Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acquired pure red cell aplasia (PRCA) is characterized by the presence of an acquired severe normochromic, most frequently normocytic anemia associated with a complete disappearance of reticulocytes and erythroid precursors in the marrow and normal production of myeloid cells and platelets. Consequently, it is presumed that the defect lies within erythroid precursors and not within stem cells as seen in aplastic anemia. Initially described as progressive anemia with exclusive absence of erythroid series in the bone marrow , PRCA is a rare bone marrow failure disorder without geographic or racial predilection. All ages can be affected, but if present in children, it is called transient erythroblastopenia of childhood (TEC) and may be difficult to distinguish from congenital causes of anemia, mainly Diamond-Blackfan anemia (DBA) (see Chapter 30 ). Former nosology included various terms such as erythrophthisis, chronic hypoplastic anemia, and pure red cell agenesis .
Acquired forms of PRCA must be distinguished from congenital forms of PRCA, which usually manifest themselves early in life (see Chapter 30 ). Acquired PRCA occurring in childhood may be difficult to distinguish from DBA. As an acquired disease, PRCA may be a primary disorder or secondary to a variety of systemic diseases, including a number of hematologic malignancies ( Table 33.1 ).
| Congenital (DBA) | ||
|---|---|---|
| Primary | Autoimmune Idiopathic | |
| Secondary | Thymoma Hematologic malignancies | CLL |
| T-LGL/chronic NK-LGL leukemia | ||
| Myeloma | ||
| NHL | ||
| MDS | ||
| ALL | ||
| Solid tumors | Renal cell carcinoma | |
| Thyroid cancer | ||
| Various adenocarcinomas | ||
| Infections | Parvovirus B19 | |
| EBV, mumps | ||
| HIV, HTLV-1 | ||
| CMV | ||
| Viral hepatitis (hepatitis A, hepatitis B ) | ||
| Leishmaniasis | ||
| Gram-positive systemic infections (e.g., staphylococcemia) | ||
| Meningococcemia | ||
| Autoimmune conditions | SLE | |
| RA | ||
| Sjögren syndrome | ||
| Mixed connective tissue disease | ||
| Autoimmune hepatitis | ||
| Anti-EPO antibodies | ||
| ABO-incompatible BMT | ||
| Minor incompatibility | ||
| Drugs and chemicals | ||
| Pregnancy | ||
| Severe nutritional deficiencies | ||
| Renal failure | ||
The inciting events in the development of PRCA are not known. However, as with idiopathic aplastic anemia, viruses or exposure to chemicals can serve as potential triggers ( Fig. 33.1 ). Theoretically, a viral infection could lead to depletion of erythroid precursors. Studies of B19 parvovirus (discussed later) suggest such an etiology. Because hematopoietic stem cells are not affected by B19 parvovirus, myeloid cells and platelets are normally produced, and upon clearance of the virus, normal erythroid production can resume. Similarly, in immune-mediated PRCA, the mechanism of erythroid inhibition may vary and may include (1) antibodies to proteins specific to erythroblasts, (2) direct cytotoxic T lymphocyte (CTL)–mediated killing of erythroid precursors, and (3) production of soluble products by CTLs such as inhibitory or proapoptotic cytokines that directly affect the erythroid series.
