Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
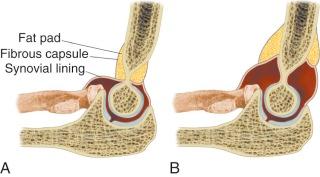
The anterior fat pad is anterior to the olecranon fossa and is routinely seen on the normal lateral view, extending inferior, from the anterior humeral cortex, obliquely. The posterior fat pad lies in the olecranon fossa and is not visible on the normal lateral view ( Fig. 11-1 ). Both fat pads are within the joint, intraarticular, extrasynovial, and therefore sensitive to any space-occupying lesion. Fluid, blood, or mass will displace the anterior fat pad superiorly and the posterior fat pad posteriorly. The anterior fat pad is displaced with small volumes of fluid that would not displace the posterior fat pad and, therefore, is more sensitive to an intraarticular pathologic process ( Figs. 11-2 and 11-3 ). Very large effusions may obliterate the anterior fat pad, in which case the displacement of the posterior fat pad is more sensitive.


The supracondylar spur, a normal variant seen in approximately 1% of the population, may be seen on the lateral view. Unlike an exostosis, it does not point away from the joint. This may be associated with compressive neuropathy.
Often there is a projection or bony flange at the lateral aspect of the supracondylar humerus, which should not be confused with periosteal reaction.
The radial tuberosity often appears as a relative area of radiolucency when seen en face on the lateral view. When the tuberosity is prominent, this radiolucency should not be confused with a true lytic lesion.
The inferior aspect of the olecranon apophysis and the far medial and lateral aspect of the distal humeral epiphysis or condyles do not always unite with skeletal maturity and should not be confused with fracture.
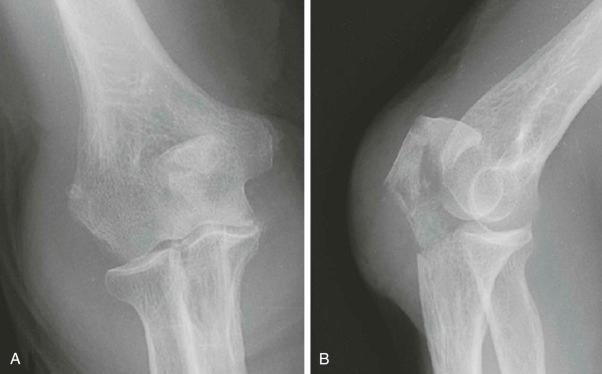
The routine radiographic examination of the elbow consists of anteroposterior and lateral views. The anteroposterior view is obtained with the forearm in supination and the elbow fully extended. The lateral view is obtained with the forearm in neutral position, midway between supination and pronation, and the elbow flexed 90 degrees. On the routine lateral view, three cortical arcs can be appreciated representing the capitellum and lateral and medial trochlear ridge. Anteroposterior internal and external oblique views may also be obtained in a search for occult fracture. The radiocapitellum view is a lateral view obtained by angling the x-ray tube 45 degrees cephalad. This projects the radiocapitellum joint compartment superior to the ulna-trochlea compartment, negating the superimposition of these anatomic structures.
The most common elbow fracture in the adult involves the radial head and neck, accounting for about 50% of all such injuries. Most occur in young adults, are nondisplaced, and result from a fall on the outstretched hand.
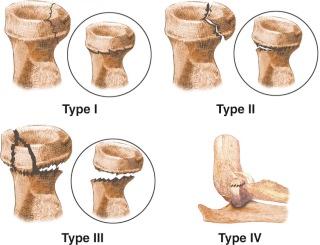
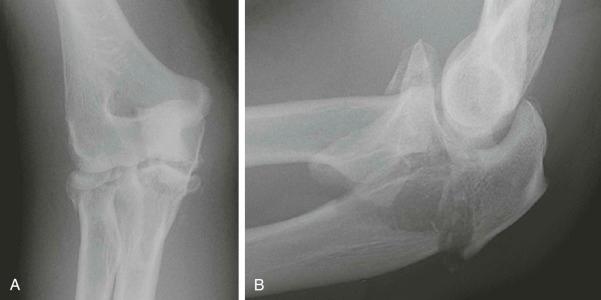
The Mason classification describes four types ( Fig. 11-4 ). Type I fractures are nondisplaced and may be difficult to visualize with radiographic examination. The radiographic appearances include vertical lucency, cortical disruption, cortical step-off or abrupt angulation, and double cortical line ( Fig. 11-5 ). Type II consists of a displaced split fragment. Type III is a comminuted fracture. A fourth type has an associated elbow dislocation.

Complex fractures of the radial head and neck are those associated with other injuries ( Fig. 11-6 ). Markedly comminuted radial head fractures may be associated with subluxation or proximal migration at the distal radioulnar joint. This combination of injuries is referred to as the Essex-Lopresti fracture, named after its first describer. Radiographic examination of the wrist is essential in such situations. Other associated injuries include proximal ulna fracture, capitellum fracture, and elbow dislocation.
The second most common elbow fracture in the adult involves the olecranon, accounting for about 20% of all such injuries. Most occur in older adults, are transverse fractures with diastasis, and result either from a fall on the outstretched hand with the elbow flexed or from direct trauma. The transverse fracture at the trochlear notch extends obliquely to the posterior cortex. Triceps retraction results in diastasis. Comminuted fractures result from direct trauma. Oblique fractures, relative to the long axis of the ulna, may be nondisplaced and difficult to see radiographically.
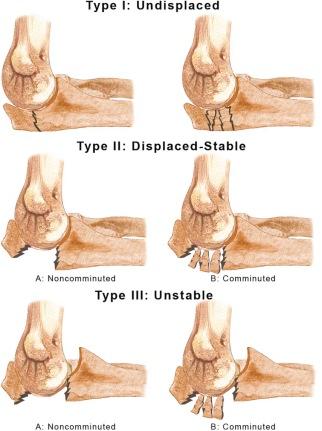
The Mayo classification system ( Fig. 11-7 ) for olecranon fractures addresses issues of comminution, displacement, stability, treatment, and prognosis. Type I, or nondisplaced, fractures account for 5% of olecranon fractures ( Fig. 11-8 ). Displaced fractures with an intact anterior bundle of the medial collateral ligament (type II) are stable and account for 85% of olecranon fractures ( Fig. 11-9 ). Type III, or displaced, unstable fractures are usually comminuted and associated with radial head fracture ( Fig. 11-10 ).


Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here