Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
These are uncommon, incidental findings at endoscopy that usually occur in women in the fifth decade of life. The vast majority are solitary; some may present as a papillomatosis. They are thought to be a reactive proliferation secondary to gastroesophageal reflux disease (GERD). In the Western population, most lesions arise in the distal esophagus, whereas mid-esophagus is the most common site of involvement reported in Japan.
The lesions are typically seen as tiny well-demarcated polyps at endoscopy. Mucosal biopsy samples appear as small whitish nodules.
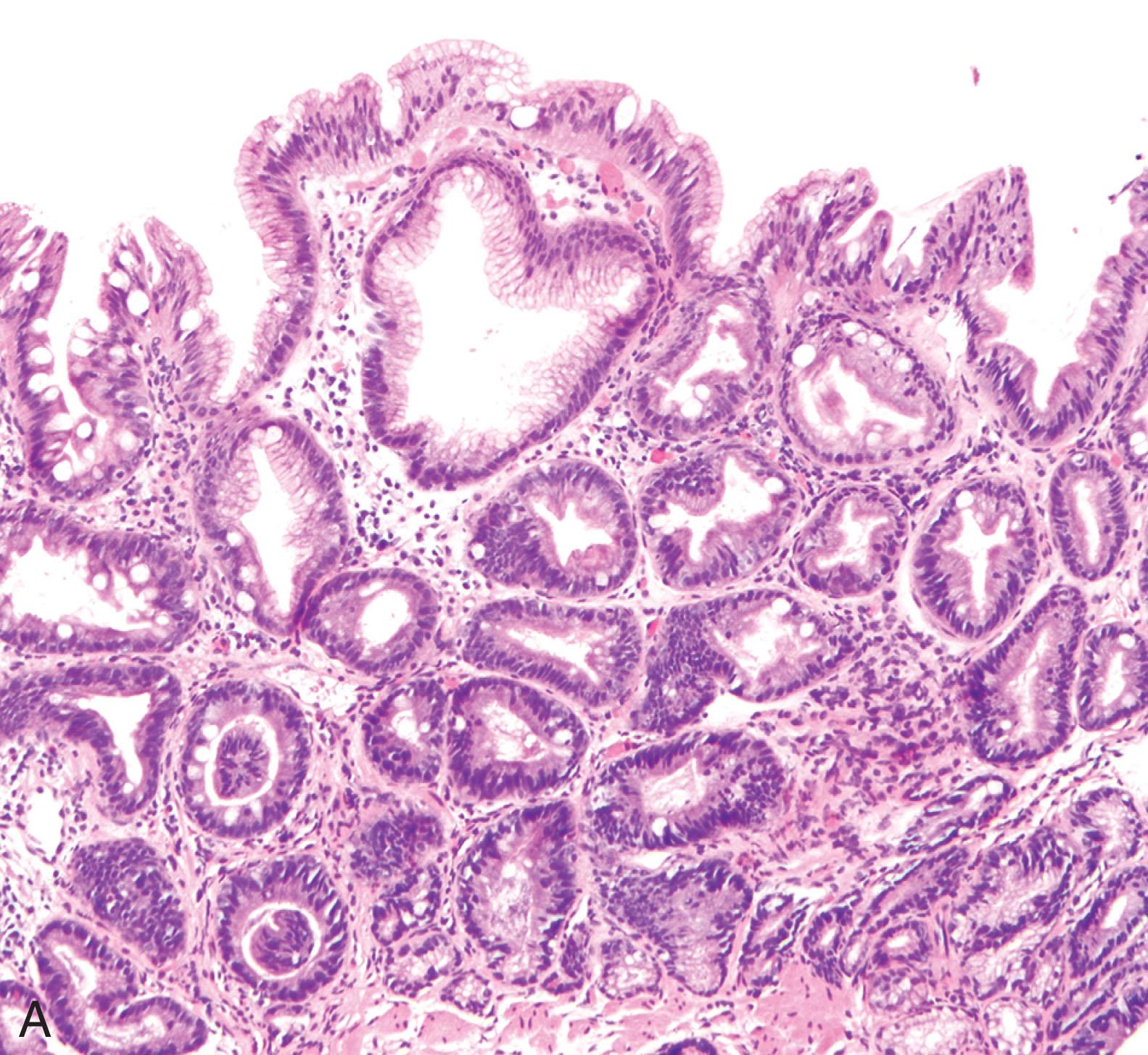
These lesions are composed of bland polypoid squamous mucosa with fibrovascular cores ( Fig. 2.1 ). Exceptional cases may display viral cytopathic effect, and these appear to be more prevalent in the upper esophagus.
