Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Vertical partial laryngectomy (VLP) is used for cancers extending to or crossing the anterior commissure. Hence the resection as typically performed entails removal of several millimeters of the contralateral vocal cord as well as the midline portion of the thyroid cartilage. This procedure is not actually a “hemi” laryngectomy as it has been termed traditionally, since: the cricoid ring remains intact, the hyoid bone is uninvolved, and usually typically only a portion of the arytenoid is resected.
“Frontolateral partial laryngectomy” or “vertical partial laryngectomy” is a more accurate designation for the procedure.The procedure removes all or a portion of one vocal cord, usually in continuity with the anterior commissure and its ligamentous attachment to the thyroid cartilage. The removal of at least the vocal process (or even the entire) ipsilateral arytenoid is required. In addition, sufficient tissue must be retained or brought in as local flaps to maintain an adequate airway, and the voice is always adversely affected.
The technique was popularized in the United States by Dr. Joseph Ogura’s group in the early 1970s (see Additional Sources for original references ). At that time, imaging and radiotherapy techniques were not as precise as they are currently; hence many surgeons preferred surgical excision to radiotherapy for cancers encroaching on the anterior commissure. Detection of persistent disease following radiotherapy is often delayed, requiring a total laryngectomy. A report from our department indicated that more larynges were preserved by initial partial laryngectomy for early glottic cancer than with radiotherapy with surgical salvage. VPL is performed for bulky or extensive early-stage glottic carcinoma, which have a reduced chance of cure with radiotherapy.
The widespread use of transoral endoscopic laser surgery, increased numbers of surgeons competent in performance of supracricoid laryngectomy, improved imaging, precise targeting of radiation therapy, and more recently the introduction of robotic surgery have decreased the use of VPL in the treatment of glottic cancer.
Laccourreye et al. compared outcomes of a series of patients with early glottic carcinoma managed with supracricoid laryngectomy with VPL, noting improved disease-free and survival benefit with the group treated with supracricoid laryngectomy.
As noted previously, many recently trained otolaryngologists have no experience with VPL in their residency. Nonetheless, the procedure remains standard in locales that do not have access to these newer modalities or for surgical salvage in selected cases following laser resection or radiation for early glottic cancers.
VLP for early glottic cancer has largely been replaced by endoscopic laser excision or supracricoid laryngectomy.
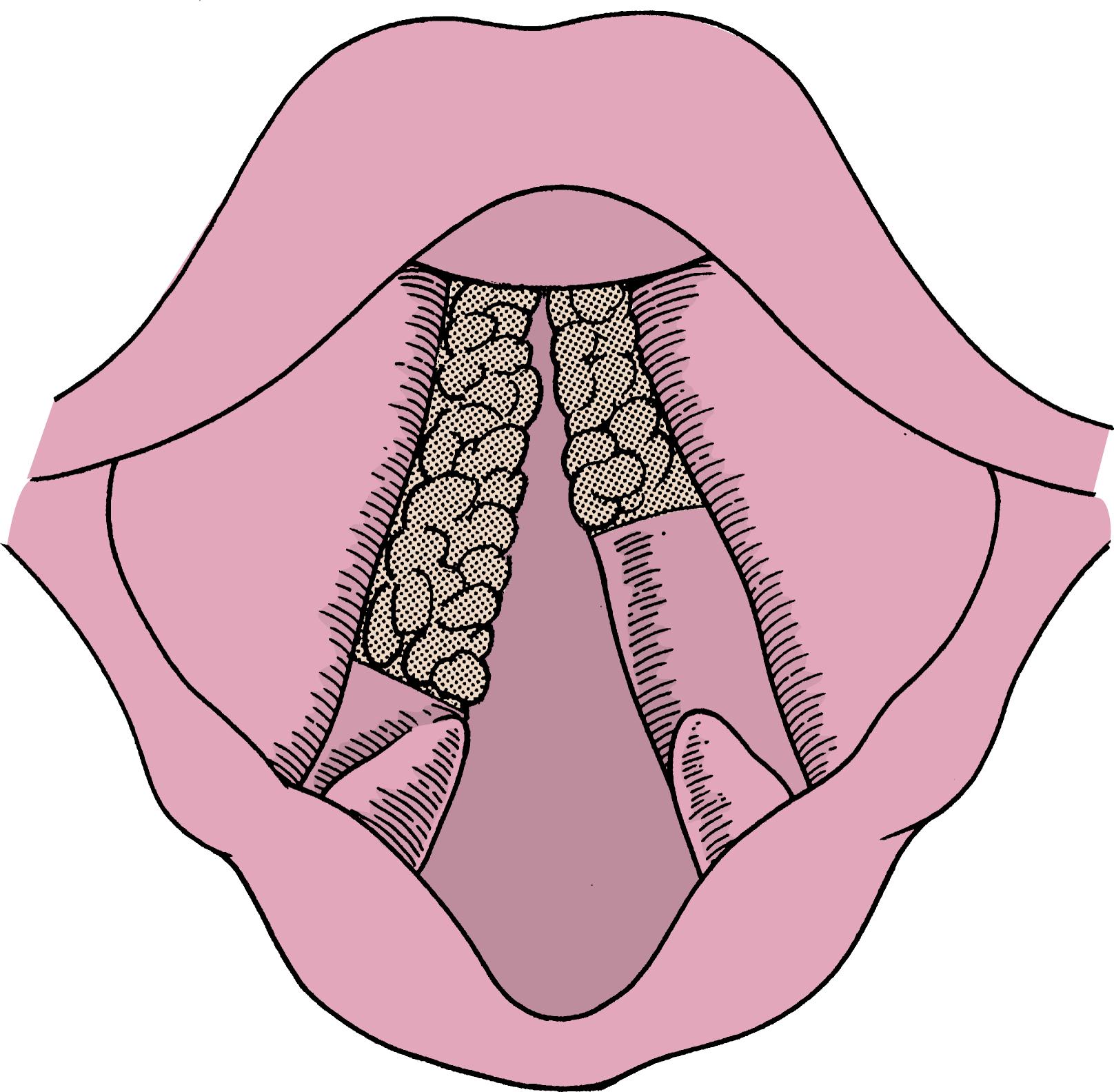
It is ideal for bulky glottic cancers that involve the anterior commissure and are confined to no more than one-third of the contralateral vocal cord with less than 1 cm of subglottic extension ( Fig. 13.1 ).
