Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
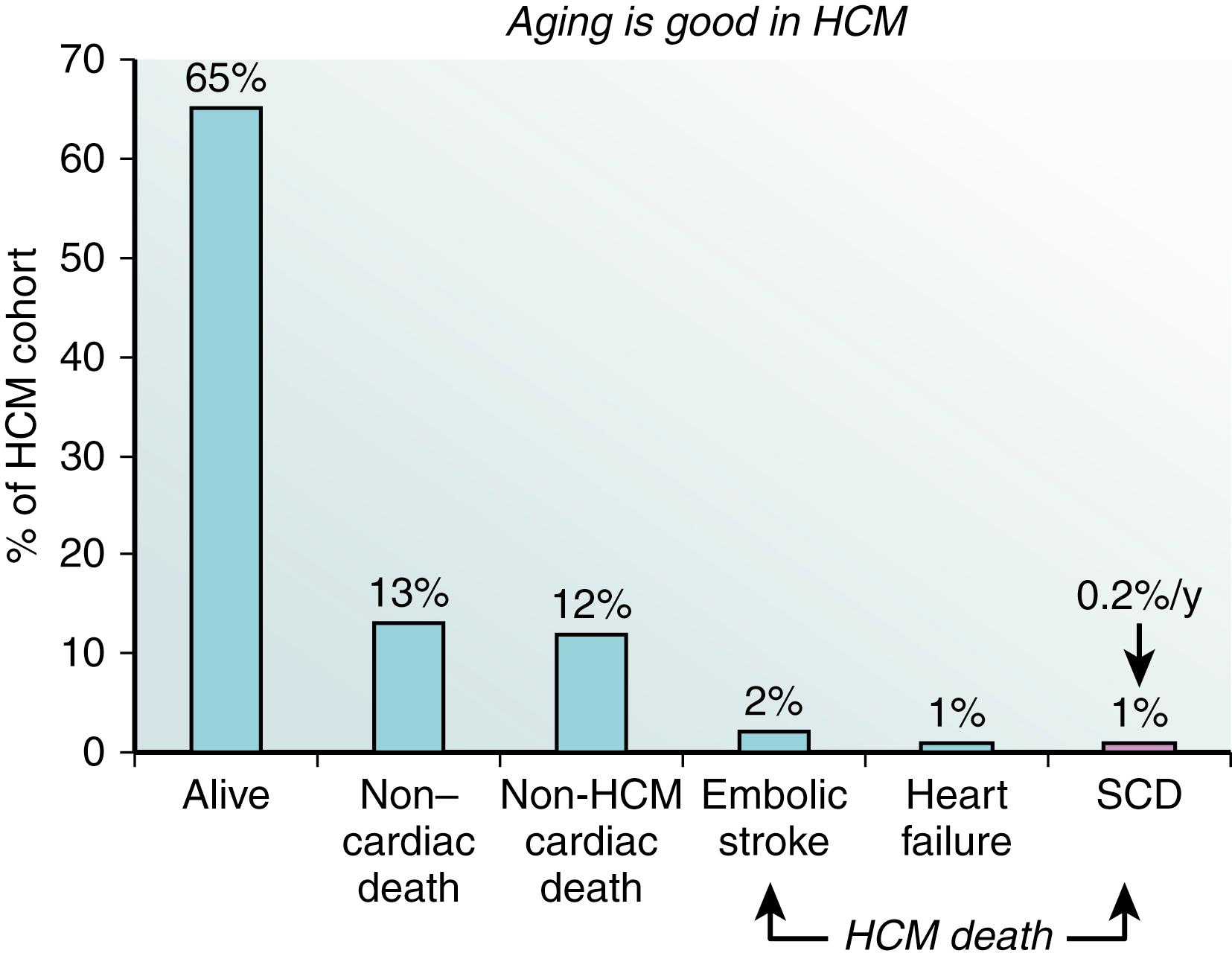
Hypertrophic cardiomyopathy (HCM) is a common genetic cardiac disease with global distribution and heterogeneous morphologic expression and natural history. , In the current cardiovascular treatment era, HCM is associated with very low disease-related mortality with an expectation for normal longevity and excellent quality of life for the majority of patients ( Fig. 89.1 ). , Nevertheless, sudden cardiac death (SCD) remains the most visible and devastating consequence of HCM. , Indeed, throughout much of its almost 60-year history, HCM has been repeatedly regarded as the most common cause of sudden death in young people.
