Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Numerous techniques of vena cava interruption have been described in the past for the prevention of PE, including femoral vein and IVC ligation, and partial interruption of the IVC by means of plastic clips, plication, or mechanical staplers. These later measures were developed to compartmentalize the vena cava to allow blood flow but trap large emboli, and they were the mainstay of treatment through the 1950s and 1960s. Despite these measures, there were high rates of IVC occlusion, significant lower extremity venous-related problems, and little improvement in outcome of patients with PE. With the development of techniques to allow transvenous delivery of intravascular vena cava devices, the Mobin-Uddin umbrella filter was introduced in 1967. Structured as a silicone membrane with a hole to allow blood flow, it was associated with a high rate of vena cava thrombosis. In 1973 the original stainless steel Greenfield filter was introduced, followed by titanium Greenfield filter in 1989 and lower profile stainless steel Greenfield filter in 1995, and, as the most extensively studied filter, is the filter design with which current filters are compared. Over the past few decades, several additional filter designs have been developed that have favorable properties, including ease of deployment, clot-trapping effectiveness, preservation of IVC flow, designs that allow filter retrieval or conversion of filter to a non-filtering device. This chapter reviews IVC filter design features, current available IVC filter types, clinical indications and guidelines for use, anatomic considerations, and techniques for placement and retrieval.
The functional goal of filters is to prevent PE by trapping venous thromboemboli in the vena cava. There are several features that are preferred for optimal function and minimal compromise, including the use of non-thrombogenic, biocompatible, non-ferromagnetic, durable implantable material. Filtering efficiency should be high without impedance of flow, and there should be a single trapping level and conical design, which provides the highest filtering-to-flow volume ratio. Ideally, the filter should have a self-centering mechanism with secure fixation to the vena cava wall, a filter hook length and angle sufficient to prevent migration when the filter is in place, and the ability to be retrieved when no longer needed without limitation of the time frame for incorporation. The optimal filter should be highly visible on imaging with ease of percutaneous delivery through a low-profile system and a simple release mechanism. Repositioning and retrievability should also be possible, and the potential for complications should be negligible. The financial cost of filter delivery should be low.
Vena cava filter design categories include the following:
Permanent filter. Placed with the intention of providing permanent, lifelong filtration, permanent filters have design characteristics that maximize secure fixation.
Optional (retrievable) filter. May have some similar design features and can function as permanent filters, optional or retrievable filters have the added feature of removal capability. Optional filters adhere to the wall of the vena cava with hooks, barbs, or radial force (or any combination of the three) but can be retrieved by image-guided catheter techniques within a device-specific time interval.
Temporary filter. These filters are not designed for permanent placement and do not have any means of fixation to the vena cava wall. Rather, temporary filters are attached to a wire or catheter that traverses the venous system and protrudes from the skin to facilitate subsequent removal.
Convertible filter. Functioning initially as a permanent filter with elements allowing attachment to the vena cava wall, convertible filters are altered structurally to allow for conversion to a non-filtration state after implantation.
Understanding individual filter structural designs, advantages, and limitations is important before placement to ensure proper filter selection. For the purpose of this chapter, only US Food and Drug Administration (FDA)-approved permanent and optional/retrievable filter designs are discussed ( Table 153.1 and Fig. 153.1 ).