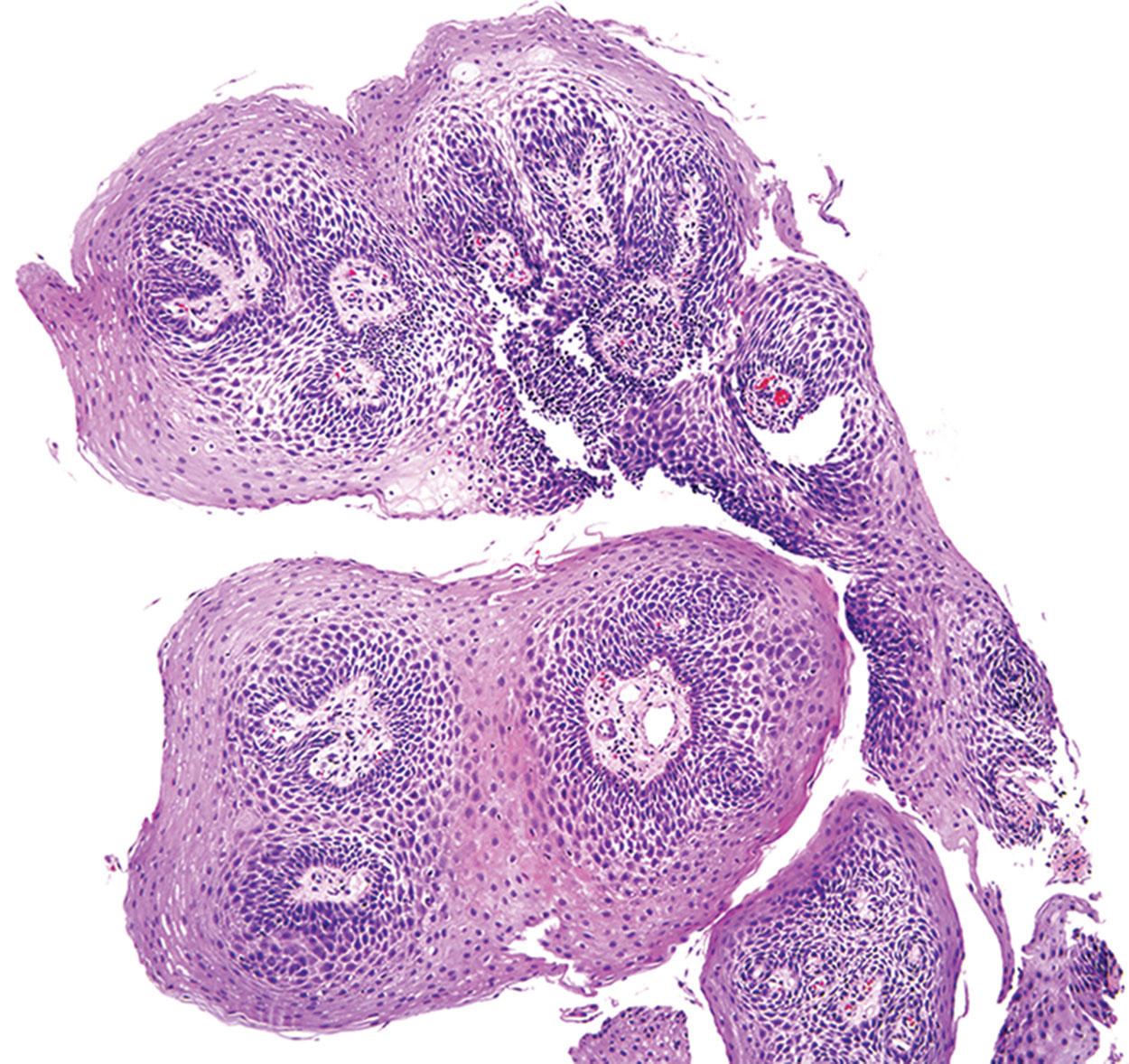
The majority of squamous papilloma are negative for human papillomavirus (HPV) by both immunohistochemistry and in situ hybridization. A subset of patients with HPV-associated laryngeal papillomatosis are reported to also have concurrent HPV-related squamous papillomatosis of the esophagus ( Fig. 2.2 ).
The differential diagnosis includes squamous dysplasia, but squamous papillomas show no epithelial atypia, and the diagnosis is usually straightforward.
Squamous papillomas have no risk of recurrence or malignant transformation.
Small, incidental nodules of the esophagus composed of proliferative benign squamous epithelium
Uncommon (<0.5%); usually involve the distal esophagus
None; other than rare examples associated with laryngeal papillomatosis, which may cause obstruction
Squamous papillomas are more common in white women, usually in their early 40 s
Incidental smooth nodular lesions on endoscopy
Small nodule with a smooth surface seen at endoscopy
Small nodular squamous proliferation aligned in a papillary configuration with fibrovascular cores
Results from immunohistochemical, polymerase chain reaction, and in situ hybridization studies for human papillomavirus are negative in most series
Papillary squamous neoplasia (low or high grade)
Fibrovascular polyps are extremely rare submucosal tumors of the esophagus that have been variably classified as lipomas, fibromas , and fibrolipomatous polyps . Most patients described in literature are middle-aged or older men, although children, infants, and women may also be