Since its emergence into HCM practice in 2000, the implantable cardioverter-defibrillator (ICD), with its proven efficacy in aborting lethal ventricular tachyarrhythmias and preventing SCD, has changed the course of the disease and increased the importance of accurate selection of patients for device therapy. This comprehensive review presents a contemporary profile of ventricular tachyarrhythmias linked to SCD and the approach to risk stratification and strategies for SCD prevention that have altered the natural history of this complex genetic disease for many patients.
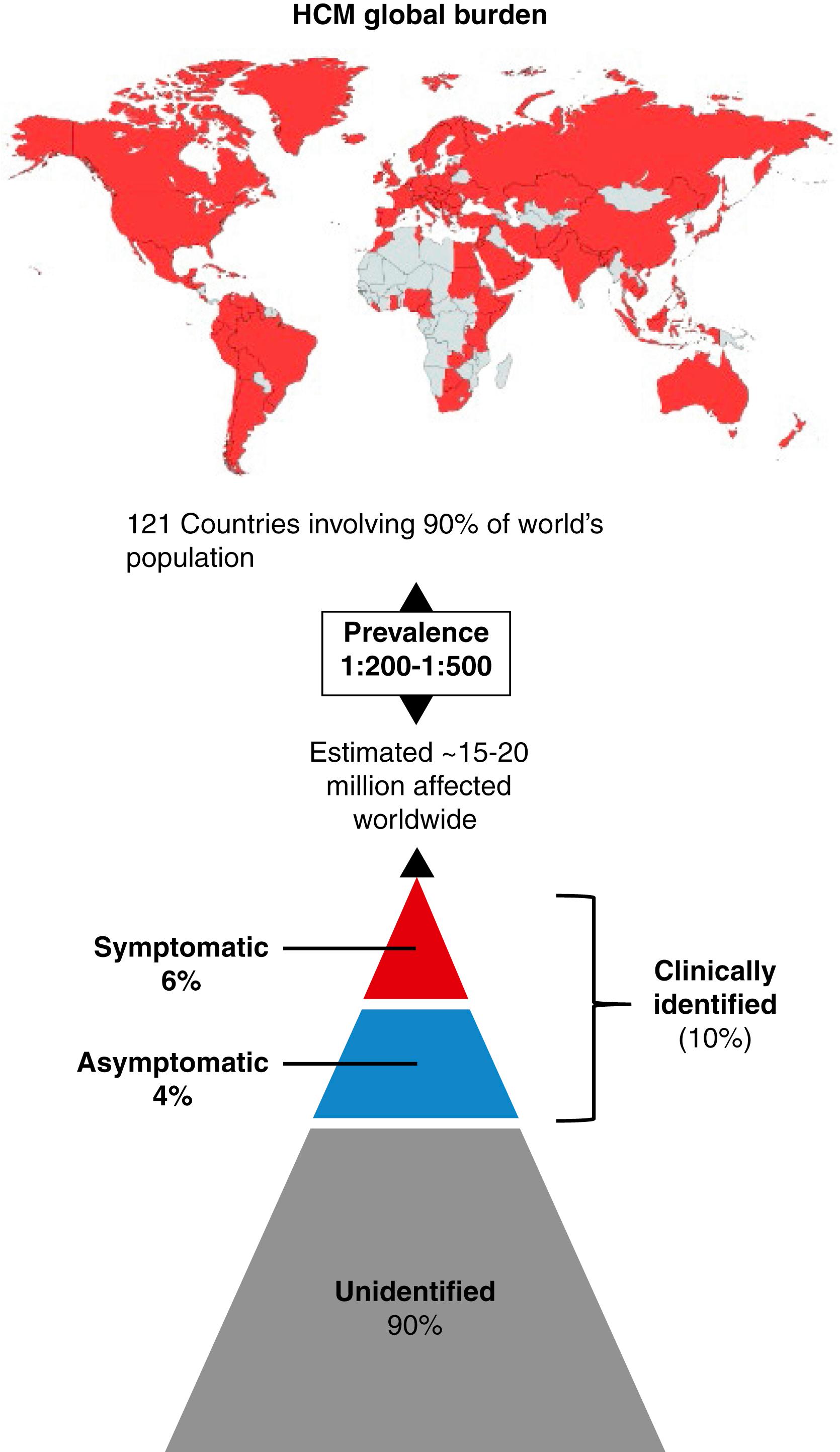
HCM-related SCD events occur in only a small minority of hospital-based, referral patient populations (about 5%), and it is much less common than other adverse disease consequences, such as atrial fibrillation (AF) or heart failure. The vast majority of affected individuals probably experience an uncomplicated, if not benign, clinical course compatible with normal or extended longevity, sometimes even into their 80s or 90s (see Fig. 89.1 ). Nevertheless, the relatively high prevalence of HCM in the general population (with estimates of 1:500 to as high as 1:200) suggests that there could be 1 million affected Americans, including a significant minority at risk for SCD, of whom only a small proportion are recognized clinically ( Fig. 89.2 ).
