Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Cardiac arrhythmias are common in critically ill patients and a frequent reason for hospital admission to areas with capability for continuous electrocardiographic monitoring and personnel trained in their recognition and management (e.g., intensive care units [ICUs] and telemetry units).
Arrhythmias are supraventricular if they originate above the atrioventricular (AV) node, such as in atrial tissue or pulmonary veins. They may compromise stroke volume and create hemodynamic instability because of excessive heart rate and/or reduced ventricular filling after losing the atrial contribution to preload. However, in the absence of accessory conduction pathways bypassing the AV node (e.g., Wolf-Parkinson-White syndrome), supraventricular arrhythmias are rarely life-threatening and may be managed without immediate urgency by pharmacologic or electrical means. In contrast, arrhythmias such as ventricular tachycardia (VT) and ventricular fibrillation (VF) that originate in the ventricular tissue may be life-threatening and require immediate treatment.
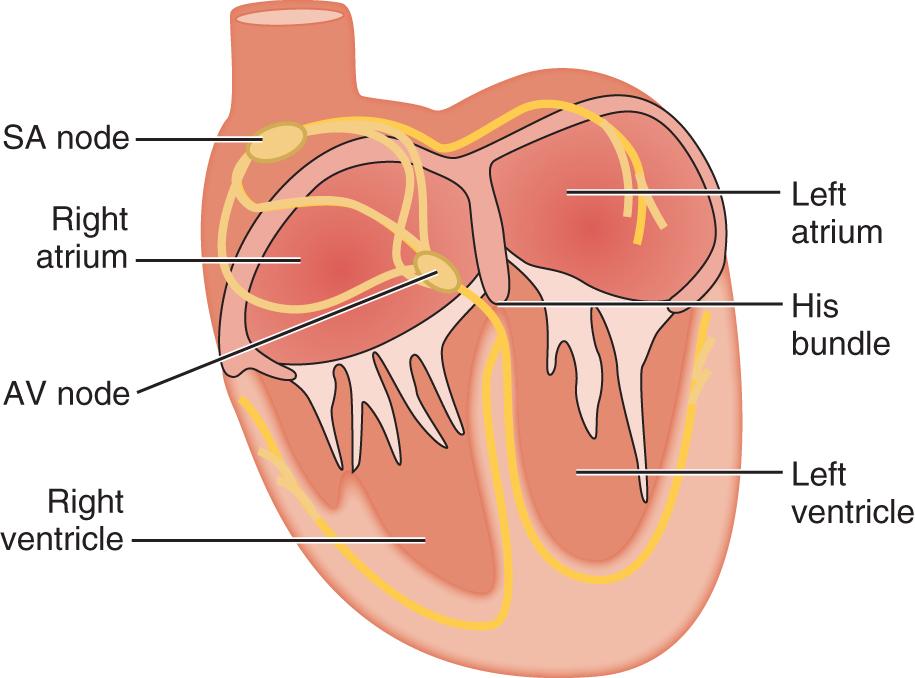
The electrical impulse originates in the sinoatrial (SA) node, located high on the right atrium near its junction with the superior vena cava ( Fig. 72.1 ). The impulse propagates through muscle fibers and specialized internodal pathways (composed of Purkinje-type fibers) to converge on the AV node, located in the interatrial septum near the tricuspid valve. The impulse then travels through the bundle of His, its left and right branches, and the Purkinje system to activate both ventricles simultaneously. A ring of fibrous tissue interposed between the atria and the ventricles prevents spread of the impulse through muscle fibers, enabling the AV node to function as a relay and filter, preventing 1:1 conduction under conditions of very rapid atrial activation such as atrial flutter (rate ∼300 s–1) or atrial fibrillation (rate ∼600 s–1).
