Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
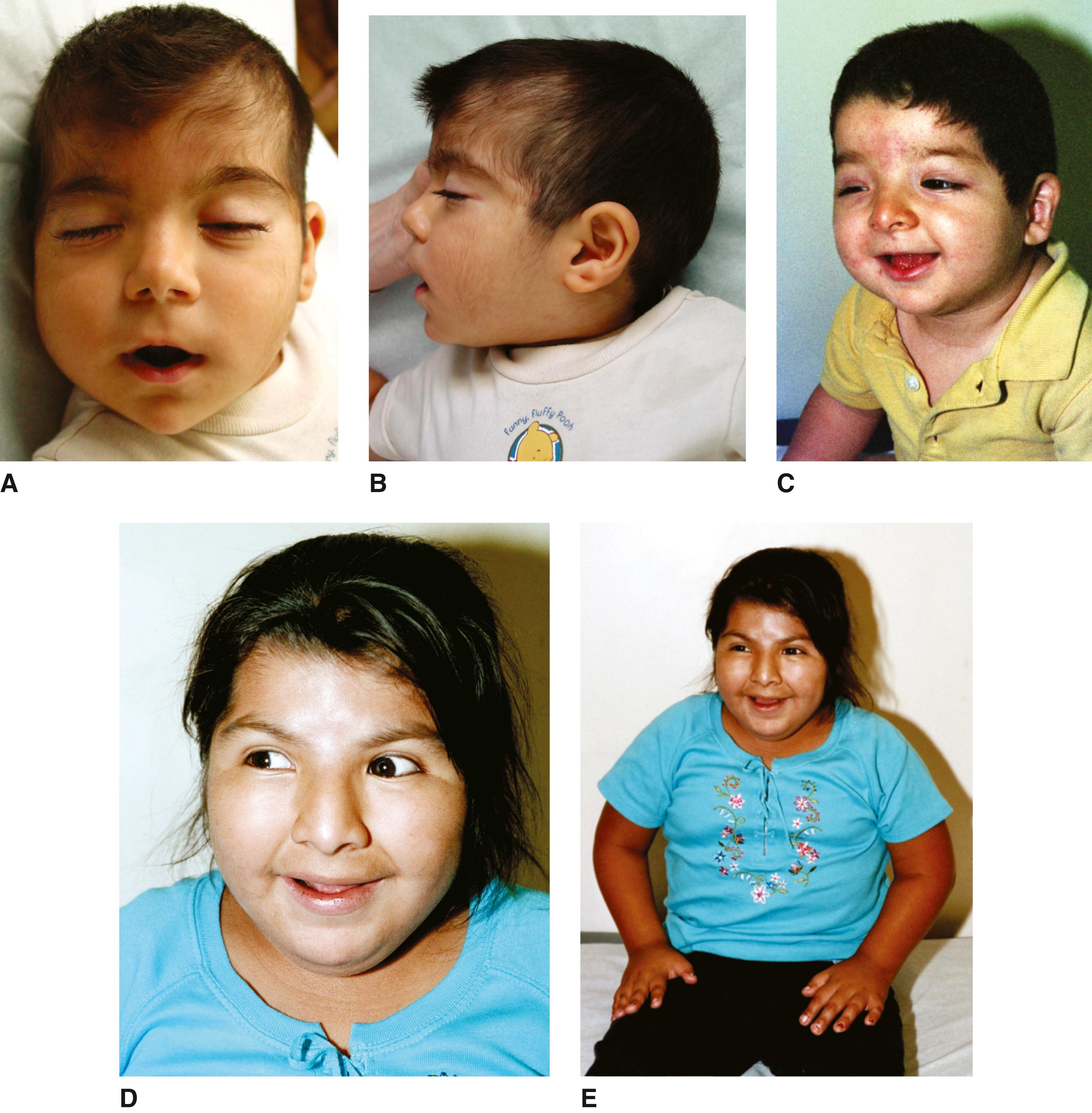
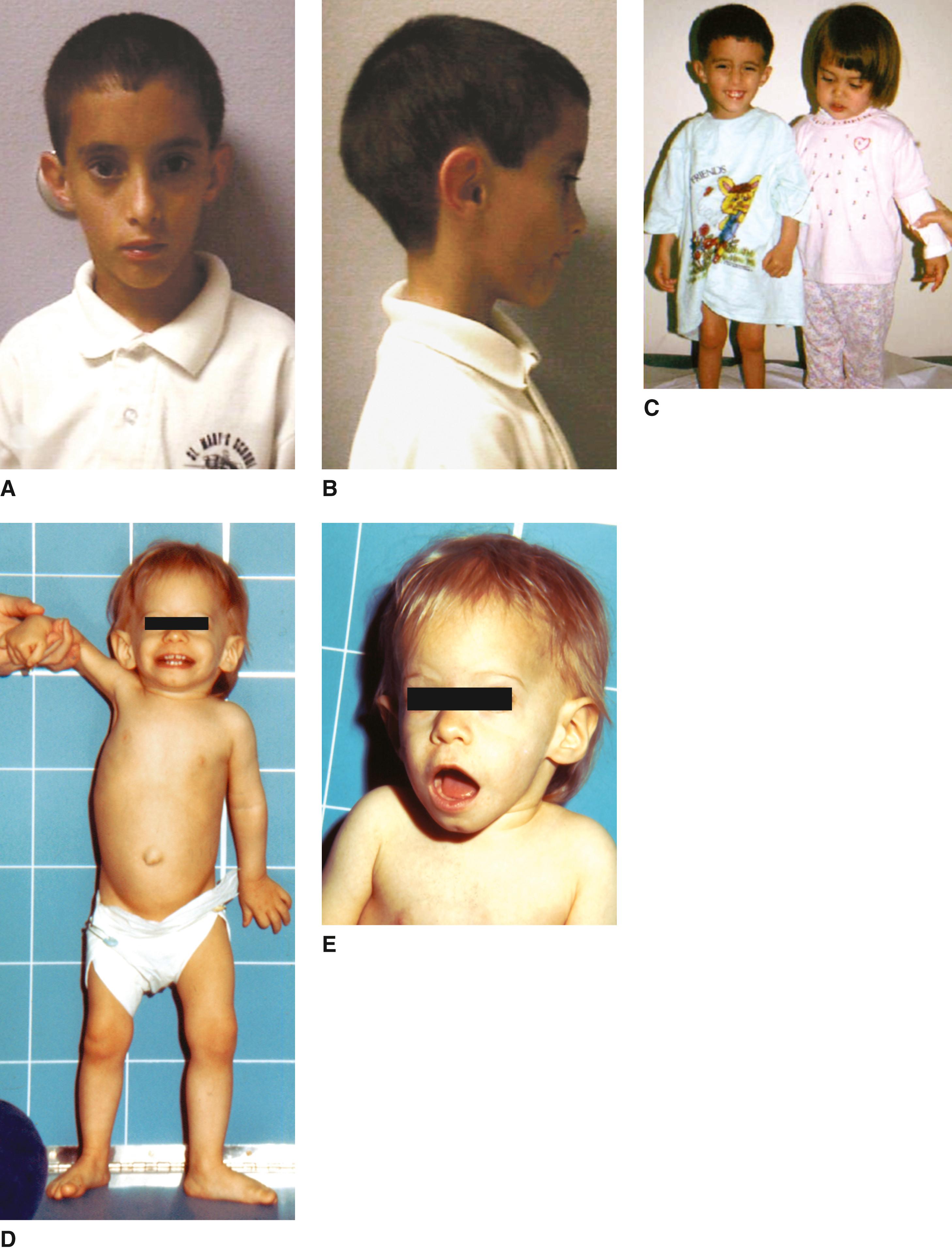
The syndrome was originally reported in 1933 by Cornelia de Lange, although Brachmann described a child with similar features at autopsy in 1916. As the molecular etiology of this condition has been elucidated, both a classic as well as nonclassic phenotypes are recognized. The disorder is now known to be caused by variants of seven genes, all of which have a regulatory or structural function in the cohesin complex. Percentages of features listed below refer to the classic cases.
Growth. Prenatal onset growth deficiency with length and weight less than the 10th percentile. Mean adult height 156 cm (males) and 131 cm (females), retarded osseous maturation (100%).
Performance. Intellectual disability and sluggish physical activity. Average intelligence quotient (IQ) ranges from below 30 to 86, with an average of 53. Those with higher IQs tend to have a higher birth weight and head circumference and less severe malformations. Initial hypertonicity (100%); low-pitched, weak growling cry in infancy (74%); high pain tolerance, severe speech and language delays, autism spectrum disorders, seizures (23%); broad-based gait.
Behavior. Hyperactivity, short attention span, aggression, self-injurious behavior, extreme shyness, anxiety, depression, obsessive-compulsive behavior, perseveration, sleep disturbance, circadian rhythm disorders.
Craniofacial. Microbrachycephaly (93%); bushy eyebrows and synophrys (98%), long, thick, curly eyelashes (99%), arched eyebrows (98%); ptosis; high myopia; peripapillary pigmentation; microcornea; tear duct malformation; depressed nasal bridge (83%); anteverted nares (85%); long philtrum, thin upper lip, and downturned angles of mouth (94%); high-arched palate (86%); late eruption of widely spaced teeth (86%); thick dysplastic posteriorly rotated ears; micrognathia (84%); prominent symphysis (66%).
Skin. Hirsutism (78%), cutis marmorata and perioral pale “cyanosis” (56%), hypoplastic nipples and umbilicus (50%), low posterior hairline (92%).
