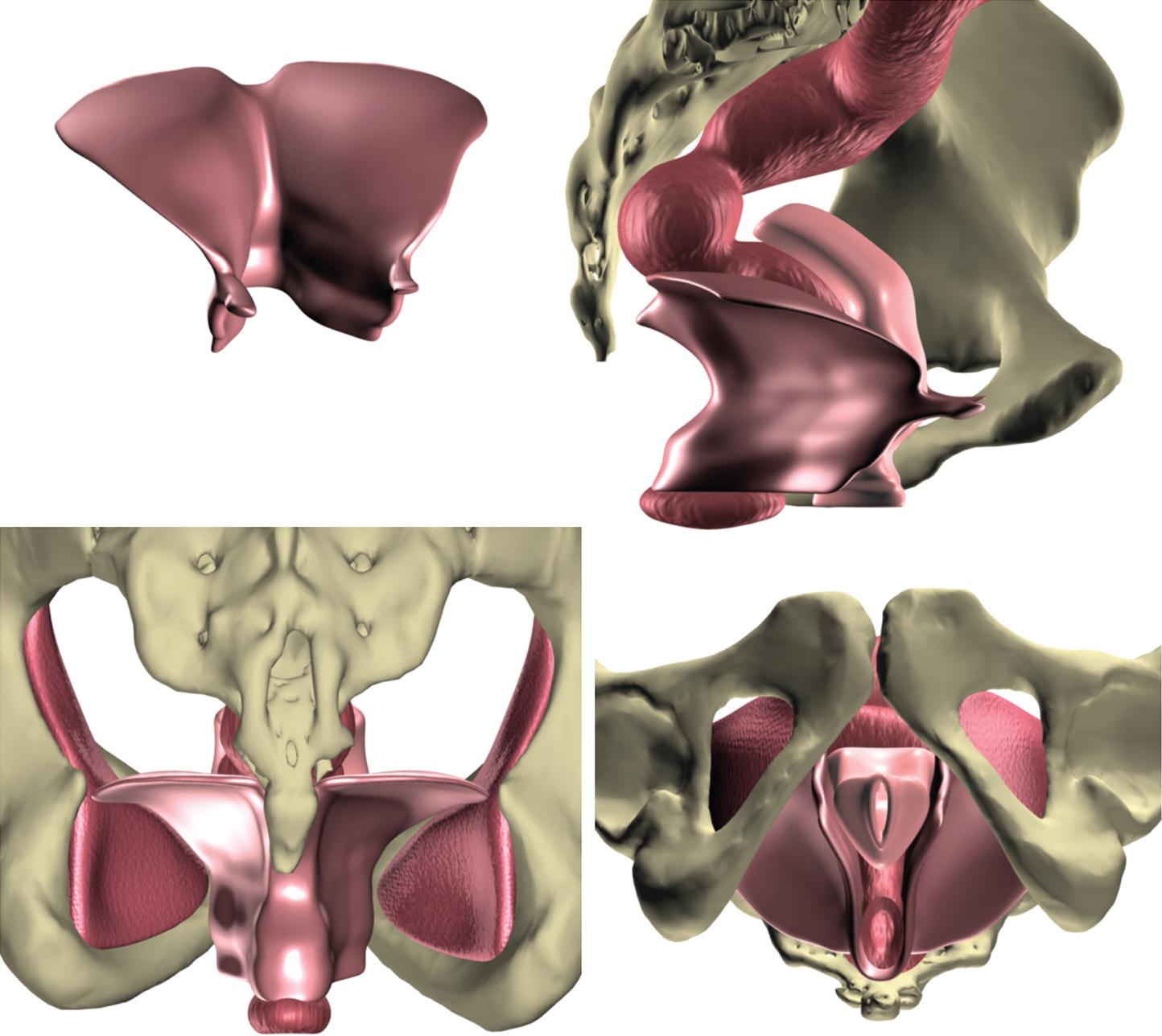
Although most anatomy and surgical texts depict the levator ani muscles as a bowl or as “funnel-shaped,” this reflects the uncontracted state of the muscles, as might be seen in a cadaver dissection, and not that of a normally functioning levator. In a woman with normal pelvic floor function, the levator ani muscle complex in its tonically contracted state has an intricate three-dimensional structure in which the anterior portion of the muscle complex (pubococcygeus and puborectalis muscles) is oriented vertically as a sling around the midurethra, vagina, and anorectum, and the posterior portion (iliococcygeus muscle) has a horizontal, upwardly biconvex shape with a “butterfly wing” appearance ( Fig. 1.3 ). Thus, the anterior portion of the levator ani complex serves to close the urogenital hiatus and pull the urethra, vagina, perineum, and anorectum toward the pubic bone, while the horizontally oriented posterior portion (levator plate) serves as a supportive diaphragm or “backstop” behind the pelvic viscera. Loss of normal levator ani tone, through denervation or direct muscle trauma, results in a more open urogenital hiatus, loss of the horizontal orientation of the levator plate, and a more bowl-like configuration. These changes can be bilateral or asymmetric. Such configurations are seen more often in women with pelvic organ prolapse than in women with normal pelvic organ support.
