Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Rehabilitation of the postmastectomy patient produces problems of varying complexity. This chapter reviews commonly used approaches for the care of postmastectomy wounds and addresses the complications encountered in these patients. The goals of postoperative care are to anticipate and prevent adverse events and to accelerate recovery.
The various operative techniques used in the treatment for breast carcinoma are described elsewhere in this text. Complications after any operation can be minimized with thorough preoperative evaluation, meticulous technique, hemostasis, and wound closure. In addition to the standard oncologic evaluation, preoperative evaluation includes assessment of the patient’s overall physiologic condition, with particular emphasis on tolerability of anesthesia, uncontrolled diabetes, hypertension, anemia, coagulopathy, and steroid dependency.
Technique at operation and wound closure is an essential part of wound repair. Meticulous hemostasis must be confirmed before closure. Closed-suction drains should be placed into the mastectomy wound site, because most patients will develop a seroma. We prefer closed-suction catheter drainage of the mastectomy wound, commercially available as Blake (Ethicon, Johnson & Johnson Health Care Systems, Piscataway, NJ) or Jackson-Pratt tubing (Baxter Healthcare, Deerfield, IL), and each system should be appropriately placed at operation to allow superomedial and inferolateral positioning to ensure thorough, dependent aspiration. After the wound is closed, the tubing is connected to a closed-suction system to ensure removal of all wound contents (e.g., clots, serum). Suction catheter drainage, as a rule, is necessary for 5 to 10 days postoperatively. Earlier removal of the catheters is allowed only when the function of this closed-system technique is compromised. Routinely, catheters are removed only when less than 30 mL of serous or serosanguineous drainage is evident for two consecutive 24-hour intervals.
The skin is closed in two layers using absorbable suture. Thereafter, the skin margins may be covered with strips of surgical tape or wound adhesive. A light, dry gauze dressing is applied to the incision. Pressure dressings over the dissected skin flaps are unnecessary and do not decrease the amount and rate of seroma formation. Negative-pressure wound therapy may have a role in reducing postmastectomy wound complications, particularly in those having prosthetic breast reconstruction. Postoperatively, the wound is carefully inspected with regard to flap adherence, and the patient is encouraged to resume preoperative activity.
In most circumstances, the breast cancer patient is allowed to begin the gradual resumption of presurgical activities. Younger women usually regain full range of motion of the arm and the shoulder soon after drain removal, whereas some older patients may require intense (supervised) exercise for several months before attaining their former levels of activity. Visits from volunteers of the American Cancer Society or the Visiting Nurse Association are of particular value for psychosocial and physical recovery of the postmastectomy patient.
Mastectomy has traditionally been a safe operation with low morbidity and mortality. Although the incidence of postoperative complications is low, physicians should be aware of the morbidity unique to mastectomy and axillary node dissection.
An analysis of National Surgical Quality Improvement Program data recently reported that return to the operating room was the most common morbidity after breast surgery, followed by superficial and deep surgical site infections. Complications can lead to readmissions after mastectomy. A recent report demonstrated a readmission rate of 5.59% after breast surgery, with infections being the most common indication for readmission. A detailed review of complications after mastectomy is outlined in the following sections.
Lymphedema affects 6% to 30% of all patients who have had a modified radical mastectomy (MRM) and is a lifelong risk after the procedure. Lymphedema occurs as a consequence of the en bloc ablation of lymphatic routes (nodes and channels) within the field of resection of the primary mammary tumor. The subsequent increase in plasma hydrostatic pressure that results with removal of these conduits may follow the surgical procedure, irradiation, or uncontrolled progression of neoplasm. Injury, capillary disruption, infection, obstruction to lymphatic or venous outflow, hyperthermia, or exercise will accelerate protein leakage into these tissues. The incidence of lymphedema may be significantly reduced by the use of the axillary reverse mapping procedure advocated by Thompson and colleagues. Lymphaticovenous bypass done at the time of axillary lymph node dissection can also be useful in reducing the incidence of lymphedema.