affected. Presenting complaints include dysphagia, substernal discomfort, and sensation of a mass. Recent data suggest these lesions are almost universally positive for MDM2 and CDK4 and show MDM2 amplification on fluorescence in situ hybridization, suggesting that the so-called “giant fibrovascular polyp” is actually a unique macroscopic appearance of atypical lipomatous tumor involving the esophagus.
On gross examination, these are sausage-like pedunculated polyps arising in the upper third of the esophagus and attached to the wall with a narrow stalk. Their surface is covered by squamous mucosa, and their cores consist of an admixture of grossly identifiable adipose tissue and firm white connective tissue.
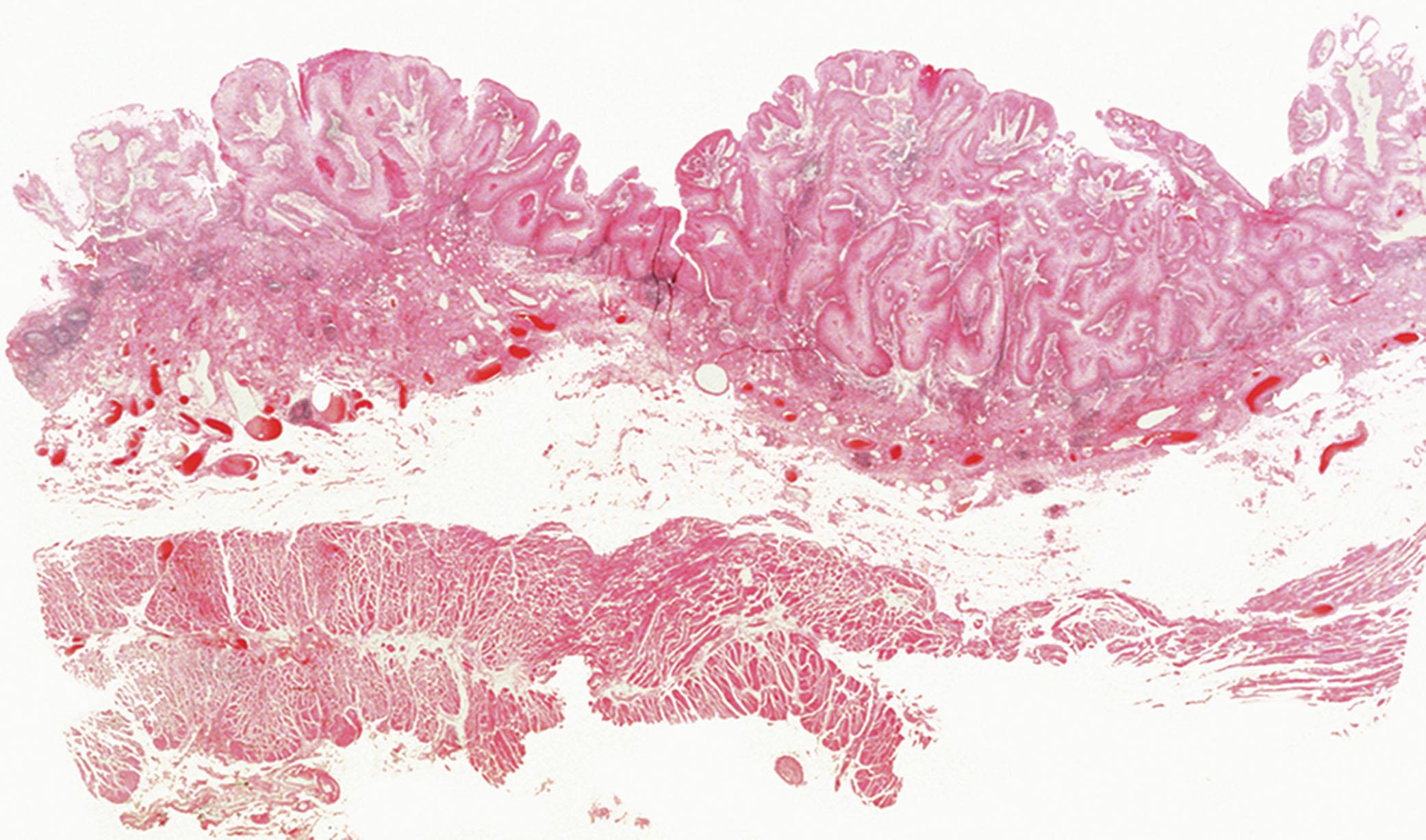
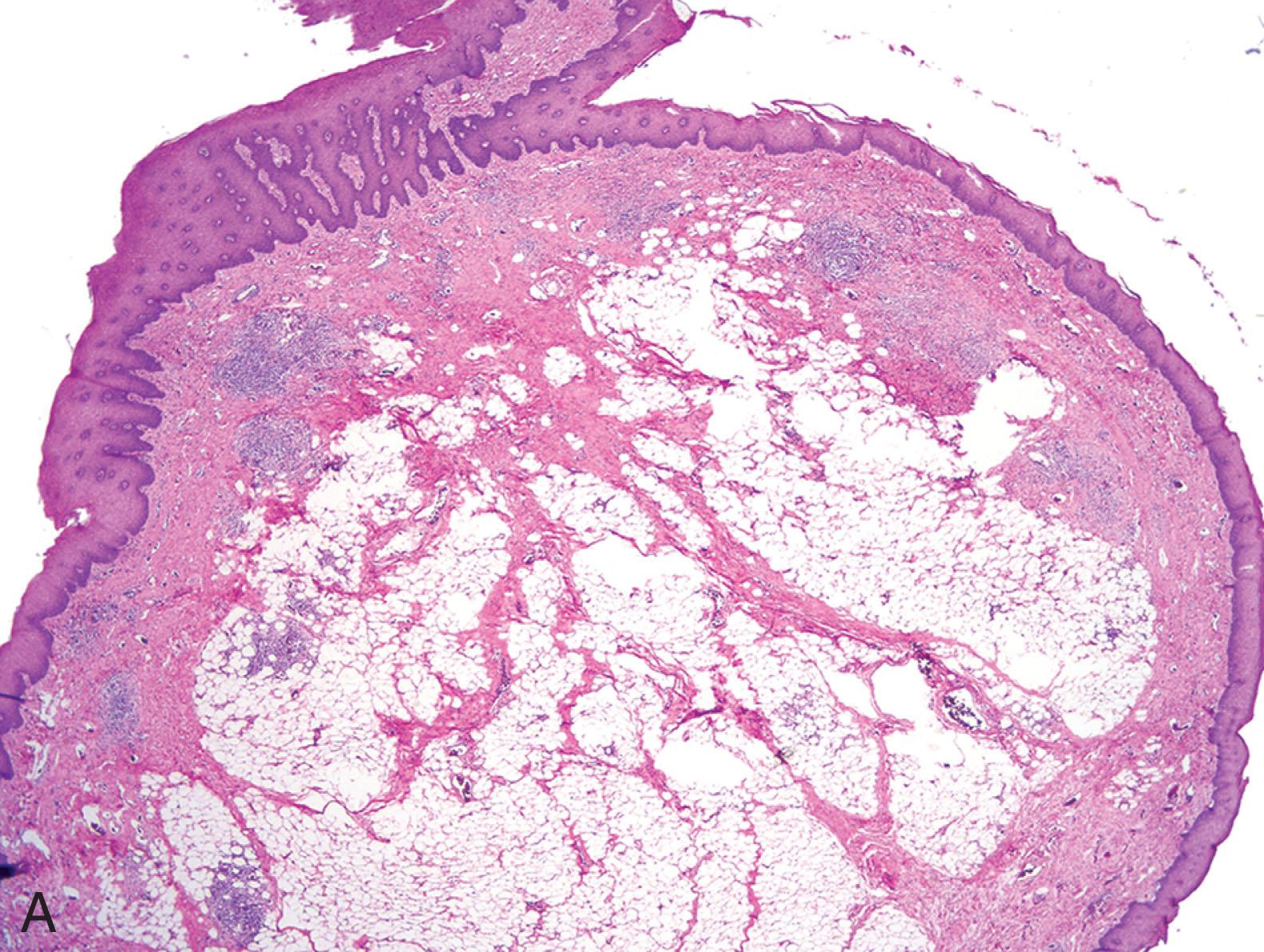
The lesions are composed of variable amount of mature adipose tissue, often separated by thick fibrous bands or sometimes a myxoid stroma and prominent vasculature, all surrounded by mature squamous epithelium ( Fig. 2.3A ). Scattered, large, atypical cells with hyperchromatic nuclei and classic atypical multivacuolated lipoblasts may also be seen ( Fig. 2.3B ). Rarely, dedifferentiated foci may also occur, similar to atypical lipomatous tumors of soft tissue.
MDM2 and CDK4 show positive staining in the adipocytic component and the atypical stromal cells in almost all cases.
Fluorescence in situ hybridization shows MDM2 amplification and ring chromosome involving chromosome 12q have been described in these lesions, similar to atypical lipomatous tumors of somatic soft tissue.