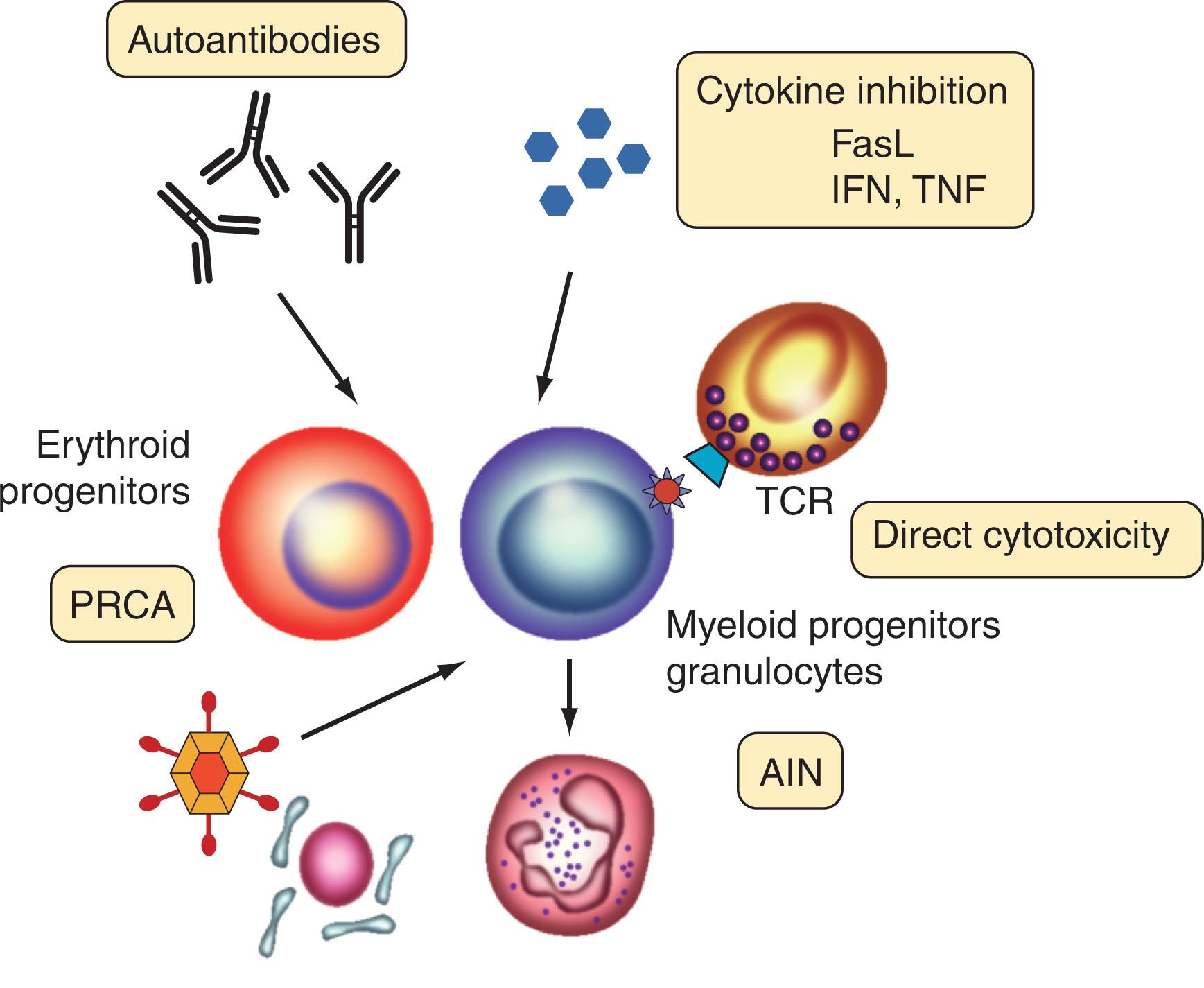
Historically, initial studies concentrated on examining the effects of soluble serum inhibitors of erythropoiesis. These investigations revealed a decline in erythroid colony formation in the presence of patient serum or failure to induce erythroid colony formation in the presence of erythropoietin. Such serum inhibitors can be detected in 40% of patients with PRCA. In 60% of patients, erythroid colony formation can be induced in vitro with hematopoietic growth factors. The inhibitory activity is localized to the immunoglobulin (Ig)G fraction and disappears upon remission. The antigenic targets for autoantibodies have not been well characterized, but various stages of erythroid differentiation can be affected (also called PRCA type A), as seen in the reduction of burst-forming unit–erythroid or colony-forming unit–erythroid. In certain cases of antibody-mediated PRCA, the involvement of the complement system is a prerequisite to disease causation. Perhaps the exception and a model for antibody-induced red cell aplasia is the identification of PRCA associated with anti-erythropoietin antibodies (also called PRCA type B) in rare cases. Consistent with the specificity of the antibodies, myeloid colony formation is not impaired, making it unlikely that a more ubiquitous inhibitory cytokine mediates the specific erythroid inhibition.
Experimental and clinical observations have suggested that PRCA may also be mediated by CTLs, which specifically recognize and kill erythroid precursors similar to CTL-mediated killing of cells in aplastic anemia. Although such a T cell–mediated erythroid response is likely to be polyclonal, rare instances of T-cell large granular lymphocyte (T-LGL) leukemia associated with PRCA or erythroid inhibition may represent an extreme form of the clonal continuum of CTL responses (see T-Cell Large Granular Lymphocyte–Associated PRCA). In addition to CTLs expressing α/β T-cell receptors (TCRs), T cells with a γ/δ TCR can mediate PRCA. The antigens/antigenic peptides triggering such a response have not been well described. However, it has been shown that T-LGLs from PRCA patients are directly capable of suppressing erythropoiesis of CFU-E in vitro. Similarly, natural killer (NK) cells have also been implicated in mediating cytotoxicity directed against erythroid precursors. NK cells, like γ/γ T lymphocytes and unlike α/β CTLs, do not rely on major histocompatibility complex (MHC)–restricted cytotoxicity, but may use killer-cell immunoglobulin-like receptors (KIRs). KIRs inhibit cytolysis when they encounter a cell bearing human leukocyte antigen (HLA) class I molecules. A lack of appropriate KIRs may predispose cells to increased attack by NK cells or γ/δ CTLs. Physiologic downregulation of KIRs has been implicated in the pathogenesis of PRCA in a patient with concomitant γ/δ T-LGL clonal proliferation. An alternative NK-cell cytotoxic mechanism independent of KIR has been reported in healthy individuals.
