Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
While rare, fractures of the distal humerus are complex and have always created unique challenges for orthopedic surgeons. Until the second half of the 20th century, most of these fractures could not be reliably fixed and therefore were treated nonoperatively. Complications including nonunion, malunion, neurovascular injury, and joint stiffness were common. Subsequently with nonoperative management, patients often could not return to employment and the psychosocial effects were substantial. With the development of principle-based internal fixation of distal humerus fractures and the advancements of total elbow arthroplasty (TEA) over the past several decades, there has been substantial improvement in the prognosis after injury. While these fractures remain a challenge for modern-day surgeons, most patients can now expect a functional elbow at the conclusion of treatment, allowing improved quality of life and contribution to society.
The elbow joint functions as a constrained hinge. The distal humerus consists of a widened portion of the metaphysis forming the medial and lateral supracondylar ridges and the corresponding articular surfaces of the humerus. Conceptually, the articular surface of the distal humerus can be divided into two separate components: ulnohumeral and radiocapitellar. The ulnohumeral joint is responsible for flexion and extension. The radiocapitellar joint supports the radius during forearm axial rotation. These joints are anatomically part of the same synovial complex, but may be viewed as functionally independent.
The ulnohumeral hinge joint can also be referred to as the ulnotrochlear joint. The trochlea forms the center of the hinge and it is supported by the medial and lateral columns. The word trochlea is Latin for pulley and the trochlea is truly shaped like a pulley. It has a 300-degree arc of thick cartilage that articulates with the semilunar notch of the ulna. This articulation is what provides the highly constrained relationship between humerus and olecranon, with substantial contributions to the bony stability of the elbow. Because of this, the integrity of the trochlea is an important part of the classification system discussed later in the chapter.
The radiocapitellar joint is the articulation between radial head and the capitellum, on the anterior aspect of the lateral column of the humerus. This is a far less constrained joint, allows for axial rotation, and accommodates flexion and extension. The capitellum is covered with thick hyaline cartilage and is spheroidal in shape. There is a groove that separates the capitellum from the trochlea. This is where the radial head articulates with the humerus throughout pronation, supination, and flexion. ,
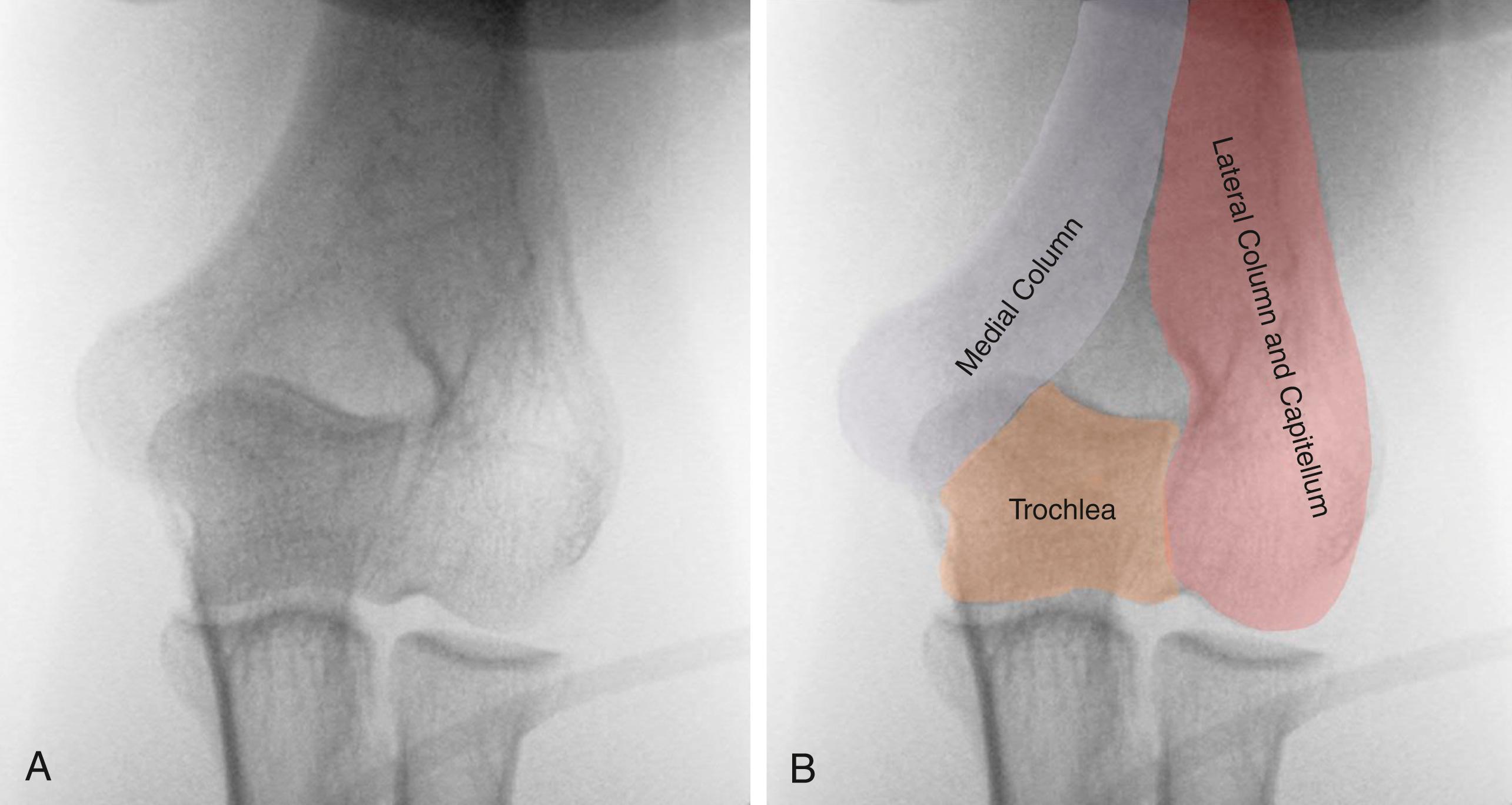
Biomechanically, in the coronal plane, the trochlea and the medial and lateral columns represent a mechanical triangle. The columns are triangular in cross section and the apices of the triangles point toward the central fossa. Because these columns support the articular surface, it is critical to restore both the medial and lateral columns when performing fracture fixation. While the medial column is entirely extra-articular, the capitellum forms part of the lateral column. The medial column ends as the medial epicondyle ( Fig. 36.1A–B ).
