Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The gallbladder and extrahepatic bile ducts show a limited spectrum of inflammatory and neoplastic disorders, but these disorders are significant because they affect a large proportion of the world’s population. The most common (>95%) is cholelithiasis. Inflammation in the gallbladder secondary to stones presents either as acute or chronic cholecystitis and may lead to significant complications such as empyema, perforation, or fistula. Carcinomas of the gallbladder are uncommon and arise from flat, polypoid or cystic precursor lesions and may sometimes be detected incidentally in patients undergoing a routine cholecystectomy. The recent World Health Organization (WHO) classification has proposed a new nomenclature for these precursor lesions to align them with precursors seen elsewhere in the pancreaticobiliary tree. Stage is the most important prognostic factor, and the 5-year survival rate is dismal because most cases are at an advanced stage at initial presentation or have multifocal biliary dysplasia.
Cholecystitis presents with intermittent postprandial epigastric or right upper quadrant pain. By far the most common underlying cause is cholelithiasis, which in some cases may also lead to obstruction of the bile duct (choledocholithiasis). Acute cholecystitis is also associated with fever and leukocytosis. Clinical examination is supported by a positive “Murphy sign” in which pain is elicited when the inflamed gallbladder descends during inspiration. The clinical impression may be confirmed by ultrasound, which demonstrates choleliths, gallbladder wall thickening, and pericholecystic fluid. Xanthogranulomatous cholecystitis may show mural nodularity and dense adhesions to adjacent organs, which may cause clinical concern for malignancy.
In 0.5% to 1% of cases, a porcelain gallbladder, characterized by diffuse calcification of the wall, is seen radiographically and intraoperatively. This finding correlates with the pathologic diagnosis of hyalinizing cholecystitis (HC) and has classically been associated with an increased risk of gallbladder carcinoma. This risk has traditionally been considered sufficient to warrant prophylactic cholecystectomy, but recent studies have shown the risk to be lower than previously reported.
Sterile acalculous cholecystitis is much less common, and most patients present with multiple other comorbidities, especially in the hospital setting. It is most commonly associated with ischemia and dysmotility. Infectious cholecystitis is rare, occurring predominantly in immunocompromised patients. The most common infections are Cryptosporidium parvum and cytomegalovirus. Rare cases of cholecystitis represent manifestations of systemic diseases, including eosinophilic cholecystitis, presenting as a component of eosinophilic gastroenteritis, primary sclerosing cholangitis (PSC)–associated cholecystitis, and immunoglobulin (Ig) G4–associated sclerosing cholecystitis, which is present in almost all patients with IgG4 sclerosing cholangitis of the bile duct.
Acute cholecystitis is characterized by mucosal erythema, friability, and ulceration. The gallbladder wall may be thickened and edematous. In severe cases, serositis may be present with a fibrinous exudate on the serosal surface. Chronic cholecystitis most often exhibits mural fibrosis with a thick and firm gallbladder wall. Extensive hyalinization and calcification (>80% of the circumferential wall) is classified as porcelain gallbladder. Xanthogranulomatous cholecystitis may be associated with mural nodules that can grossly mimic malignancy ( Fig. 15.1A ). Cholesterolosis, which is found in approximately 20% of cholecystectomy specimens, results in a stippled mucosal surface, often described as “strawberry gallbladder” ( Figs. 15.1B and C ). Choleliths or choledocholiths may be present. Cholesterol gallstones, the most common type, are yellow-green, whereas gallstones composed of abundant bilirubin (“pigment stones”) are black or brown. Black pigment stones are sometimes associated with hereditary hemolytic conditions, although the majority of cases are sporadic.