The sacral plexus is formed by the nerve roots of L4, L5, and S1 to S4 and is located on the anterior surface of the piriformis muscle on the lateral pelvic floor and sidewalls. The sacral plexus gives rise to multiple nerve branches, including the sciatic nerve, the superior gluteal nerve, the pudendal nerve, and the nerve to the levator ani. The pudendal nerve innervates the striated urethral and anal sphincters as well as the deep and superficial perineal muscles and provides sensory innervation to the external genitalia. Although there is variability in the branching patterns of the pudendal nerve, it consistently originates from the S2 to S4 (with S3 providing the largest contribution) sacral nerve trunks. Together, the pudendal vessels and nerve follow a complex course as they leave the pelvis. With the nerve oriented medially and the vessels laterally, the pudendal neurovascular bundle travels behind the sacrospinous ligament at the ischial spine, exiting the pelvis through the greater sciatic foramen ( Fig. 1.4 ). It then enters the ischioanal fossa through the lesser sciatic foramen and travels through the pudendal canal (Alcock’s canal) on the medial aspect of the obturator internus muscles before emerging in the perineum, where the bundle separates into several branches that terminate within the muscles and skin of the perineum and the clitoris. The neuroanatomy of the perineum, including the pudendal nerve branches, are described later in the chapter.
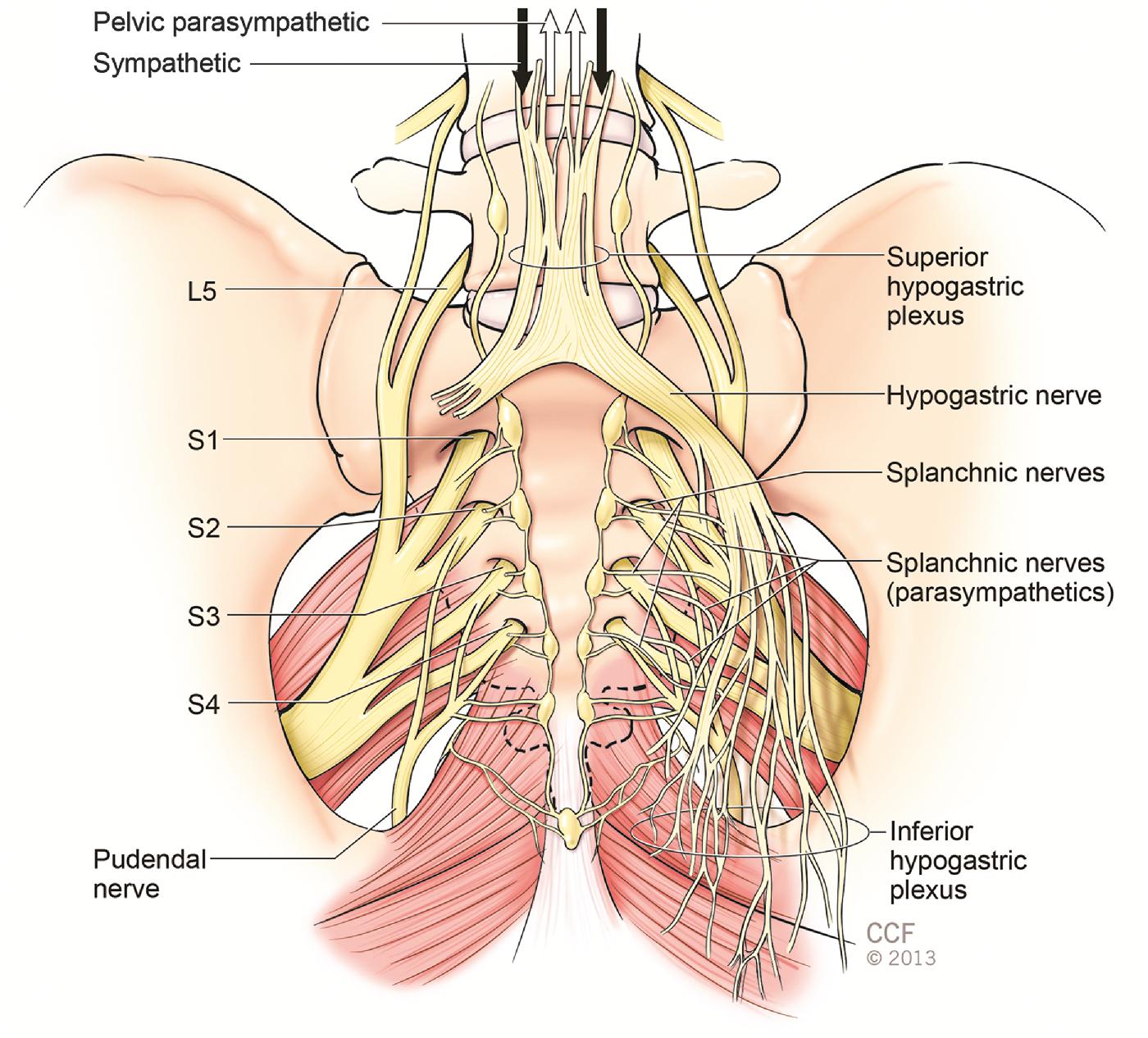
Although the muscles of the pelvic floor were initially thought to have innervation from direct branches of the sacral nerves on the pelvic surface and via the pudendal nerve on the perineal surface, evidence indicates that these standard descriptions are inaccurate, and that the levator ani muscles are innervated primarily, if not solely, by a nerve traveling on the superior (intrapelvic) surface of the muscles, without contribution of the pudendal nerve ( Fig. 1.5 ). Other lumbosacral branches include the nerves to the piriformis and obturator internus, the pelvic splanchnic nerves, and the cutaneous nerves.
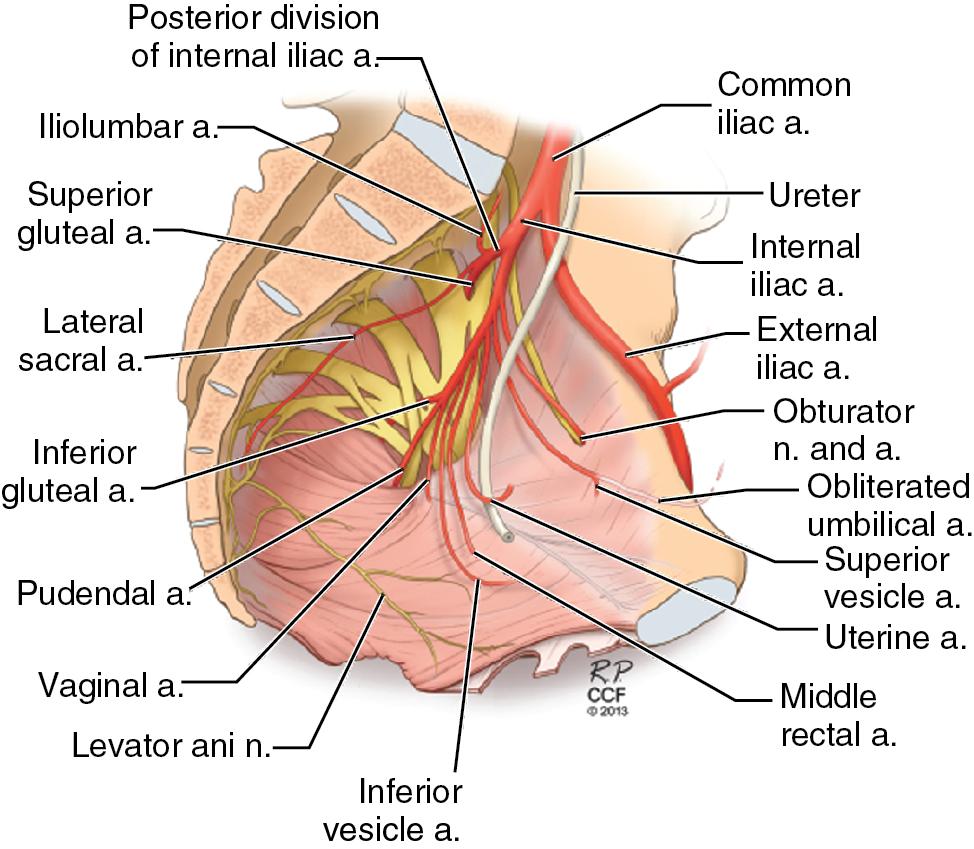