Action potentials, once initiated in pacemaker cells, propagate through both atria and ventricles. The electrical impulse depolarizes cardiac myocytes and opens voltage-dependent Ca 2 + channels. Influx of Ca 2 + causes Ca 2 + -induced Ca 2 + release via ryanodine receptors located in the sarcoplasmic reticulum to activate contractile proteins and elicit contraction. Each action potential is produced as a result of time- and voltage-dependent opening and closing of different types of plasma membrane ion channels, mainly involving influx of Na + and Ca 2 + (inward currents) and efflux of K + (outward currents).
Cells from the Purkinje system and muscle tissue have a stable resting potential of approximately −90 mV (negative inside), largely as a result of a background (also called leak ) K + current known as inward rectifier (I K1 ). Because this K + channel is open at rest, it “anchors” the membrane potential to a voltage close to the K + equilibrium potential. Because of its inward rectification properties, I K1 is turned off during depolarization, which is critical for maintaining the action potential duration.
Phase 0 is the initial rapid upstroke of the action potential. Triggering an action potential requires depolarization to a level between −70 and −80 mV, which is the threshold for activation of fast voltage-gated Na + channels (I Na ) and is normally achieved upon arrival of another action potential. The I Na drives the membrane potential toward the Na + equilibrium potential, reversing the membrane potential to approximately +20 mV (overshoot). This is phase 0 of the action potential and is followed by repolarization in four phases ( Fig. 72.2 ).
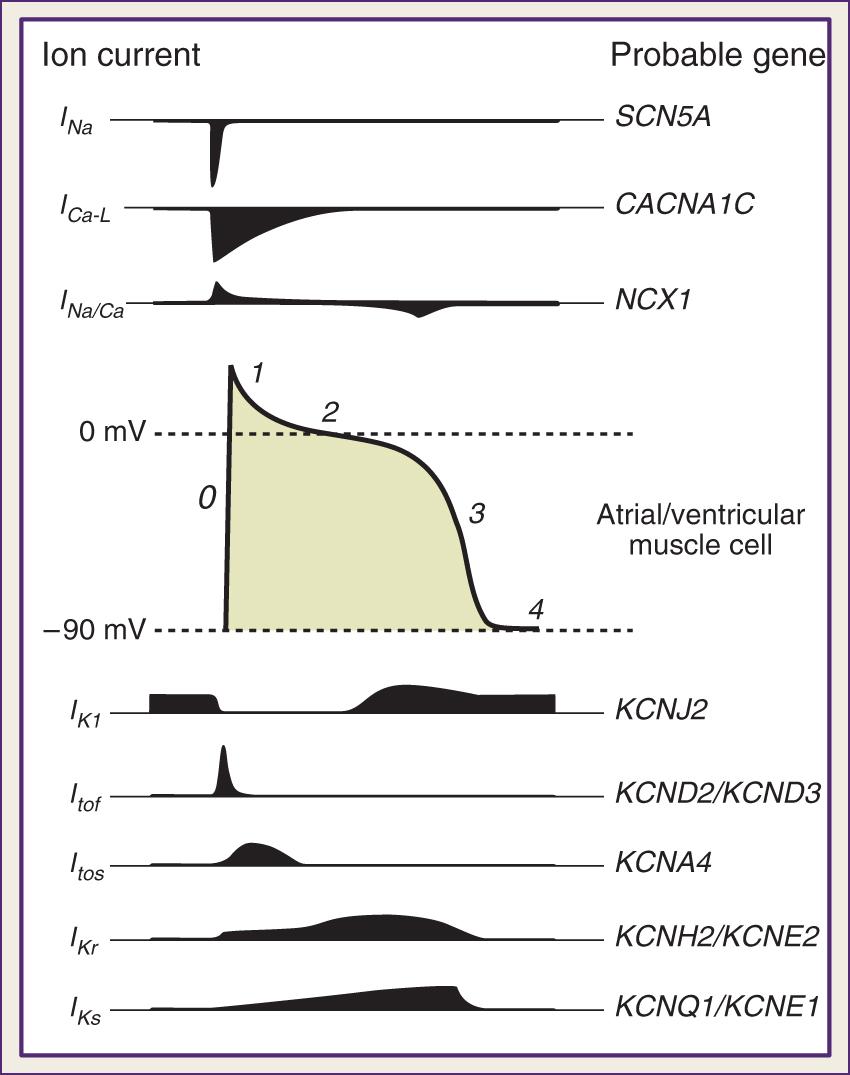
Phase 1 is the early rapid repolarization period that occurs just after the upstroke (phase 0) of the action potential. Phase 1 is produced by activation and subsequent inactivation of a “transient” K + current (I To ) and is composed of “fast” recovering (I Tof ) and slowly recovering (I Tos ) currents. I Tof is thought to be the predominant contributor to I To in ventricular myocardium. Because K + channels that produce I To are expressed at higher levels in the subendocardium and mid-myocardium than in the subendocardium, I To contributes to the repolarization inhomogeneity.