Peripheral Th lymphocyte polarization has been implicated in the pathogenesis of PRCA. Polarization toward the Th2 functional subtype during disease relapse and normalization of Th1/Th2 ratio after effective treatment has been associated with both monoclonal gammopathy- and thymoma-associated PRCA.
Primary PRCA occurs in the absence of any underlying disorder. It may be acute and self-limited or may be a chronic and refractory condition. Acute forms are uncommon. Most cases are protracted and chronic, unlike TEC, which is an acute and self-limited disorder. Most of the cases of classic primary PRCA are autoimmune in origin, but a significant proportion will remain idiopathic in origin in spite of an exhaustive workup.
In B-cell chronic lymphocytic leukemia (CLL), PRCA can be observed in up to 6% of cases. A recent study found 0.5% of their 1750 CLL patients has PRCA. This diagnosis should be considered in CLL patients who demonstrate anemia and reticulocytopenia. Definite diagnosis requires bone marrow biopsy which will show absence of erythroid precursors and red cell aplasia. The underlying pathogenetic mechanisms are not clear, and the inhibition of the erythroid series does not appear to be mediated by a soluble factor. The distinction between whether the PRCA is a result of the primary B-cell CLL disease or its therapy becomes difficult in circumstances when PRCA presents as a late event. In most cases, PRCA cannot be attributed simply to infiltration of the marrow by lymphoma cells.
Although neutropenia is a typical finding in T-LGL leukemia, PRCA with varying degrees of erythroblastopenia can also be observed in 10% to 68% of patients with T-LGL leukemia, with much higher rates in Asian populations. It is found to be commonly associated with signal transducer and activator of transcription (STAT)3 mutant T-LGL leukemia. In such a setting, PRCA is often accompanied by red cells with an increased mean corpuscular volume. It is possible that PRCA associated with T-LGL leukemia represents an extreme form of the T-cell–mediated disease that, if polyclonal, might be classified as idiopathic PRCA.
Thymoma is associated with PRCA; thus a chest X-ray examination or computed tomographic (CT) scan should be included in the workup for PRCA. Antibodies with direct inhibitory effects against erythroid precursors may be present. T-cell–mediated inhibition of erythropoiesis has also been implicated in the pathogenesis of PRCA associated with either benign or malignant thymomas. A late onset immunodeficiency condition, Good syndrome, which is characterized by hypogammaglobulinemia and thymoma is associated with PRCA in 33% of the patients. Thymectomy is the usual initial treatment approach ; however, incomplete responders, nonresponders, and patients who relapse are common, necessitating additional therapies in the form of azathioprine, intravenous immunoglobulins (IVIg), and cyclosporine A (CsA).
Pregnancy-associated PRCA is a self-limited syndrome that may occur at any age of gestation. It has a high risk for relapse during subsequent pregnancies and can be safely managed with either blood transfusions or corticosteroids. Patients with other forms of PRCA may also be more prone to relapse during pregnancy.
Parvovirus B19 is a single-stranded deoxyribonucleic acid (DNA) virus, which in normal individuals causes fifth disease (erythema infectiosum) in children and arthropathy in adults. It is of particular concern in patients with sickle cell disease. The cellular receptor for the virus is the P antigen, a blood group antigen also responsible for the agglutination reaction that occurs in the presence of the virus. Detection of parvovirus B19–specific IgM without antiparvovirus B19 IgG supports the diagnosis of acute infection, whereas the parvovirus B19–specific IgG suggests immunity. Addition of parvovirus B19 in vitro to cultures of erythroid progenitor cells completely abolishes erythroid colony formation. Primary infection causes lifelong immunity; however, it is possible that a latent virus may persist in a healthy individual for years.