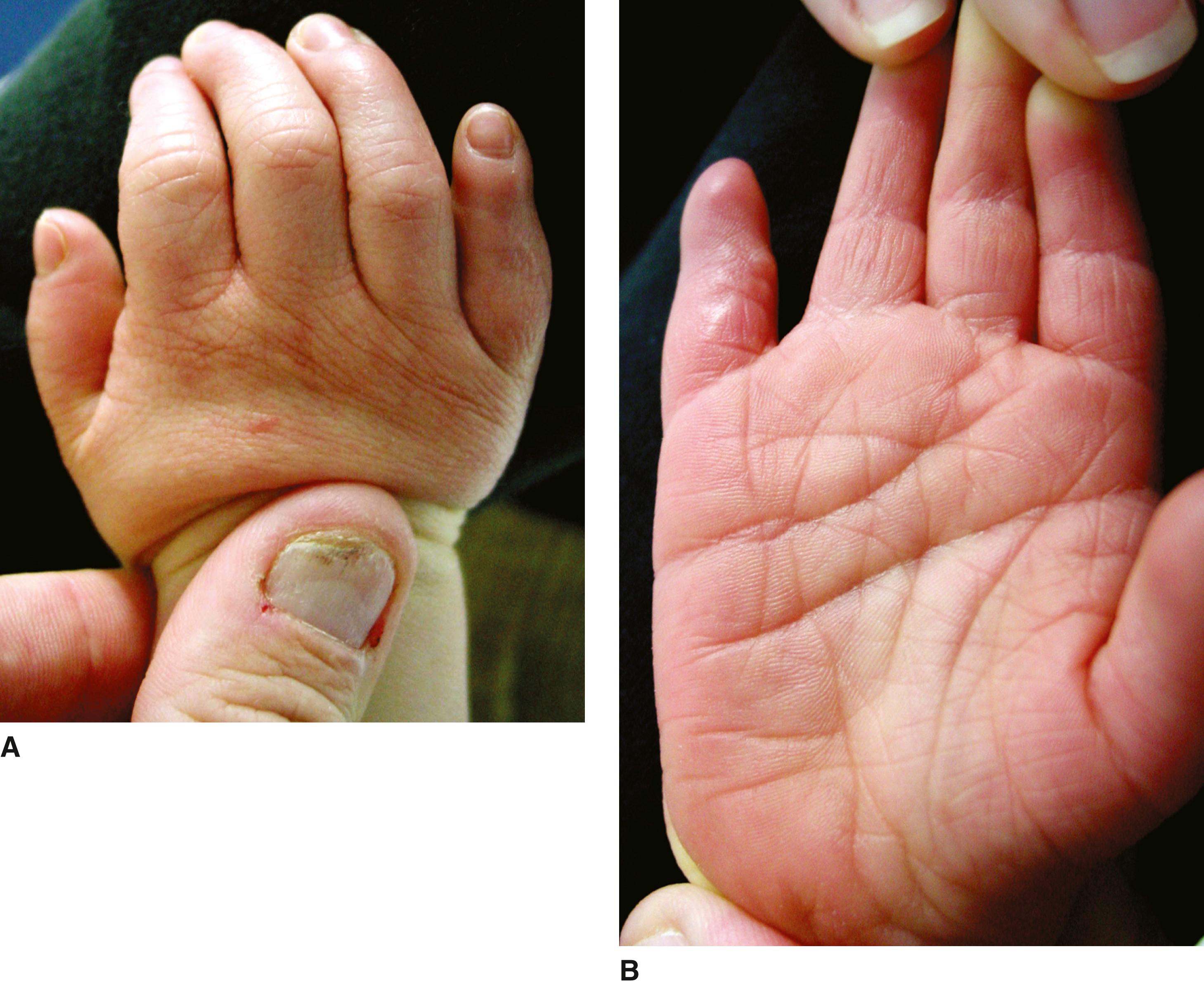
Limbs. Micromelia (93%), phocomelia and oligodactyly (27%), clinodactyly of fifth fingers (74%), single transverse palmar crease (51%), proximal implantation of thumbs (72%), flexion contracture of elbows (64%), syndactyly of second and third toes (86%), cold extremities.
Genitalia. Hypoplasia in males (57%), undescended testes (73%), hypospadias (33%), hypoplastic labia majora.
Gastrointestinal. Gastroesophageal (GE) reflux (>90%), Barrett esophagus (10%), malrotation with risk for volvulus (>10%).
Imaging. Mandibular spur present up to 3 months of age, dislocated/hypoplastic radial head, hypoplastic first metacarpal and fifth middle phalanx, short sternum with precocious fusion and 13 ribs, enlarged cerebral ventricles, white matter atrophy.
Other. Strabismus, nystagmus, blepharitis; short neck (66%); cleft palate (20%); submucous cleft palate (14%); hearing loss secondary to canal stenosis; ossicular malformation or cochlear anomaly (60%); congenital heart defects (33%); structural renal anomalies; thrombocytopenia, including idiopathic thrombocytopenic purpura.