The main differential diagnosis is secondary esophageal involvement of the esophagus by contiguous extension of a primary mediastinal liposarcoma. The latter typically presents as a large mural mass while primary esophageal atypical lipomatous tumors presents as a slender elongated polyp with a narrow base. Inflammatory polyps of the esophagus usually occur in the distal third and show a fibromuscular stroma without an adipocytic component. The diagnosis of a “giant fibrovascular polyp” should not be made unless careful microscopic evaluation and ancillary work-up have completely excluded the possibility of an atypical lipomatous tumor.
Complete excision is curative in most cases, although local recurrences have also been described. Excision can be accomplished by endoscopic ligation or surgical excision when the base of the lesion is poorly visualized by endoscopy. Metastasis has not yet been reported from these lesions.
Submucosal-based esophageal tumor composed of adipocytes and atypical stromal cells, thick-walled blood vessels and a fibrocollagenous or myxoid stroma similar to atypical lipomatous tumor of soft tissue
Very rare; usually in the upper third of the esophagus
May cause morbidity and rare mortality based on obstruction of the esophagus or aspiration
Male predominance
Typically middle aged to older
Present with dysphagia, mass sensation, retrosternal discomfort, or regurgitation of the mass
Local excision is curative
Long, slender, finger-like lesion with a narrow stalk arising from the esophageal wall and protruding into the lumen
Mature squamous mucosa with underlying adipose tissue with adipocytes of variable size, atypical stromal cells, multivacuolated atypical lipoblasts in a fibrocollagenous or myxoid stroma rich in blood vessels
Positive for CDK4 and MDM2
MDM2 amplification on FISH
Ring chromosomes involving chromosone 12q
Inflammatory polyps
Secondary involvement by mediastinal liposarcoma
Barrett’s esophagus (BE) arises as a complication of chronic GERD. Its incidence is rising in the Western Hemisphere and parallels the increase in esophageal adenocarcinoma. Other risk factors for BE include male sex, white race, advanced age, and truncal obesity; cigarette smoking is a minor contributor. The presence of Barrett’s mucosa in the esophagus does not cause symptoms, which makes it hard to screen the population for this precursor lesion of significant clinical consequence. The major importance of BE is the marked predisposition it confers on patients for subsequent development of esophageal adenocarcinoma through inflammation to metaplasia to dysplasia to adenocarcinoma sequence. However, most patients with esophageal adenocarcinoma present with cancer and do not carry a prior diagnosis of BE. Periodic surveillance and biopsy for early detection of neoplasia is the current standard of care for BE patients, but only a small minority of those under surveillance develop adenocarcinoma.
