Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
This chapter includes an accompanying lecture presentation that has been prepared by the authors: ![]() .
.
Topectomy/lesionectomy is an excellent procedure for the treatment of drug-resistant focal epilepsy when the epileptogenic focus can be isolated
Intraoperative electrocorticography (ECoG) provides real-time feedback to improve maximal safe epileptogenic focus resection
Preoperative planning with anesthetic considerations is critical to ensure minimal disruption of intraoperative ECoG findings
Electrocorticography (ECoG) is a critical tool in the epilepsy surgeon’s arsenal, enabling the identification of regions of significant epileptogenicity or identifying areas where provoked epileptiform activity during cortical stimulation can be used to guide a focused resection—a lesionectomy. In this chapter, we discuss the role of ECoG and how it can guide and tailor surgical resection. We cover the history of ECoG-guided lesionectomy, anesthetic protocols for ECoG, the role of ECoG in functional mapping, and how to harness ECoG in real time to influence resection decisions during topectomies and lesionectomies.
Krause, Kocher, and other neurosurgical pioneers identified a link between local brain injury (cranial trauma) and an increased incidence of epilepsy in the 1880s. Initially, they postulated that this was caused by CSF pressure on the cortical surface, with the damaged dura thought to contribute to the initiation and progression of seizures. This hypothesis led to initial operations consisting of trephination without direct resection of the cortex, and in some series, these operations did not even include incision of the dura. Although overall mortality from trephination was high (∼10% to 14%), Krause identified an association between focal Jacksonian motor seizures, visible lesions, and the advent of epilepsy.
The first description of targeted epileptogenic focus resection was a case series of three patients in whom a lesionectomy by Horsley led to a complete resolution of epilepsy. The modern era of neurophysiology is a direct result of an interdisciplinary collaboration between neurophysiologists and neurosurgeons. In 1909, Harvey Cushing capitalized on advances in animal models and initial human stimulation studies by David Ferrier and Robert Bartholow. , He demonstrated that intraoperative stimulation of the postcentral gyrus leads to sensory sensations in the contralateral hand. A new milestone in epilepsy surgery was a consequence of World War I. Ottfried Foerster, a neurologist turned neurosurgeon, utilized galvanic cortical stimulation in war veterans with epilepsy from penetrating cerebral injuries to identify epileptogenic scarred cortex that he then resected, with an improvement in epilepsy. A young Wilder Penfield, funded by the Rockefeller Foundation, traveled to Germany to learn the techniques of stimulation mapping from Foerster. Their work together led to the description of cortical scar and the process of excision using subpial techniques providing for a cure of the epilepsy. These surgical techniques of subpial resection of lesions described by Penfield have been the backbone of epilepsy surgery and have also been extended to the resection of gliomas.
Electrocorticography in humans was first described in 1924 by Hans Berger in a patient with a skull defect. The technique was developed and refined for intraoperative assessment by Penfield and Herbert Jasper at the Montreal Neurological Institute to enable the detection of epileptogenic foci. They combined cortical electrical stimulation with electroencephalogram (EEG) recording for intraoperative localization of epileptic brain tissue. , The cortex was stimulated to evoke the patient’s habitual aura and to guide resection. This combination of invasive EEG (i.e., intraoperative ECoG) and direct cortical electrical stimulation led to improved localization of the cerebral lesion, a crucial advance given that available neuroimaging at the time was radiography and pneumoencephalography. Jasper identified “random spikes” generated by epileptogenic lesions in the brain and delineated how electrical stimulation independent of patient-reported auras or overt seizures could be used to guide intraoperative decision making. ,
Advances in EEG with digital acquisition and storage led to the use of simultaneous prolonged video and invasive EEG to record a patient’s habitual seizure as the standard for localizing epileptogenic brain. In addition, with the emergence of CT and MRI, the utilization of intraoperative ECoG declined as a result of improved preoperative diagnosis and localization of lesional and epileptogenic tissue. Recent advances and developments in PET, ictal single-photon emission computed tomography (SPECT), and magnetoencephalography (MEG) have further facilitated the noninvasive identification of focal epileptogenic brain. However, despite these advances, intraoperative ECoG continues to have a well-defined role in the neurosurgeon’s toolbox for epilepsy surgery.