Astigmatism, optic atrophy, coloboma of the optic nerve, cataracts, Coats disease, proptosis, choanal atresia, hypertrophic cardiomyopathy, later-onset dysplastic heart valves, hiatus hernia, diaphragmatic hernia, pyloric stenosis, brachyesophagus, esophageal adenocarcinoma, inguinal hernia, hematometra, split foot, scoliosis, leg length inequality, absent second to third interdigital triradius, thoracic meningocele.
These patients show a marked retardation of growth, evident by the time of birth and, as a rule, they fail to thrive. Feeding difficulties, including regurgitation, projectile vomiting, chewing, and swallowing difficulties, often continue well beyond 6 months. Because of the extremely high rate of GE reflux and intestinal malrotation, search for these features in infancy is critical. Although a high percentage of affected children have severe intellectual disability, a significant number have a much higher potential relative to performance than earlier studies have suggested, particularly among those less classically affected. Hearing loss and visual disturbances are common. Blepharitis improves with age. Chronic sinusitis may be lifelong. Puberty occurs at the normal time, although it may be incomplete with irregular menses being common. Adults are small and have a tendency toward obesity. There is some evidence of early aging in adults. Early long-term sequelae of GE reflux, including Barrett esophagus and esophageal adenocarcinoma, have been seen. Episodes of aspiration in infancy, apnea, complications related to bowel obstruction, diaphragmatic hernia, and cardiac defects appear to constitute the major hazards for survival in these patients.
Cornelia de Lange syndrome (CdLS) is a result of mutations in one of seven cohesion-associated genes. Mutations in NIPBL , located at 5p13, cause 65% of cases, whereas deletions account for 5%. This gene functions in an autosomal dominant fashion. Most cases are sporadic and there is marked variability in expression. Mutations in SMC1A , located at Xp11.22, are responsible for 5% of cases. This gene is inherited in an X-linked manner and accounts for many of the familial, as well as many of the milder, cases observed. HDAC8 variants have been reported in 65 individuals with both classic and nonclassic phenotypes. Distinctive features include ocular hypertelorism, a large anterior fontanel, and a happy personality. The gene is located on the X chromosome. ANKRD11 variants have been reported in five individuals, all having a nonclassic phenotype. RAD21 variants have been reported in 23 individuals with this disorder. BRD4 variants have been reported in a small number of cases; one case with a mutation in SMC3 at 10q25 has been published. Mosaicism occurs frequently in this disorder. Of individuals with classic features, 15% to 20% have mosaic NIPBL. It is expected that mutations in other cohesin-related genes will be identified.
Based on the cardinal clinical features, diagnostic criteria for CdLS have been established:
