Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Zoonoses, derived from the Greek words zōio (animal) and nósos (disease), are infectious diseases transmitted from animals, both wild and domestic, to humans or from humans to animals. Among emerging or reemerging infectious diseases, 60 to 75% are zoonoses. Most recently, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; Chapters 335 , 336 , and 337 ) has shown the devastating effects of zoonotic transmission followed by travel-related human spread.
Zoonotic pathogens or their toxins can be transmitted by several different routes: direct contact with animals or their products (e.g., tissue, urine, or excreta); animal bites and scratches; arthropod vectors; and consumption of contaminated food or water. Zika virus ( Chapter 352 ), Borrelia burgdorferi ( Chapter 297 ), Babesia microti ( Chapter 324 ), and Plasmodium knowlesi ( Chapter 316 ) are well-recognized vector-transmitted zoonotic pathogens. However, many arthropod vector–borne pathogens, such as Plasmodium falciparum ( Chapter 316 ) or Bartonella quintana ( Chapter 291 ), are not zoonotic because they are transmitted from human to human through the vector but lack an animal reservoir. Similarly, many infections acquired from the environment also are not zoonoses; examples include melioidosis ( Burkholderia pseudomallei ; Chapter 282 ) and histoplasmosis ( Histoplasma capsulatum ; Chapter 308 ). Understanding the epidemiology and transmission of zoonotic versus nonzoonotic infections is critical for implementing control measures at local, regional, and international levels.
Zoonotic spillover occurs when barriers that prevent a zoonotic agent from gaining access to and infecting a human are breached or fail. Such issues include factors related to the interaction between the reservoir host and the pathogen, including where the reservoir host lives; the prevalence of the pathogen within the host; the likelihood of its release from the infected reservoir host; the ability of the pathogen to survive and disseminate after release from the host; and human characteristics that affect the ability of the pathogen to enter and propagate within humans, such as structural barriers, immunity to infection, and genetic predisposition to infection. Zoonotic infections, not surprisingly, are difficult to predict because distinct barriers are not equally shared for each pathogen/reservoir combination owing to the great genomic diversity of animals, humans, and microbes.
In the United States, about 60% of people own a pet. Dogs and cats are most frequent. However, other pets include fish, birds, reptiles, hamsters, guinea pigs, rabbits, and horses. Moreover, exotic animals, including large cats, primates, and bears, are legal with or without a permit in many U.S. states. Wildlife-related recreation exposes more than 90 million U.S. residents to increased risk for zoonoses, and 72 million observe, feed, or photograph birds and other wildlife.
Climate change ( Chapter 16 ) can both increase the likelihood of spillovers (the complicated process by which pathogens defy natural barriers and infect new animal species) and affect chains of transmission. Climate change is expected to increase the risk for zoonoses over the next 50 years because of extreme temperatures that cause increased rainfall and violent storms, rising sea level and floods that could augment zoonotic diarrheal disease, loss of biodiversity, collapse of ecosystems, an increase in pests, and the spread and increase in both neopteran (biting insect) and acarid (tick and mite) vectors of zoonotic pathogens.