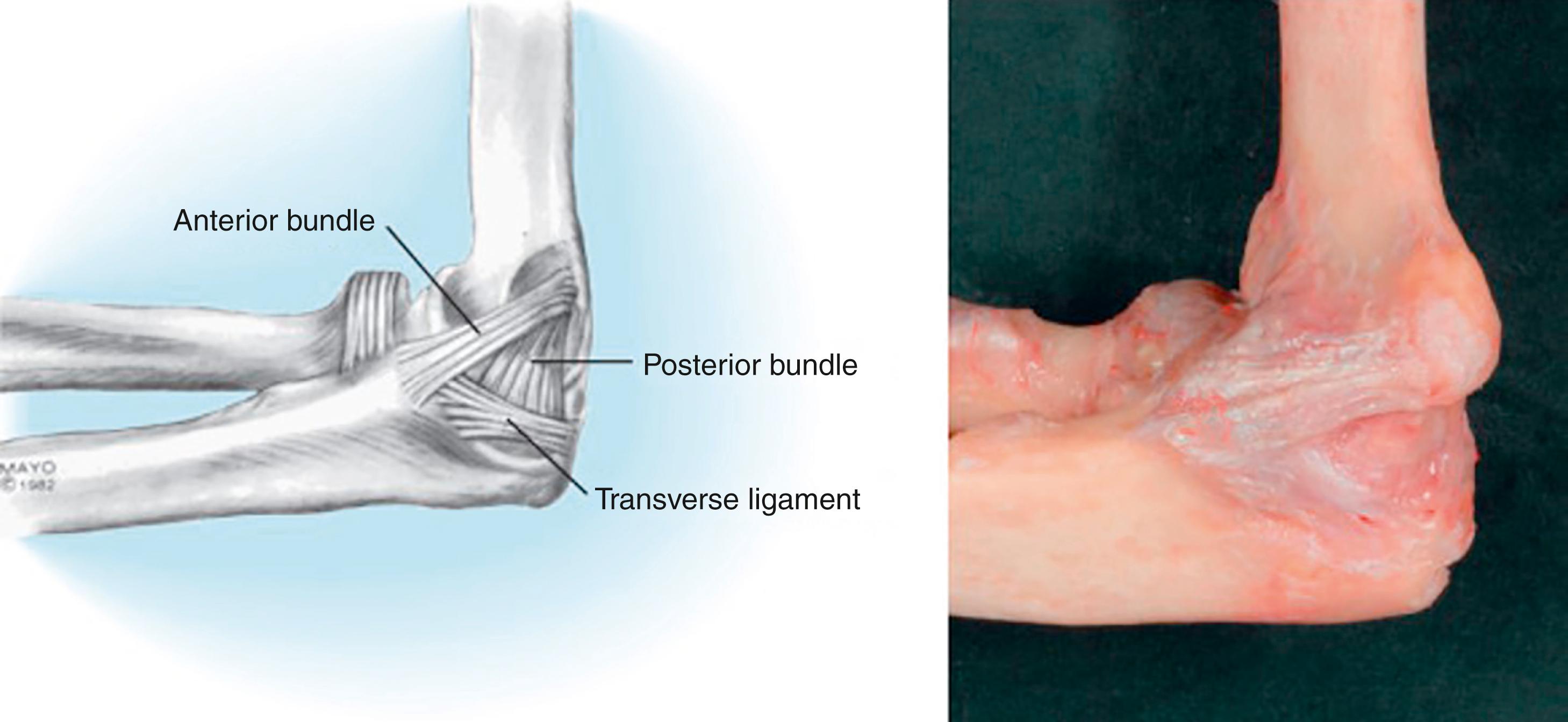
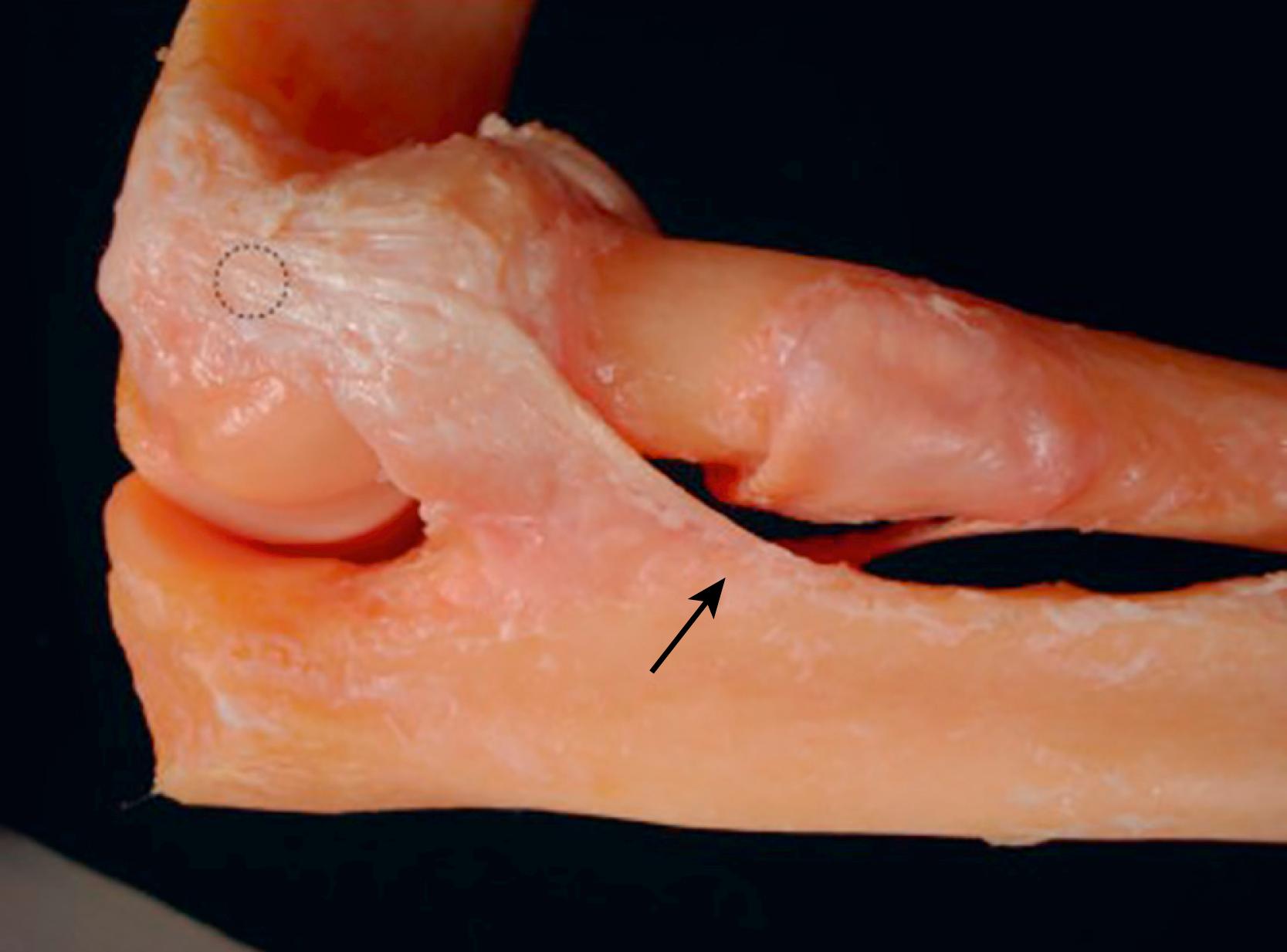
The ulnohumeral joint is also constrained by ligamentous supports. Medially, the medial ulnar collateral ligament (mUCL or MCL) originates on the distal aspect of the medial epicondyle and attaches to the ulna at the sublime tubercle ( Fig. 36.2 ). The medial epicondyle also functions as the origin of the flexor/pronator mass. The MCL is a major contributor to valgus and posteromedial rotary restraint. Thus, due to the ligamentous contribution of the MCL to elbow stability, anatomic reduction of the bone origin of this structure is important. The lateral column terminates as the lateral supracondylar ridge and epicondyle, which provide origins for the lateral collateral ligament and extensor mass ( Fig. 36.3 ). These soft tissue structures also contribute to elbow stability.