Phase 2, the plateau phase, is produced by Ca 2 + influx via opening of L-type voltage-gated Ca 2 + channels (I Ca-L ) , and K + efflux via a delayed rectifier K + channel (I K ). Both I Ca and I K are activated by the initial depolarization produced by Na + influx during phase 0 . The relatively small inward (I Ca ) and outward currents (I K ) produce little net current, resulting in a near-flat phase 2. During the plateau phase, Ca 2 + channels slowly inactivate with time and Ca 2 + influx decreases, but the K + current (I K ) increases with time, producing a net increase in outward current near the end of phase 2 .
Phase 3 corresponds to the late strong repolarization and is produced by the delayed rectifier K + current. The delayed rectifier K + current (I K ) has a rapid (I Kr ) and a slow (I Ks ) component. , Although both I Ks and I Kr are critical for producing the strong repolarization, they possess quite different activation and inactivation kinetics. The magnitude of I Kr is greater than that of I Ks during the rapid repolarization phase, and therefore I Kr plays an important role in bringing the cell membrane potential back toward the resting state. Both are implicated in acquired and heritable forms of long QT syndrome. Near the end of the repolarization phase, I K1 begins to increase as the cell membrane potential returns toward −90 mV and thus partly contributes to the final setting of the resting potential.
Phase 4 is the resting fully repolarized state and is produced by reopening of the inward rectifier background K + channels as the cell membrane potential is brought close to −90 mV. During this phase, the ionic balance is restituted by the action of the Na/K pump. This is an important phase that allows diastolic filling of the relaxed ventricle.
In cells of the SA and AV nodes, voltage-gated Na + channels are in the inactive state, and phase 0 is produced by I Ca-L . Because the activation kinetics of I Ca-L are slower than that of I Na , phase 0 is slanted and in part responsible for the slow SA and AV node conduction velocity (∼50 cm·s − 1 ) relative to that in the His-Purkinje system (~400 cm·s − 1 ) and muscle cells (~100 cm·s − 1 ). Pacemaker activity of SA and AV node cells results from slow phase 4 depolarization (known as prepotential or pacemaker potential ) to ~−40 mV. Slow depolarization involves opening of the hyperpolarization-activated inward Na + current (also known as the “funny current,” I F ) and opening of T-type voltage-gated Ca 2 + channels (I Ca-T ). The T-type Ca 2 + channel is activated at a more negative membrane potential than that of the L-type Ca 2 + channel and thus contributes to the pacemaker potential. The phase 3 repolarization produced by activation of the delayed rectifier K + current (I K ) is a prerequisite for subsequent activation of I F. I K is large at the beginning of phase 3 but decreases quickly with time as the cell membrane potential becomes negative, and this event helps start the subsequent slowly depolarizing pacemaker potential (phase 4). Cells of the His–Purkinje system have latent prepotential activity and can become active when SA or AV node activity is depressed or their impulses are blocked (i.e., “escape rhythm”). Muscle cells exhibit prepotential activity only under abnormal circumstances.
