Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Pediatric trauma is the leading cause of death in children older than one year in the United States. Although vascular injuries are infrequent, occurring in 0.6% to 1% of trauma patients, , they constitute an important cause of mortality after trauma. Efforts to curb death and morbidity after automobile accidents, such as wearing seat belts and using car seats, may have mitigated the mortality due to pediatric vascular injuries but other studies suggest that the rate of vascular injuries has not been significantly affected. , Likely, the most common cause of pediatric vascular injury is iatrogenic injury after peripheral interventions. Outside of the United States and Europe, warfare which does not discriminate civilians from combatants has also resulted in significant vascular injuries among noncombatants, many of whom are, unfortunately, young children. ,
The spectrum of treatment choices for vascular injuries includes expectant therapy, vessel ligation, direct vessel repair, or interposition graft repair. In adult patients, both endovascular and open vascular options are available. It is difficult to standardize the management of pediatric patients with vascular injuries due to a diverse set of factors. First, these vascular injuries are rare, occurring in less than 0.6% of pediatric patients who present with trauma. Additionally, many different specialties participate in repair of these injuries ranging from pediatric surgeons, adult trauma surgeons, vascular surgeons, orthopedic surgeons, neurosurgeons and plastic surgeons. Each specialty brings their unique perspective and background in how to deal with these injuries, which makes arriving at a consensus difficult. Furthermore, pediatric vascular injuries are far more technically challenging to treat, and this adds significant complexity to the choice of treatment for these injuries. The unique issues with these patients include size (diameter) of the injured vessel, spasticity of young vessels, and the choice of treatment must accommodate ongoing axial growth in this pediatric population. It is possible to apply the same principles and techniques of adult trauma to the older child, but the younger child may require different approaches. For example, in pediatric patients with blunt vascular injuries, historically, definitive arterial reconstruction has not always been the preferred management approach. Ligation or expectant therapy (systemic heparin without repair) was the most common choice of treatment. Adverse outcomes, such as loss of axial growth leading to debilitating gait disturbances, limb overgrowth due to traumatic arteriovenous fistula (AVF), and amputation have prompted calls for a more aggressive approach in management of pediatric extremity vascular injuries.
This chapter is structured to describe the multiple components associated with pediatric vascular injuries including epidemiology, diagnosis, treatment, and outcomes of these injuries.
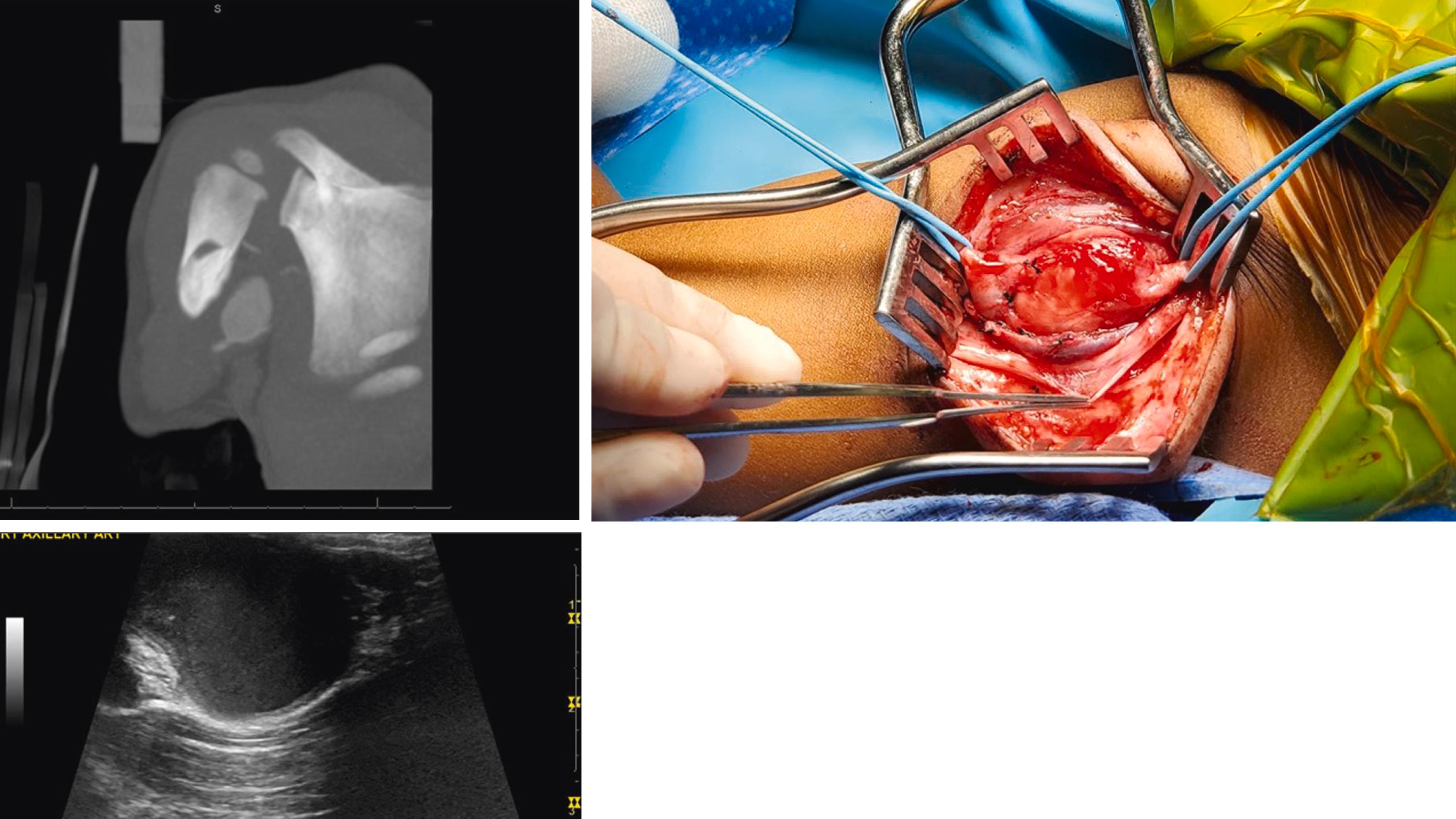