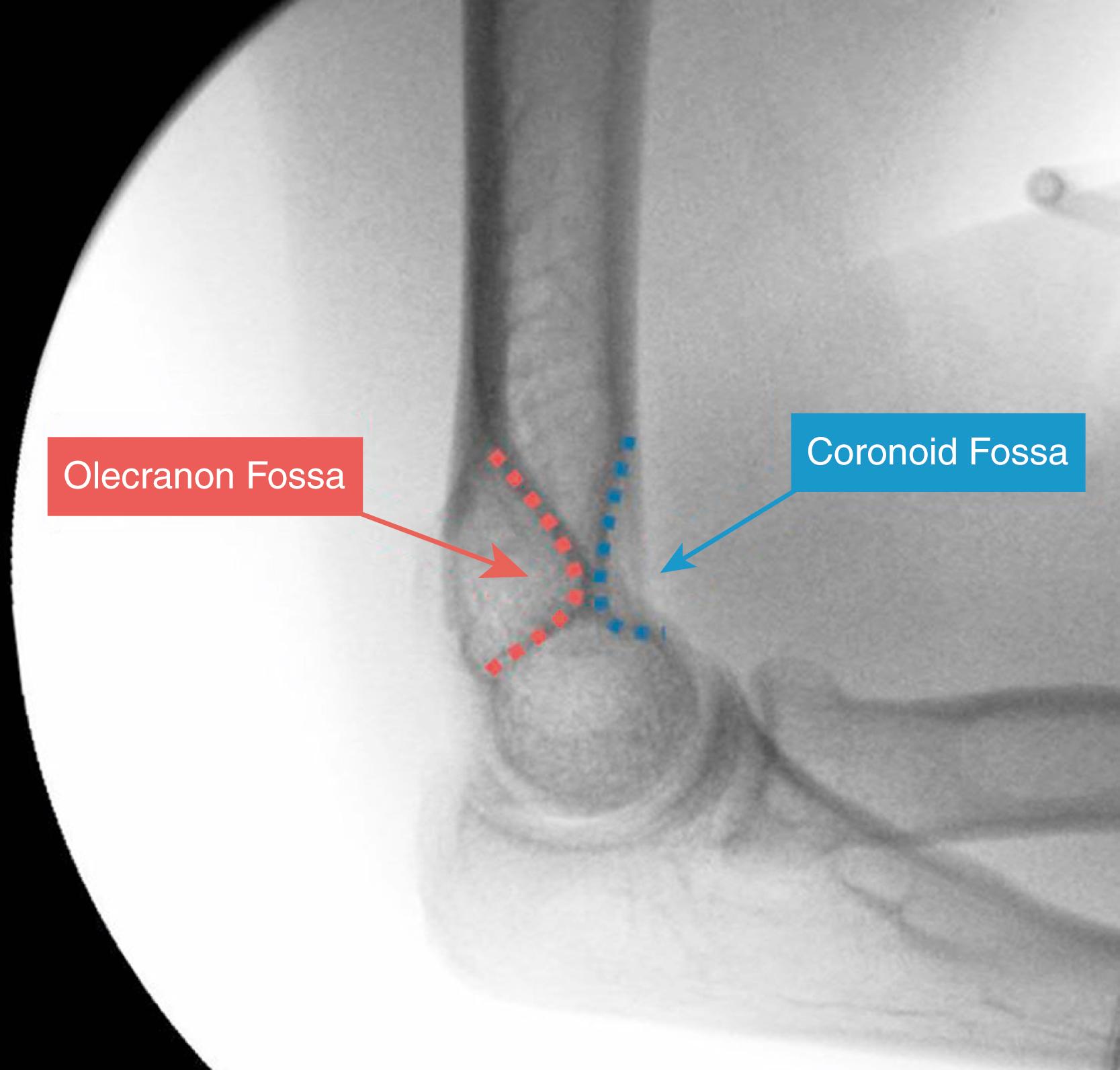
The olecranon and coronoid fossa are located proximal to the trochlea between the medial and lateral columns. These fossae accommodate the proximal ulna during extension and flexion ( Fig. 36.4 ). Impingement of the proximal ulna into these fossae, which can occur with inadequate fracture reduction, supracondylar shortening, or inadvertent insertion of screws through these fossae, will impede elbow range of motion (ROM) postoperatively.
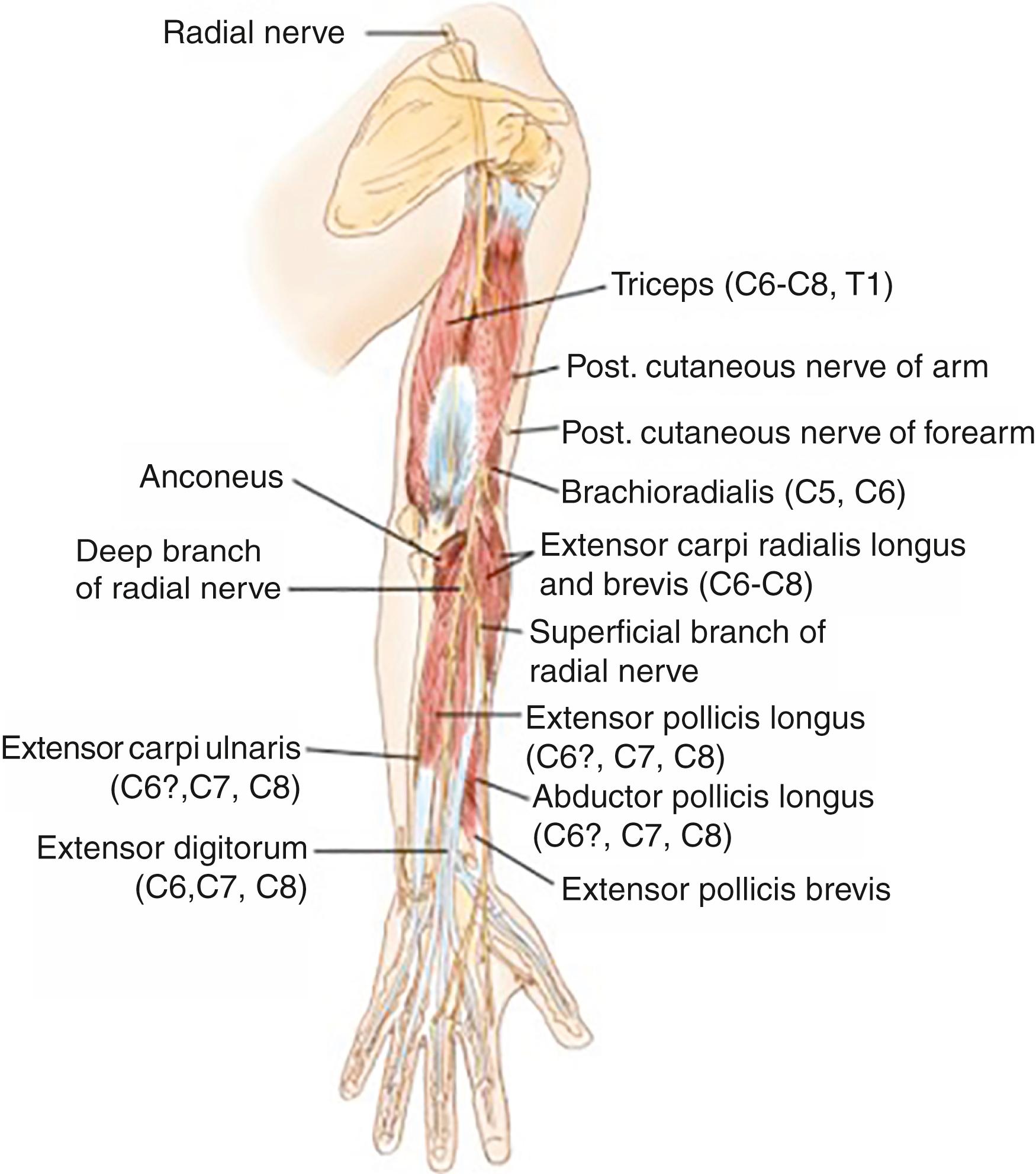
To safely manage distal humerus fractures, understanding the anatomy of the neurovascular structures in the elbow region and their precise locations is required. The radial nerve enters the spiral groove of the humerus 20 cm proximal to the medial condyle and then circles around the posterior humeral shaft. It exits the spiral groove approximately 10–15 cm proximal to the lateral epicondyle. The lateral antebrachial cutaneous nerve and the motor branches to the triceps and anconeus branch were off at this location. The radial nerve then courses anteriorly through the lateral intramuscular septum. While the nerve courses between the brachialis and the brachioradialis, it bifurcates into the posterior interosseous nerve (PIN) and the radial sensory nerve. The radial nerve is at risk when there is proximal extension of fractures into the spiral groove, with excessive traction, and when using longer lateral plates during fixation ( Fig. 36.5 ).