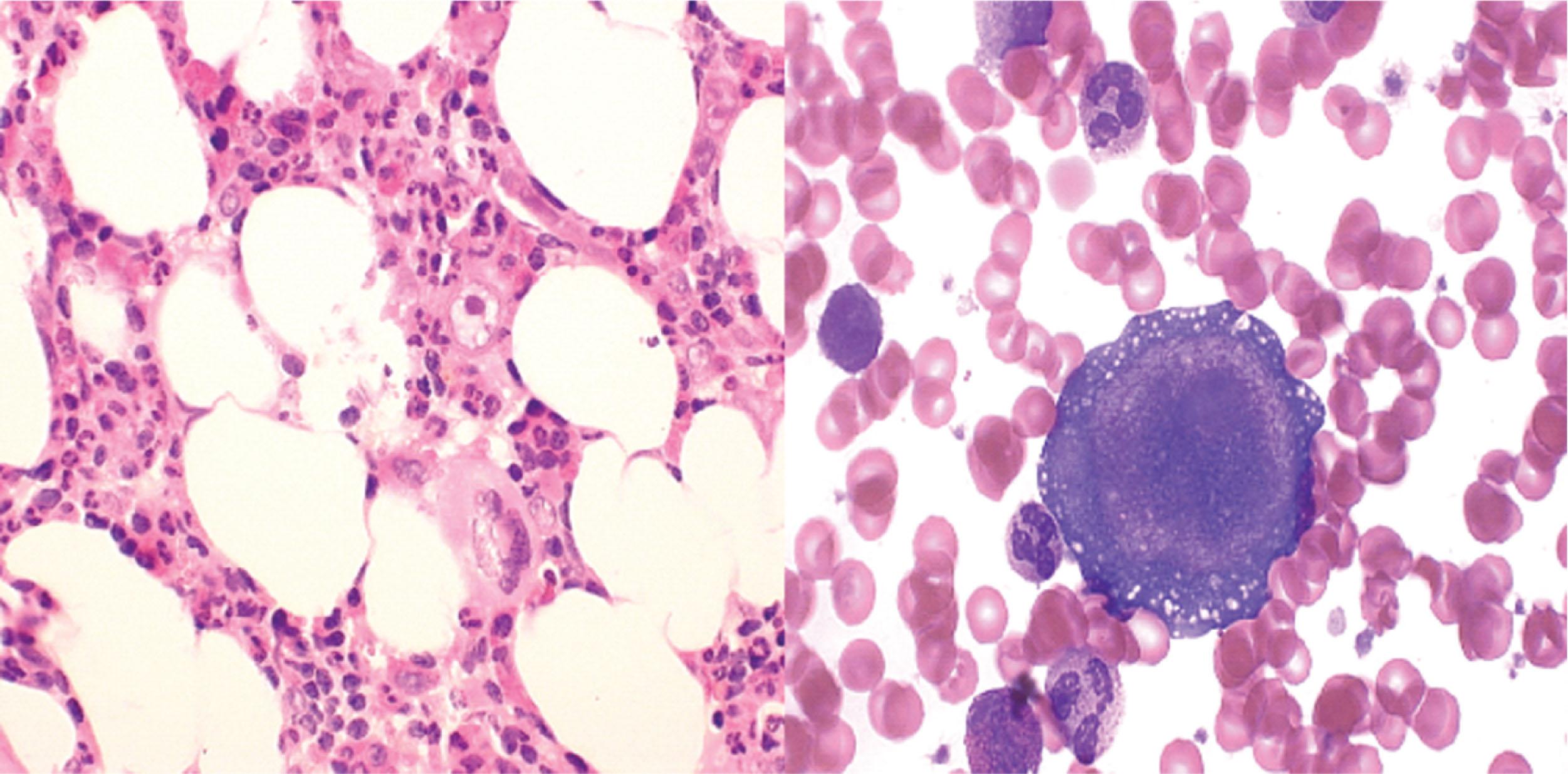
A transient aplastic crisis is a typical complication of a primary parvovirus B19 infection in patients with increased red cell turnover (usually chronic hemolysis, e.g., hemoglobinopathies, and hereditary red blood cell [RBC] membrane disorders, e.g., hereditary spherocytosis). In typical cases, acute reticulocytopenia results in a sudden drop in hemoglobin (Hb)/hematocrit levels as RBC destruction is not supported by a suppressed marrow. Occasionally, characteristic giant pronormoblasts may be seen in marrow aspirates ( Fig. 33.2 ). Aplastic crisis is often self-limiting with the evolution of a protective IgG response. Viral titers in the serum of affected patients may be high.
A more chronic form, parvovirus B19–related PRCA, may develop in immunocompromised patients as, for example, in acquired immunodeficiency syndrome (AIDS) (see Chapter 152 ). In such cases, IVIg can produce remarkable responses. High doses of IVIg are required (>2 g/kg) because an insufficient dose may not produce the desired effect. DNA dot blot hybridization is the best diagnostic test for the detection of viremia. Parvovirus B19 can also be detected by polymerase chain reaction (PCR), a routinely available test, but this method may provide a high rate of false-positive results. However, if negative, it excludes B19 parvovirus–mediated disease. Improved tests have been developed that allow for the detection of neutralizing antibodies and infectivity of parvovirus B19.