| Filter Device | Manufacturer | Material | Design | Approach | Delivery Catheter Size: Inner Diameter (Fr) | Maximum Caval Diameter (mm) | Maximum Deployed Length (mm) | FDA-Approved Use |
|---|---|---|---|---|---|---|---|---|
| Stainless steel Greenfield filter | Boston Scientific, Natick, MA | Stainless steel | Conical Single trapping |
Femoral/jugular | 12 | 28 | 49 | Permanent |
| Titanium Greenfield filter | Boston Scientific, Natick, MA | Titanium | Conical Single trapping |
Femoral/jugular | 12 | 28 | 47 | Permanent |
| Simon nitinol filter | Bard Peripheral Vascular, Tempe, AZ | Nitinol | Conical Bilevel |
Femoral/jugular/antecubital | 7 | 28 | 38 | Permanent |
| Denali | Bard Peripheral Vascular, Tempe, AZ | Nitinol | Conical Bilevel |
Femoral/jugular | 8.4 | 28 | 50 | Optional |
| VenaTech LP filter | B. Braun/VenaTech, Bethlehem, PA | Cobalt Chromium | Conical Single trapping |
Femoral/jugular | 7 | 28 | 43 | Permanent |
| VenaTech Convertible | B. Braun/VenaTech, Bethlehem, PA | Cobalt Chromium |
Conical Single trapping |
Femoral/jugular | 12.9 | 28 | — | Convertible |
| TrapEase filter | Cordis Endovascular, Miami, FL | Nitinol | Double basket | Femoral/jugular/antecubital | 6 | 30 | 50 | Permanent |
| OptEase filter | Cordis Endovascular, Miami, FL | Nitinol | Double basket | Femoral/jugular/antecubital | 6 | 30 | 54 | Optional |
| Bird’s nest filter | Cook Inc., Bloomington, IN | Stainless steel | Variable | Femoral/jugular | 12 | 40 | 80 | Permanent |
| Günther Tulip filter | Cook Inc., Bloomington, IN | Conichrome | Conical Single trapping |
Femoral/jugular | Femoral 8.5 Jugular 7 |
30 | 50 | Optional |
| Celect Platinum | Cook Inc., Bloomington, IN | Conichrome | Conical Single trapping |
Femoral/jugular | 7 | 30 | 51 | Optional |
| ALN Optional Filter | ALN, Bormes Les Mimosas, France | Stainless steal | Conical | Femoral/jugular/brachial | 7 | 28 | 55 | Optional |
| Option, Option Elite | Argon Medical Devices, Inc., Plano, TX | Nitinol | Conical | Femoral/jugular/ antecubital/popliteal | 6.5 | 30 | 56.5 | Optional |
| Sentry | Boston Scientific, Natick, MA | Nitinol frame, Bioabsorbable filament | Conical | Femoral/jugular | 7 | 16–28 | 57.7 | Convertible |