The autonomic nervous system innervates the pelvis through the superior and inferior hypogastric (or pelvic) plexuses (see Fig. 1.4 ). The superior hypogastric plexus receives sympathetic input from the thoracic and lumbar splanchnic nerves (T5–L2) and afferent pain input from the pelvic viscera. It lies over the bifurcation of the aorta in the presacral space and splits into two hypogastric nerves that run along the internal iliac vessels. This sympathetic innervation promotes organ storage by causing relaxation of the bladder and rectum and contraction of the smooth-muscle components of the urethral and anal sphincters. Parasympathetic input derives from S2 to S4 via the pelvic splanchnic nerves that travel to join the hypogastric plexus through the lateral pelvic wall and promote evacuation of the bladder and rectum. When the hypogastric nerves are joined by the pelvic splanchnic nerves, the pelvic plexuses (inferior hypogastric plexus) are formed. The pelvic plexuses consist of three areas: the vesical plexus, the uterovaginal plexus, and the middle rectal plexus extending bilaterally to provide autonomic innervation of their corresponding viscera.
The uterus is a muscular organ consisting of the uterine fundus, isthmus, and cervix. The uterus and cervix are continuous with the anterior apical portion of the vagina and are connected superiorly to the ovaries via the uteroovarian ligaments. The ovaries receive their blood supply from the ovarian (gonadal) vessels that originate from the aorta. The uterus receives most of its blood supply bilaterally from the uterine arteries (see Fig. 1.5 ). The uterine arteries originate at the anterior division of the internal iliac arteries and reach the lower uterine segment within the cardinal ligament. The arteries caudally give off the vaginal branches and continue along the lateral surface of the uterus to anastomose with the ovarian blood supply.