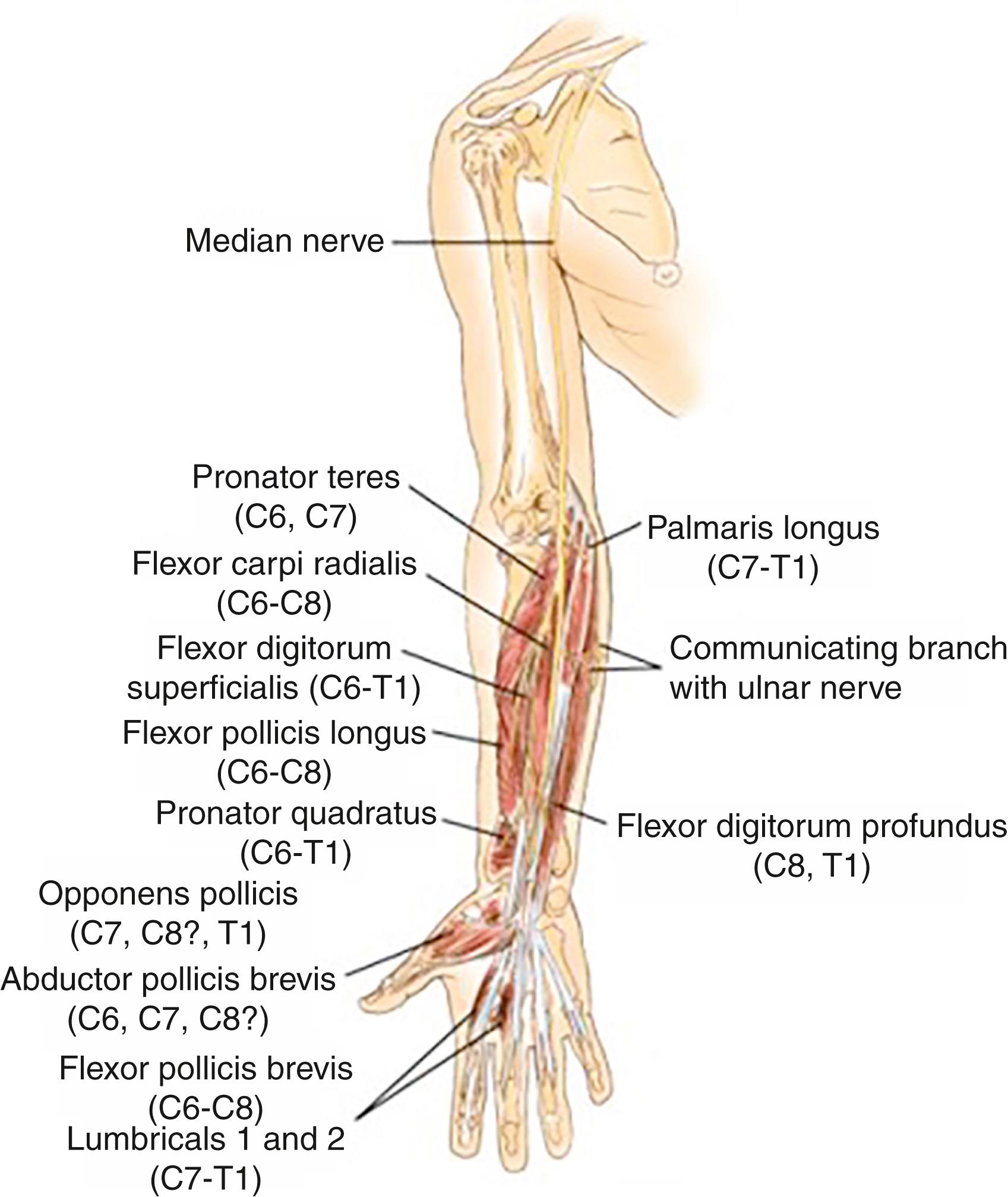
In the anteromedial aspect of the arm, the median nerve and brachial artery travel together between the biceps and brachialis muscles, with the median nerve lying medial ( Fig. 36.6 ). They both course anterior to the medial intermuscular septum and then under the bicipital aponeurosis into the medial antecubital fossa. They then course between the heads of pronator teres and distally under flexor digitorum superficialis. Injury to these structures has been reported infrequently, likely due to the protection provided by the brachialis muscle.