| Angel Catheter | Mermaid Medical | Nitinol | Conical | Femoral | 8 | 15–30 | 50 | Temporary |
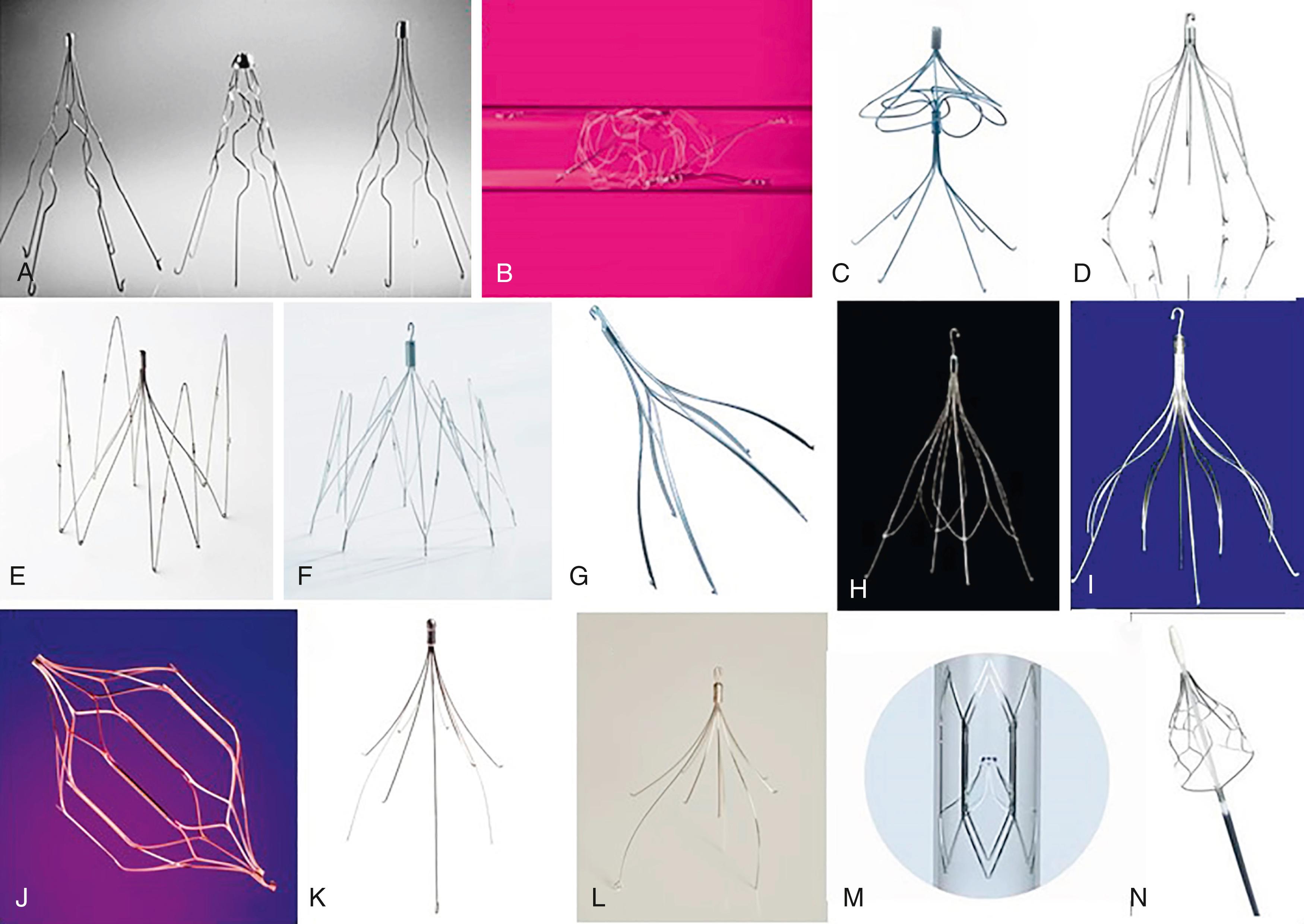
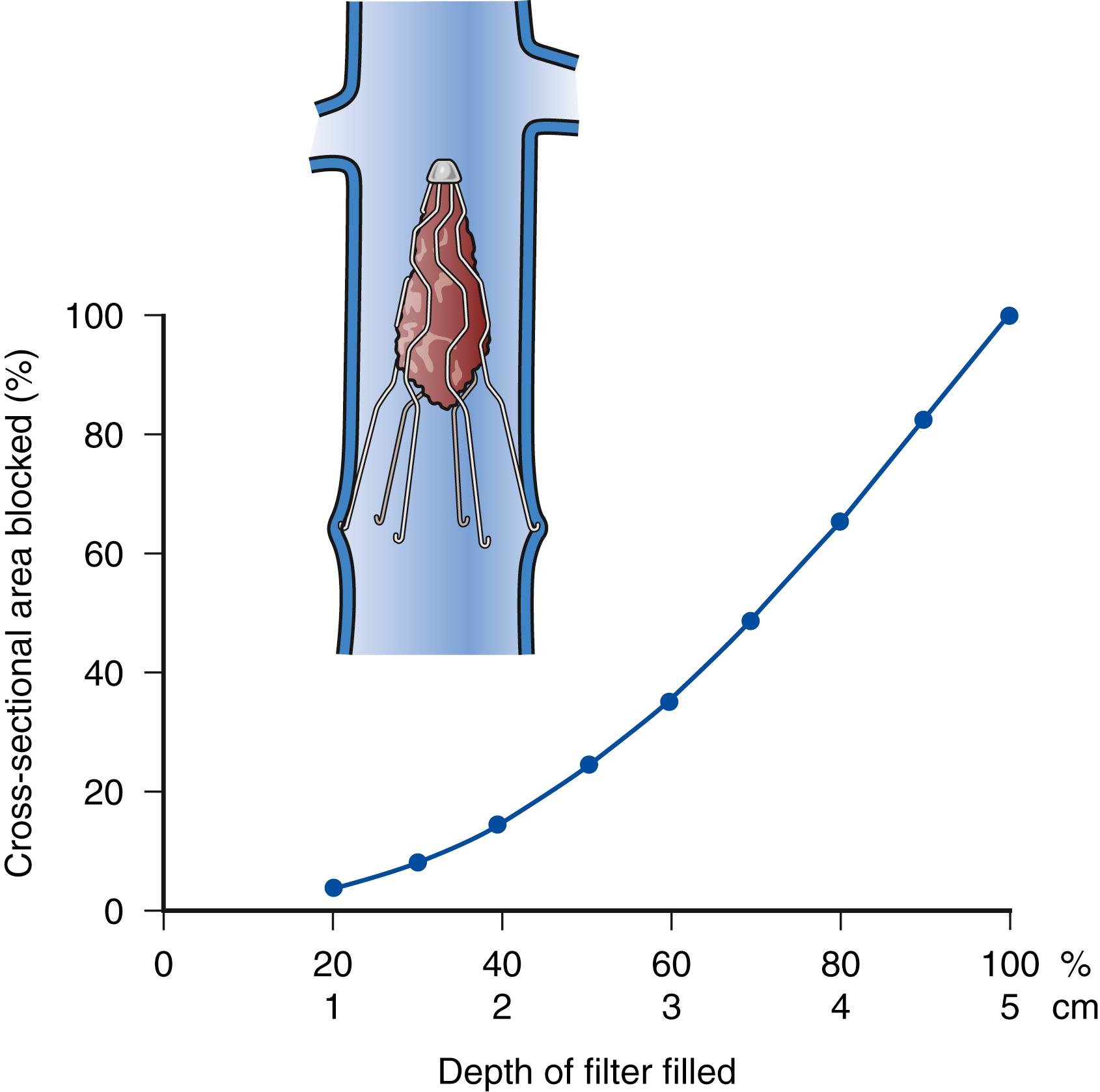
Conical filter design is optimal and permits progressive central filling while allowing circumferential blood flow peripherally, which helps to maintain vena cava patency. For example, the conical geometry of the Greenfield filter makes it possible for thrombi to fill and occlude 70% of the filter cone, a volume of thrombus of approximately 4 cm 3 (34.3% of the total volume), while reducing the cross-sectional area by less than 50%. If the cone is filled to 80% of total volume, the reduction in cross-sectional area is 64%, at which point venous flow begins to decrease and venous pressure proximal to the filter begins to increase ( Fig. 153.2 ). Although other filter designs have double trapping levels or double basket designs and have higher capacity to capture smaller emboli, flow dynamics are reduced compared with single trapping conical designs and may be associated with higher vena cava occlusion rates.
Although rapid and stable incorporation may be desirable for permanent filter design to maintain position and prevent migration, retrievable filter designs need to have sufficient incorporation to prevent migration but not so much that retrieval cannot be accomplished. Altering the filter hook contact point to allow retrievability may have the disadvantage of an increased tendency for filter leg penetration or filter migration. This has also resulted in different filter hook length and angle configurations. Although some filters (such as Greenfield filter) incorporate recurved configuration to create a contact angle of 80 degrees, allowing better hook incorporation without full penetration into the vena cava, other filters (such as Celect Platinum, Denali, OptionElite, ALN Optional filters) use different hook configuration to prevent excessive incorporation and facilitate retrievability. Filter designs such as VenaTech LP and OptEase do not depend on filter legs for fixation, thereby minimizing potential for