The uterus is a midline organ positioned posterior to the bladder and anterior to the rectum. Condensations of peritoneum form the cardinal and broad ligaments, the round ligaments, and the suspensory ligaments of the ovary (infundibulopelvic ligament). The cardinal ligaments are a condensation of the endopelvic fascia, which is part of the supportive structure of the uterus. They extend outward and laterally from the uterine isthmus and cervix in a three-dimensional fan-like manner and are continuous with the endopelvic fascia of the pelvic sidewall. In addition to playing a role in upper vaginal support, they divide the deeper pelvis into avascular planes anteriorly called the paravesical space and posteriorly called the pararectal space. The retropubic space (space of Retzius) is continuous with the paravesical space. The borders of the paravesical space are the obturator internus and neurovascular bundle laterally, the cardinal ligament posteriorly, the pubic symphysis anteriorly, and the obliterated umbilical artery medially. The borders of the pararectal space are the cardinal ligament anteriorly, the rectum medially, the internal iliac artery laterally, and the sacrum posteriorly.
The vagina is a hollow, fibromuscular tube with rugal folds that extends from the vestibule to the uterine cervix. In the standing woman, the upper two-thirds of the vagina is almost horizontal, whereas the lower one-third is nearly vertical. The vaginal wall is histologically composed of three layers. It is lined by a nonkeratinized stratified squamous epithelium that lies over a thin, loose layer of connective tissue, the lamina propria. The lamina propria contains no glands. Coursing through the lamina propria are small blood vessels. Vaginal lubrication is via a transudate from the vessels, the cervix, and the Bartholin’s and Skene’s glands. Beneath the lamina proppria is the vaginal muscularis, a well-developed fibromuscular layer consisting primarily of smooth muscle with smaller amounts of collagen and elastin. The muscularis is surrounded by an adventitial layer, which is a variably discrete layer of collagen, elastin, and adipose tissue containing blood vessels, lymphatics, and nerves. The adventitia represents an extension of the visceral endopelvic fascia that surrounds the vagina and adjacent pelvic organs and allows for their independent expansion and contraction.