The reported incidence of any vascular injury among patients younger than 16 years is 0.6% in the US National Trauma Data Bank. This, however, does not account for iatrogenic injuries that are sustained during instrumentation for vascular or cardiac procedures ( Fig. 188.1 ). Although the exact prevalence of iatrogenic injuries is unknown, since these occur during hospitalization for admissions other than trauma, few case series have evaluated their experience with these types of injuries. In tertiary pediatric hospitals, iatrogenic vascular injuries range from 33% to 100% of an institution’s experience with pediatric vascular trauma. These penetrating vascular injuries can occur from misadventures during intravenous (IV) insertion, arterial puncture for blood gas analysis, transfemoral diagnostic or intervention procedures, umbilical artery catheterization or during surgery (e.g., during cardiopulmonary bypass operations or during orthopedic procedures). It is estimated that half of pediatric vascular injuries across all ages are iatrogenic penetrating injuries. The prevalence of iatrogenic injuries decreases with advancing age. Neonates have the highest frequency of iatrogenic vascular injuries which then declines in the 2- to 6-year-old range (50% iatrogenic), followed by those children over 6 (33% iatrogenic). Lin and colleagues identified four factors in their series of patients with iatrogenic injuries that were associated with increased risk of iatrogenic femoral complications. These included: age younger than 3 years, type of therapeutic intervention, ≥3 earlier catheterizations and the use of a 6-F or larger guide catheter. Even with heparinization and use of appropriately sized catheters, the thrombosis rate ranges from 1% to 25%. , Both artery and vein accessed can be thrombosed after intervention. In a report of neonatal injuries after instrumentation, for example, two of seven patients presented with phlegmasia cerulea dolens who were interestingly successfully treated by leech therapy.
Other causes of vascular trauma become more prevalent as a child’s age increases and, as noted above, more than two-thirds of vascular injuries in children over the age of 6 are due to noniatrogenic causes. Mechanism of pediatric vascular injuries differs in and out of war zones. In a review of the National Trauma Data Bank, the most common cause of trauma in children was motor vehicle accidents. , Other causes of trauma in decreasing order of frequency included firearm injuries, stab wounds, and falls. , Blunt injuries constituted the majority of injuries in this study of the US National Trauma Registry , which was similar to Swedish registry data. In most large contemporary single institutional studies, penetrating causes were the most frequent causes of noniatrogenic vascular injuries in children over 6 years of age. , , , It is observed that pediatric patients with blunt injury had an overall higher injury severity score than those presenting with penetrating injuries. Needless to say in areas of the world in which children are exposed to warfare, these unfortunate children are more prone to sustain penetrating vascular injuries due to high-energy gunshot wounds and IEDs with complex wounds and combined bony and tissues injuries.