penetration. Similarly, although some filters do not have self-centering features, others such as Denali and Celect Platinum have included independent self-centering mechanisms to minimize potential tilt. To improve self-centering of the filter, some designs such as VenaTech LP and Optease have increased contact points with the vena cava wall, which prevents tilt but may lead to increased incorporation and a possible tendency for vena cava occlusion. While these additional filter features may allow for better centering to better optimize flow dynamic, they do not offer any additional filtering capacity and can potentially lead to filter centering strut penetration of the vena cava wall.
Newer filter technology has led to availability of convertible filter designs which function as a filter upon deployment but are altered structurally to allow for conversion to a non-filtration state after implantation. Filters such as Vena-Tech Convertible requires removal of the filtration portion through a separate percutaneous procedure. Filters such as Sentry have a dissolvable filament that allows spontaneous bioconversion with retraction of the filter arms to the IVC wall around 60 days thereby restoring an open unobstructed IVC lumen.
A temporary filter (Mermaid Angel catheter) is also now clinically available and is designed to remain attached to a central venous catheter, allowing placement and removal at the bedside in critical care patients who may need transient protection during critical illness. The conical, self-expanding, nitinol filter has wide proximal openings that allow the capture of clots in the distal end of the filter. The distal end of the filter is free floating on the central venous catheter so that the filter can expand to the diameter of the vena cava. The filter is permanently attached to the multi-lumen catheter to ensure secure positioning, while simultaneously providing access to the central venous system for administration of medications, fluids, or blood products; blood sampling; and monitoring of central venous pressure. Attachment to the catheter facilitates retraction of the filter bedside when filtration is no longer needed.