The 2011 American Gastroenterology Association (AGA) guidelines defined BE as intestinal-type metaplastic epithelium that replaces stratified squamous mucosa in the esophagus and predisposes to cancer development, requiring both endoscopic evidence of columnar metaplasia and histologic demonstration of goblet cells. However, in Japan and much of Europe and the United Kingdom, goblet cells are not required to diagnose BE. The term columnar lined esophagus is used instead of BE, emphasizing the endoscopic rather than histologic definition of the entity. The requirement for goblet cells is still used in the United States because population-based studies have shown a much higher risk of esophageal adenocarcinoma in patients with intestinal metaplasia than in those without intestinal metaplasia. Including patients without goblet cells into the periodic surveillance pool has major implications for cost of care and cannot be justified unless the risk in nongoblet metaplastic columnar epithelium is shown to be significant and comparable to those with goblet cells in longitudinal outcome studies. Detection of goblet cells is susceptible to sampling error. At least eight random biopsies or four biopsies per centimeter of columnar epithelium are recommended to obtain the maximum yield of intestinal metaplasia on histologic examination. According to the recently published 2016 American College of Gastroenterology guidelines, BE should only be diagnosed if there is extension of metaplastic columnar epithelium 1 cm or greater proximal to the GEJ. This change was recommended because patients with less than 1 cm of metaplastic columnar epithelium have a very low risk of esophageal adenocarcinoma in long-term follow-up studies, which does not justify routine surveillance. However, the AGA criteria do not have a length requirement and only require definite columnar mucosa lining the distal esophagus with intestinal metaplasia detected on biopsies from this segment.
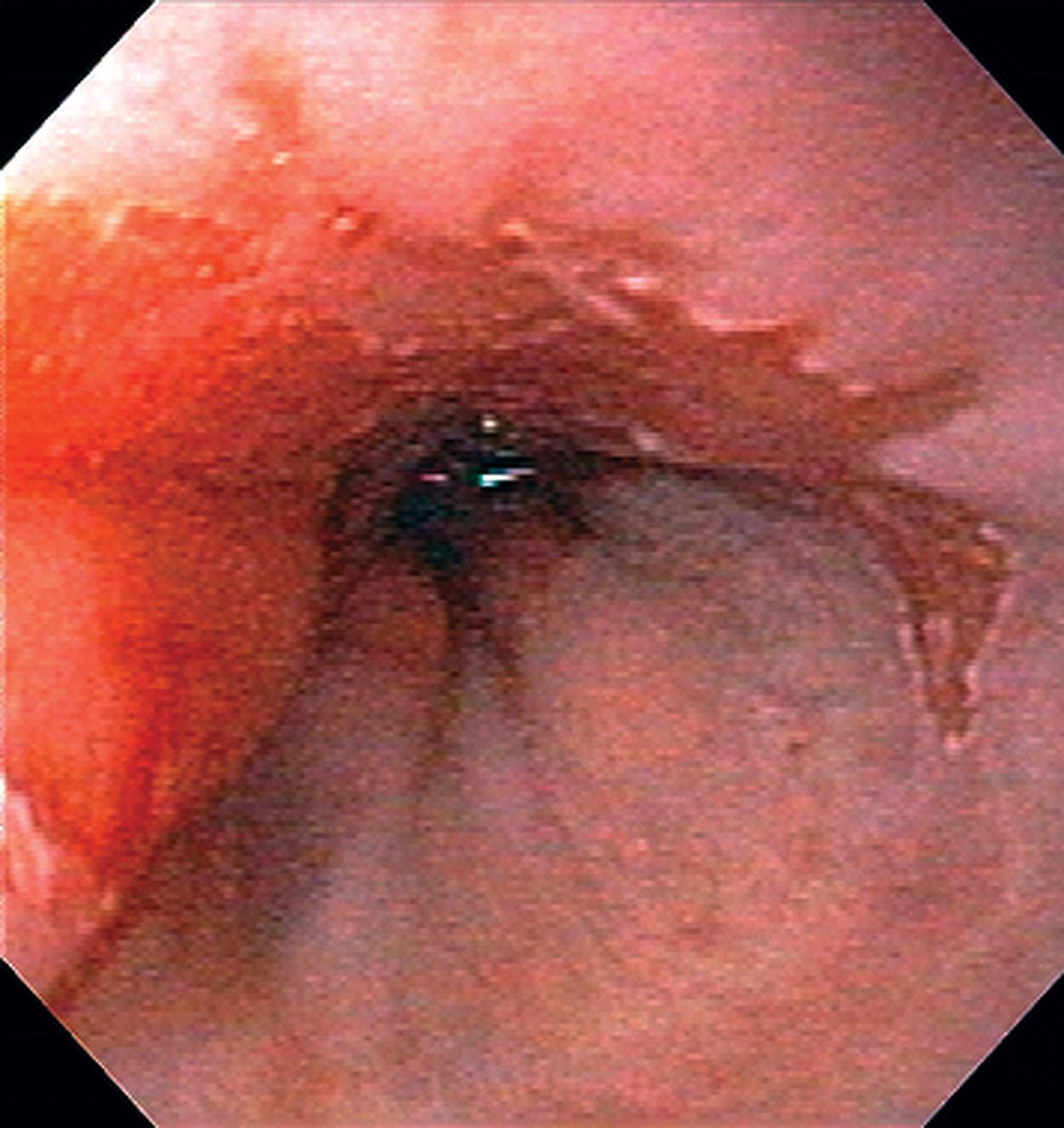
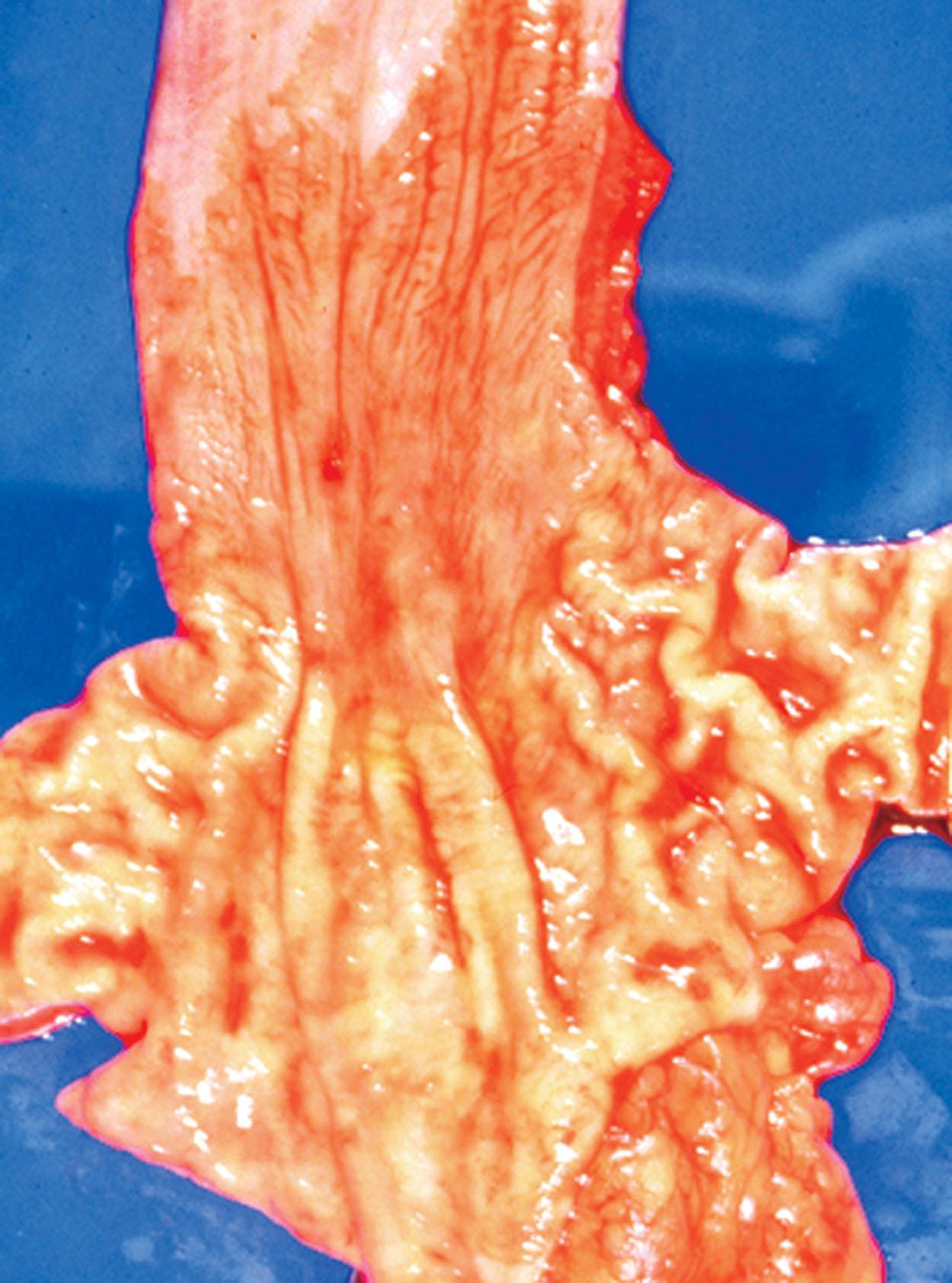
Barrett’s esophagus appears as tongues and patches of red salmon-colored mucosa that extend up from the gastroesophageal junction (GEJ) for variable distance into the tubular esophagus and contrasts with the pearly gray-pink color of the normal squamous epithelium ( Figs. 2.4 and 2.5 ). Traditionally, short-segment BE is defined as less than 3 cm of metaplastic columnar epithelium, and long-segment BE is defined as greater than 3 cm of metaplastic columnar epithelium. This distinction is important because although short-segment BE is more common, it is less likely than long-segment BE to give rise to esophageal adenocarcinoma.