The preceding paragraphs describe the primary ionic mechanisms that produce phase 0 through phase 4 of the cardiac action potentials. Other ion channels, antiporters, pumps, and receptor agonists can also modulate the shape of the action potential in response to various stimuli such as high sympathetic tone and hypoxia. For example, a nonselective cationic channel gated at resting potential by intracellular Ca 2 + is present in cardiac myocytes. This channel produces an inward Na + current (I NS ) that may contribute to delayed afterdepolarizations when Ca 2 + is released from the sarcoplasmic reticulum. I K(ATP) is a K + current carried through channels inhibited by intracellular adenosine triphosphate (ATP) and is opened under conditions of ischemia and hypoxia. I K(ATP) contributes to action potential shortening and the characteristic ST-segment elevation observed during myocardial ischemia. ,
The sarcolemmal Na + /Ca 2 + exchanger is another important modulator of the action potential. Because it exchanges one Ca 2 + for three Na + , it generates a current (I Na/Ca ) whose direction depends on Na + and Ca 2 + gradients and the membrane potential. ,
Adrenergic receptor stimulation also modulates the action potential by modifying channel activity. For example, beta-1 adrenoceptor stimulation increases I Ca-L activity and Ca 2 + influx, enhancing inotropic action. Beta-1 adrenoceptor stimulation also activates K + channels, shortening the action potential duration. Alpha-1 adrenoceptor stimulation acting via Gq protein on the Na + /K + pump, K + channels, and phospholipase C can alter impulse initiation and repolarization, an effect linked to triggered arrhythmias via early and delayed afterdepolarizations and abnormal automaticity during ischemia and reperfusion. ,
Muscarinic receptors (M 1 ) coupled to Gi protein are highly expressed in pacemaker and atrial cells. M 1 receptor stimulation by acetylcholine released from the efferent vagus nerve innervating the cells of the SA and AV nodes produces slowing of the heart rate and conduction velocity, which is a parasympathetic response.
Cardiomyocytes can also react to mechanical forces through stretch-activated ion channels and other mechanisms, including mechanical modulation of Ca 2 + handling and interaction with other mechanosensitive cells. , These mechanisms are probably involved in commotion cordis, precordial thump, and fist pacing.
Abnormalities in impulse generation and conduction are responsible for the genesis and maintenance of ventricular tachyarrhythmias.
Abnormalities in impulse generation are generally the result of automaticity or triggered activity.
Automaticity refers to the emergence of ectopic pacemaker activity resulting from enhanced normal automaticity or development of abnormal automaticity.
Enhanced normal automaticity occurs when cells with intrinsic pacemaker potentials (e.g., cells from the AV node or His–Purkinje system) that are normally suppressed by the SA node fire at rates that escape such suppression. This phenomenon may result from effects on phase 4 prepotentials yielding earlier development of action potentials (i.e., less maximal polarization, faster depolarization, or lower threshold potential) or from shortening of the action potential duration with earlier return to phase 4 . Enhanced normal automaticity is usually the result of adrenergic stimulation, which increases the slope of the pacemaker potential by acting on I F .
Development of abnormal automaticity refers to impulses originating in cells without intrinsic pacemaker potential and typically occurs by generation of depolarizing currents during phase 4 (e.g., ischemia). Abnormal automaticity can develop in atrial and ventricular muscle cells and in specialized tissues other than the SA and AV node. Examples include accelerated idioventricular rhythms and some VTs developing 24–72 hours after acute myocardial infarction.
Triggered activity refers to arrhythmias that arise from afterdepolarizations, defined as alterations in membrane potential that occur during repolarization. Afterdepolarizations are considered early if they develop during phase 2, phase 3, or early phase 4 of the action potential and are characterized by transient retardations in repolarization ( Fig. 72.3 ). If of enough magnitude, they can trigger an “extra” action potential. Early afterdepolarizations are typically associated with conditions that prolong the action potential (e.g., increased sympathetic tone, exogenous catecholamines, hypoxia, acidosis, bradycardia, etc.), enabling increased Ca 2 + entry through I Ca-L and can trigger torsades de pointes, a form of VT. In the setting of heart failure, Ca 2 + sparks occurring during phase 2 or phase 3 consequent to loss of synchrony in Ca 2 + release at the start of the action potential can generate enough I Na/Ca current to trigger early afterdepolarizations.
