Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
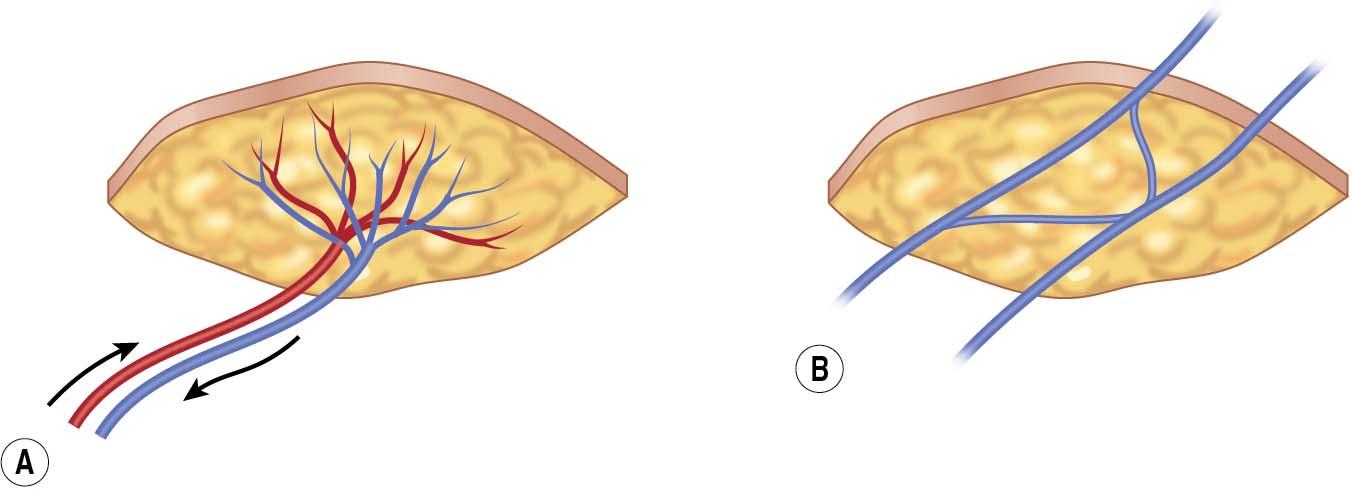
The venous flap is a thin, pliable flap consisting of skin, subcutaneous tissue, and veins. It differs from conventional flaps in that it is not an arterial afferent and venous efferent flap ( Fig. 93.1A ). Instead, inflow and outflow occur through the venous system of the donor tissue (see Fig. 93.1B ). These flaps can be well shaped to fit different wounds and provide great mobility, permitting wide range of motion (ROM) of the hand for pinch and grip.
The venous flap is a versatile reconstructive option because it can be harvested without sacrificing the main donor artery and does not entail deep dissection. There are many possible donor site options because the flap is not limited by the arterial direction or the size of the vascular pedicle.
There are two subcategories of venous flap:
The purely venous flap ( Fig. 93.2A ) consists of total venous perfusion. Both the afferent and efferent veins from the flap are anastomosed with veins at the recipient site. Although this design has theoretical applications, it is seldom used because the low oxygen concentration in the venous flow is thought to hinder perfusion and nutrient circulation.