Because of difficulties comparing data on different filters, several guidelines outlining reporting standards for filter devices have been published. Potential vena cava filter-related complications include the following definitions:
Filter migration or embolization. Movement of the filter from its deployment position by >2 cm in either caudal or cephalad direction.
Thrombotic occlusion. Occlusion of the vena cava at the level of the IVC filter, can be primary, caused by the presence of the filter, or secondary after capture of thromboembolic debris.
Filter tilt. Tilting of the filter compared to the IVC axis by >15 degrees, which can decrease effective filtration and protection from PE.
Filter perforation. Extension of the filter strut or anchor >3 mm beyond the adventitial layer of the vena cava wall.
Filter fracture. Loss of structural integrity of the filter leading to separation of filter leg components.
Overall reported complications for vena cava filters include pulmonary embolism (PE) (2%–5%), fatal PE (0.7%), death linked to filter insertion (0.12%), venous access site thrombosis (2%–28%), filter migration (3%–69%), vena cava penetration (9%–24%), vena cava obstruction (6%–30%), venous insufficiency (5%–59%), filter fracture (1%), and guide wire entrapment (1%). , Penetration of the IVC wall by filters is also being noted with increasing frequency. In a systematic review, overall frequency was 19%, with 8% exhibiting symptoms usually due to organ/structure involvement. Although asymptomatic filter penetration is often noted incidentally on imaging, endovascular retrieval or surgery is usually required for symptomatic patients. Table 153.2 summarizes data on different filter types. Overall, most of the available filters are approximately equivalent in prevention of PE, but there is some variation in complication rates.
| Filter Device | PE: Overall (%) | Complication Rates | Tilt >15 degrees | Filter leg penetration (%) | |||
|---|---|---|---|---|---|---|---|
| PE: Fatal (%) | Insertion Site Thrombosis (%) | Vena Cava Thrombosis (%) | Filter Migration (%) | ||||
| Stainless steel Greenfield | 3.5 | 1.3 | 8.6 | 3.5 | 2.0 | a | 2–15 |
| Titanium Greenfield | 3.4 | 1.8 | 13.1 | 4.4 | 7.5–15 | a | 13–50 |
| Percutaneous stainless steel Greenfield | 2.7 | 0.3 | 4.3 | 3 | 2.6 | a | 1.0 |
| Simon nitinol | 3.3 | 1.8 | 11.5 | 5.2 | 0–5 | a | 25–95 |
| Bird’s nest | 3.4 | 1.5 | 7.4 | 2.8 | 1.1 | a | 85 |
| VenaTech LP or LGM | 3.6 | 0.9 | 15.3 | 9.5 | 6-18.4 | a | a |
| TrapEase | 0.9 | a | 0.4 | 2 | 0.9 | ||
| OptEase | 1.6 | a | 0.8 | 3.7 | 0.3 | 5.6 | 1.9 |
| G2 | 3.4 | a | — | 3.7 | 4.5 | 44 | |
| Recovery G2 | 1.0 | a | 10.4 | 1.0 | 0.8 | 15.5 | 15.1 |
| Günther Tulip | 0.9 | 0.4 | a | 2.3 | 0.7 | 5.9 | 22–78 |
| Celect | 1.1 | a | 1.2 | 0.6 | 0.6 | 12.1 | 22–93 |
| ALN Optional | 0.7 | a | 14.0 | 1.8 | 0.5 | a | 3.4 |
| Rex Option | 4.0 | a | 18.0 | 1.0 | 2.0 | a | 2.9–10 |
| Denali | a | a | a | a | a | a | 2.5 |
a Limited or insufficient systematically reviewed published data to report.
Although it remains unclear whether filters actually improve survival, they do provide protection against PE. Because the risk for PE in patients with proven VTE and contraindications to anticoagulation is high, potential complications of filters must be balanced against the risk of no filter. Randomized evidence on permanent filters is limited. In the PREPIC (Prevention of Recurrent Pulmonary Embolism by Vena Cava Interruption) trial, 400 patients with proximal DVT with or without PE were randomized in a 2 by 2 factorial study design to filter placement versus no filter and unfractionated heparin versus enoxaparin. There was a significantly lower incidence of PE with filter protection during the first 12 days (1.1% vs. 4.8%), but the filter group had a significantly increased incidence of recurrent DVT at 2 years (20.8% vs. 11.6%). Eight-year follow-up data from the PREPIC trial confirmed the previous findings of cumulative recurrent PE (6.2% vs. 15.1%, filter vs. no filter, respectively) but increased recurrent DVT (35.7% vs. 27.5%) and no difference in post-thrombotic venous insufficiency or survival. The authors concluded that although permanent filter use may be beneficial in patients at high risk for PE, systematic use in the general population with VTE is not recommended. Unfortunately, no firm conclusions regarding filter efficacy in the prevention of PE can be drawn from the PREPIC trial given that the study design varies significantly from the wider application in current clinical practice (i.e., patients with documented VTE in whom anticoagulation has failed or cannot be administered).