The clinical profile of the typical SCD victim in HCM is that of a predominantly asymptomatic (or mildly symptomatic) patient younger than 35 years, whereas the average age for first appropriate ICD shock in high-risk HCM patients is 43 years. , Nevertheless, the likelihood of SCD events does not increase linearly with age and is low for clinically stable patients who reach 60 years or older ( Fig. 89.3 ). This observation translates to higher thresholds for prophylactic ICD implants in this older age group. No difference has been reported for SCD risk between the genders or with respect to race.
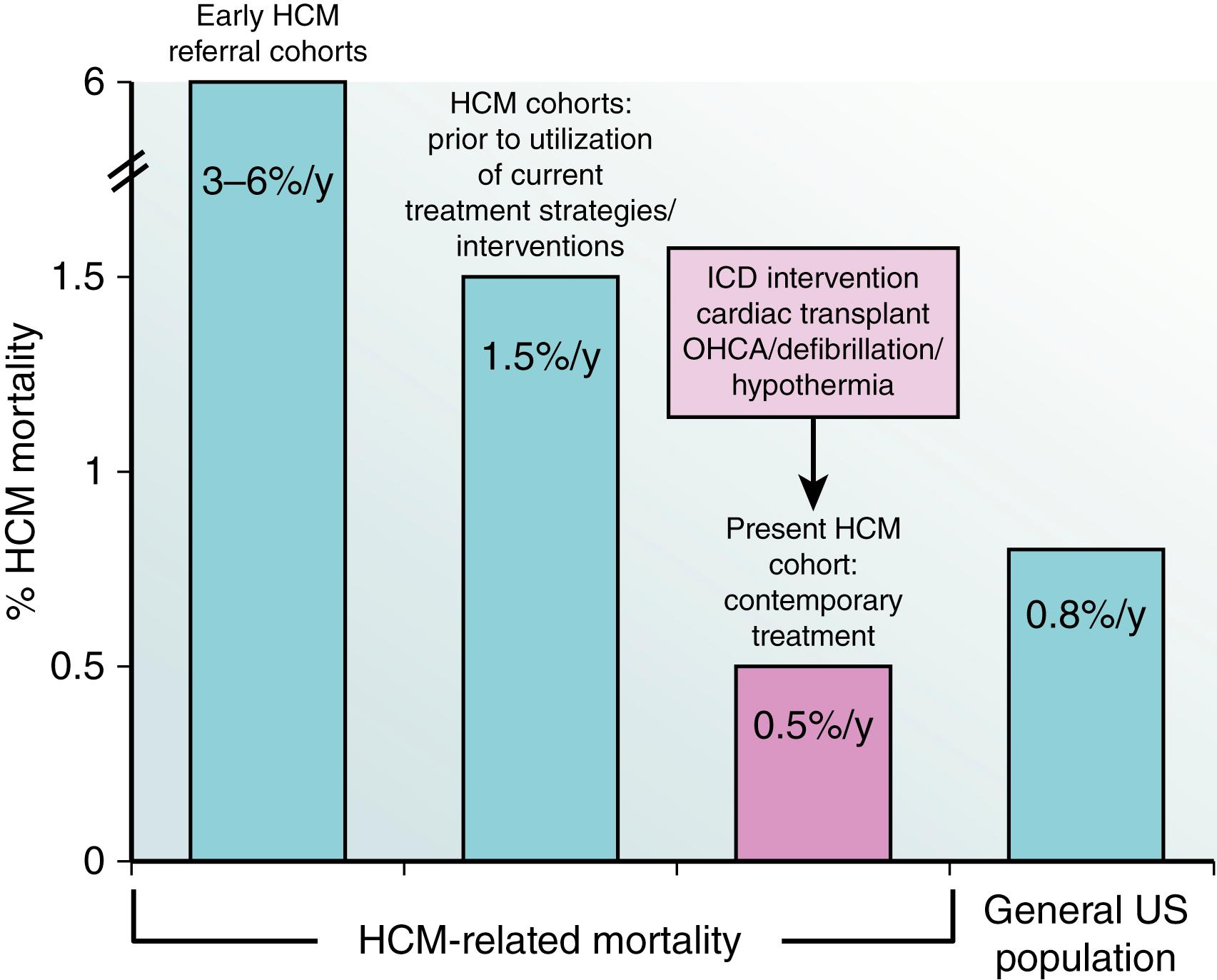
Mortality rates in HCM have evolved considerably over time, decreasing from the 6% per year reported from hospital-based cohorts in the older HCM literature. Thereafter, reports from less selected cohorts, in the pre-ICD era, placed HCM-related mortality (largely because of SCD) at 1.5% to 2.0% per year ( Fig. 89.4 ). In the current era of contemporary cardiovascular treatments, risk stratification, and ICDs, disease-related mortality for HCM is 0.5% per year across all ages (see Fig. 89.4 ). ,