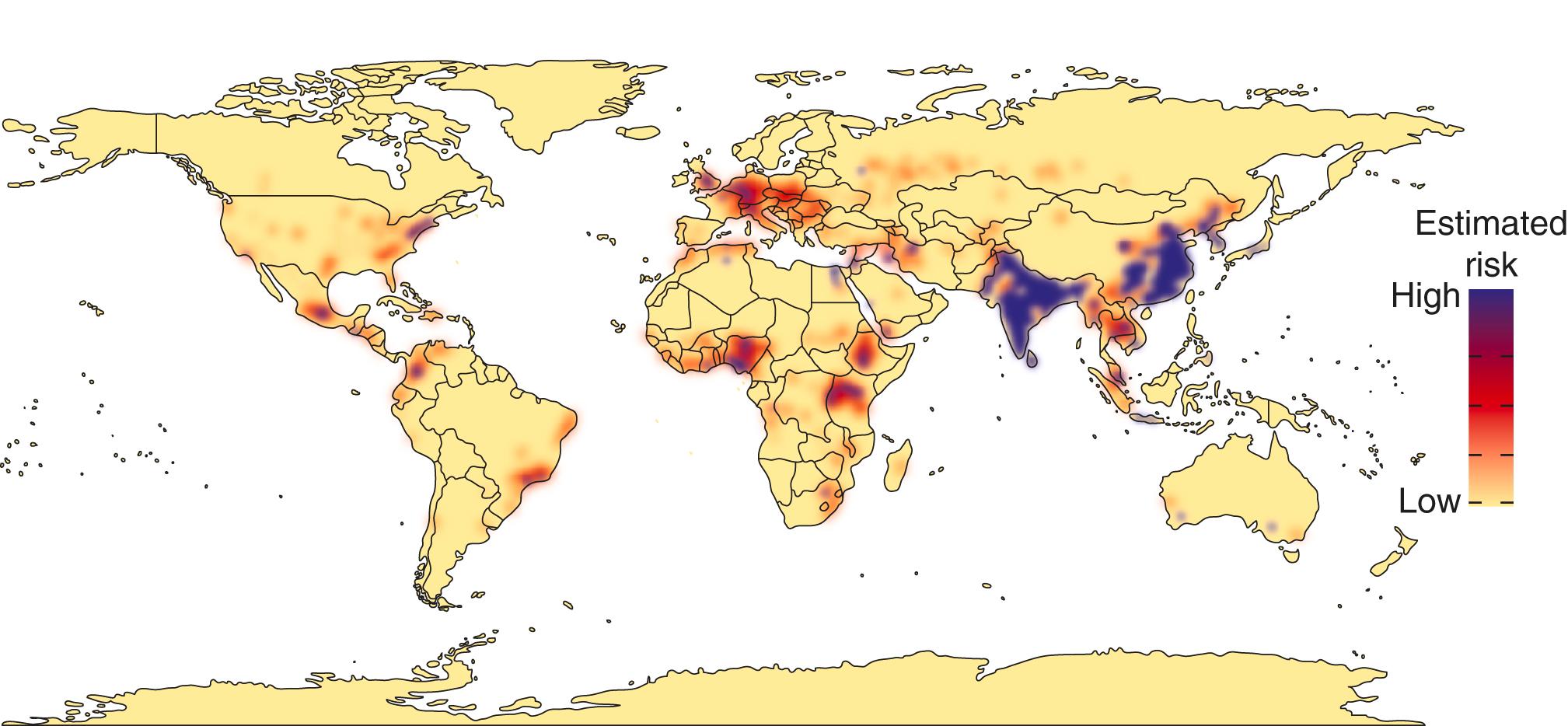
Most emerging zoonoses are acquired from contact with wildlife. Key factors that predict emergence of zoonoses are origin in tropical forest regions, increases in mammal biodiversity, changes in anthropogenic land use related to agricultural practices, and illegal wildlife trade ( Fig. 303-1 ). Residential and other land development directly related to human activity is by far the strongest predictor of risk.
Zoonoses are transmitted through one or more of several mechanisms: direct contact with animals or infected materials and/or related inhalation; animal bites and scratches; bites or mechanical transmission by arthropod vectors; and consumption of contaminated foods ( Table 303-1 ). Direct contact with animals is a well-documented mechanism for acquiring viral, bacterial, protozoan, and fungal zoonotic pathogens. The risk is particularly high for individuals whose occupations or recreations involve contact with animals. For example, in a study of veterinarians in Oregon, contact-related ringworm was the most common zoonosis, and rabies the most dangerous; cats were the most likely source of contact-related zoonoses. Significant risks also exist for farmers, abattoir workers, and animal handlers. Leptospirosis ( Chapter 298 ), which likely is one of the most neglected of all zoonoses worldwide with an estimated 1 million cases and nearly 60,000 deaths annually, is commonly acquired through direct contact with contaminated rodent urine; however, many wild and domestic animals can become colonized and excrete the spirochete in their urine. Coxiella burnetii ( Chapter 302 ) is distributed worldwide and acquired by inhalation of dust contaminated with excretions, such as milk, urine, and feces, and/or birth products, from infected animals.