The walls of the vagina are in contact except where its lumen is held open by the cervix. The vaginal lumen is H-shaped, with the principal dimension being transverse. In addition, the upper vagina is supported by connective tissue attachments to the sacrum, coccyx, and lateral pelvic sidewalls; these are identified at surgery as the cardinal and uterosacral ligament complex.
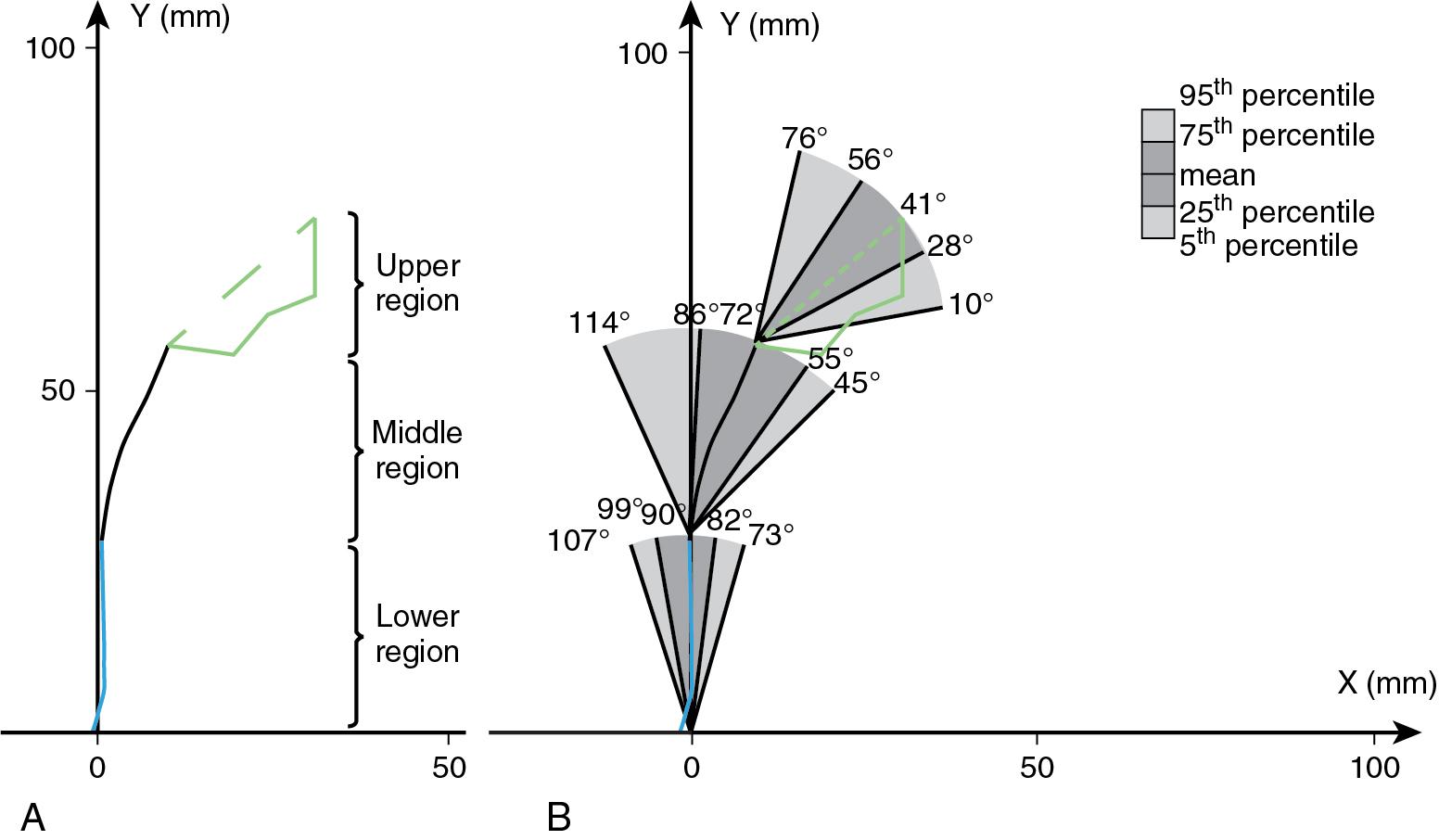
There is considerable variability in vaginal length, size, and width among women. Based upon magnetic resonance imaging studies of women with normal support, the average length of the anterior vaginal wall is 6.3 cm, with a wide range of 4.4 to 8.4 cm. Similarly, the average length of the posterior vaginal wall is 9.8 cm, with a range of 5.1 to 14.4 cm ( ). The vaginal width is greatest at its cranial portion and decreases as it passes through the pelvic diaphragm, to its smallest width at the introitus. There are large variations in transverse dimensions; in one study, as much as a five-fold variation was seen in total vaginal surface area (34–164 cm 2 ) ( ). In women with normal vaginal support, there are three major vaginal axes, with an average angle of 90 degrees relative to the horizontal for the lower vagina, 72 degrees for the middle vagina, and 41 degrees for the upper vagina; however, these angles vary significantly among women ( ; Fig. 1.6 ).