As in other partial laryngectomy surgical procedures, accurate staging and careful attention to details of the procedure are paramount, especially if it is to be used as a salvage procedure.
History of present illness
Hoarseness is almost always the presenting symptom for early glottic cancer. Symptoms of otalgia, dyspnea, or dysphagia suggest a more advanced stage, and prompt careful evaluation is needed to ensure that the appropriate surgical procedure is selected.
The history, laryngeal photographs, and imaging from referring otolaryngologists are helpful but do not replace real-time examination in both the clinic and the operating room.
Diagnosis is achieved with appropriate examination and biopsies. If a biopsy was performed at another institution, most surgeons require that the pathology slides be obtained for re-review by in house pathologists.
The site and stage of the cancer must be accurately determined.
Past medical history
Prior treatment: Was this cancer previously treated by endoscopic excision or radiation therapy? Prior radiation therapy is not a contraindication, although postoperative wound complications may be more likely.
Medical illnesses: Many patients with cancer of the head and neck have significant comorbidities, which must be identified prior to scheduling surgery.
Is the patient able to tolerate a surgical procedure?
Is the patient able to tolerate aspiration; a common consequence of the surgery?
Surgery—particularly any prior laryngeal or tracheal surgery
Eliciting a history of substance abuse is important, particularly a history of alcohol dependence, which may lead to postoperative alcohol withdrawal syndrome if not recognized preoperatively. Smoking has been demonstrated to impair healing; hence patients should be encouraged to stop smoking. Nicotine withdrawal can be managed with transdermal nicotine release patches in the perioperative period.
Awake fiber-optic or telescopic laryngeal endoscopy: Awake endoscopy is the most important part of the examination, as it affords accurate assessment of vocal cord mobility as well as an estimate of the location, size, and extent of the cancer.
Oral cavity: It is important to rule out second primary cancers.
Neck: Palpation of the neck may reveal adenopathy or direct extension of cancer into the soft tissue anteriorly.
Although theoretically not necessary, most surgeons favor imaging to assist with staging the patient with a bulky cancer of the glottis, particularly since more than one-third of clinically staged T2 glottis cancers are found to be more extensive on pathologic examination.
Thin-cut axial computed tomographic images of the larynx may provide important information regarding tumor extension beyond the confines of the endolarynx. A chest radiograph or computed tomography (CT) scan is required to rule out a second primary cancer of the lung.
T1-2 cancer of the glottis
Impaired mobility or fixation of the vocal cord suggests invasion into the vocalis muscle and possibly a higher stage. Extension to the arytenoid and anterior commissure may require resection of additional tissue, such as more than half of the contralateral vocal cord, which may impair adequate glottic reconstruction (see Fig. 13.1 ).
The cancer does not extend onto the cricoid cartilage (1 cm anteriorly, 0.5 cm posteriorly).
Vertical partial laryngectomy (VPL) is an ideal salvage procedure for early cancers not controlled by primary radiotherapy or CO 2 laser. However, extensions of the standard procedure may lead to undesirable morbidity, particularly in previously treated patients.
Medical comorbidities with increased risk relating to general anesthesia and inability to tolerate mild aspiration. In these situations radiation therapy would likely be the preferred modality.
Cancer extending beyond the limits of resection to involve more than one-third of the contralateral vocal cord, entire ipsilateral arytenoid, or mucosa on cricoid cartilage.
Discontinue anticoagulants 3 to 5 days preoperatively.
Mark the side of the cancer on the skin, and confirm with preoperative endoscopy prior to incising the skin.
Administer perioperative antibiotics.
The patient must understand that the quality of his or her voice will never be normal, and that it may be substantially worse than preoperatively.
VPL may lead to swallowing impairment due to inadequate laryngeal closure during deglutition. Patients must know that swallowing function may worsen with time due to age-associated loss of pharyngeal muscle tone and lung function.
If excessive tissue is removed, the airway may be borderline or inadequate, even to the extent of requiring a long-term tracheostomy.
Many surgeons specify in the consent process that if the extent of the tumor is found to be greater than anticipated at the time of surgery, a total laryngectomy will be performed at the same sitting.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here