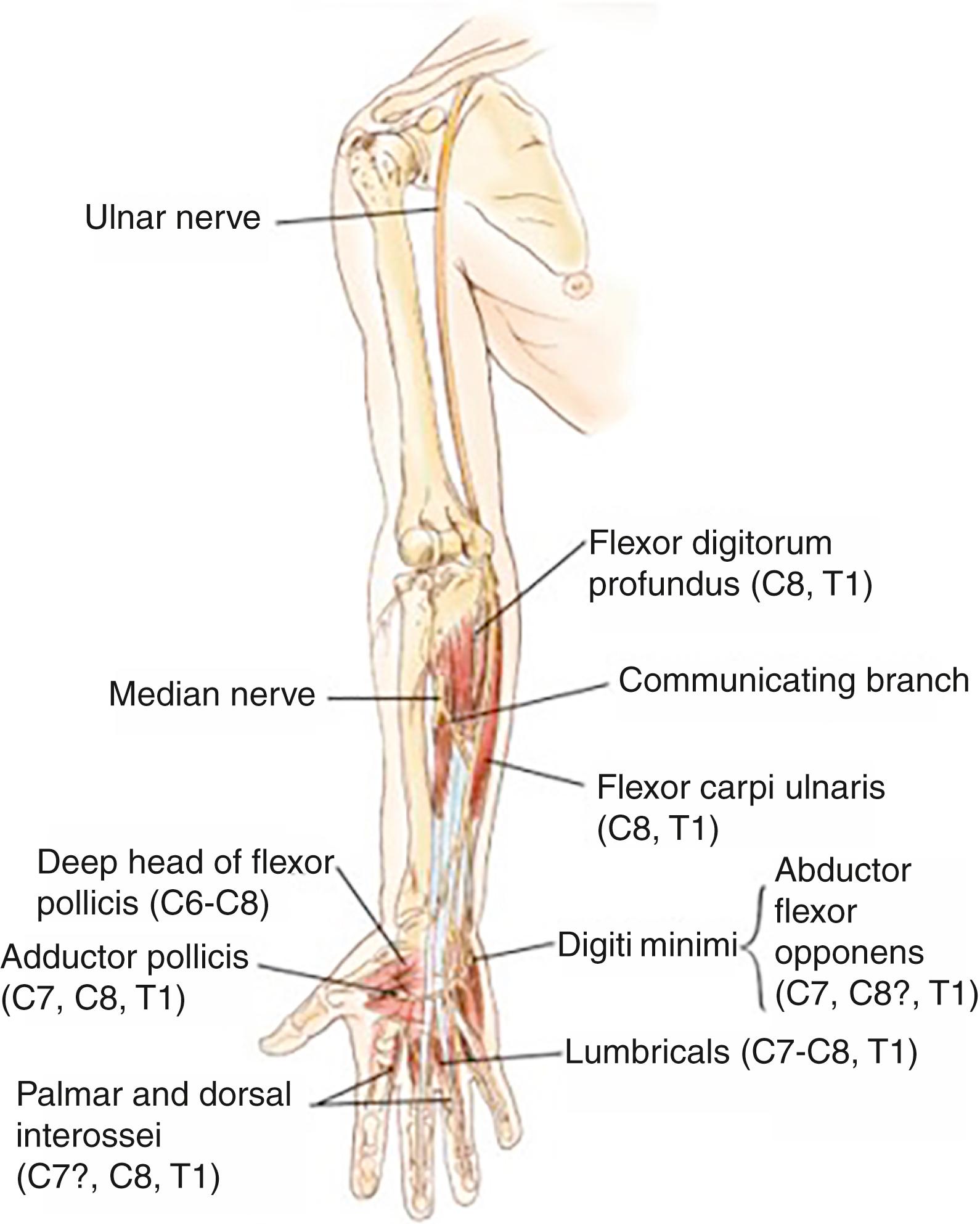
The ulnar nerve travels anterior to the medial intermuscular septum in the upper arm until reaching the arcade of Struthers. It then pierces the intermuscular septum and enters the posterior compartment, where it travels with the medial head of the triceps. The ulnar nerve then courses behind the medial epicondyle and into the cubital tunnel, where it rests on the MCL. The ulnar nerve enters the anterior forearm between the two heads of flexor carpi ulnaris ( Fig. 36.7 ). Injury to the ulnar nerve can occur either as a consequence of the injury or secondary to nerve manipulation at the time of surgery during initial injury or iatrogenically during open reduction internal fixation (ORIF) and occurs in 20% of patients postoperatively.
Management of the ulnar nerve during distal humerus fixation remains a controversial topic. While identification and protection of the nerve are required for safe surgical management, there is controversy about the value of transposition. Transposition decompresses the nerve and allows it to run a new course safely away from internal fixation devices and fracture fragments. However, the extent of dissection necessary to transpose the ulnar nerve can devascularize the nerve and contribute to unintended iatrogenic injury. The data do not clearly support transposition or in situ nerve placement and thus remain based on the surgeon’s preference.