The presence of a true fascia between the vagina and adjacent organs has been debated. Surgical terms such as pubocervical fascia and rectovaginal fascia refer to layers that are developed as a result of separating the vaginal epithelium from the muscularis or by splitting the vaginal muscularis layer. Anteriorly, the vagina lies adjacent to and supports the bladder base, from which it is separated by the vesicovaginal adventitia (endopelvic fascia). The urethra is fused with the anterior vagina, with no distinct adventitial layer separating them. The terminal portions of the ureters cross the lateral fornices of the vagina on their way to the bladder base. Posteriorly, the vagina is related to the cul-de-sac, to the rectal ampulla, and inferiorly to the perineal body. Embryologically, an extension and fusion of the peritoneum from the cul-de-sac attached to the posterior surface of the vaginal muscularis forms the rectovaginal septum. A layer of adventitia separates the muscular layer of the rectum from the posterior vaginal wall, except at the level of the perineal body, where there is fusion of the vaginal muscularis and connective tissue of the perineal body. The dense connective tissue of the perineal body extends 2 to 3 cm cephalad from the hymenal ring along the posterior vaginal wall and forms what some have called the rectovaginal fascia. Although at the time of surgery there appears to be an identifiable fascial plane, , , and have each concluded that between the adjacent organs is primarily vaginal muscularis or loose fibroadipose tissue, and that no fascia is histologically present.
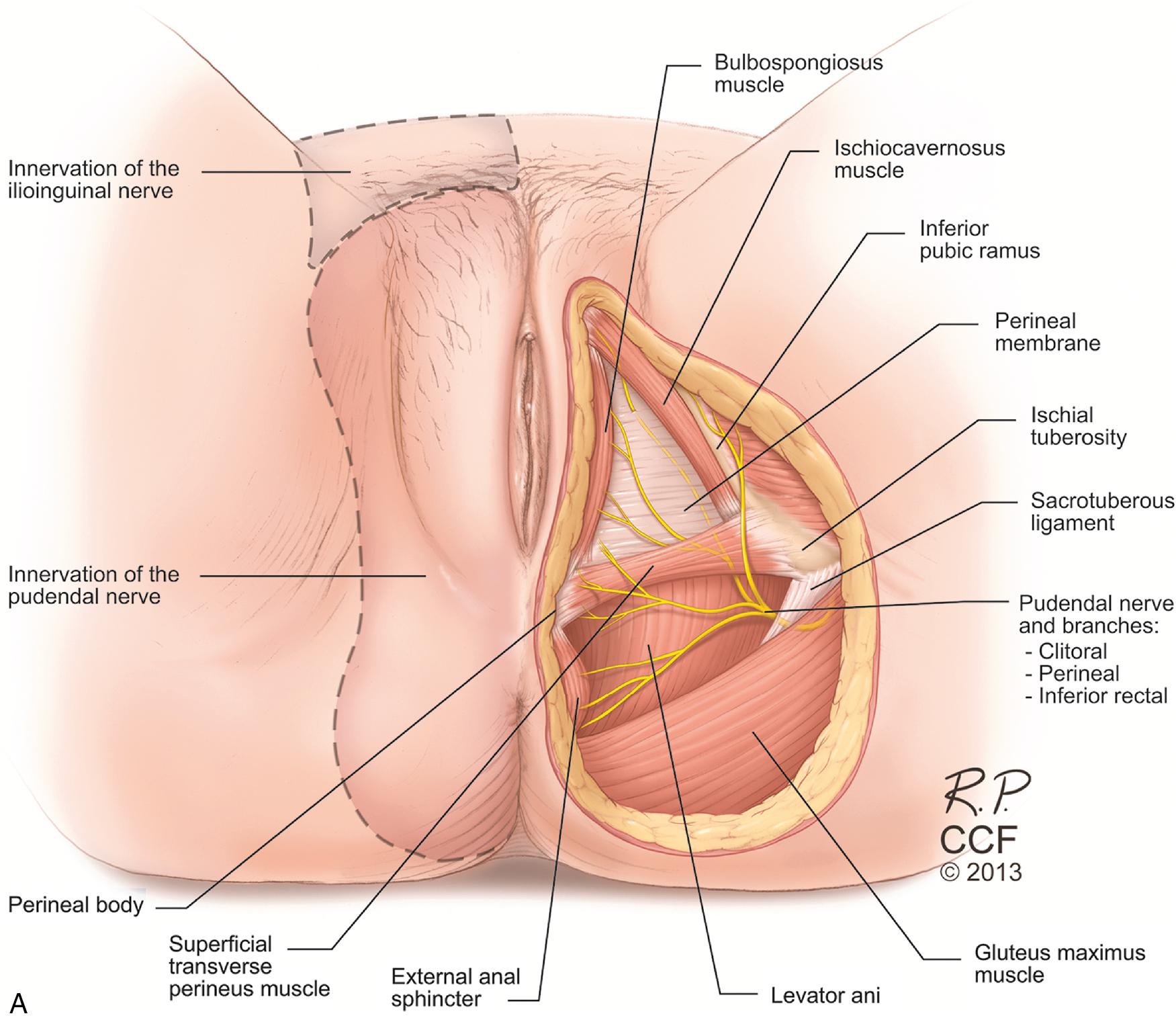