Several other viral infections, including viral hepatitis (A and C ), Epstein-Barr virus (EBV), cytomegalovirus (CMV), human T-Lymphotropic virus (HTLV)-1, and human immunodeficiency virus (HIV), have been implicated as causative agents of PRCA. Little is known about the exact mechanisms underlying these disorders, but they likely involve T-cell–mediated suppression as observed during HTLV-1 infection and EBV or antibody-mediated destruction of RBC precursors, as in hepatitis C–induced PRCA. Frequently the presence of multiple comorbidities and medications makes it difficult to isolate the causative agent of PRCA.
The majority of connective tissue diseases associated with PRCA are autoimmune in nature. Several rheumatologic diseases have been associated with PRCA, including adult-onset Still disease, dermatomyositis, mixed connective tissue disease, polymyositis, rheumatoid arthritis, Sjögren syndrome, and systemic lupus erythematosus. The pathogenesis of the PRCA in this setting may vary and includes autoantibody-mediated erythroid inhibition, autoantibody directed against erythropoietin, and CTL-mediated killing of erythroid precursors.
Various chemical agents and drugs have been associated with PRCA. The mechanisms responsible for erythroid inhibition may be diverse depending on the offending agent ( Table 33.2 ) but may include induction of antibodies targeting the drugs or drugs bound to cellular and plasma proteins. Another possible mechanism involves drug-mediated triggering of T-cell responses, or direct toxicity to the erythroid series as seen with diphenylhydantoin.
|
|
Recombinant erythropoietin is used in the treatment of anemia of various origins, including anemia of chronic disease, renal disease, and a variety of bone marrow failure syndromes, particularly myelodysplastic syndromes (MDS). Cases of PRCA have developed as a consequence of antibody formation against endogenous erythropoietin or while receiving treatment with recombinant erythropoietin. The latter condition has been referred to as epoetin-induced PRCA or EPO-PRCA with initial cases related to exposure to epoetin alpha (Eprex; 92%) and epoetin beta (NeoRecormon; 8%). There are reports of human erythropoietin (HuEpo) neutralizing antibody PRCA related to the use of biosimilar recombinant HuEpo in Thailand. There are several risk factors associated with the development of EPO-PRCA, including subcutaneous (SC) route of administration, use of epoetin alpha stabilized in a human serum albumin (HSA)–free formulation, use of silicone oil as lubricant in prefilled Eprex syringes, and use in patients with chronic renal disease. This observation has led to modification in the storage, handling, and administration of Eprex favoring IV administration, especially with Eprex stabilized with HSA-free formulation, and avoidance of the SC non-HSA–stabilized Eprex. Diagnostic criteria have also been proposed incorporating major features (treatment with epoetin for at least 3 weeks, decrease in Hb by 0.1 g/dL/day without transfusions or transfusion requirement of about 1 unit/week to keep Hb levels stable, reticulocyte count less than 10 × 10 9 /L, no major drop in other blood lineages), minor features (skin and systemic allergic reactions), and accessory investigations to exclude other causes. The most commonly used tests to detect antibodies are enzyme-linked immunosorbent assay, radioimmunoprecipitation assay, and surface plasmon resonance. Once antibodies are detected, their neutralizing ability is tested using an in vitro bioassay. Following establishment of diagnosis, management should include discontinuation of exogenous erythropoietin, administration of immunosuppressive agents, or, in cases of anemia secondary to renal insufficiency, renal transplantation.
In contrast to HLA matching, ABO blood group incompatibility plays a minor role in the success of allogeneic hematopoietic stem cell transplantation (HSCT). However, PRCA may be associated with major ABO incompatibility between the donor and recipient, leading to inhibition of donor erythroid precursors by residual host isoagglutinins. This complication is more commonly observed following the use of nonmyeloablative conditioning regimens. PRCA may also be resistant to the withdrawal or decrease of immunosuppression, or donor lymphocyte infusions. Responses to rituximab, erythropoietin, plasma exchange, and azathioprine have been reported. A case responsive to a purified CD34 + cell infusion has also been reported. Multiple cases of successful treatment with daratumumab (IgG1k monoclonal antibody directed against CD38) have also been reported. Resolution of PRCA is generally associated with a decrease and subsequent disappearance of host isoagglutinins.
Immune dysregulation, polyendocrinopathy, enteropathy, X-linked (IPEX) syndrome is a rare X-linked recessive condition typically seen during infancy. Clinical features may include type 1 diabetes mellitus, eczema, and autoimmune hepatitis. Anemia can be severe at diagnosis because the fall in Hb occurs over a protracted period of time and patients often exhibit a good degree of adaptation. Arrest of erythropoiesis is obvious with a profound reticulocytopenia.
A complete blood cell count with differential, peripheral smear review, reticulocyte count, and a bone marrow examination remain the cornerstone in the diagnosis of PRCA. The classic hematologic picture of PRCA includes a normocytic, normochromic anemia (anemia associated with T-LGL leukemia is often macrocytic) with a normal white blood cell and platelet count. The reticulocyte count is reduced to less than 1% when corrected for the degree of anemia (a reticulocyte level greater than 2% is not compatible with the diagnosis of PRCA) ( Fig. 33.3 ).