The blood supply of the distal humerus is another factor to consider. The distal humerus has an extensive anastomotic blood supply. The extraosseous blood supply can be categorized into medial, lateral, and posterior arcades. These arcades receive blood supply from a variety of arteries around the elbow. Perforating vessels from these three arcades contribute to the interosseous blood supply. The rich local blood supply facilitates revascularization of large fracture fragments, and with the exception of capitellar shear fractures, osteonecrosis is relatively rare after internal fixation of distal humerus fractures.
The age distribution of distal humerus fractures follows a trimodal pattern. The age of the patient and the nature of the injury affect fracture patterns, comminution, and bone loss. Pediatric supracondylar fractures, which are very common, exceed the scope of this chapter. In the young/middle-age adult population, high-energy distal humerus fractures are most commonly the consequence of motor vehicle accidents or other high-energy trauma. The most common type of adult distal humerus fracture, however, occurs in elderly patients with underlying osteopenia or osteoporosis after a mechanical fall from standing. The increasing independence and longevity afforded by modern lifestyles and health care have increased the frequency of these fractures in the elbow surgeon’s practice.
A careful assessment of the pathoanatomy of distal humerus fractures by the treating surgeon is critical. Anteroposterior (AP) and lateral X-ray of distal humerus fractures are routinely obtained as a basic imaging modality ( Figs. 36.8 and 36.9 ). When patient features and fracture complexity suggest the use of elbow arthroplasty, plain radiographs may be sufficient. On the contrary, in the majority of fractures considered for internal fixation, plain radiographs are inadequate to assess the complex geometry of the distal humerus and its fractures. Furthermore, in our practice, we prefer three-dimensional computed tomography (3D CT) to traction views based on the ability to accurately interpret fracture fragments. For this reason, we almost always obtain a CT scan after application of a temporary splint. Obtaining the CT scan with the patient’s arm over their head allows substantially improved visualization of fracture fragments and bony detail, especially in larger patients. This can typically be done without substantial increase in patient discomfort. 3D rendering can contribute greatly to the surgeon’s understanding of the fracture pattern and is requested in essentially all of these injuries. Using the 3D CT scan, a more complete understanding of the extent and severity of the injury can be obtained ( Figs. 36.10 and 36.11 ).




A careful physical examination can help determine whether neurovascular structures are injured. The skin should be assessed for possible open fractures; abrasions should be cleaned and investigated to avoid missing an open fracture ( Fig. 36.12 ). The radial pulse should be palpated and compared to the contralateral limb. A wrist and hand examination should be completed to assess for wrist pain and distal radioulnar joint (DRUJ) instability and pain. This is especially advisable in the setting of associated proximal ulna and/or radius fractures. In the setting of high-energy distal humerus fractures, a thorough secondary and tertiary survey should be completed to assess for associated injuries.

Several main pathoanatomical factors differentiate the severity of the injury and can help guide decision-making and treatment. First, intra-articular involvement (and the degree of intra-articular involvement) is critical. Extra-articular fractures requiring surgery can typically be repaired through a “triceps-on” approach. These fractures seem to be associated with a lower rate of posttraumatic contracture and typically have a more predictable postoperative outcome. Intra-articular fractures, particularly those with intra-articular comminution and segmental intra-articular involvement, typically necessitate additional distal exposure, through some variation of a triceps-reflecting approach (most commonly olecranon osteotomy). It is our opinion that intra-articular fractures with a fracture line separating the medial epicondyle from the medial trochlea are especially challenging ( Figs. 36.13 and 36.14 ).


A second critical factor is whether the fracture is open or closed. In most cases of open distal humerus fracture, the distal humerus is driven through the triceps posteriorly and out through the skin. This typically leaves a substantial defect in the triceps tendon and, in some cases, can be associated with bone loss ( Fig. 36.15 ). In these cases, early parenteral antibiotics, aggressive debridement of the open fracture, and sometimes staged management are indicated. Antibiotic-eluting cement beads may be inserted at the fracture site, which may be temporarily stabilized with a splint or external fixator.

One additional factor that should be scrutinized in preoperative imaging is the degree of supracondylar comminution. In young patients, with good bone quality and minimal comminution, a direct extra-articular reduction can often facilitate anatomic reduction of the intra-articular portion of the fracture. However, in older patients, or in patients with profound supracondylar comminution, the narrow column structure of the distal humerus can preclude an accurate extra-articular read. In cases of substantial supracondylar comminution, a nonanatomic reduction is accepted, utilizing supracondylar shortening, in order to get bony apposition and compression.
Finally, although rare, some patients can have associated fractures to the proximal radius and ulna. These fractures will necessitate additional treatment plans to address them. In some cases, an olecranon fracture can be utilized as the olecranon osteotomy. In other cases, radial head pathology or ligament injuries need to be addressed in addition to the distal humerus. All these structures should be carefully scrutinized on preoperative imaging.
Due to increasing acceptance of operative treatment, multiple classification systems have been created. A useful classification system should reliably describe the pattern of the injury, guide treatment, predict prognosis, and facilitate research. As is true for many other anatomic areas, a comprehensive and effective classification system remains elusive for distal humerus fractures. No classification scheme has had high rates of inter- and intraobserver agreement.
The AO/OTA (AO Foundation/Orthopaedic Trauma Association) classification system provides an effective framework for discussing and treating distal humerus fractures ( Fig. 36.16 ). Similar to classification systems for other periarticular fractures, these fractures are first classified as extra-articular ( Fig. 36.16A ), partial intra-articular-single column ( Fig. 36.16B ), or complex intra-articular-both columns ( Fig. 36.16C ). The increasing complexity and location of comminution are further used to subdivide each category of fracture. These subdivisions become increasingly complex and unwieldy. However, understanding the patterns and concepts outlined by the AO/OTA classification system can assist surgical decision-making and communication.