Anatomic location of injuries is somewhat dependent on the mechanism of injury. Overall, however, the most common site of noniatrogenic vascular injuries in pediatric population is upper extremity vessels. , , , , Penetrating upper extremity injuries are significantly more common than the truncal vessels, which include abdominal, thoracic, and cervical vessels. Among patients with blunt mechanism of injury, upper extremity vessel injuries constitutes a third of vascular injuries often combined with an orthopedic trauma. , In patients with noniatrogenic injuries, penetrating injuries are significantly more common in the vessels of the upper extremity than other vessels. , , , , Neck vascular and truncal artery injuries, however, carry the highest mortality rates, in excess of 50%. , , Most of these patients sustain concomitant significant organ injuries , and these patients have significantly higher injury severity scores (ISS) than patients with other injuries (e.g., 45.4 ± 19.8 vs. all injured patients 12.3 ± 11.7 in one study ). In one study, truncal injuries significantly increase the odds of mortality independent of all other confounders. In a contemporary NTDB study, site of injury was not an independent statistically significant factor of mortality in multivariate analysis although the odds of mortality increased ( P = NS) with neck and truncal vascular injuries. However in this study, ISS score, Glasgow coma scale of less than 9 and shock (defined as SBP <90) were all independent predictors of mortality.
It should be noted that venous injuries are less common than arterial injuries and more difficult to diagnose in pediatric population. For that reason, there are few studies on the natural history of these injuries and consequently not too many scientifically proven guidelines on how to manage this type of injury. It is noted that combined arterial and venous injuries significantly increase the odds of mortality. In most contemporary studies of pediatric vascular injuries, the most common site of observed venous injury was the IVC , , followed by other truncal vessels, such as cervical veins, portal veins, and iliac veins. The most commonly injured extremity vein is the femoral vein. In one study of injuries to the truncal vessels, Hamner et al. noted a mortality rate of 67% among patients with IVC injury making these injuries significantly morbid.
Anatomical landmarks used to access arteries and veins in adults for insertion of large-bore IV catheters or arterial access are not as helpful in children, and this is one of the major contributing factors to iatrogenic injuries in children. In children, for example, there are reports of 12% to 33% minor overlap of femoral vein and artery which can lead to inadvertent arterial injury during venous access obtained without ultrasound guidance. Use of ultrasound during peripheral intervention has shown to significantly decrease complications after interventional procedures in adults, but the effects of routine use of ultrasound on preventing these injuries among the pediatric population merit further exploration.
Another significant contributor to the iatrogenic injuries is the size of vessels used for pediatric interventions. Using ultrasound, Warkentine et al. showed a significant correlation between size of the femoral artery and child’s weight and body surface area. In a large study of pediatric patients undergoing cardiac catheterization, the authors developed a risk scoring system for the prediction of serious adverse events (SAE) among these pediatric patients. In this model, age <30 days and weight <2.5 kg, and procedures that required endovascular intervention (i.e., required larger sheaths) were highly predictive of SAEs that included vascular injuries. These findings correlate well with the observation by Lin et al. noting a high correlation of vascular injuries with the use of larger (>6 F) sheath. The effects of sheath size and complications afterward in pediatric population may be due to significant spasm encountered in these arteries after catheterization. In an older study, Mortensen has demonstrated complete arterial occlusion due to arterial spasm around a catheter in children. It was observed by Franken and colleagues that size of catheter in relationship to the size of artery can significantly affect arterial spasm. Franken and colleagues observed that when either catheter diameter was greater than 50% of arterial diameter or when catheter diameter was less than 1.9 mm smaller than arterial diameter significant spasm was observed. The smaller size of pediatric vessels and highly spastic nature of these vessels can lead to spontaneous thrombosis and severe persistent vasospasm that may last for hours. Other physiologic factors that contribute to arterial thrombosis in this patient population are related to the low intravascular volume and other medical conditions that exist in these children. Children requiring cardiac catheterization often suffer from low cardiac output that can also exacerbate thrombosis by relatively low flow to the distal tissue beds.
Iatrogenic and traumatic vascular injuries may lead to disruption, obstruction, or spasm of injured vessels. Obstruction of the vessel will lead to occlusion of the vessel and downstream ischemic symptoms that require urgent attention and restoration of flow. When vasospasm is suspected, conservative therapy after removal of the offending agents (e.g., a catheter) may be adequate to alleviate vasospasm and restore arterial flow. The most common pediatric vascular injury is blunt brachial artery injury after supracondylar fracture. Arterial spasm after orthopedic injury may lead to ischemic arm after this injury. These injuries are often self-limiting and improve after orthopedic repair, and unless the arm is significantly ischemic, observation and conservative therapy may be equally effective as surgery (see later). , Adjuncts. such as use of intra-arterial vasodilators or papaverine, may reverse spasm and restore blood flow if spasm does not improve. Warming the patients with injured lower extremity arteries may also reverse arterial spasm.