| DISEASE/ETIOLOGIC AGENT | TRANSMISSION | RESERVOIR HOST | CLINICAL MANIFESTATIONS |
|---|---|---|---|
| VIRUSES | |||
| Bourbon virus | Ticks? | ? | Fever, fatigue, rash, headache, myalgia, nausea, vomiting; leukopenia, thrombocytopenia |
| Heartland viruses | Amblyomma americanum tick bites | Deer? | Fever, headache, fatigue, anorexia, nausea, myalgia, arthralgia; thrombocytopenia, leukopenia |
| Zika virus | Aedes aegypti and Aedes albopictus mosquito bites | Nonhuman primates, sheep, bats, rodents | Rash, fever, arthralgia, conjunctivitis, myalgia, headache, retroorbital pain; congenital microcephaly, Guillain-Barré syndrome |
| Avian influenza (H5N1) | Inhalation | Poultry, wild and domestic waterfowl, other birds | Influenza-like illness, shortness of breath, difficulty breathing, viral pneumonia with or without acute respiratory distress syndrome, respiratory failure, multiorgan diseases |
| Hendra virus | Direct contact; horses | Flying fox | Fever, cough, sore throat, meningitis, encephalitis |
| Nipah virus | Contact, ingestion | Bats | Fever, headache, shortness of breath, difficulty breathing, encephalitis |
| BACTERIA AND RICKETTSIAE | |||
| Q fever Coxiella burnetii |
Indirect (aerosol) exposure | Goats, sheep, cattle, wildlife | Acute: fever, fatigue, photophobia, headache; cough with pneumonia; hepatitis; chronic: endocarditis, immunosuppression, chronic renal insufficiency |
Spotted fever rickettsiosis
|
Amblyomma maculatum ticks, Dermacentor occidentalis ticks | Small mammals, cattle? Small mammals | Fever, rash, eschar, myalgia, chills, fatigue, arthralgia, headache, lymphadenopathy Fever, headache, myalgia, arthralgia, malaise, lymphadenopathy (children), rash, eschar |
| Plague Yersinia pestis |
Fleas | Small mammals | Fever, chills, headaches, carbuncles, lymphadenopathy with buboes, pneumonia, sepsis |
| PROTOZOA AND HELMINTHS | |||
| Zoonotic malaria Plasmodium knowlesi |
Anopheles leucosphyrous group mosquitoes | Macaques and monkeys | Fever, chills, headache, rigors, malaise, myalgia, cough, nausea, abdominal pain, vomiting, diarrhea |
| Babesiosis Babesia microti |
Ixodes scapularis ticks | Small mammals | Fever, anemia, thrombocytopenia, elevated lactate dehydrogenase, hyperbilirubinemia, increased alanine aminotransferase and aspartate aminotransferase |
| Chagas disease Trypanosoma cruzi |
Triatomine insects in Triatoma , Rhodnius , and Panstrongylus genera | Rodents, raccoons, skunks, coyotes | Chagoma (Romaña sign), fever, lymphadenopathy, edema, hepatosplenomegaly, myocarditis, meningoencephalitis; cardiomyopathy (arrhythmia, heart failure, atrioventricular/branch blocks, thromboembolism); gastrointestinal (dysperistalsis, megaesophagus, megacolon) |
| Baylisascariasis Baylisascaris spp |
Ingestion of contaminated materials | Raccoons, skunks, badgers | Larva migrans (visceral, neural); diffuse unilateral subacute neuroretinitis |
| FUNGI | |||
| Talaromycosis Talaromyces (Penicillium) marneffei |
Direct contact, indirect contact? | Bamboo rats | Fever, cutaneous or subcutaneous lesion(s), malaise, anemia, dyspnea, weight loss, lymphadenopathy, nonproductive cough, anemia |
In addition to direct tissue injury, animal scratches and bites are a common cause of zoonotic infections. In the United States alone, an estimated 4.5 million dog bites occur annually and 900,000 result in infection; therefore, approximately 1 in every 72 people is affected. Examples of pathogens include Capnocytophaga canimorsus from dog bites, as well as Pasteurella multocida ( Chapter 288 ) and Bartonella henselae, the etiologic agent of cat-scratch disease, from cat bites. In some regions of the world, endemic rabies ( Chapter 383 ) is rampant.