Acute or chronic inflammatory injury to the gallbladder, usually as a consequence of cholelithiasis
10% to 20% of adult population in the United States and Western Europe with cholelithiasis
80% to 90% are calculous cholecystitis; rest are acalculous
1000 to 4000 per 100,000 individuals present with symptomatic disease
Complications include sepsis, abscess, perforation, peritonitis, and fistulas
Risk increases with age
Female predominance for calculous cholecystitis
Males affected more frequently for acalculous cholecystitis
North American Indians affected more commonly than White Americans, African Americans, and Asians
Right upper quadrant or epigastric pain with tenderness (“Murphy sign”)
Fever, nausea, vomiting
Mild jaundice may be present
Peptic ulcer, pancreatitis, kidney stones
Appendicitis or intestinal obstruction

Features of acute cholecystitis include neutrophilic or eosinophilic infiltration, mucosal erosion or ulceration, hemorrhage, gangrenous necrosis, and reactive epithelial changes ( Fig. 15.2 ). The predominant findings in chronic cholecystitis are mural fibrosis, muscular hypertrophy, and a variable degree of mononuclear cell infiltration ( Fig. 15.3 ). Mucosal invaginations through the muscularis propria, known as Rokitansky-Aschoff sinuses, are frequently seen in chronic cholecystitis and are usually associated with muscular hypertrophy. The sinuses may undergo striking cystic change because of outflow obstruction and can mimic a neoplastic process ( Fig. 15.4 ). Inflammatory polyps may also be present. In cases of both acute and chronic cholecystitis, these polyps may have associated reactive epithelial changes and must be distinguished from the polypoid dysplastic lesions. Pyloric gland and intestinal metaplasia may also be present as a consequence of chronic injury and repair ( Fig. 15.5 ). Less frequently, squamous metaplasia may be seen. Xanthogranulomatous cholecystitis is caused by extravasation of bile into the gallbladder wall, eliciting a florid histiocytic response ( Fig. 15.6 ). Reactive fibroblasts are present, which can be so cellular as to mimic a mesenchymal neoplasm. Clues to a benign diagnosis include bland histology, abundant foamy macrophages, and admixed cholesterol clefts and bile pigment. Cholesterolosis is characterized by clusters of cholesterol-laden macrophages that accumulate under the epithelial surface. It is generally considered an incidental finding and does not necessitate further work-up.



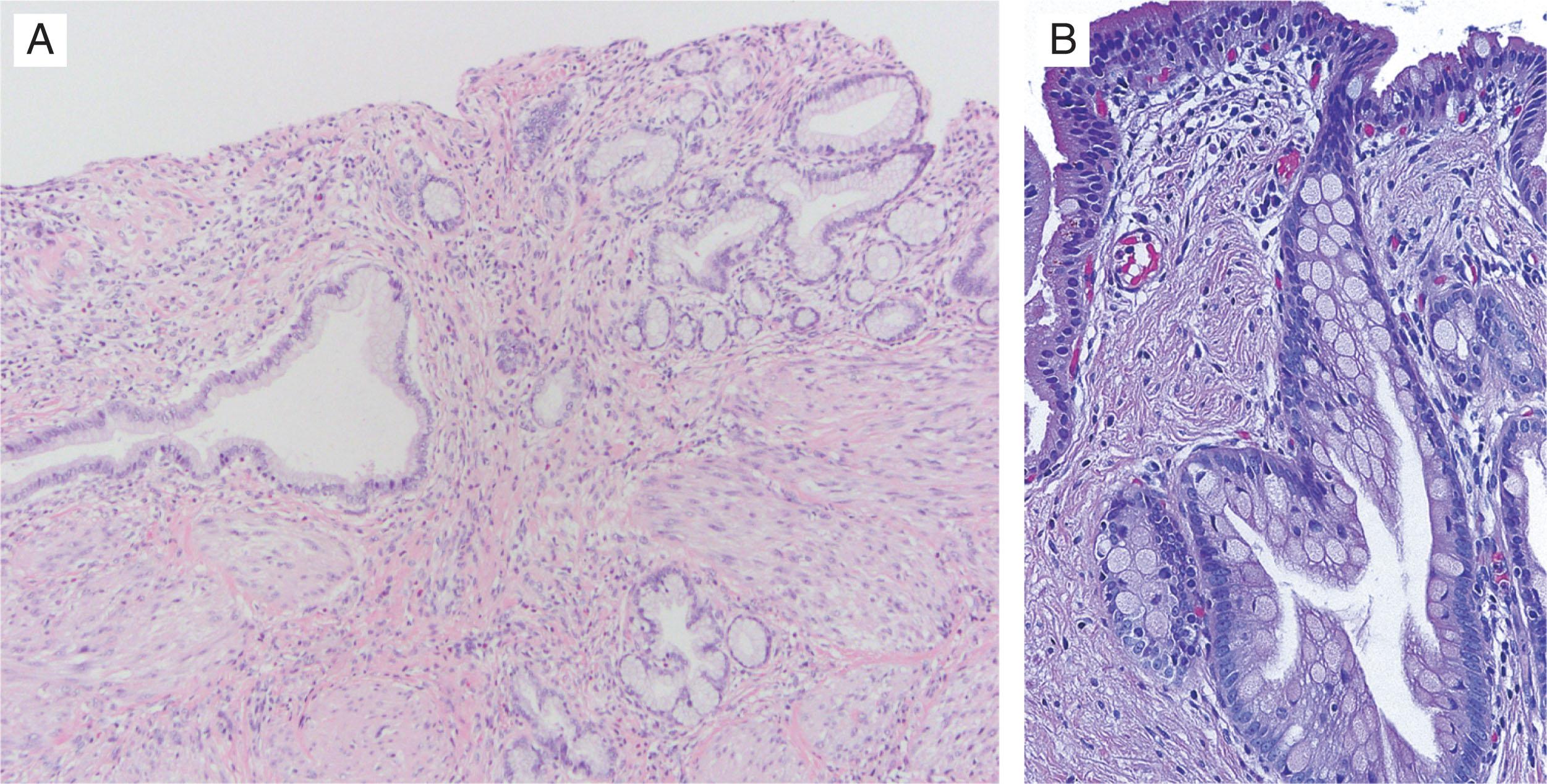