Cardinal features include (1) Synophrys and/or thick eyebrows; (2) short nose with low nasal bridge and/or upturned nasal tip; (3) long and/or smooth philtrum; (4) thin upper lip and/or downturned corner of mouth; (5) hand oligodactyly and/or adactyly; (6) diaphragmatic hernia (two points are given for each feature present).
Suggestive features include global development delay and intellectual disability, prenatal growth retardation, postnatal growth retardation, pre- or postnatal microcephaly, small hands and/or feet, short fifth fingers, hirsutism (one point is given for each feature present).
Clinical scores:
≥11 points, of which at least 3 are cardinal: =Classic CdLS;
9 or 10 points of which at least 2 are cardinal: Nonclassic CdLS:
4 to 8 points of which 1 is cardinal: molecular testing for CdLS is indicated:
<4 points: insufficient to indicate molecular testing for CdLS.

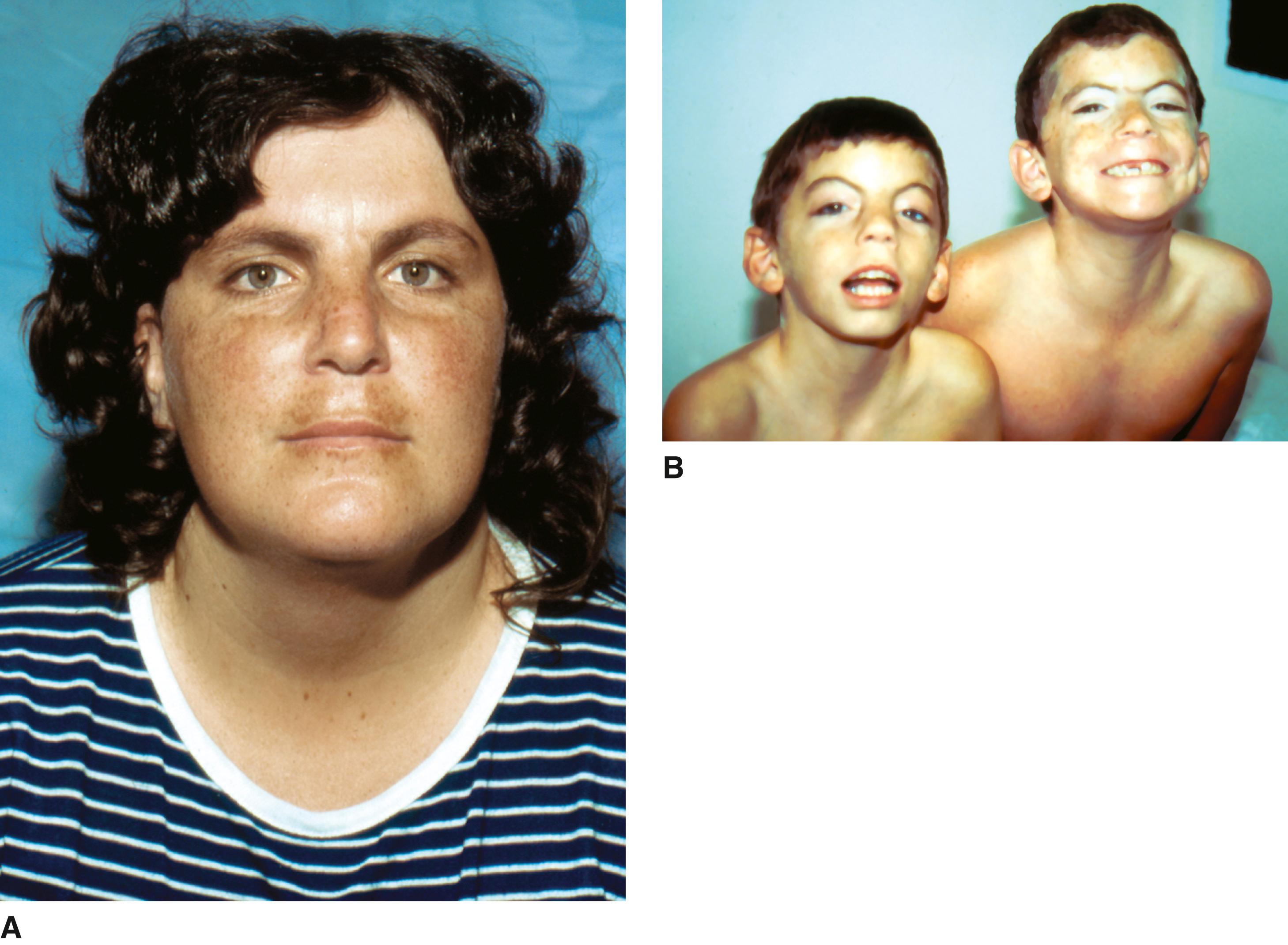
Rubinstein and Taybi set forth this clinical entity in 1963. This disorder is rare, occurring with an estimated frequency of 1 in 100,000 to 1 in 125,000 newborns.
Growth. Postnatal onset of growth deficiency; in adults, average height of 153 cm in males and 147 cm in females; average weight of 48 kg in males and 55 kg in females. Retarded osseous maturation (74%).
Performance. IQ 30 to 79, with an average of 51; 52% have an IQ less than 50. Speech difficulties (90%), seizures (23%; however, 57% have an abnormal electroencephalogram [EEG]); stiff, unsteady gait (85%); hypotonia (67%); hyperreflexia (40%).
Behavior. Social and friendly in childhood with short attention span, attention-deficit/hyperactivity disorder, motor stereotypies. In adults, anxiety, depression, mood instability, and aggressive behavior.
Craniofacial. Microcephaly (35%), large anterior fontanel (41%), delayed closure of fontanel (24%), frontal bossing (33%), frontal hair upsweep (20%), low anterior hairline (24%), low posterior hairline (42%), downslanting palpebral fissures (88%; however, only half of children younger than age 5 will manifest this); maxillary hypoplasia with narrow palate (100%), small mouth (56%); prominent or beaked nose with or without nasal septum extending below alae nasi and short columella (90%), deviated nasal septum (71%); micrognathia (49%); low-set and/or malformed ears (84%); heavy eyebrows (76%), highly arched eyebrows (73%), long eyelashes (87%); nasolacrimal duct stenosis (43%); ptosis (36%); epicanthal folds (55%); strabismus (69%); enophthalmos (22%).
Limbs. Broad thumbs with radial angulation (87%), broad great toes (100%), other fingers broad (87%), fifth finger clinodactyly (62%), persistent fetal fingertip pads (31%), deep plantar crease between first and second toes (33%), flat feet (72%).
Other skeletal. Scoliosis (42%), cervical hyperkyphosis (37%).
Imaging. Spina bifida occulta (47%), small flared iliac wings (26%).
Genitourinary. Cryptorchidism (78% of males), renal anomalies (52%).
Skin. Hirsutism (75%), capillary hemangioma (25%), keloid formation (22%).
Cardiac. Defects, most frequent of which are patent ductus arteriosus, ventricular septal defect, and atrial septal defect, occur in approximately one-third of cases.