Epilepsy has a prevalence of 0.8% to 1.2% in the population and is the second most frequent chronic neurologic disorder. Despite significant advances to the medication arsenal for epilepsy, approximately 30% to 40% of patients have drug-resistant epilepsy. After treatment failure with two appropriate drugs with therapeutic serum levels, only 3% of these patients eventually become seizure-free with additional medical therapy trials alone. , As such, surgical management should be explored in such patients given the low probability of therapy success with additional medications. However, less than 1% of such patients the United States are referred to epilepsy centers. The average delay between the diagnosis of refractory epilepsy and surgery is greater than 20 years. The best prognostic factors that predict favorable outcomes in cases with drug-resistant epilepsy are a discrete structural lesion on MRI, location in an area that can be safely excised, concordance with EEG localization, and consistent seizure semiology to that area.
The indications for intraoperative ECoG have significantly evolved over the past century. ECoG remains widely used in 60% to 70% of epilepsy centers in North America. As a result of intraoperative time constraints and pragmatic issues with seizure induction in the operating room, ictal activity is not commonly provoked, and thus interictal epileptiform activity is predominantly utilized to identify the epileptogenic zone. Intraoperative ECoG is used in two contexts: (1) to optimize resection margins, with post-resection recordings used to assess the completeness of resection and (2) to detect afterdischarges (rhythmic transient epileptiform activity induced by the stimulation) during functional mapping of eloquent cortex during cortical stimulation.
The conceptual aspects of intraoperative ECoG have not changed significantly since initial development in the 1930s. ECoG electrodes placed on the cortical surface yield signals with excellent spatial and spectral resolution compared with scalp EEG. Historically, ball-shaped carbon-tip electrodes (usually 16 to 20) attached to a Montreal or Medusa frame were individually placed over the cortical region of interest. This frame allowed for fine adjustment of the distance between contacts and continued access to the cortex for concomitant functional mapping. These frames have mainly been replaced with a flexible disposable grid or strip electrodes that are quick and easy to place over a large region of the exposed cortex. ECoG recordings are recorded, digitized, and concurrently displayed on a computer screen in the operating room for interpretation by the surgeon and neurophysiologist. The background ECoG represents the basal cortical electrical activity and is similar