Hyalinizing cholecystitis is defined by paucicellular hyaline sclerosis that obliterates all of the layers of the gallbladder wall ( Fig. 15.7 ). It is typically seen, on average, in patients one decade older than other variants of cholecystitis and in those with long-standing gallbladder inflammation. Focal or diffuse dystrophic calcification may be present in the gallbladder wall. HC cases with diffuse (>80%) calcification correlate with porcelain gallbladder, but all cases of radiographically identified porcelain gallbladder show HC histologically. However, the converse is not always true. Paucicellular hyalinizing sclerosis of HC may be present in some patients with only minimal or no mural calcification. HC, and in particular cases with minimal or no calcification, is associated with an increased (10%–20%) risk for gallbladder carcinoma. Given this risk, complete histologic examination of gallbladder specimens with HC is warranted. Carcinomas associated with HC are generally very well differentiated and may be paucicellular with only scattered neoplastic glands present in the wall. An overt desmoplastic response is not always present.
Acute cholecystitis: mucosal erythema, friability, and ulceration or frank necrosis
Chronic cholecystitis: mural fibrosis with thick, firm wall
Xanthogranulomatous cholecystitis: mural nodules and extension into adjacent organs may mimic malignancy
Choleliths may be present
Thick wall with calcification in porcelain gallbladder
Mucosal erosion, ulcer, or hemorrhage with neutrophilic infiltrate in acute cholecystitis
Transmural necrosis in gangrenous cholecystitis
Chronic inflammation with mural thickening, pyloric gland, and intestinal metaplasia in chronic cholecystitis
Foamy histiocytes with a reactive spindle cell proliferation in xanthogranulomatous cholecystitis
Hyalinized wall with calcification in porcelain gallbladder
Not relevant

Neoplasia involving the gallbladder is diagnosed in two distinct clinical scenarios. Dysplasia or early carcinoma may be an incidental diagnosis in a gallbladder removed for acute or chronic cholecystitis. In other instances, cholecystectomy is performed for a preoperative finding of a mass lesion suspicious for cancer. Not surprisingly, the clinical presentation and morphologic differential diagnosis are quite different in these two situations. For this reason, early and advanced gallbladder carcinomas are discussed under separate headers later. However, it must be emphasized that early and advanced cancers are not distinct entities and represent two stages of the same neoplastic process.