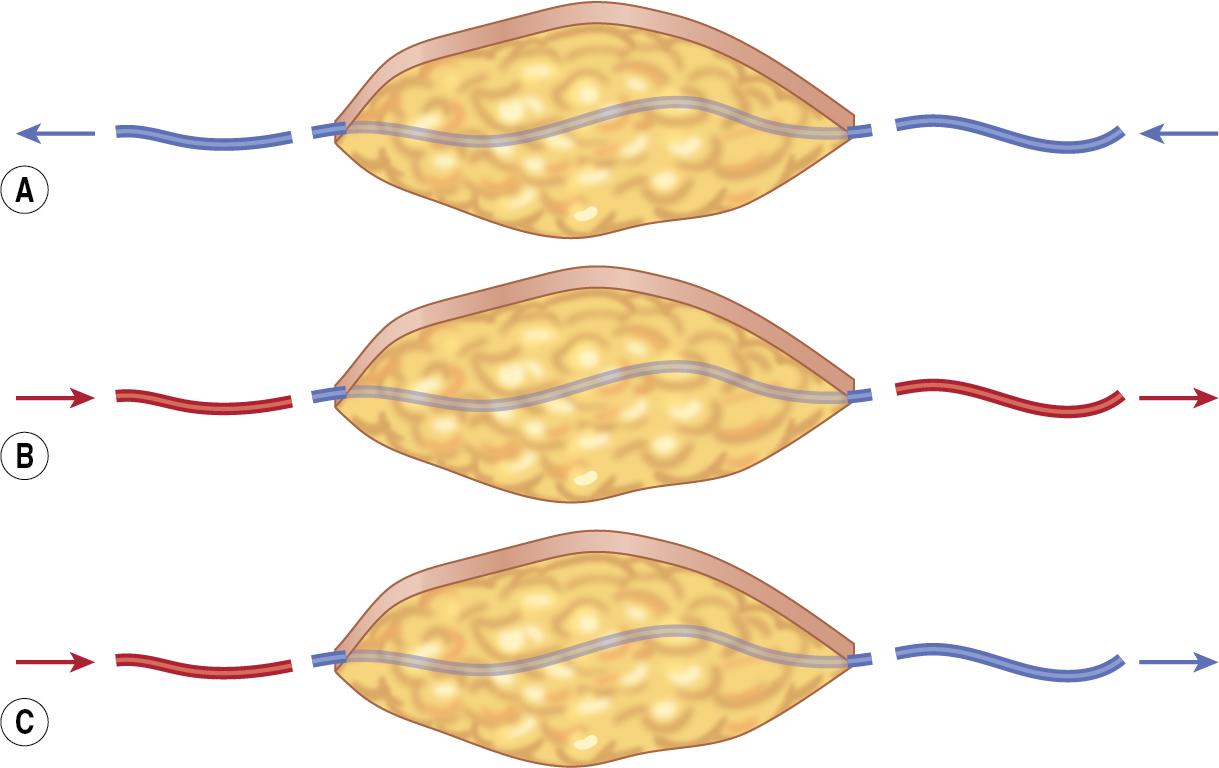
The arterialized venous flap (AVF) consists of arterialized venous perfusion. The afferent vein is anastomosed to an artery at the recipient site. The efferent vein is anastomosed to an artery or vein. The AVF is the most commonly used venous flap and will be discussed in this chapter.
A-A type (arterial flow-through; see Fig. 93.2B ): The A-A type is mostly used as a vascular conduit to repair arterial defects and provide soft tissue coverage.
A-V type (arterial inflow and venous outflow; see Fig. 93.2C ): Unlike the A-A type, the A-V type has more extensive applications because there are more veins available for anastomosis at the recipient site.
The AVF can be designed with antegrade or retrograde flow, meaning that blood flows either through or against the venous valves within the afferent vein.
In an antegrade AVF, perfusion is limited because the lack of resistance within the afferent vessel encourages blood to travel straight through the flap instead of entering the peripheral tissues ( Fig. 93.3A ). When blood does reach the periphery of an antegrade AVF, congestion may occur as a result of the low pressure gradient across the flap and the limited number of drainage points.
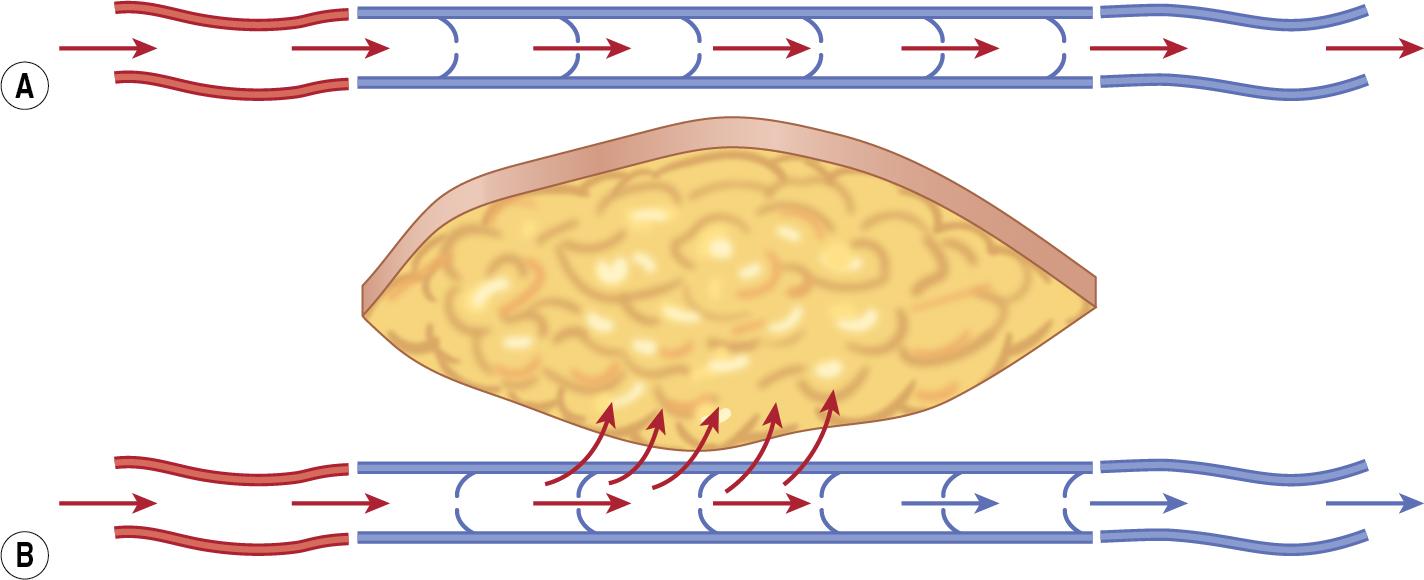
In a retrograde AVF, the IV pressure increases against the valves and theoretically forces the blood into the peripheral circulation (see Fig. 93.3B ).
The potential limitations of the AVF must be taken into consideration when determining flap size. A retrograde AVF can be larger than an antegrade AVF because the resistance within the flap vessels encourages more widespread perfusion. Nevertheless, to avoid complications, the maximum size should not exceed 50 cm 2 .
The venous flap is a good option for many hand and digit repairs because it is thin and mobile, with several potential donor sites:
The volar forearm, dorsal foot, and the medial side of the lower leg provide good coverage of the dorsal hand and digits, which need a thin and mobile flap to maintain full motion.
The thenar, hypothenar, and medial plantar regions are well suited to cover defects of the fingertip and finger pulp, which is glabrous and has a thick cutaneous layer and less flexibility.
The venous flap can also be used to repair composite defects:
Skin and vessel defects: The AVF is used to reconstruct soft tissue and vascular defects simultaneously. It can be used for segmental defect in avulsion injury or finger replantation. As a vascular conduit, the A-A type AVF can feed the distal tissues of the digits.