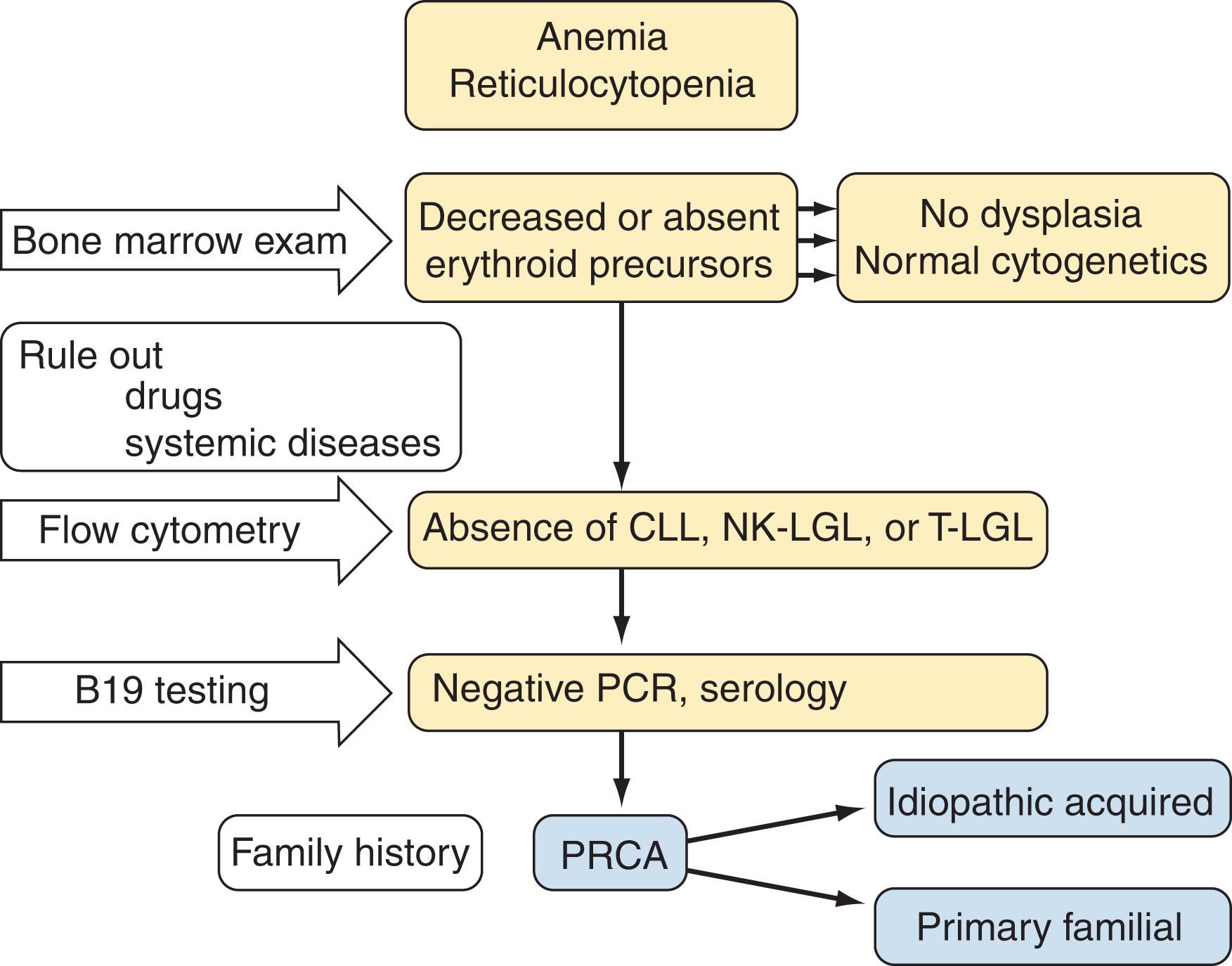
The bone marrow examination generally shows absence of cells belonging to the erythroid lineage and the normal appearance of granulocytic and monocytic precursors and megakaryocytes. Erythroid precursors, if present, are usually less than 1%, and only a few residual proerythroblasts or basophilic erythroblasts may be seen. Blast cell numbers and cellularity are within normal limits. There are no dysplastic changes, ringed sideroblasts, or reticulin fibrosis. Cytogenetic evaluation is normal. In some cases, neutropenia, mild thrombocytopenia, eosinophilia, thrombocytosis, leukocytosis, or relative lymphocytosis may be seen. Cytogenetic abnormalities, if present, may indicate concomitant MDS and is a poor prognostic marker for both response to treatment and propensity to leukemic transformation. During the course of PRCA patients, ineffective erythropoiesis characterized by a maturation arrest at the proerythroblast or basophilic erythroblast stage may be observed and signifies either partial response to treatment or initial recovery from treatment or a prelude to the development of full-blown PRCA.