to scalp EEG, but without the dura, skull, and scalp attenuation. ECoG signals are highly variable, with a wide range of spectral content spanning DC to ∼600 Hz. The power spectral density of ECoG shows spectral peaks of characteristic oscillation and broadband 1 over frequency dependence , and can vary significantly with the brain region. More recently normal ECoG, recorded from patients with epilepsy but outside the seizure generating regions, has been published. ,
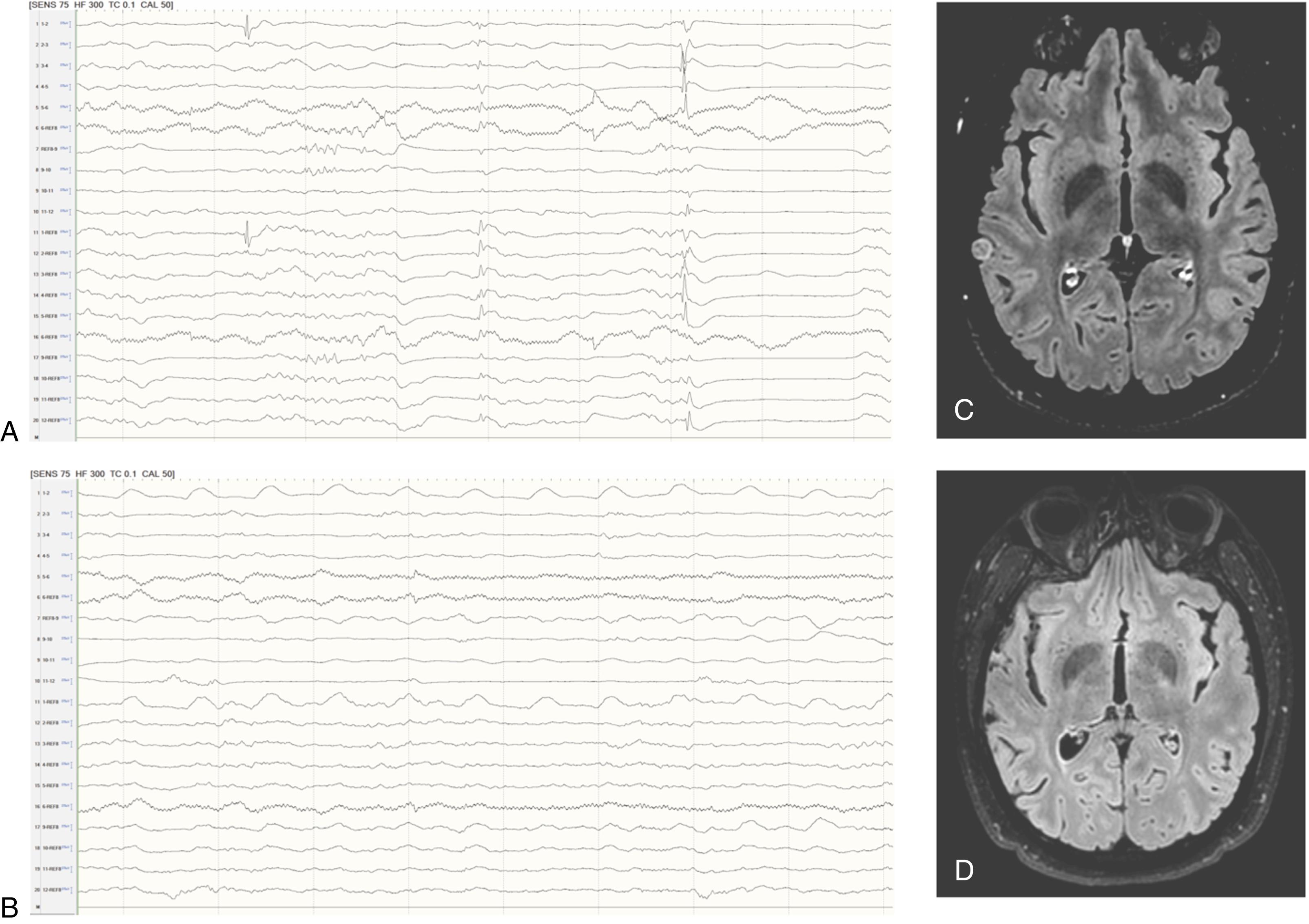
Intraoperative ECoG generally lasts for a short duration (typically 15 to 30 minutes); thus it is rare to capture a spontaneous seizure (ictal event) during these recordings and usually only spontaneous interictal epileptiform activities are detected. Lesional tissue (scar/sclerosis) may manifest as low-frequency high-amplitude activity (also known as slowing ), interictal spikes, polyspikes, sharp waves, spikes-and-wave, sharp-and-slow wave complex, pathologic high-frequency activity, or any combination ( Fig. 91.1 ). The presence of such pathologic interictal patterns have a high positive predictive value for the diagnosis of epilepsy, but caution is required in interpretation for those with prior neurosurgical procedures, other neurological disorders, and pharmacologic therapy. , These interictal epileptiform activities generally represent the area around the epileptogenic focus. Furthermore, in some cases, the morphology of these discharges can help determine the distance of the recording from the focus (higher amplitude equates to a closer recording site to the focus). In some specific lesions, unique ECoG signatures can be detected, for example, with cortical dysplasia. After surgical resection, especially in the extratemporal locations, ECoG is used to guide resection completeness by assessing residual epileptiform activities ( Fig. 91.2 ). This strategy does have a limitation in that the distribution of interictal spike activity may be significantly larger than the epileptogenic zone and should be interpreted in the context of other data in the individual patient.

Interestingly, early studies have found that ECoG-guided surgical resections did not improve surgical outcome. , However, later studies have suggested that this lack of correlation is partly caused by the surgical resection not being tailored to intraoperative ECoG findings. , Furthermore, ECoG in MRI normal temporal lobe epilepsy surgery found that complete resection of brain regions generating interictal epileptiform discharges on baseline intraoperative ECoG were associated with excellent outcomes. Studies have demonstrated that in some instances, ECoG has a clear benefit by allowing for real-time feedback with a refinement of surgical resection boundaries.