Perhaps the best known zoonoses are transmitted through arthropod bites, such as mosquitoes, flies, or ticks and mites. Vector-borne zoonotic viral infections include West Nile virus ( Chapter 352 ), Eastern equine encephalitis virus ( Chapter 352 ), Nipah virus ( Chapter 383 ), and Hendra virus ( Chapter 331 ). P. knowlesi ( Chapter 316 ), Babesia microti ( Chapter 324 ), Leishmania spp ( Chapter 319 ), and Trypanosoma spp ( Chapters 317 and 318 ) are examples of vector-borne zoonotic protozoal infections. Leishmania , with 700,000 to 1 million new cases per year, is associated with epidemics across southern Asia, northern Africa, and South America. Trypanosoma brucei rhodesiense and T. brucei gambiense, agents of African trypanosomiasis and human sleeping sickness ( Chapter 317 ), are transmitted by biting tsetse flies in Africa; cases have been declining in recent years as a result of control efforts, with fewer than 1000 new cases reported in 2019 despite an estimated 65 million people at risk.
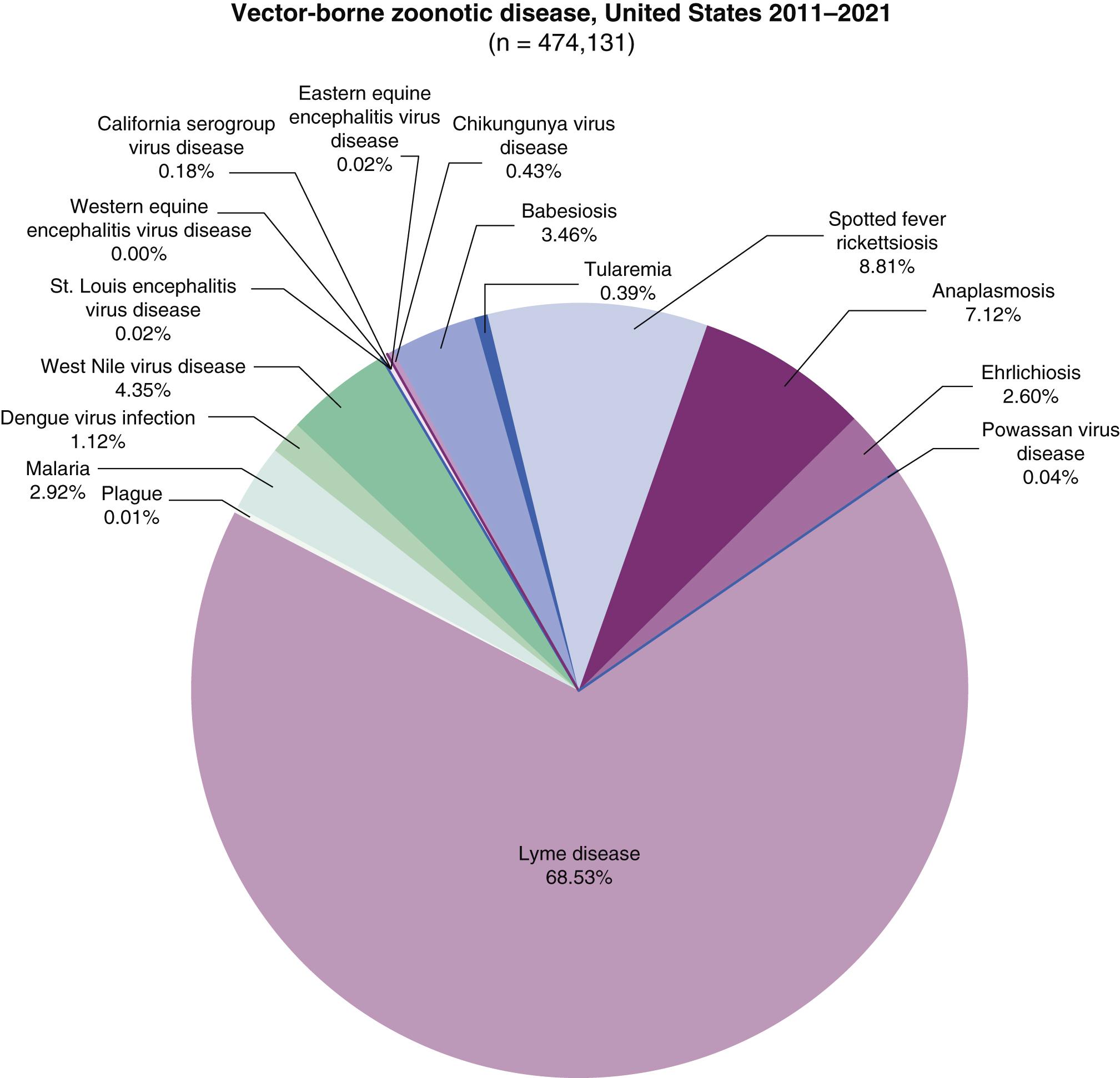
Ticks and mites are the most important vectors of zoonotic disease in the developed world. In the United States from 2012 to 2016, 217,000 of 242,000 (90%) reported cases of vector-borne zoonosis were attributed to tick-borne infections, especially B. burgdorferi ( Chapter 297 ; Fig. 303-2 ); recent studies provide evidence that the actual number of B. burgdorferi infections is more than 10 times that reported. Worldwide, ticks, lice, and