Given the paucity of randomized data, determining the best permanent versus optional filter design is difficult. Some studies have used meta-analysis of data to compare the different filter designs and document the efficacy of filters in the prevention of PE and complication rates. In the randomized open label, blinded end point PREPIC-2 trial for hospitalized patients with acute PE, the use of retrievable vena cava filters plus anticoagulation compared with anticoagulation alone did not reduce the risk of symptomatic recurrent PE at 3 months. Although PREPIC-2 did not support the use of retrievable filter in patients with acute PE who can be anticoagulated, the role of retrievable filters in patients who cannot be anticoagulated, those with DVT but no PE, or for other selected relative indications remains unclear based on current evidence.
Despite lack of clear supporting evidence, filter use expanded significantly in the United States over the past few decades, but has seemingly peaked with most volume trends now in the downward direction. This increase in filter utilization seemed to parallel availability of optional filters and their expanded use for VTE prophylaxis. With the expanding use of optional vena cava filters, there has been a growing body of literature and reports to the FDA Manufacturer and User Facility Device Experience (MAUDE) database that led FDA to issue a communication of risk of adverse events with long-term use on August 9, 2010: “Since 2005, the FDA has received 921 device adverse event reports involving IVC filters, of which 328 involved device migration, 146 involved embolizations (detachment of device components), 70 involved perforation of the IVC, and 56 involved filter fracture.” The FDA raised concern that some of these events may be related to retrievable filters being left in place for an extended time, beyond the time when risk of PE has subsided. As a result, the FDA recommended that “implanting physicians and clinicians responsible for the ongoing care of patients with retrievable IVC filters consider removing the filter as soon as possible when protection from PE is no longer needed.” In an external follow-up study of the MAUDE database of 1606 reported adverse events involving 1057 filters, 86.8% involved retrievable filters vs. 13.2% for permanent filters, although this data source is limited by self-reporting mechanisms and may underestimate true filter complication rates. The FDA updated the original 2010 safety communication on May 6, 2014, reiterating the importance of filter removal as soon as protection from PE is no longer needed and when the risk/benefit profile favors removal based on the patient’s overall health status. In addition, the FDA is now requiring collection of clinical data for currently marketed IVC filters in the United States to address further safety questions for both permanent and retrievable filter designs either by manufacturers conducting postmarket studies (522 studies) or through manufacturers’ participation in the ongoing PRESERVE (PREdicting the Safety and Effectiveness of InferioR VEna Cava Filters) study, which began enrolling in 2015.
Complicating the decision to use retrievable filters is poorly defined timing of possible retrieval. For example, based on FDA indications for use (IFU), retrieval of Günther Tulip filters is recommended within 20 days, OptEase filters within 14 days, and the Celect filter within 52 weeks, while more recently approved filters like Denali, OptionElite, and ALN Optional do not have clearly specified time windows for retrieval. Further confusing best timing are case reports suggesting that potential retrieval at extended periods is possible for all filters but can be more problematic with a higher failure to retrieve rates. Regardless, the longer a filter is in place, the less successful retrieval will be, as shown in a recent systematic review documenting technically successful retrieval rates of 99% at 1 month and 94% at 3 months, falling to 37% at 12 months. Until further data are available, the optimal period for retrieval of currently available optional filters probably falls within a few months of placement, after which the technical success of retrieval will diminish.