Many cases of early gallbladder neoplasia are found unexpectedly at the time of pathologic evaluation of a routine cholecystectomy rather than by symptomatic presentation or radiographic imaging. Gallbladder dysplasia can be divided into flat (or micropapillary) lesions (biliary intraepithelial neoplasia [BilIN]) and exophytic lesions (intracholecystic papillary neoplasm [ICPN]). Exophytic lesions may be suspected on preoperative imaging, but BilIN is usually clinically occult. Early invasive gallbladder carcinoma with invasion into the lamina propria (T1a) or into the muscular layer (T1b) arising from BilIN cannot be identified preoperatively with certainty. ICPNs are present in 0.5% of all cholecystectomies and about 6% of all gallbladder carcinomas arising in an ICPN.
Risk factors for BilIN and early gallbladder carcinomas include cholelithiasis, chronic cholecystitis, history of gallbladder polyps, PSC, anomalous union of pancreatobiliary ducts, and familial adenomatous polyposis. In contrast to flat dysplasia, ICPN is not strongly associated with cholelithiasis. Both types of dysplasia are associated with advanced age. There appears to be geographic variance in the incidence of early gallbladder carcinoma. Asia and South America have two to three times the incidence in North America and Europe.
As expected, flat dysplasia or BilIN is invisible on gross examination and is detected in random sections from a cholecystectomy. However, ICPN, by definition, is a grossly visible lesion, typically 1 cm or larger, with a median size around 2 cm. Some ICPNs are friable and may be present as detached fragments within the gallbladder lumen. They can be mistaken for luminal debris if this possibility is not considered. Mild thickening of the gallbladder wall may be seen in early invasive carcinomas, but this is often too subtle to be of practical utility, especially because most inflamed gallbladders are edematous. Adequate sampling is key to ensure an accurate diagnosis. Although there is some variation in “optimal practice” based on expert opinion, most agree on the general principle that more sections should be taken with increasing degrees of atypia or dysplasia. The cystic duct margin and one to three sections of representative mucosa are sampled routinely in all cholecystectomy specimens. When low-grade dysplasia or epithelial atypia insufficient for a definite diagnosis of dysplasia is found, submission of extra random sections is useful to exclude high-grade dysplasia or to detect more easily diagnosed foci of neoplasia, respectively. When high-grade dysplasia is seen, thorough sampling is mandatory to rule out an invasive carcinoma. Similarly, multiple additional sections should be submitted in T1a or T1b carcinomas to exclude a more advanced tumor. Areas grossly suspicious for invasive carcinoma should be entirely examined. ICPNs should be submitted entirely along with generous sampling of adjacent mucosa because they are commonly associated with high-grade dysplasia or invasive carcinoma away from the grossly apparent lesion.
Neoplasia confined to the gallbladder epithelium (dysplasia) or carcinoma confined to the lamina propria (T1a) or the muscular wall (T1b)
Approximately 2% to 5% of patients undergoing cholecystectomy in North America and Europe
Higher incidence in South America and Asia
Risk factors: cholelithiasis, primary sclerosing cholangitis, advanced age, gallbladder polyps, familial adenomatous polyposis, anomalous union of pancreatobiliary ducts
6% of all cancers arise in an intracholecystic papillary neoplasm
Dysplasia: cholecystectomy with negative margins is curative
Early carcinoma: favorable prognosis (∼90% 5-year survival) if gallbladder is examined entirely to exclude deeply invasive tumor
Female predominance
Mostly affects adults
Often asymptomatic
Cholecystitis and cholelithiasis are usual indications for cholecystectomy
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here