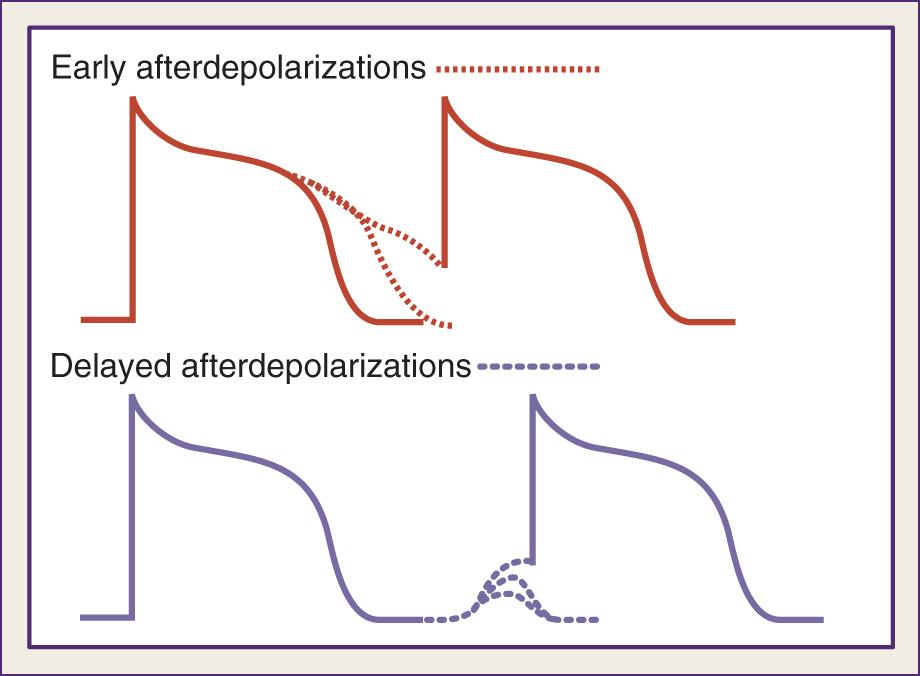
Afterdepolarizations are considered delayed if they develop in late phase 4 and may also reach the threshold for triggering an action potential (see Fig. 72.3 ). The main underlying abnormality is intracellular Ca 2 + overload, triggering Ca 2 + release from the sarcoplasmic reticulum and depolarizing currents (i.e., inward I Na/Ca currents). Delayed afterdepolarizations are classically associated with digitalis toxicity; however, they can also occur with myocardial stretch, hypertrophy, catecholamines, ischemia, and reperfusion. In heart failure, increased expression of the Na + -Ca 2 + exchanger along with abnormalities in the ryanodine receptor predispose to delayed afterdepolarizations.
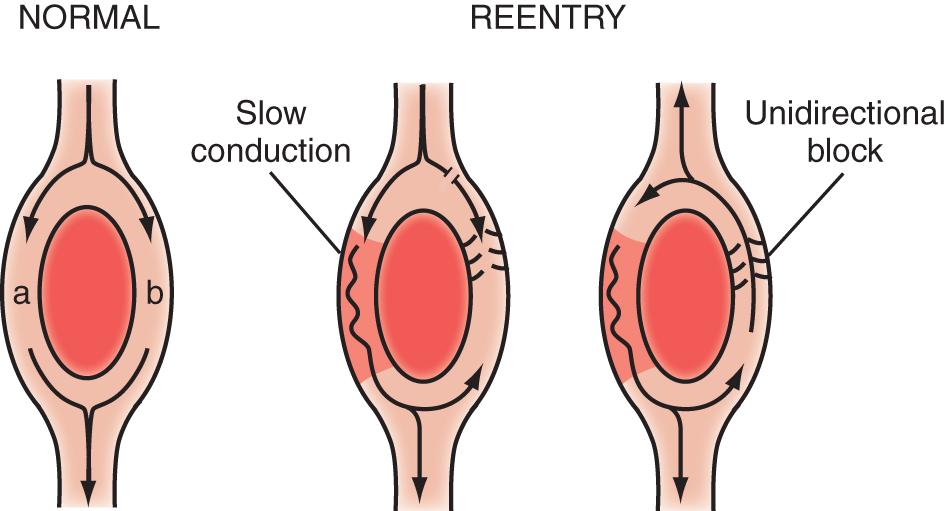
Abnormalities in impulse conduction leading to reentry account for the vast majority of sustained VTs. Reentry occurs when a propagating impulse reenters and reexcites a region of previously excited tissue after its refractory period is over. Several forms of reentry have been described, including circus movement, phase 2, and reflection.