Anesthesia has a significant influence on intraoperative ECoG. Although initial studies by Penfield and Foerster utilized rudimentary anesthesia and in some cases only local anesthetic, anesthesia protocols and choice of agents have undergone significant advances with increased understanding of interactions between anesthetics and cerebral activity. Most anesthetic drugs affect neuronal activity and lead to substantial excitatory or inhibitory effects on cerebral activity. ECoG is altered by different anesthetic levels, so it is critical to maintain a stable anesthetic depth during intraoperative ECoG. With light anesthesia, the most common finding is high-frequency, low-amplitude waves. With increased depth of anesthesia, α waves (8 to 12 Hz) become dominant, and with increasing anesthesia depth, they are replaced with high-frequency β activity (13 to 30 Hz). Finally, as sedation continues to increase, high-amplitude low-frequency ϴ waves (5 to 7 Hz) and δ waves (1 to 4 Hz) develop. Lastly, the ECoG becomes burst-suppressed or isopotential. There are significant institutional variations in the choice of agents utilized for ECoG; however, common guidelines and our thought process regarding anesthesia protocol are described in the following text.
Premedication benzodiazepines should be avoided in all cases because of the risk for disrupting baseline findings and significant difficulty in obtaining reliable ECoG findings. Propofol is a short-acting agonist of type A gamma-aminobutyric acid (GABA) receptors and a blocker of N- methyl- d -aspartate (NMDA) receptors, leading to global CNS depression. Propofol affects ECoG in a dose-dependent fashion, with lower doses accentuating β activity that can mimic or mask epileptiform spikes. The short duration of action of propofol allows it to be eliminated simply by turning off the medication. This rapid cycling profile allows for the “asleep-awake-asleep” process for awake procedures. Inhalational anesthetics act to potentiate GABA and inhibit nACh and glutamate receptors. These inhaled agents are commonly utilized for maintenance of general anesthesia; however, inhaled agents can influence ECoG properties. For example, in some studies, sevoflurane was found to suppress epileptiform activity, whereas in other cases it promoted widely distributed and nonlocalizable epileptiform activity. , Dexmedetomidine is an α 2 adrenoceptor agonist that has anxiolytic, analgesic, and sedative properties. This medication has an excellent safety profile with no known interference with epileptiform activity. Dexmedetomidine also has minimal effects on hemodynamic stability, reduces rates of perioperative tachycardia, and has minimal impact on respiratory drive. Opioids act through the mu-opioid receptor and at low doses, confer no effect on background or spike detection; however, higher doses activate interictal epileptiform activity. Opioids are primarily utilized because of their synergistic effects, leading to a reduced need for other anesthetic agents despite the risk for increased interictal activity. Pharmacologic activation of interictal activity and seizures using opioid agonists for diagnostic purposes in epilepsy surgery has been postulated and may prove useful; however, the specificity of the response for accurate mapping of epileptogenic brain in temporal lobe epilepsy was not successful. ,
If no spontaneous interictal discharges are elicited, iatrogenic activation using electrical stimulation may isolate the lesion of interest. Furthermore, in patients with multifocal discharges, activation can promote organization and propagation of discharges to help identify the focus. After an iatrogenic activation, several responses can occur including (1) run of interictal epileptiform discharges, (2) electrographic seizure, or (3) electroclinical seizures. Electrically induced seizures are a good indicator of abnormally increased baseline excitability. If intraoperative seizures occur, they are typically focal seizures related to the cortical stimulation and will spontaneously resolve after discontinuing the stimulation. In the event of continued seizures, sterile ice-cold saline solution administered to the cortex should be the first-line therapy because of a shorter suppression effect on the subsequent recording. Intraoperative generalized tonic-clonic seizures are much less frequent; however, if ice-cold saline solution does not stop the seizures, aggressive treatment must be prepared with small boluses of propofol (10 to 50 mg), benzodiazepines (midazolam 2 to 5 mg), or thiopental sodium (25 to 50 mg). However, these intravenous anesthetic drugs may suppress interictal activity and interfere with future recordings.