It is important to exclude vitamin B 12 and folate deficiencies, and depending on the etiology and associated disease, other blood and bone marrow findings may be seen. The presence of giant and vacuolated pronormoblasts in the bone marrow examination should raise the suspicion for parvovirus B19 infection. The presence of large granular lymphocytosis, neutropenia, and/or thrombocytopenia, expansion of CD3 + CD8 + CD57 + T cells, clonal cytotoxic T cells as documented by TCR gene rearrangement, expansion of specific TCR Vβ region family gene segment, and splenomegaly may point toward concomitant T-LGL leukemia. B-cell lymphocytosis, especially of the CD5 + /CD19 + /CD20 + /CD23 + /cyclin D − /SmIg −dim phenotype with concomitant lymphadenopathy, hepatosplenomegaly, hypogammaglobulinemia, and thrombocytopenia may be very suggestive of a B-cell CLL. Another laboratory finding that may help point to a secondary cause of PRCA includes the presence of monoclonal gammopathy. Parvovirus B19 DNA titers (DNA hybridization and amplification techniques) may show high levels of the virus at 10 genome copies per milliliter, but it is important to note that serologic (IgM and IgG) titers are usually absent. Erythropoietin antibodies, antinuclear antibodies, and/or complement consumption may point toward a specific disease mechanism. A radiographic workup may also be useful in the clinical workup because chest X-ray examination or CT scan may show evidence of a thymoma.
PRCA can be easily differentiated from aplastic anemia and other types of bone marrow failure syndromes. A distinction between MDS with erythroid hypoplasia and idiopathic PRCA may be more difficult. In childhood, TEC has to be distinguished from DBA, but a history of normal blood counts, late onset of manifestations, and a transient disease course are characteristic of TEC.
The distinction between primary and secondary forms of PRCA is essential because many secondary types have specific and very effective therapies ( Table 33.3 ). All potentially offending drugs should be discontinued, and drug-associated PRCA should remit within 3 to 4 weeks. Nutritional deficiencies (B 12 and folic acid) should be excluded and treated if present. The therapy of primary and secondary forms of PRCA refractory to the treatment of an underlying disease may be challenging and should include a sequential trial of various immunosuppressive agents until a response is achieved. Spontaneous remissions have been reported.
| Agent | Study | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Chikkappa | Means | Au | Dessypris | Zecca | Lacy | Charles | Sloand | Abkowitz | |
| Steroids | 18/41 | 9/29 | 9/36 | — | |||||
| Cytotoxic agents | 24/54 | 14/29 | 8/27 | — | |||||
| Antithymocyte globulin | 2/6 | 0/1 | 8/12 | 6/6 | |||||
| Cyclosporine A | 6/7 | 6/9 | 3/4 | 4/5 | 2/3 | ||||
| Splenectomy | 4/23 | 0/1 | 0/1 | ||||||
| Daclizumab (Zenapax) | 6/15 | ||||||||
| Rituximab | 1/1 | ||||||||
| Alemtuzumab (Campath) | 2/2 | ||||||||
| Methotrexate | 2/37 | ||||||||
In cases associated with thymoma, thymectomy is the usual initial treatment of choice before immunosuppression and may induce remission with return of erythropoiesis in 4 to 8 weeks in about 30% to 40% of patients. Patients who fail to respond to surgery should be treated as patients with idiopathic PRCA. The removal of a thymoma may improve responsiveness to immunosuppressive therapy. Thymectomy in the absence of a thymoma in other forms of PRCA is not recommended. In circumstances where surgical resection of thymoma is contraindicated, radiation therapy with or without chemotherapy may be administered.
Supportive care includes blood transfusions and iron chelation with deferasirox (Exjade) which is an oral iron chelator developed for treating transfusion-related iron overload syndromes.
Prednisone therapy is associated with significant response rates (approximately 40%) and should constitute the initial therapeutic approach. Initial responses are generally observed after 4 to 6 weeks. A slow taper of prednisone is suggested over a period of 3 to 4 months. The disease may relapse, and the minimal maintenance dose of corticosteroids may need to be established to maintain the desired Hb levels. Trials of prednisone therapy without clinical response longer than 8 weeks are not warranted.