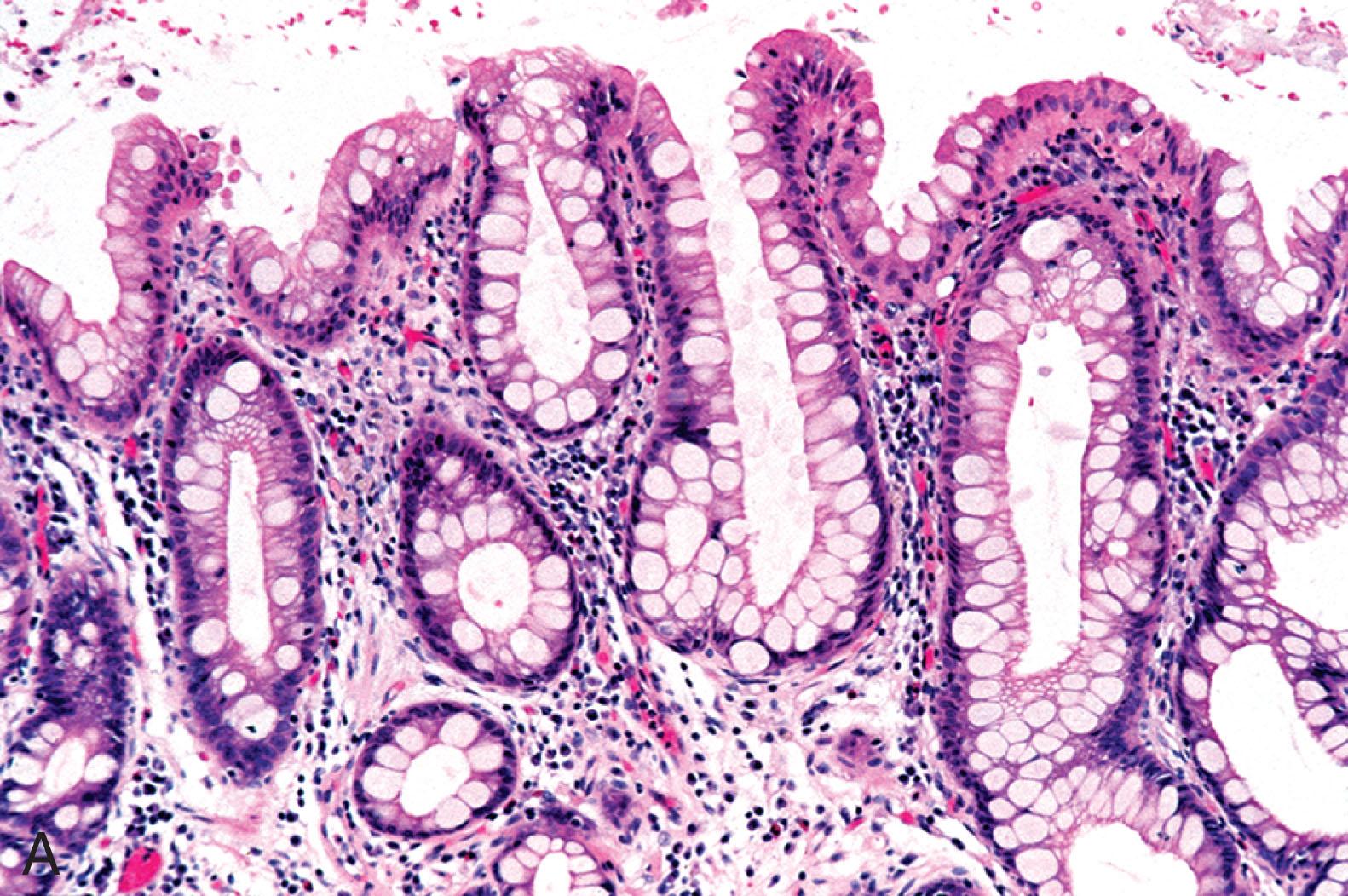
A majority of patients with BE have a concurrent hiatal hernia, and biopsies from the columnar segment in the distal esophagus may show a cardia- or oxyntocardiac-type glandular epithelium or an intestinalized epithelium with goblet cells. Goblet cells are readily identifiable on hematoxylin and eosin–stained slides, and ancillary stains are unnecessary ( Fig. 2.6 ). Typically, these goblet cells are admixed with gastric-type lining cells, and this type of metaplasia is termed incomplete . Multilayered epithelium is a hybrid epithelium consisting of mucin-containing glandular cells and basally located squamous cells, frequently seen in patients with GERD and may be a precursor of BE ( Fig. 2.7 ). Its presence is not routinely reported in GEJ or esophageal biopsies, and it should not be considered to represent BE. The metaplastic intestinalized mucosa often lays down a new muscularis mucosae, resulting in two distinct layers: a delicate, frayed, superficial layer and a deep, thick, compact, native muscularis mucosae. The latter can be mistaken for muscularis propria because of its thickness.