Previous attempts to evaluate the degree of arm lymphedema have been classified by Stillwell according to the percentage of volume increase. This methodology has been subsequently investigated and further refined. We grade an increase of less than 10% in arm volume as mild, whereas an increase of greater than 80% is classified as severe.
Factors that have been identified as risk factors for the development or progression of lymphedema include the extent of axillary dissection, the use of axillary radiotherapy, pathologic nodal status, infection or injury, and obesity. Gilchrist stresses the importance of free and complete active range of motion of the arm and shoulder in the early postoperative period. Traditionally it has been believed and taught that avoidance of excessive sun exposure, injections, infections, or other potentially active or passive injury to the ipsilateral extremity is paramount to prevent lymphedema. Two recent studies, however, have challenged this notion. A study by Ferguson and colleagues involved prospective evaluation of a large cohort of breast cancer patients. Factors associated with lymphedema development include high body mass index, cellulitis, prior axillary node dissection, and regional radiation therapy. These authors found no association between injections in the arm, blood pressure measurements in the arm, air travel, or trauma and lymphedema. This is similar to the findings in the Physical Activity and Lymphedema (PAL) trial, which showed no association between blood draws, blood pressure measurements, or air travel and lymphedema risk. Further study is warranted to further define the optimal balance of lifestyle management, upper extremity precautions, and lymphedema risk.
Furthermore, early recognition of incipient edema by the patient and immediate physical therapy with compression massage often alleviates and augments the prophylaxis of further edema. When lymphedema is severe, the mechanical expression of tissue fluid, with application of an intermittent pneumatic compression device, may be helpful, although a recent small, randomized trial has questioned its value compared with conservative measures. The physician may wish to prescribe antibiotics if there is evidence of supervening cellulitis. The arm should be elevated above heart level when the patient is inactive. A more thorough discussion of medical, mechanical, and surgical treatment of chronic lymphedema is provided in Chapter 36 .
Wound infection after mastectomy has been reported to be between 1% and 20%. A large 2012 study from the Mayo Clinic reported infection rates between 2.7% and 8.0% depending on the definition of wound infection used. Infectious complications have been shown to be more common in patients having bilateral mastectomy than unilateral mastectomy.
Infection of the mastectomy wound or ipsilateral arm may represent serious morbidity in the postoperative patient and produces an immediate disability that may progress to late extensive tissue dissection that creates thin, devascularized skin flaps. Thereafter, progressive tissue necrosis provides a medium that supports bacterial proliferation with invasive tissue infection. Early debridement of obviously devascularized tissue is an important prophylactic adjunct to prevent progressive invasive infection. When abscess formation does occur, attempts should be made to culture the wound for aerobic and anaerobic organisms, with immediate Gram stain of identifiable strains to document the bacterial contaminant. The predominant organisms are Staphylococcus aureus and Staphylococcus epidermidis .
A meta-analysis examining five prospective randomized controlled trials of preoperative prophylactic antibiotics versus placebo demonstrates that prophylactic antibiotics in breast surgery substantially reduce the incidence of postoperative wound infections without any adverse sequelae from the antibiotic administration. We currently use a first-generation cephalosporin before the incision (given intravenously within 30 minutes before the incision) in patients undergoing a mastectomy. Furthermore, it is suggested that reducing postoperative infections is important to prevent delays in adjuvant therapy and reduce cost.