With an increased understanding of anesthetic regimens limiting potentially catastrophic seizures, stimulation can be harnessed to interrogate different regions of the brain for mapping eloquent areas of the brain. This mapping can further delineate resection guidelines intraoperatively, promoting maximal epileptogenic focus removal while preserving critical eloquent tissues.
Functional mapping is accomplished with intraoperative cortical stimulation to localize eloquent cortex areas, which, when disrupted, leads to a clear neurologic disability including language, motor, sensory, or visuospatial deficit. The precentral and postcentral gyrus location is commonly identified by somatosensory evoked potential (SSEP) phase reversal over the central sulcus, allowing for maximal removal of the lesion and minimizing postoperative functional deficits. A patient is typically awake to minimize the effects of the anesthesia; however, motor mapping can be achieved while patients are under sedation. Cortical stimulation involves directly applying a series of electrical impulses to the cortex and monitoring clinical response. Stimulation is typically via a biphasic, constant-current, balanced square-wave stimuli with increasing amplitude and closely spaced electrodes in a bipolar fashion. Throughout this process, ECoG is utilized to monitor for afterdischarges to detect and help avoid inducing seizures. The process of cortical mapping will allow for a map of the eloquent cortex to shape the surgical resection strategy.
Cortical surface SSEPs help localize the sensorimotor cortex intraoperatively. SSEPs with mirror-image waveforms are found on either side of the central sulcus. Interpretation is typically based on several features, including the maximum N 20 amplitude, phase reversal of N 20 -P 20 across the central fissure, and the presence of small negative potentials leading up to the N 20 . , Unlike other methods of functional mapping, intraoperative SSEPs can be performed while the patient is under general anesthesia.
In general, cortical stimulation to assess eloquent motor function is through direct visualization; however, EMG electrodes can be used to supplement observation for more subtle findings. Limited pulse bursts can be utilized to map motor function, a technical consideration that will help minimize induced seizures. Sensory function can be mapped at multiple sites in the brain including the postcentral gyrus, the secondary sensorimotor region in the parietal operculum, and the mesial frontal cortex in the supplementary sensorimotor area.
Resection in the nondominant hemisphere can be conducted in front of the precentral gyrus. Resection of the precentral motor cortex is generally only preferred when there is already substantial preoperative contralateral paresis. Resection of the postcentral sensory cortex in the arm or leg can cause significant proprioceptive deficits; however, the face can typically be resected without substantial consequences. In the nondominant hemisphere, the parietal cortex posterior to the postcentral gyrus can be removed; however, in the dominant hemisphere, the parietal lobe should be limited to only the superior parietal lobule because of the risk for damaging language, resulting in a Gerstmann syndrome.
Language mapping is critical for eloquent language as, despite advances, fMRI can mistake participating regions of the cortex from essential language regions. Language mapping with cortical stimulation is the current “gold standard,” with stimulation lasting for 3 to 5 seconds to assess language tasks. Speech arrest, anomia, paraphasias, and perseverations are considered positive findings, including impaired tongue motor response (lack or excessive motion) or afterdischarges.
Anatomic considerations for language include the Broca speech area, which is anatomically located within the opercular, inferior frontal gyrus. The parietal speech area is 1 to 4 cm above the Sylvian fissure and 2 to 4 cm behind the postcentral sulcus. Temporal speech areas extend posteriorly behind the postcentral sulcus and 2 to 3 cm behind the Heschl gyri. The Wernicke area does not have definite anatomic features; thus language mapping is critical for dominant-hemisphere resections.
Ultimately, functional mapping helps provide further understanding and real-time feedback in identifying eloquent areas, especially as studies with masses or epileptogenic lesions in an eloquent area did not have a traditional cortical language region. These disruptions were significant enough that the language site could be localized with surgical exposure in only 58% despite successful and safe resection. Unlike the considerable advancements in localization and refinement of epileptogenic focus, complete with the identification of eloquent adjacent tissues, the methodology of surgical resection has not significantly changed in the past century.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here