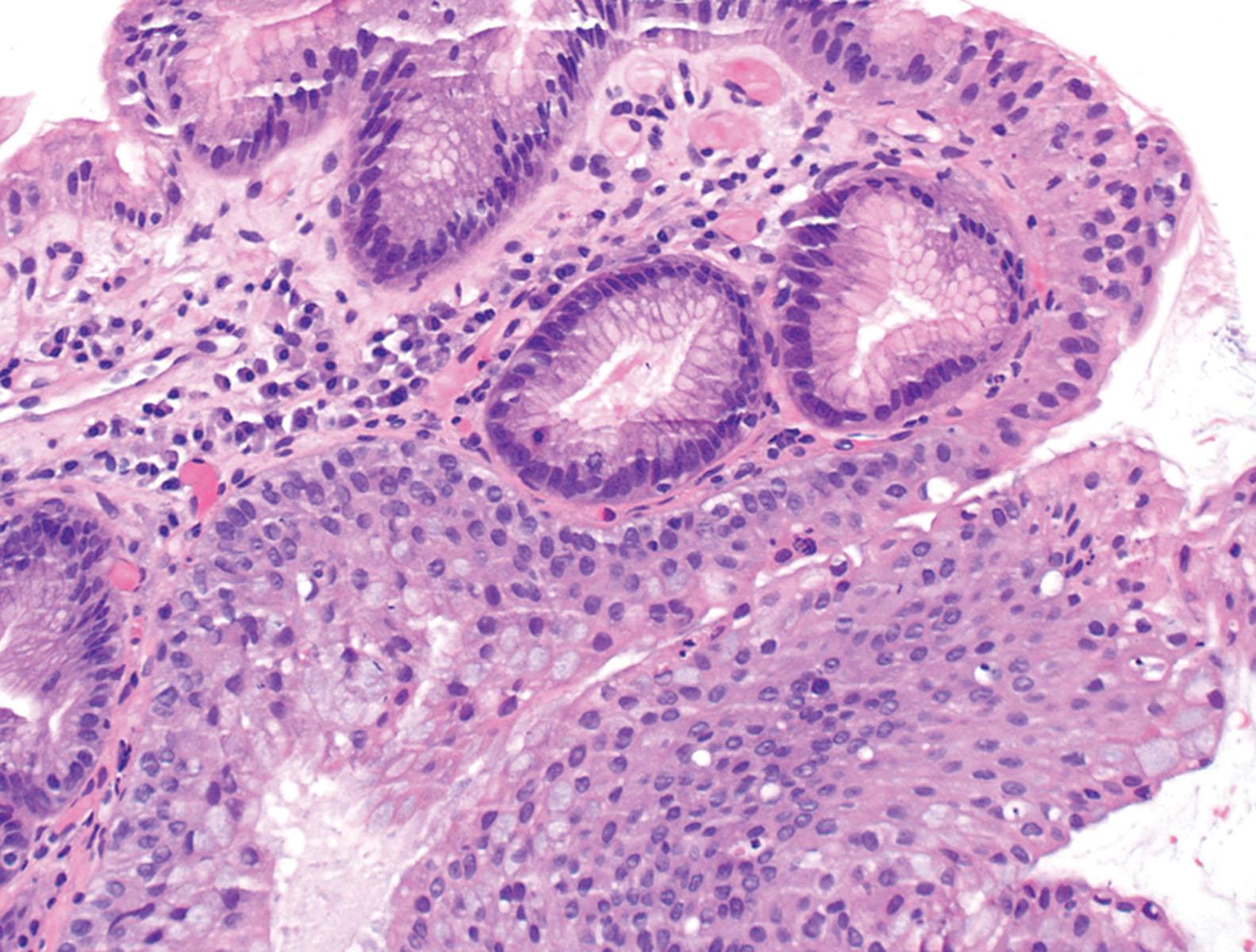
The differential diagnosis of BE includes gastric carditis with intestinal metaplasia (CIM), seen in approximately 30% of patients with an abnormal squamocolumnar junction. CIM is most often associated with Helicobacter pylori infection and has a lower incidence of dysplasia compared with BE. Autoimmune gastritis may also cause CIM and should be considered in the differential diagnosis when only GEJ biopsies are available. Certain histologic features have been described to help distinguish BE from CIM. These include metaplastic crypts buried underneath squamous mucosa, hybrid glands consisting of cardia-type and intestinalized glands, and esophageal glands and ducts. The presence of esophageal glands or ducts adjacent to foci of intestinal metaplasia is diagnostic of BE ( Fig. 2.8 ); other features are suggestive but not definitive.
Barrett’s esophagus is a preneoplastic precursor lesion with the risk of adenocarcinoma being approximately 0.5% per year. Patients with nondysplastic BE are therefore recommended periodic endoscopic surveillance at 3- to 5-year intervals. Therapy is largely based on treating GERD, typically with proton pump inhibitor therapy.
Columnar epithelium in the tubal esophagus with intestinal metaplasia on biopsy (US definition). In addition, some gastroenterology societies in the United States have also included a length (>1 cm) requirement. Goblet cells are not part of the definition in many parts of Europe and Japan ( columnar-lined esophagus used as a synonym for Barrett’s esophagus [BE])
5% of individuals with gastroesophageal reflux disease
Strong risk factor for esophageal adenocarcinoma, with an estimated annual rate of progression of approximately 0.5%
White male predominance with a median age in the early 50 s
Usually asymptomatic; reflux symptoms may lead to screening for BE
Well-defined criteria for screening patients for BE are lacking
Salmon-colored mucosa in the esophagus
May appear as a markedly irregular Z-line, a visible tongue of columnar epithelium, or a discrete island of columnar epithelium surrounded on all sides by squamous mucosa
Admixture of cardia-type, oxyntocardiac-type, and intestinalized glands
Intestinal metaplasia is typically of incomplete type, which shows goblet cells interspersed gastric foveolar-type cells
Double muscularis mucosae may be present
PAS-AB stain highlights goblet cells but is not recommended for routine diagnosis
Intestinal metaplasia of the gastric cardia secondary of Helicobacter pylori or autoimmune gastritis
Esophageal glands or ducts, when present, are helpful in establishing a diagnosis of Barrett’s esophagus. Endoscopic correlation needed in the remaining cases
Barrett’s esophagus arises as a complication of chronic reflux disease and is the major predisposing risk factor for esophageal adenocarcinoma. Other risk factors include obesity, older age, and to a lesser extent, smoking and alcohol intake. Any condition that causes chronic local irritation and inflammation of the esophageal mucosa appears to predispose to squamous cell carcinoma (SCC). Significant alcohol intake, especially in combination with smoking, greatly increases the risk of SCC. Other predisposing factors include achalasia and esophageal diverticula in which food retention leads to local release of chemical irritants, frequent consumption of extremely hot beverages, and ingestion of lye or other caustic liquids. SCC is also linked to low socioeconomic status and to nutritional deficiency syndromes, such as the Plummer-Vinson syndrome (dysphagia, iron-deficiency anemia, and esophageal webs).
Nonepidermolytic palmoplantar keratoderma (tylosis), a rare autosomal dominant disorder defined by a genetic abnormality at chromosome 17q25, is a familial syndrome that predisposes patients to SCC. It is characterized by hyperkeratosis of the palms and soles and thickening of the oral mucosa. It confers up to a 95% risk for SCC of the esophagus by the age of 70 years. A polymorphism that increases the risk for esophageal squamous carcinoma has also been identified in individuals with inactive aldehyde dehydrogenase.