Stored ICD electrograms in HCM patients document that aborted SCD events are caused by ventricular fibrillation (VF) and rapid monomorphic ventricular tachycardia (VT). To date, there is no evidence that bradyarrhythmias play a role in HCM-related SCD. , The basic mechanisms leading to VT/VF and SCD are incompletely characterized but likely multifactorial and complex, including triggered activity, reentry, and abnormal automaticity. At the cellular level, inactivation of ICaL is delayed and the late sodium current is increased, contributing to prolongation of the cardiac action potential. Further cellular consequences include disruption of myocyte sodium and calcium homeostasis with increased susceptibility to early and delayed afterdepolarizations and triggered automaticity. These can potentially induce reentrant VT, facilitated by slowed myocardial conduction velocity because of myocardial fibrosis and myocyte disarray ( Fig. 89.5 ).
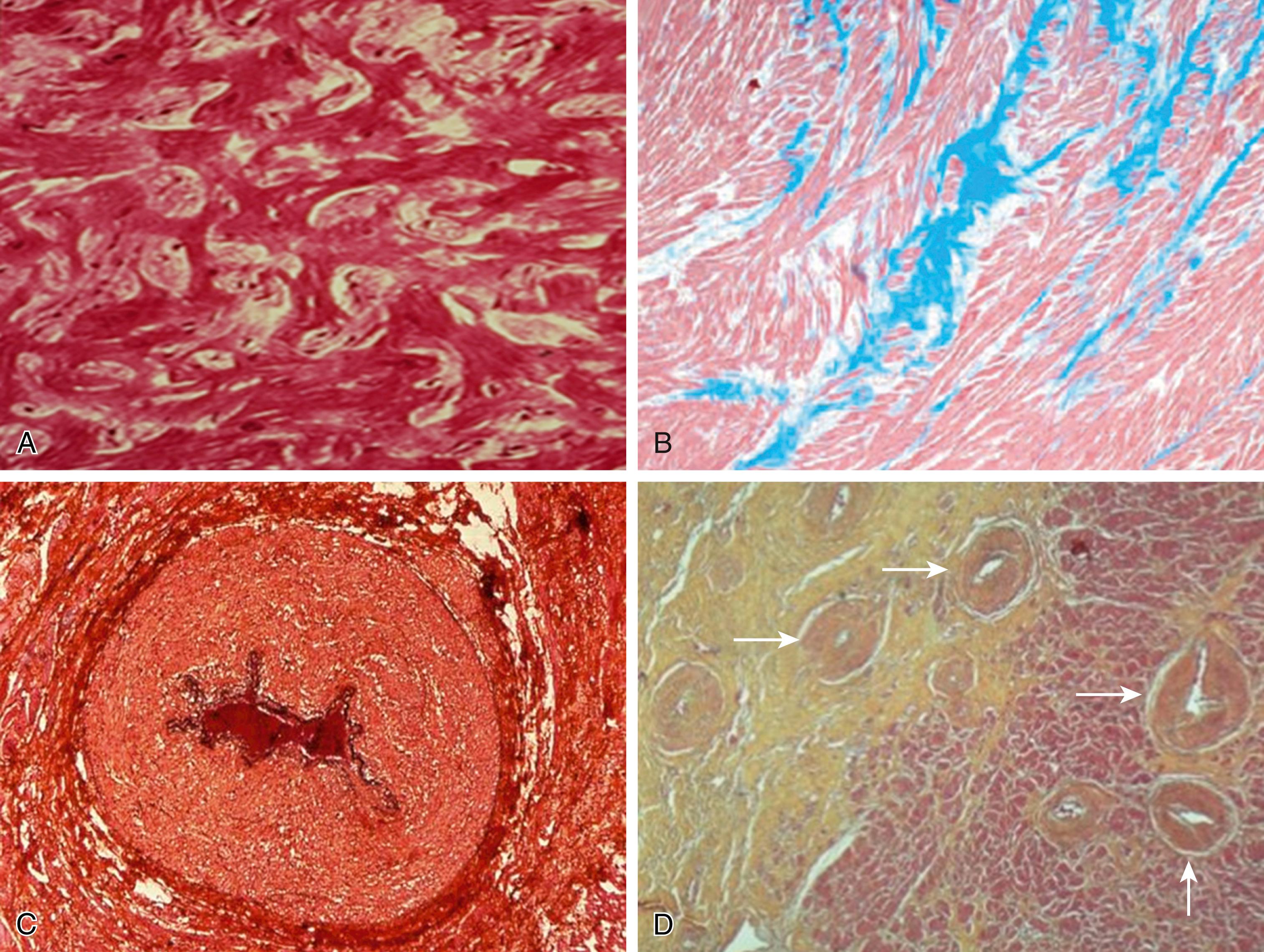
It is also likely that microvascular ischemia caused by structurally abnormal intramural arterioles can reduce the resting membrane potential of the myocyte, causing abnormal automaticity that might initiate VT (see Fig. 89.5 ). Disturbances of the autonomic nervous system may also trigger VT through enhanced automaticity and may explain the observation of sinus tachycardia preceding VT/VF in about one-third of cardiac arrests in HCM patients, providing a possible mechanism for arrhythmogenic events during vigorous physical activity.