mites are also significant, but underrecognized, causes of vector-borne bacterial zoonoses. Examples of neglected vector-borne bacterial zoonotic disease include tick- and louse-borne relapsing fever borreliosis ( Chapter 297 ); spotted fever group rickettsioses ( Chapter 302 ), transmitted principally by hard body (ixodid) ticks; and typhus group rickettsioses ( Chapter 302 ), transmitted by fleas and lice. Scrub typhus ( Chapter 302 ), caused by the rickettsia Orientia tsutsugamushi and transmitted by the larval stage (chigger) of a trombiculid mite, occurs across much of Asia and Oceania and is now emerging in Africa and South America; it is estimated to cause as many as 1,000,000 infections each year globally.
Many important zoonotic infections are acquired through consumption of contaminated foods or water. The list of potential pathogenic agents is vast and includes viruses (such as hepatitis A and E virus; Chapter 134 ); prions (such as bovine spongiform encephalopathy; Chapter 371 ); bacteria (e.g., Salmonella [ Chapter 284 ], Campylobacter [ Chapter 279 ], Listeria [ Chapter 272 ]; and Brucella [ Chapter 286 ]); protozoa (such as Cyclospora [ Chapter 324 ], Cryptosporidium [ Chapter 321 ], Toxoplasma [ Chapter 320 ], and Giardia [ Chapter 322 ]); and helminths (such as Taenia [ Chapter 325 ], Trichinella [ Chapter 327 ], Opisthorchis [ Chapter 326 ], and Clonorchis [ Chapter 326 ]).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here