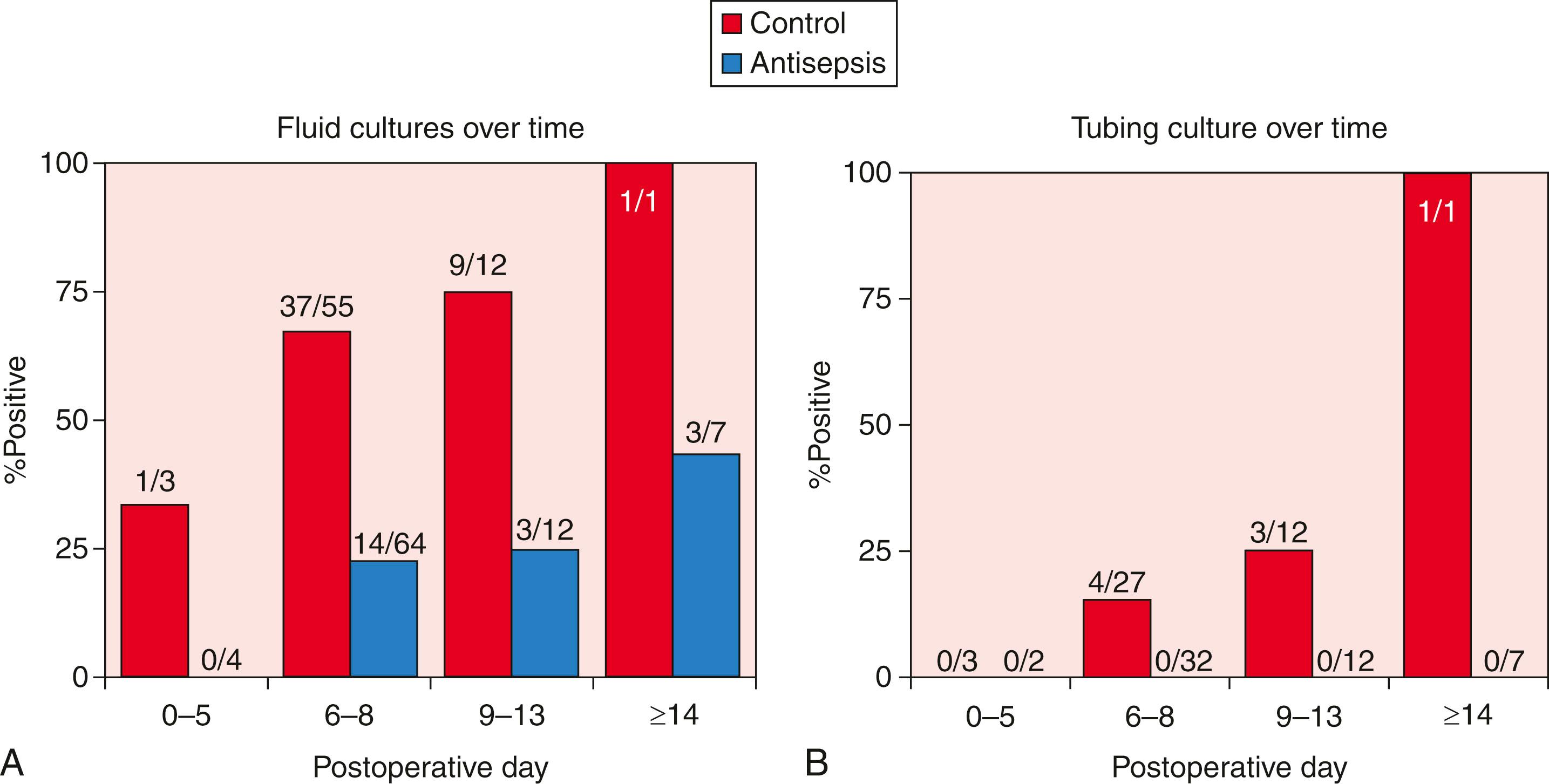
Recent data have suggested that drain antisepsis may have an important role in reducing wound infections after breast surgery. Degnim and colleagues demonstrated that drain bulb irrigation with a dilute sodium hypochlorite solution can significantly reduce bacterial colonization of the drain ( Fig. 37.1 ). Furthermore, in a randomized trial, the technique of drain bulb irrigation combined with the use of chlorhexidine disc dressing was associated with a significant reduction in postoperative infections in breast cancer patients.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here