Cataract, glaucoma, ocular coloboma, nystagmus, myopia, Duane retraction syndrome, exophthalmia, talon cusps of teeth, enamel hypoplasia, posterior helical pits, cardiac conduction defects, camptodactyly, polydactyly, syndactyly, simian crease, distal axial triradius, duplicated halluces, patellar dislocation, dislocation of radial head, Perthes disease, bifid uterus, paratubal cystadenoma, pectus excavatum, sternal anomalies, angulated penis, hypospadias, shawl scrotum, Hirschsprung disease, eosinophilic esophagitis, café au lait spots, stereotypic movements, mirror movements, hypohidrosis, obstructive sleep apnea, absence of corpus callosum, large foramen magnum, parietal foramina, Chiari I malformation and syrinx, tethered cord, mediastinal vascular ring, premature thelarche, thyroid hypoplasia, cerebral artery dissection, tumors (neuroblastoma, medulloblastoma, oligodendroglioma, meningioma, pheochromocytoma, thyroid cancer, rhabdomyosarcoma, leiomyosarcoma, seminoma, odontoma, choristoma, pilomatrixomas).
Infancy and childhood are complicated by respiratory infections, obstipation, and feeding difficulties. A poor polysaccharide antibody response has been demonstrated in a few patients. Aggressive assessment and treatment of gastroesophageal reflux are warranted. Constipation is very common. Global developmental delay is universal, with most patients testing in the severe to moderate range of intellectual disability. However, performance outside of this range has been reported. Recurrent ear infections with hearing loss and dental problems primarily associated with overcrowding of the teeth occur frequently. Hand and/or foot surgery frequently improves grasp, oppositional function, and comfort. Unusual reactions to anesthesia (respiratory distress and cardiac arrhythmias) have been reported, as well as tracheal collapse after muscle relaxants. Scoliosis may develop in childhood. Management of ingrown toenails and early treatment of paronychia are warranted. More than 90% of affected individuals survive into adulthood and most achieve some independence in self-care and communication. Obesity, eating issues, obstructive sleep apnea, and keloids are common problems for adults. There is some suggestion that adults may have decreased abilities over time. Affected individuals have an increased risk for a variety of benign and malignant tumors, although no screening protocol has been recommended.
The majority of cases (>99%) are sporadic. Mutations in two genes, CBP (CREB binding protein) in 60% of clinically diagnosed cases and EP300 in 8% to 10%. The preponderance of affected individuals with a known molecular abnormality have point mutations or small deletions or insertions in CBP at 16p13.3. Translocations, inversions, and large deletions involving contiguous genes at 16p13.3 have also been described, and some evidence indicates that large deletions are associated with a more severe phenotype and increased mortality. The clinical phenotype in patients with EP300 mutations is usually less severe than the CBP phenotype, with the exception of the nasal columella protruding below the alae nasi. Also different between the clinical phenotypes associated with the two genes, angulation of the thumbs and halluces is extremely uncommon in the EP300 phenotype. A risk for recurrence of 0.5% to 1% for unaffected parents of an affected child has been suggested based on the finding of somatic mosaicism and variable expression in a few families.