Skin and tendon defects: The AVF can be used to reconstruct skin and tendon defects simultaneously. Common methods include forearm tendocutaneous AVF with palmaris longus (PL) tendon or dorsalis pedis tendocutaneous AVF with extensor digitorum longus (EDL) tendon.
Skin and nerve defects: The innervated AVF can restore both sensory function and skin coverage of the hand or digit when a nerve graft is anastomosed with the digital nerves. For instance, an AVF from the dorsum of the foot carries branches of superficial peroneal nerves to the recipient site.
Contraindications include infection of the recipient site, inadequate debridement resulting in unhealthy tissue, and lack of reliable blood vessels available for anastomosis at the donor site.
Although there are cases of large venous flap survival, such as 70 to 120 cm 2 , survival is not reliable for defects greater than 50 cm 2 .
The size and depth of the wound are assessed, and the wound is completely debrided. There must be sufficient blood supply over the wound bed. The healthy wound bed should be red and shiny in appearance and bleed easily.
Apply a tourniquet so that the veins engorge within the donor site and then assess the venous distribution ( Fig. 93.4 ). Mark the number and location of veins. Also determine which veins should be afferent versus efferent based on their size and orientation. As the size of the flap increases, the number of outflow veins should also increase to encourage venous drainage.

Evaluate the potential donor areas to determine whether the skin characteristics and venous distribution are compatible with the recipient site. Options include the volar side of the distal forearm, back of the foot, medial side of the lower limbs, and thenar and hypothenar regions.
Any site is suitable to repair small defects (less than 10 cm 2 ).
The distal forearm is ideal to repair soft tissue defects of medium size (11–24 cm 2 ).
The medial side of the lower extremity and the dorsal foot are used to repair large soft tissue defects (at least 25 cm 2 ).
The thenar and hypothenar regions are used to repair small soft tissue defects in the fingertips or finger pulp because of the similar skin features. The thick, glabrous skin from these regions can withstand high shearing forces on the palm.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here