Alternative therapies may include cyclosporine, oral cyclophosphamide, azathioprine, antithymocyte globulin (ATG), rituximab, and alemtuzumab (see Table 33.3 ). Erythropoietin and darbepoietin are usually not effective as a sole agent but may hasten recovery following an adequate trial of cyclophosphamide. No randomized trials exist to favor a particular treatment based on efficacy. The choice of therapy may be influenced by clinical clues. For example, the presence of LGLs may suggest the use of cyclophosphamide or CsA, hypogammaglobulinemia may be corrected with IVIg, whereas detection of hypergammaglobulinemia or monoclonal protein may suggest a choice of rituximab. Most refractory cases may require administration of ATG. The age of the patient may influence the choice of the cytotoxic agent, which may pose a significant risk for the development of secondary leukemias, especially with a prolonged administration.
Danazol is a synthetic attenuated androgen that has been used for many years for the treatment of a variety of hematologic disorders, mainly myelofibrosis. Danazol is given at 200 mg orally (PO) twice per day up to 600 mg daily. It has been used in combination with steroids or other agents and has shown efficacy in PRCA secondary to multiple etiologies.
IVIg is also effective in several types of PRCA. Higher doses of usually 2 g/kg of IVIg for 5 days are necessary for the treatment of parvovirus B19 virus–induced PRCA. In AIDS patients with parvovirus B19 virus–induced PRCA, a regimen consists of induction therapy with 1 g/kg daily for 1 to 2 days followed by 1 g/kg for 2 days.
Azathioprine is an imidazolyl derivative of mercaptopurine that inhibits DNA synthesis by inhibition of purine metabolism. In PRCA, it may be given at a dose of 2 to 3 mg/kg/day IV and has been found to be effective in patients nonresponsive to cyclophosphamide.
Oral cyclophosphamide may be started at a dose of 50 mg orally (PO) daily, with a maximal dose of no more than 150 mg daily. Blood counts should be monitored, and the dose may be escalated accordingly. Trials of therapy longer than 3 months without signs of response are not warranted. Monitoring of the reticulocyte count may allow for the early assessment of response. Often, a delayed response may be seen when cyclophosphamide is withdrawn, reflective of balance between immunosuppression and cytotoxicity. It has been shown to be efficacious in combination with CsA in T-LGL-associated PRCA.
Rituximab given by IV infusion weekly for 4 weeks has been found to be efficacious in PRCA. PRCA in a variety of settings, including B-cell CLL, EBV-associated posttransplant lymphoproliferative disease, ABO-incompatible allogeneic HSCT for acute myeloid leukemia, and hairy cell leukemia variant, has been successfully treated with rituximab. In cases refractory to immunosuppressive agents affecting T-cell function, rituximab or low-dose alemtuzumab constitute a reasonable option. Rituximab is effective in patients with PRCA owing to ABO incompatibility following HSCT.
CsA can be administered at a dose of 5 to 10 mg/kg PO daily in divided doses. CsA can be combined with prednisone at doses of 20 to 30 mg PO. The trough levels of CsA should be monitored. An adequate trial of therapy is considered 3 months of therapy. The response rates may be as high as 60% to 80%. After a response is achieved, the therapy should be continued for 6 months followed by a slow taper.
Horse ATG may be given to refractory cases at a dose of 40 mg/kg IV daily for 4 days with prednisone at 1 mg/kg. Concomitant prednisone should be administered and then tapered over 2 to 3 weeks. A therapeutic response should occur within 3 months post-therapy, although responses at or beyond 6 months may be observed.
Methotrexate (MTX), an antimetabolite, at low doses (7.5 to 15 mg/week PO) is useful in treating PRCA, especially in patients with concomitant LGL leukemia. The responses are generally sustained, and therapy is well tolerated. MTX may be given in conjunction with other therapies like cyclophosphamide or CsA.
Alemtuzumab (Campath, anti-CD52 monoclonal antibody) is a recombinant DNA–derived humanized monoclonal antibody directed against the cell surface glycoprotein CD52, which is expressed on the surface of normal and malignant B and T lymphocytes. It is currently approved for multiple sclerosis and available on compassionate use for other indications. Former IV dosing has been replaced by SC administration (initial dose of 3 mg, and subsequent doses at 10 mg once or twice weekly). The usual cumulative dose before response is around 50 to 100 mg. Alemtuzumab has been tested in a variety of lymphoproliferative disorders, including B-cell lymphomas (BCLs) and T-LGL leukemia. Similarly, PRCA occurring in the context of these conditions previously unresponsive to other therapies has been shown to be responsive to this agent.
Daratumumab (Darzalex, anti-CD38 monoclonal antibody) is an IgG1k human monoclonal antibody directed against the cell surface glycoprotein CD38 expressed on many immune cells, including plasma cells. It is currently approved for treatment of refractory multiple myeloma (see Chapter 91 ). It has been shown to have efficacy in multiple case reports in refractory PRCA secondary to ABO mismatched allo-HSCT.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here