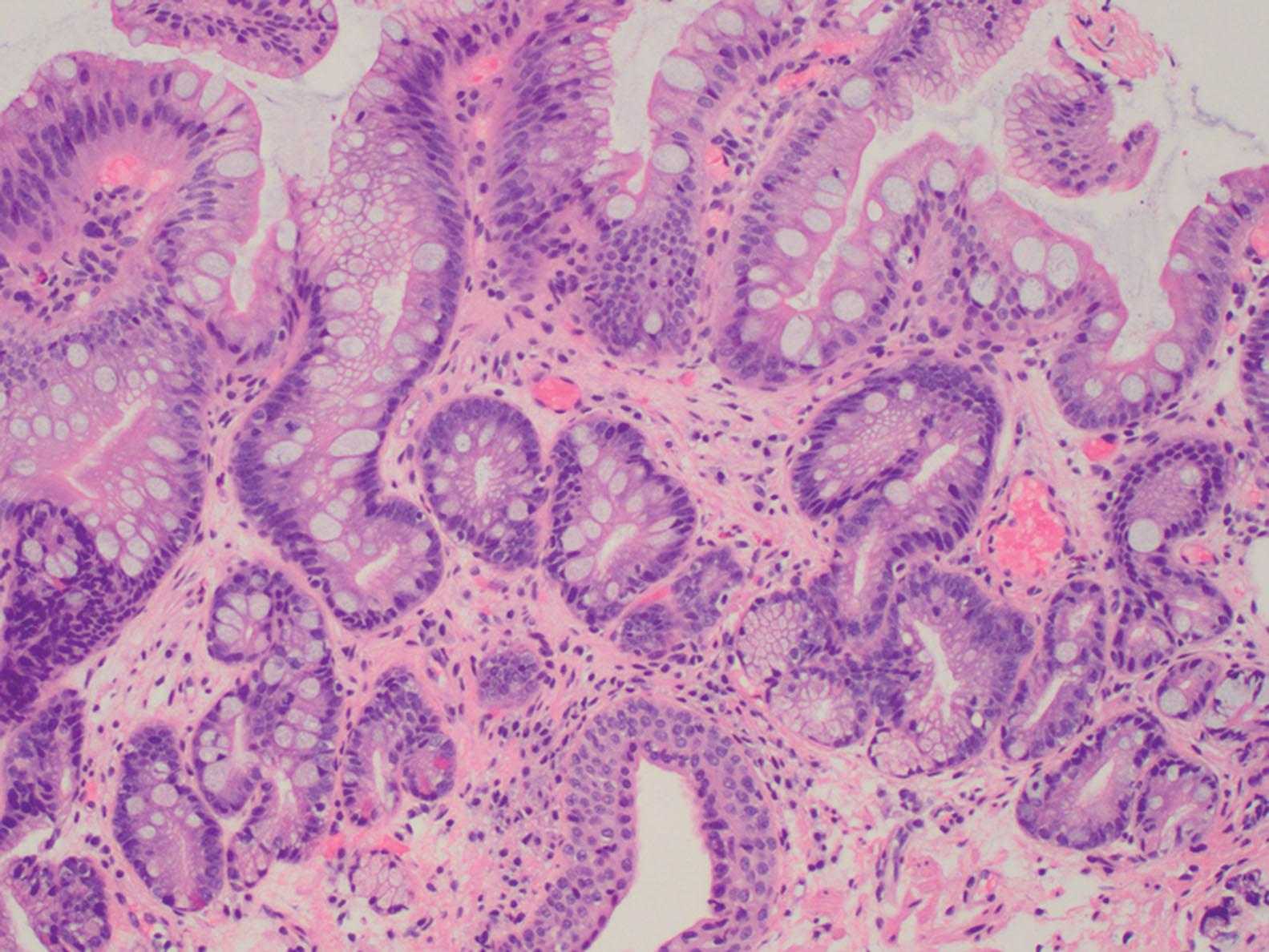
Surveillance biopsies from patients with BE are classified as negative for dysplasia, indefinite for dysplasia (IND), low-grade dysplasia (LGD), and high-grade dysplasia (HGD) ( Table 2.1 ). Histologic features that are helpful in evaluation of BE biopsies include the presence of architectural complexity, cytologic atypia involving the surface epithelium, and the presence of lamina propria inflammation, erosions, or ulcers. Surface maturation is key to diagnosis of nondysplastic BE. The proliferating nuclei in the basal part of the intestinalized crypts are larger, more hyperchromatic, and more stratified than those at the surface, which are generally arranged in a monolayer with polarized basal nuclei. Architectural abnormalities include gland crowding, crypt branching and budding, and villiform change. Cytologic features of dysplasia include nuclear enlargement and hyperchromasia, irregular nuclear contours, coarse chromatin with prominent nucleoli, and loss of polarity. In “normal polarity,” the long axis of the nucleus remains perpendicular to the basement membrane and the nuclei are aligned parallel one to another, whereas “loss of nuclear polarity” refers to loss of this perpendicular and parallel orientation. Inflammation with consequent reparative changes can impart worrisome cytologic alterations that can be mistaken for dysplasia. An abrupt morphologic change from adjacent mucosa favors a diagnosis of dysplasia.
| Dysplasia | Surface Maturation | Architecture | Cytology | Inflammation | Nuclear Polarity |
|---|---|---|---|---|---|
| Negative | + | Normal; abundant lamina propria between glands | Nuclear stratification and mitoses limited to gland base; smooth nuclear contours and inconspicuous nucleoli | −/+ | Maintained |
| Indefinite | +/− | Normal to slight crowding of glands | Nuclear irregularity and hyperchromasia or mitoses typically limited to gland base | +/− | Maintained |
| Low grade | − | Mild to marked crowding of glands | Pencillate, stratified, hyperchromatic nuclei extending to surface epithelium (resemble colonic tubular adenoma) | −/+ | Maintained |
| High grade | − | Marked crowding of glands; villiform architecture | Enlarged hyperchromatic nuclei, coarse clumped chromatin, nucleoli may be prominent; loss of polarity, frequent mitoses | −/+ | Lost |
In BE without dysplasia, the glands tend to be straight with smooth contours, crypt budding or branching is minimal, and abundant lamina propria is present between glands. The cytologic atypia, if any, is confined to the basal aspect of the crypts, while the surface epithelium shows maturation with small basally located nuclei and abundant cytoplasm ( Fig. 2.9 ). Mitoses may be present but are localized to the basal crypt epithelium. Nuclei have smooth nuclear membranes with fine chromatin and inconspicuous nucleoli. In the setting of reactive changes, epithelial cells in the zone of inflammation may display nuclear enlargement, and nucleoli may become more prominent, but nuclear contours are generally smooth with a vesicular chromatin, small nucleoli and the overall nuclear-to-cytoplasmic ratio is preserved. There may be loss of cytoplasmic mucin, but surface maturation is preserved.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here