Unique to vascular injuries is the creation of traumatic AVFs due to iatrogenic or other traumatic causes. Since these fistulae are often asymptomatic initially, they may go undetected for years. These injuries can then lead to high-flow cardiac failure by gradual enlargement of the fistula communication and subsequent increase in demand for cardiac output. Flow disturbances due to these fistulae can lead to both high-pressure venous and ischemic arterial ulcers in the affected limb. Additionally, in certain cases, high flow to the affected extremity may lead to limb overgrowth. Once diagnosed, the majority of these AVFs can be ligated or coiled.
Diagnosis of penetrating vascular injuries is easier since these patients present with hard signs of vascular injuries. Hard signs, including external bleeding and/or expanding hematoma, are reliable indicators of vascular injuries. When these signs are absent, the diagnosis of pediatric vascular injuries requires a high index of clinical suspicion and careful vascular examination. As noted above the majority of noniatrogenic traumatic pediatric vascular injuries in countries at peace are due to blunt mechanisms. , , Without evident hard signs of vascular injuries in many patients with blunt arterial injuries, the diagnosis of pediatric vascular injuries can be difficult and requires careful vascular exam and radiographic studies. As in adults, examination of the affected and contralateral extremity includes skin color, capillary refill, and pulse examination even in the absence of actual vascular injuries, because, as noted previously, pediatric vessels are highly reactive and can go in spasm due to trauma leading to reduced or absent pulses. In one series of noniatrogenic traumatic injuries, Myers and colleagues noted 26% of intraoperative spasm as the cause of low pulse exam in pediatric patients. Additionally, combined orthopedic and arterial injuries, a very common occurrence in pediatric population, can lead to significant arterial spasm which can often be corrected after such injuries have stabilized. It is therefore important in the multiply injured child with trauma, lacking hard signs of vascular injury, to address life-threatening injuries first, resuscitate and warm the child, and then re-evaluate pulses to avoid unnecessary diagnostic tests and possible operative intervention.
In the absence of hard signs of vascular injury, serial exams using continuous wave hand-held Doppler can be an effective tool. Doppler can be used to listen to the pulse if it is absent but more importantly it can be used to measure ankle–brachial index (ABI) in the injured extremity. Doppler can also be used for measurement of the injured extremity index (IEI), which like ABI, allows for the Doppler occlusion of an injured limb compared to a non-injured extremity. Katz and colleagues showed that ABI in children younger than 2 is not as reliable as in older children. These authors observed that ABI is less than 1.0 until the child is above 25 months of age or has attained a body surface area of greater than 0.5 m 2 . For this reason, Cannon et al. recommend using IEI in children instead of ABI and recommend strong consideration of poor perfusion as due to vascular injuries or systemic causes when IEI is less than 0.9 in children older than 2 and less than 0.88 in children aged 2 and under. No direct comparisons of these two measurements are made in any study, but given the limitations of ABI in children younger than 2, IEI seems to be a more accurate objective test of ischemia due to injury. Pulse oximetry has also been shown to be effective in following patients with arterial injury, for example, in those who have blunt brachial injury due to supracondylar fracture. Regardless of the technique used, if resuscitation, warming, and correction of bony injuries does not correct the malperfusion of an injured limb, diagnostic tests should be used to identify the location and severity of the arterial injury.
Duplex ultrasound can identify the location and severity of these injuries in children suspected of vascular injuries ( Fig. 188.1 ). High specificity and sensitivity of arterial duplex suggests that Duplex should be the first investigation study in evaluating arteries and able to detect arterial injuries. Limitation of duplex is related to the location of injury and the operator’s ability to perform it. For example, duplex can be highly useful in detection of cervical carotid injuries, but it cannot assess other more proximal truncal or cephalad arterial injuries. Computed tomography (CT) angiogram (CTA) has been shown to be a very reliable study for detection of blunt truncal injuries, such as when a child has signs of direct trauma to neck, chest, or abdomen such as the seat belt sign. CTA is often employed in patients with multiple injuries and can often detect occult truncal injuries that were missed during physical exam or not appreciated due to the location of the injury ( Fig. 188.2 ). CTA has also become very useful in the detection of extremity arterial injuries in children regardless of the child’s size ( Figs. 188.1 and 188.2 ). When CTA is not helpful and in selected cases, angiography may be indicated. Angiography should be performed only as the last resort given the significant risks of angiography in young children. Angiography is very useful in identifying the location of arterial injury and may assist in distinguishing arterial injury from vasospasm. If diagnostic tests are not conclusive, in the setting of limb hypoperfusion, exploration of the suspected artery is indicated regardless of patient’s age and size.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here