The high frequency of ambulatory asymptomatic ventricular tachyarrhythmias in HCM is disproportionate to the relatively low prevalence of SCD in this patient population. On 24- to 48-hour ambulatory (Holter) electrocardiogram (ECG) monitoring, 90% of HCM patients demonstrate ventricular tachyarrhythmias, which are often frequent and complex, including bursts of nonsustained ventricular tachycardia (NSVT), which occur in 20% to 30% of patients and are a risk marker for SCD. , About 10% of patients show particularly frequent ambulatory ectopy, including combinations of frequent premature ventricular depolarizations, couplets, and at least one NSVT burst in a 24-hour monitoring period.
During the early pre-ICD history of HCM, strategies for SCD prevention focused on a variety of empiric pharmacologic interventions, including β-blockers, procainamide, quinidine, verapamil, and amiodarone, all of which are now regarded as obsolete for this purpose. Although such approaches were popular because they were the only treatment options then available, these drugs failed to provide absolute protection from SCD or ventricular tachyarrhythmias and, in some cases, may have been proarrhythmic. , , In addition, ICD trials in HCM have demonstrated that a substantial proportion of patients experience appropriate shocks for VT/VF while taking β-blockers and/or antiarrhythmic drugs. ,
The ICD was introduced into cardiovascular medicine for SCD prevention in the 1980s thanks to the vision and work of Michel Mirowski, who worked with Morton Mower at the Sinai Hospital in Baltimore, despite antagonism from the cardiology establishment. Availability of the ICD ultimately created a paradigm shift in which ineffective drug strategies were replaced with the implantation of sophisticated devices that recognize and automatically terminate potentially lethal ventricular tachyarrhythmias.
Notably, of the first three ICD patients studied in 1980 at Johns Hopkins Hospital to determine whether the device would reliably and automatically terminate VF, two had HCM. Each had previously survived two cardiac arrests, making them eligible for this new therapy. Nevertheless, application of the ICD to patients with genetic heart disease (including HCM) was largely ignored for the next 20 years, as studies of device therapy largely focused on patients with ischemic heart disease. ,
ICDs were employed sparingly in HCM patients until the landmark New England Journal of Medicine report in 2000 demonstrated the efficacy of ICD therapy in providing absolute protection from SCD in a series of patients. Thereafter, greater numbers of HCM patients as well as patients with other, less common, structural heart diseases, such as arrhythmogenic right ventricular cardiomyopathy, received prophylactic ICDs.
Because the initial clinical ICD studies focused on coronary artery disease (CAD) populations, there are certain distinctions between high-risk HCM and CAD patients that deserve consideration. ICD candidates with CAD average age of 65 years at implant, usually have systolic dysfunction with prior myocardial infarction (MI), and often have extracardiac comorbidities. Because of their relatively advanced age, the device is needed for a relatively shorter duration of time compared with HCM patients who are generally at least 25 years younger than CAD patients at the time of prophylactic ICD implant and may have fewer or no comorbid diseases (especially in the case of adolescents and young adults). , , Younger HCM patients have potentially decades-long risk periods with the ICD, with greater likelihood of incurring device-related complications. Because of the low HCM-related SCD rate in clinically stable patients older than 60 years (even in the presence of risk markers), a higher threshold for primary prevention implants for most patients in this age group is prudent, with decisions made on a case-by-case basis (see Fig. 89.3 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here