Interstitial duplication of 16p13.3, including the gene CBP, has been reported in several patients, causing intellectual disability, a recognizable dysmorphic phenotype of midface hypoplasia, a prominent nose with bulbous tip, upslanting short palpebral fissures, thin upper lip, protruding ears, proximally placed short thumbs, camptodactyly of fingers and toes, and talipes equinovarus. Tetralogy of Fallot, atrial septal defect, vertebral fusions, and other anomalies have been noted. Normal growth is common.

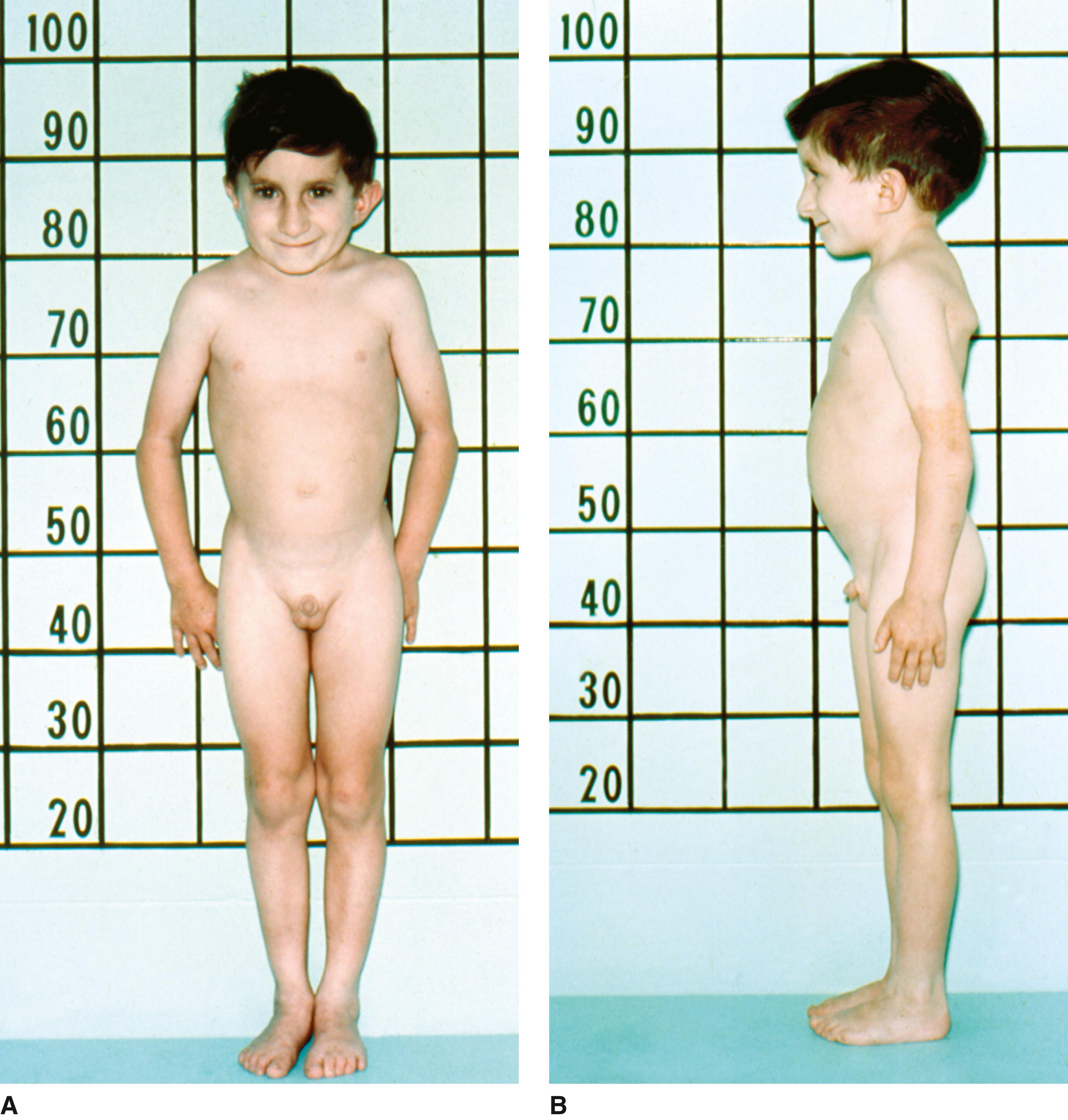
Pelletier and Feingold described the initial patient with this disorder in 1973. One year later, Leisti and colleagues reported a child with almost identical features and suggested the term “Floating-Harbor syndrome,” an amalgam of the names of the hospitals where the initial two patients were evaluated (Boston Floating and Harbor General, Torrance, California). Approximately 50 patients have been reported with this condition.
Growth. Birthweight and length at third percentile; postnatal growth deficiency, delayed bone age.
Performance. Severe speech and language delay; borderline normal to moderate intellectual disability; behavior problems, including hyperactivity, poor attention span, and aggression.
Craniofacial. Short palpebral fissures with deep-set eyes; triangular shape to nasal tip; wide mouth with downturned corners; low-set, posteriorly rotated ears. In midchildhood the nose becomes bulbous with a prominent nasal bridge, the columella becomes broad, the philtrum short and smooth, and the vermilion border thin.
Other. Low posterior hairline, short neck, broad chest, fifth finger clinodactyly, brachydactyly, clubbing, broad thumbs, joint laxity.
Microcephaly, trigonocephaly owing to metopic suture synostosis, dental problems, abnormal electroencephalograph, pulmonary stenosis, tetralogy of Fallot with atrial septal defect, adult-onset hypertension, triangular face, rib anomalies, high-pitched voice, preauricular pit, delayed motor skills, accessory or hypoplastic thumb, subluxated hypoplastic radial head, cone-shaped epiphyses, Perthes disease, clavicular pseudoarthrosis, celiac disease, abdominal distention, constipation, hirsutism, long eyelashes, spinal dysraphism, cerebral aneurysm, postpubertal menorrhagia, precocious puberty, growth hormone deficiency, hypothyroidism.
The facial features are most recognizable in midchildhood. During childhood, height and weight tend to parallel the third percentile. The speech difficulties are severe and relate primarily to motor speech production. A slurred quality to the speech is characteristic. Hypernasality is common and often associated with velopharyngeal incompetence. The majority of children are in special education settings. The three adults live in assisted living situations and hold part-time jobs in unskilled positions and have elementary literacy skills.
This disorder presumably has an autosomal dominant inheritance pattern. Mutations in SRCAP , which encodes SNF2-related CREBB activator protein, are responsible. SRCAP serves as a coactivator for CREB-binding protein (CREBBP), which is also known as CBP.
CBP is the gene responsible for Rubinstein-Taybi syndrome, which has a number of phenotypic similarities to those of Floating-Harbor syndrome.
This pattern of malformation was described independently by Silver and colleagues and by Russell in 1953 and 1954. Silver emphasized the skeletal asymmetry as a feature of the disorder. This was a variable finding in the patients described by Russell. Diagnostic criteria were established by Wakeling and colleagues. Features are most apparent in infancy and early childhood. It is probable that this condition is both under- and overdiagnosed.