Data on the efficacy and safety of retrievable filters are derived from smaller series with insufficient long-term data in comparison to other permanent filter designs to warrant permanent implantation. With the lack of extended outcome data for optional filters, the decision to use a retrievable filter instead of a permanent filter should be based on the intent to discontinue filtration. To determine optimal timing for filter retrieval based on a mathematical model, the FDA published a quantitative decision analysis weighing risk of PE versus risk of IVC filters over time showing a risk–benefit profile cross point favoring removal of IVC filter between 29 and 54 days. Factored into this decision of permanent vs. optional filter should be the anticipated required duration of protection from VTE vs. the risk associated with anticoagulation compared to increased filter dwell time. In patients with proven VTE, anticoagulation should be resumed as soon as possible when the risk has diminished. For patients in whom filters are placed for prophylaxis of VTE, anticoagulation should be restarted in accordance with published VTE prophylaxis guidelines. When the risk of resuming anticoagulation is extended, permanent filtration may be preferable. Optional/retrievable filters should not be used as a replacement for a permanent filter if permanent PE prevention is needed. Optional filters are preferred in the following clinical scenarios: (1) indications for permanent filters are not present; (2) the risk of clinically significant PE is acceptably low; (3) return to high risk for VTE is not anticipated; (4) life expectancy is long enough that the benefit of filter removal will be realized; and (5) the filter can be removed safely or converted.
Indications for the use of vena cava filters are shown in Box 153.1 , and supported by the evidence-based guidelines from the 2012 and 2016 American College of Chest Physicians (ACCP). , Without anticoagulation, the risk of PE developing in patients with VTE is high, and it may be fatal in as many as 25% of patients (see Ch. 152 , Pulmonary Embolism: Presentation, Natural History, and Treatment). In general, both 2012 and 2016 ACCP guidelines, and 2019 American Society of Hematology guidelines recommend against IVC filter use for prophylaxis, although the strength of this recommendation varies based on low certainty in the evidence of effects. Resumption of anticoagulation as soon as possible is recommended because, although vena cava filters are effective in preventing PE, they are not for prevention of DVT.
Documented VTE with contraindication to anticoagulation
Documented VTE with complications of anticoagulation
Recurrent PE despite therapeutic anticoagulation
Documented VTE with inability to achieve therapeutic anticoagulation
Poor compliance with anticoagulation
Free-floating iliocaval thrombus
Renal cell carcinoma with renal vein extension
Venous thrombolysis/thromboembolectomy
Documented VTE and limited cardiopulmonary reserve
Documented VTE with high risk for anticoagulation complications
Recurrent PE complicated by pulmonary hypertension
Documented VTE – cancer patient
Documented VTE – burn patient
Documented VTE – pregnancy
VTE prophylaxis – high-risk surgical patients
VTE prophylaxis – trauma patients
VTE prophylaxis – high-risk medical condition
Chronically occluded vena cava
Vena cava anomalies
Inability to access the vena cava
Vena cava compression
No location in the vena cava available for placement
Expanded relative indications based on inconclusive evidence have included poor compliance with anticoagulation; free-floating iliocaval thrombus; renal cell carcinoma with renal vein extension; placement in conjunction with venous thrombolysis or thromboembolectomy; presence of DVT and limited cardiopulmonary reserve or chronic obstructive pulmonary disease; recurrent PE complicated by pulmonary hypertension; proven DVT in an oncology, burn, or pregnant patient; and venous prophylaxis in high-risk surgical, medical, or trauma patients, as shown in Box 153.2 .
Critically ill
Previous DVT
Family history of DVT
Morbid obesity
Malignancy
Known hypercoagulable state
Prolonged immobility
Multiple traumatic injuries
Spinal cord injury
Closed head injury
Complex pelvic fractures
Multiple long-bone fractures
Major operation
Intracranial hemorrhage
Solid intra-abdominal organ injury
Pelvic or retroperitoneal hematoma
Ocular injury
Medical problems (cirrhosis, end-stage renal disease, peptic ulcer disease, medication, coagulation disorder)
Recent multi-societal clinical practice guidelines in 2020 review the most updated evidence and provides more current recommendations for the use of IVC filters in a range of clinical scenarios. These multispecialty guidelines are summarized in Box 153.3 . As outlined in the 2019 American College of Radiology Appropriateness Criteria for Management of Venous Thromboembolism – IVC filters, evidence-based guidelines are applied to specific clinical conditions and after an extensive analysis of current medical literature from peer-reviewed journals and the application of well-established methodologies (RAND/UCLA Appropriateness Method and Grading of Recommendations Assessment, Development, and Evaluation, GRADE), the appropriateness of IVC filters for these specific clinical scenarios has been rated. The appropriate use criteria for IVC filters is shown in Table 153.3 .
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here