The perineum is divided into two compartments: superficial and deep. These are separated by a fibrous connective tissue layer called the perineal membrane. The perineal membrane is a triangular sheet of dense fibromuscular tissue that spans the anterior half of the pelvic outlet. It was previously called the urogenital diaphragm; this change in name reflects the appreciation that it is not a two-layered structure with muscle in between, as was previously thought. The perineal membrane provides support to the vagina and urethra as they pass through it. Cephalad to the perineal membrane lies the striated urogenital sphincter muscle, which compresses the mid- and distal urethra ( Fig. 1.7 ). The borders of the perineum are the ischiopubic rami, the ischial tuberosities, the sacrotuberous ligaments, and the coccyx ( Fig. 1.8 A). A line connecting the ischial tuberosities divides the perineum into the urogenital triangle anteriorly and the anal triangle posteriorly. The perineal body marks the point of convergence of the bulbospongiosus muscles, the superficial and deep transverse perinei, the perineal membrane, the external anal sphincter, the posterior vaginal muscularis, and the insertion of the puborectalis and pubococcygeus (puboperinealis) muscles. The bulbospongiosus originates on the inferior surface of the superior pubic rami and the crura of the clitoris. It inserts on the perineal body, where its fibers blend with the superficial transverse perinei and the external anal sphincter. The superficial transverse perinei are bilateral muscles that extend from the medial ischial tuberosities to insert on the perineal body. The ischiocavernosus muscles originate from the medial ischial tuberosities and ischiopubic rami. They insert on the inferior aspect of the pubic angle.