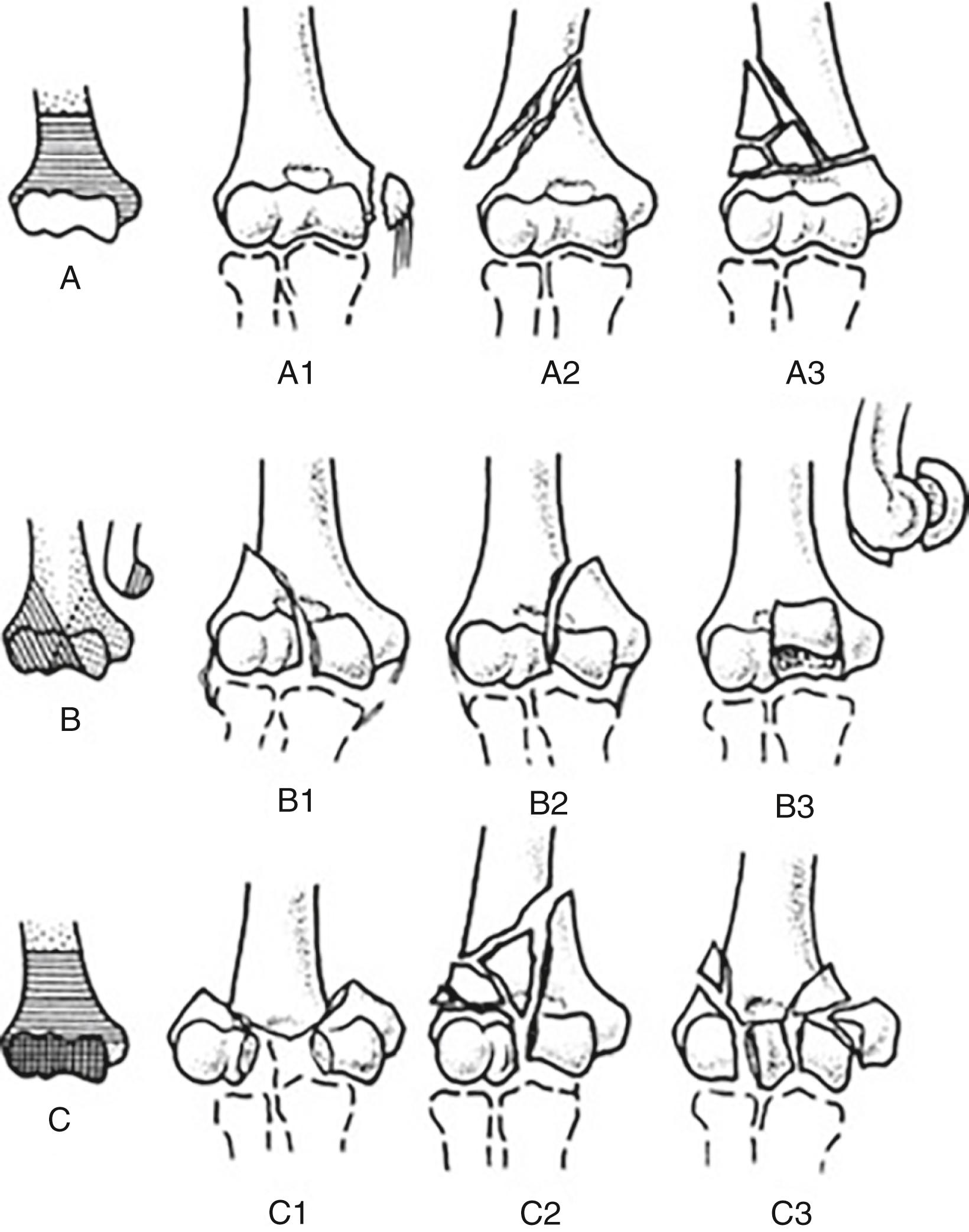
Other commonly used classification schemes are the Milch and the Jupiter classification schemes. At our institution, we typically divide fractures as described in the most recent edition of Morrey’s The Elbow and Its Disorders . First, fractures are divided into extra-articular fractures and intra-articular fractures. Extra-articular fractures include (1) transcondylar fractures (transverse fractures through the condyles at or below the top of the olecranon fossa) ( Figs. 36.17 and 36.18 ), (2) supracondylar fractures ( Figs. 36.19 and 36.20 ), and (3) epicondyle fractures (avulsions of the lateral or medial epicondyle). Intra-articular fractures are divided into either (1) intercondylar fractures (fractures of the columns with intra-articular involvement) ( Figs. 36.21–36.23 ) or (2) purely articular fractures, which are typically isolated articular shear fracture of the capitellum. Further fracture classification is provided descriptively.







Broadly, treatment can be divided into three categories: nonoperative management, ORIF, and TEA. Nonoperative management is considered for nondisplaced fractures and, particularly, in the elderly and infirm population. In select patients, conservative treatment may lead to an acceptable outcome, even in the absence of bony union. ORIF is the treatment of choice for the vast majority of distal humerus fractures, particularly in the young and healthy. Modern fixation methods have made this treatment regimen more reliable and have decreased the risk of catastrophic failure. In elderly patients presenting with a complex fracture pattern, elbow arthroplasty is a reasonable option for the primary treatment of comminuted intercondylar distal humerus fractures.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here