Circus movement is the most widely studied reentry model and encompasses four distinct models: ring, leading circle, figure of eight, and spiral wave.
The ring model is the simplest, and it is useful to illustrate the basic mechanism of reentry ( Fig. 72.4 ). The ring model requires two contiguous paths separated by unexcitable tissue. One path— b in Fig. 72.4 —has a zone of unidirectional block, whereas the other path—a in Fig. 72.4 —allows slow but bidirectional conduction. Once the impulse traveling path a reaches path b, it propagates retrogradely to subsequently reenter path a . To establish reentry, the circling impulse wavelength must be shorter than the reentry circuit path length, allowing its leading edge to find tissue in an excitable state. The circling impulse wavelength is the product of conduction velocity and refractory period, and conditions that slow conduction or shorten refractoriness favor reentry. The ring model commonly involves AV accessory pathways and the AV node. Reentry is usually triggered by the arrival of a premature beat. Unidirectional block may result from increased refractoriness caused by anatomic abnormalities (e.g., fibrosis, accessory pathway, bundle branch block) or functional defects (e.g., ischemia, action of drugs).
The leading circle model is similar to the ring model but without requiring anatomic obstacles and can develop in structurally uniform myocardium by a properly timed premature impulse.
The figure-of-eight model was first described in experimental myocardial infarction. It encompasses two reentry circuits moving alongside a functional conduction block (ischemia or infarct) in opposite directions, forming a pretzel-like configuration.
The spiral wave model is a more complex version of the leading circle model and involves a core and filaments and can be described as reentry in two dimensions. It has been used to explain monomorphic and polymorphic VTs and VF. In monomorphic VT, the spiral wave is anchored and unable to drift, whereas in polymorphic VTs—such as torsades de pointes—the spiral is thought to drift. In VF, the spiral wave is thought to break up into multiple rotating spiral waves that continuously extinguish and re-create. Yet some authors have proposed a single rapidly shifting spiral, and others have postulated a stationary rotor whose frequency of excitation is exceedingly high, resulting in multiple areas of intermittent block.
Phase 2 reentry refers to local reexcitation consequent to repolarization heterogeneity with areas of markedly shortened repolarization—essentially obliterating phase 2 of the action potential—next to areas of normal repolarization. Local reexcitation may precipitate VT during myocardial ischemia. Action potentials of normal duration may alternate with ones of shorter duration during myocardial ischemia, yielding beat-to-beat alternans (temporal dispersion) and site-to-site alternans (spatial dispersion) and promote regions with conduction block and regions with injury current, leading to reentry and VTs. The degree of spatial and temporal dispersion progresses during ischemia, suggesting this mechanism may be an important trigger of VT and VF during acute myocardial ischemia. , In the surface electrocardiogram (ECG), dispersion of the action potential duration manifests as T-wave alternans, which is a predictor of VF.
Reflection refers to a back-and-forth propagation of the impulse over the same functionally unexcitable tissue, with recurrent activation of the proximal region as a result of electrotonic currents. The area of unexcitable tissue could result from ischemia and lead to extrasystolic activity. Reflection differs from classic reentry in that the impulse travels along the same pathway in both directions.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here