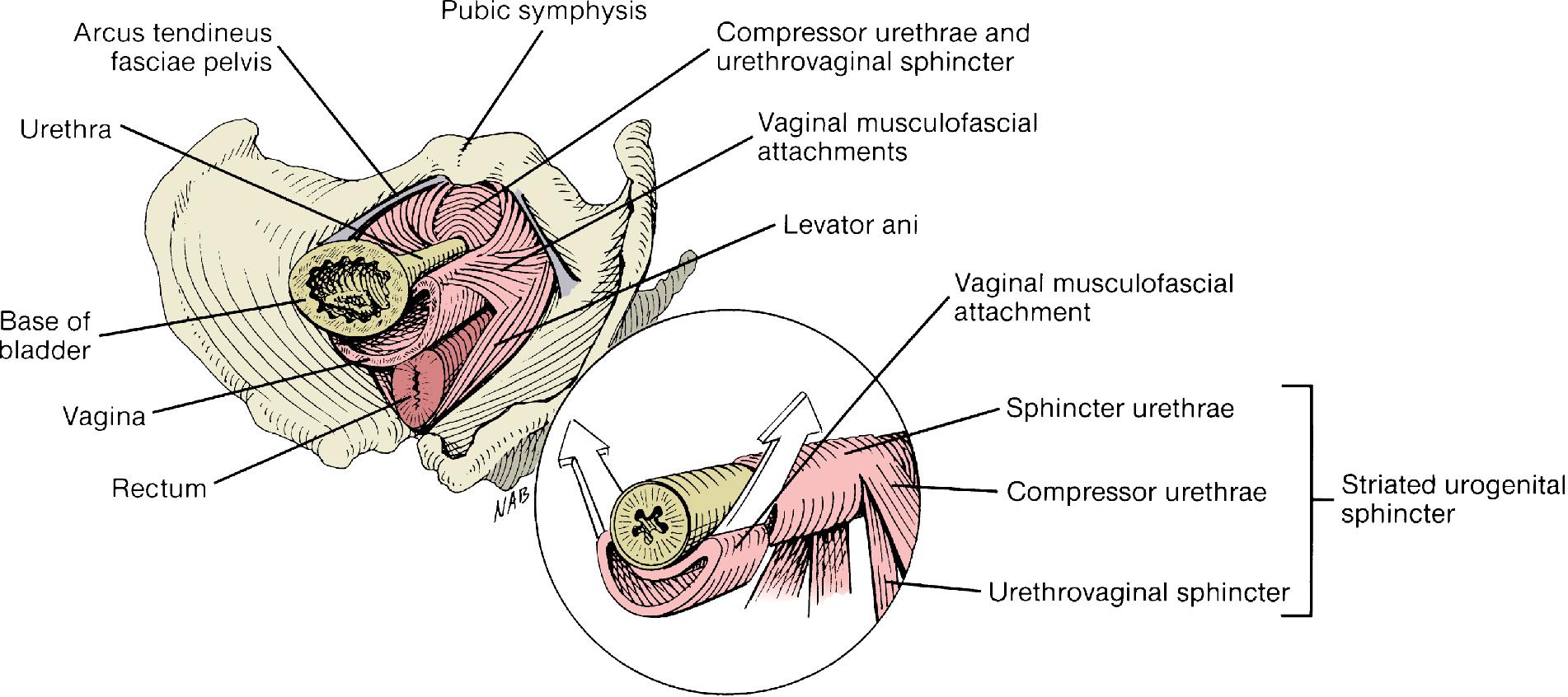
The deep perineal compartment is composed of the deep transverse perineus muscle, portions of the external urethral sphincter muscles (compressor urethrae and urethrovaginal sphincter), portions of the anal sphincter, and the vaginal musculofascial attachments.
The neurovascular anatomy of the perineum is illustrated in Fig. 1.8 A and B. The motor and sensory innervation of the perineum is via the pudendal nerve. The pudendal nerve originates from S2 to S4, exits the pelvis through the greater sciatic foramen, hooks around the ischial spine, and then travels along the medial surface of the obturator internus through the ischiorectal fossa in a thickening of fascia called Alcock’s canal. It emerges posterior and medial to the ischial tuberosity and divides into three branches to supply the perineum: the clitoral, perineal, and inferior rectal (inferior hemorrhoidal) branches. The inferior rectal nerve provides innervation to the external anal sphincter. The blood supply to the perineum is from the pudendal artery, which travels with the pudendal nerve to exit the pelvis. Similar to the nerve, there are three main branches, with rich collateral anastomoses.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here