Growth. Small stature, of prenatal onset with length and weight usually equal to –2 SD, minimal postnatal catch-up growth; immature osseous development in infancy and early childhood, preservation of head circumference (relative macrocephaly); asymmetry.
Performance. Mild global delay, speech delay.
Craniofacial. Small, triangular facies with frontal prominence, late closure of the anterior fontanel, downturned corners of mouth; facial asymmetry, possible bluish sclerae in early infancy, low-set posteriorly rotated ears, and micrognathia; eye findings include visual refractive errors, strabismus, and tortuous retinal vessels.
Skin. Café au lait spots.
Limbs. Asymmetry, short incurved fifth finger.
Other. Tendency toward excess sweating, especially on the head and upper trunk, during infancy; liability to fasting hypoglycemia from about age 10 months to age 2 to 3 years.
Metopic craniosynostosis, iris coloboma, cleft palate, bifid uvula, velopharyngeal insufficiency, syndactyly of second to third toes, camptodactyly, radial hypoplasia, limited elbow supination, absent thumb, scoliosis, Sprengel deformity, hip dysplasia, talipes equinovarus, renal anomaly, posterior urethral valves, hypospadias, cryptorchidism, clitoromegaly, and inguinal hernia; cardiac defects; malignancy, including craniopharyngioma, testicular seminoma, hepatocellular carcinoma, and Wilms tumor; gastrointestinal abnormalities, including gastroesophageal reflux, esophagitis, and food aversion; growth hormone deficiency.
Affected children have prenatal-onset growth deficiency and typically do not catch up postnatally. Feeding difficulties are seen in 86% and include weak suck, absence of hunger, gastroesophageal reflux, and food aversion. There tends to be a gradual improvement in growth, weight, and appearance during childhood and especially during adolescence. Most school-age children eat normally. As a result, the adult usually appears more normal than the infant with this disorder. Final height attainment can be up to 5 feet. Slow motor development is common. Approximately one-third have learning disabilities. Because of the small facies, the upper head may appear large, although head circumference is well within the normal range. This appearance, plus the relatively large fontanels in early infancy, may give rise to a false impression of hydrocephalus, which is not the case. Somewhat frequent feedings and adequate glucose intake during illness should be ensured from age 6 months until age 3 years, the period of enhanced liability to fasting hypoglycemia. Growth hormone (GH) deficiency should be considered if the linear growth rate reaches a plateau. GH treatment has been shown to be of benefit in these patients, even in the absence of GH deficiency.
The majority of cases are sporadic. The condition is genetically heterogeneous. A molecular etiology is identified in up to 60% of patients. Roughly 50% will manifest hypomethylation of the paternal allele of the H19 gene on chromosome 11p15 associated with imprinting control region 1 (ICR1), which includes H19 and IGF2 . Maternal uniparental disomy for chromosome 7 (mar UPD7) accounts for 5% to 10% of cases. UPD7 may be complete or segmental (7p11.2-p13 and 7q31-qter appear to be the critical regions). Other molecular mechanisms include translocations, maternal UPD11, paternal deletions at 7q32, maternal inheritance of duplications within ICR1 and/or ICR2 on11p15, and multilocus hypomethylation. A small number of patients with submicroscopic deletions or duplications in these imprinted regions have also been described. The remainder are of unknown etiology. Several cases with maternally inherited microduplications or translocations have been familial.
Negative results warrant consideration of further testing for CNVs, chromosome 14q32 methylation abnormalities (associated with Temple syndrome, see below), matUPD20, matUPD16, CDKN1C and IGF2 mutations, and multilocus imprinting disturbances.
Molecular abnormalities at the paternally methylated imprinted locus on chromosome 14q32, including mat UPD14, paternal microdeletions, and hypomethylation of the DLK1/GTL2 IG-DMR result in Temple syndrome, which has significant overlap with SRS and is associated with being small for gestational age, postnatal growth deficiency, hypotonia, delay of motor skills, and early puberty as well as small hands and feet.
Patients scoring four or more of six cardinal clinical criteria including small for gestational age (either birthweight or birth length), postnatal growth deficiency, relative newborn macrocephaly, protruding forehead, body asymmetry, and feeding difficulties and/or low body mass index (BMI) should be considered to have a clinical diagnosis of SRS if two of the features are prominent forehead and relative macrocephaly. Conversely it is unlikely that patients with less than four of the six cardinal clinical criteria have SRS. However, it is recommended that molecular testing be done in patients with only three of six criteria because patients with mat UPD7 have fewer clinical features of SRS than patients with some other molecular phenotypes. Finally, it is important to recognize that a negative molecular test does not exclude a diagnosis of SRS.
Silver-Russell syndrome has been associated with the use of assisted reproductive technologies, although the reason for this apparent relationship remains obscure.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here